Influence of Aquatic Therapy in Children and Youth with Cerebral Palsy: A Qualitative Case Study in a Special Education School
Abstract
1. Introduction
2. Materials and Methods
2.1. Design
2.2. Context
2.3. Participants
- (a)
- Family context: children and youth with a diagnosis of CP, between the ages of 3 and 21 (the age range for the school), who at the time of the study had been receiving aquatic therapy for at least one year and who signed the informed consent; their parents, who signed the informed consent.
- (b)
- Educational and therapy contexts: health care and education professionals taking care of the children involved in AT at the time of the study, members of the teaching or rehabilitation staff, and who signed the informed consent.
2.4. Sampling Strategies
2.5. Recruitment Procedure
2.6. Research Team and Reflexivity
2.7. Data Collection
2.7.1. Non-Participant Observation and Informal Interviews
2.7.2. In-Depth Interviews and Focus Groups
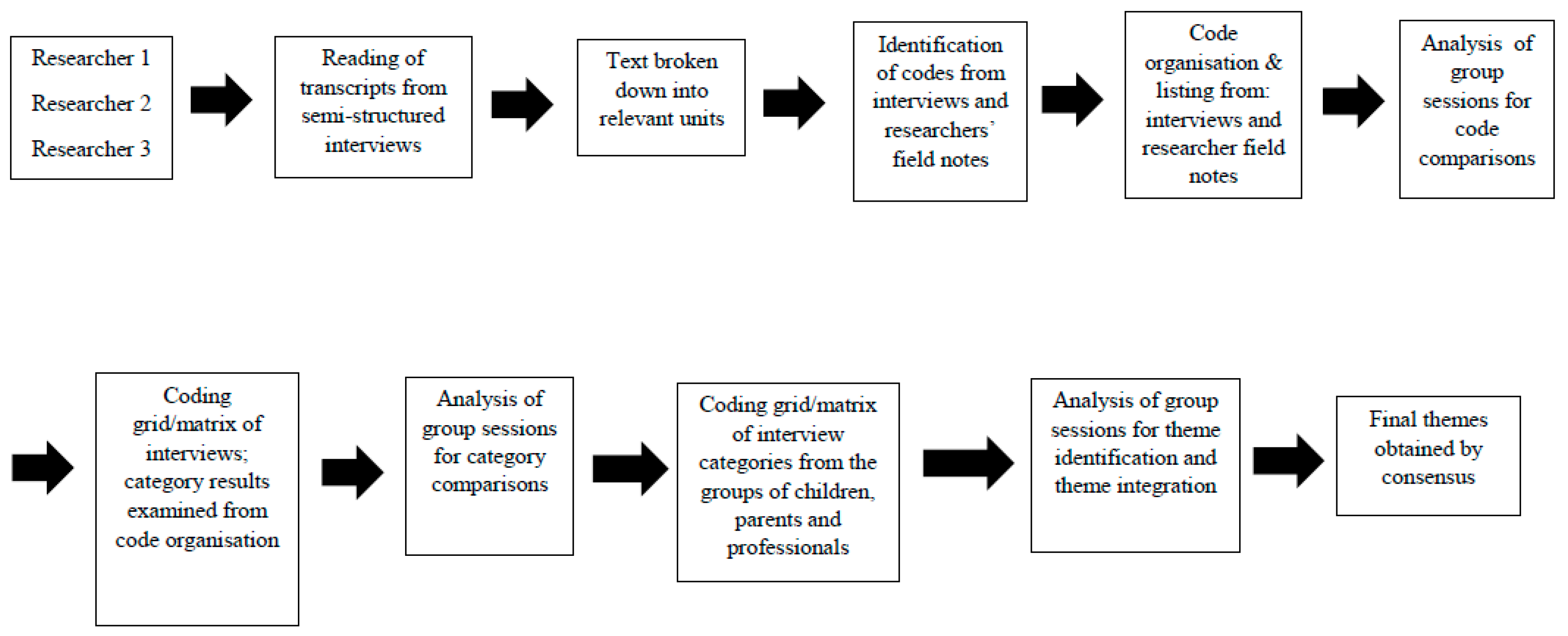
2.8. Data Analysis
2.9. Quality Criteria
2.10. Ethics
3. Results
3.1. Theme 1—Connection with the Environment
“Yes, because for me, water is like my brain, because I feel more alert, I don’t know, it’s like it wakes me up.”(Student interview)
“They pay more attention to conversations as soon as they get into the water, and then they react in the playground when something seems funny or interesting to them, they are more awake than before they get into the water.”(Therapist interview)
“He goes into the water smiling and making sounds. A huge change in behavior and attitude has taken place, compared to how subdued he was. Once in the water, he wants to kiss his therapist while he is being held in the water, breaking into laughter. Afterwards, his face is happy, coupled with an infectious laughter.”(Informal interview with participant)
“I think they become more mentally active and connected, because, for example, we go down to the pool in the summer and he is more aware of the people around him, who are splashing him, who are making different noises ... he is more attentive to the things that are close to him, more receptive and expressive of how he feels.”(Parent focus group)
3.2. Theme 2—Postural Improvements and Mobility
“It seems that when we dress her to go back to the classroom she has no joint resistance for putting her arms into the shirt sleeves. Once seated in her wheelchair she has good postural control.”(Informal interviews with participants)
“Their posture is better when they leave and as a result of this better posture they are more willing to do things for their hygiene or clothing. And I think that by moving with less effort in the water, they also improve their posture and their ability to change postures later on.”(Therapist interview)
“Those with more spasticity do come to speech therapy sessions more relaxed when they come from the pool and are more likely to work calmly.”(Therapist interview)
“Hypertonia is one of the things that makes it very difficult for them, and when they work in water they notice that they move with more fluidity in general, as it is easier for them to move their bodies in the water.”(Teacher interview)
“I feel my knees moving, that’s new, I like to feel that they are free.”(Student interview)
“... and in the pool, well if you see him, the other day, walking, in the pool, because he goes with a walker outside, and (in the pool) he walks alone, and he was encouraged to do things by himself.”(Informal participant interview)
“It is an environment where it is easier to mobilize compared to dry land conditions, so, first you see what the person can do regarding mobility in the water, and then this can be applied in the classroom or the dining room, encouraging us to reinforce this.”(Interview with therapist)
“She independently climbs the ramp leading outside the pool, sits on the mat, puts on her flip flops, and without any help from anyone, she turns over and gets out of the water.”(Informal participant interview)
“I end up exhausted, the water lets me move more, and when I finish and get out, if I’ve gone over the top, I can feel it.”(Student interview)
“Normally they come out feeling more alert, but those who spend more time in their wheelchairs do leave the pool more tired, during the session you can tell that their visual tracking worsens, so we give our own feedback so that the next pool session is lighter.”(Therapist interview)
“That day the overall experience of the parents is that they notice that they return more tired, falling asleep earlier.”(Teacher interview)
“The day at the pool is a comforting sleep... for everyone. He rests and we rest, something so necessary and unusual.”(Parent focus group)
3.3. Theme 3—Possibility of performing Tasks
“She is interacting with guttural sounds and making small joyful sounds in class. She is relaxed and attentive. There is smooth, multisensory communication.”(Informal interviews with participants)
“Although they speak a little louder and interact thanks to the technology of the tablet speaker, they remain concentrated on their work and assignments and are able to write more calmly.”(Teacher interview)
“Concerning the orofacial work, relaxation and preparation, I notice they are better after going to the pool. In this sense, afterwards, of course, this favors changes in speech, they are able to articulate better. I notice changes in swallowing and feeding on a motor level, which is what we work on the most, together with breathing.”(Therapist interview)
“After the pool, they eat the cream of zucchini soup at full speed. They tend to eat very quickly, feeling hungrier when they get out of the water. He waits for the second course by eating bread and chatting with his classmates.”(Informal interviews with participants)
“We arrive at the pool and he goes to the mirror and quickly, without hesitation, begins to undress. He does it alone, in front of the mirror, he starts taking off his top and a sneaker, he looks at himself in the mirror, smiles, gets excited by shouting, moderately.”(Informal participant interviews)
“...but it had quite a large impact on the first day and she asked her family to please shave her to go to the water, her initiative was great, but it is true that, unfortunately, we don’t have many cases that can have that much of an effect on their own hygiene, given their condition.”(Teacher interview)
“When she is in the water playing with other children I see her face that says... ‘I can do it too’, her desire to do participate, and it is not something that they usually express.”(Parent focus group)
3.4. Theme 4—Learning and Transfer
“After getting out of the water she goes to dance class, where she watches the indications given by the teacher from her wheelchair. As it is the older children’s turn to use a walker, she looks at them, leans on her adapted headboard, interacts with the music without losing sight of the dance floor, as if memorizing it, very attentive for how young she is.”(Informal interview with participant)
“J. when returning to the classroom, he worked better using the tablet for reading and writing. He writes while the teacher spells the word correctly and presses the talkfree device to hear what he has written.”(Informal participant interview)
“When they go, they are very motivated because they like it very much and they feel like going… they are like: come on, let’s finish up now, let’s do whatever we have to do and let’s go to the swimming pool and have fun.”(Professional interview)
“Although we are told that we are going to work a lot in the water, for me it is a game within the school, the fun moment.”(Student interview)
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Blair, E.; Cans, C. The definition of Cerebral Palsy. In Cerebral Palsy; Panteliadis, C.P., Ed.; Springer: Basel, Switzerland, 2018; pp. 13–17. [Google Scholar]
- Bourke-Taylor, H.M.; Cotter, C.; Lalor, A.; Johnson, L. School success and participation for students with cerebral palsy: A qualitative study exploring multiple perspectives. Disabil. Rehabil. 2018, 40, 2163–2171. [Google Scholar] [CrossRef]
- Schenker, R.; Coster, W.; Parush, S. Participation and activity performance of students with cerebral palsy within the school environment. Disabil. Rehabil. 2005, 27, 539–552. [Google Scholar] [CrossRef] [PubMed]
- Mei, C.; Reilly, S.; Reddihough, D.; Mensah, F.; Green, J.; Pennington, L.; Morgan, A.T. Activities and participation of children with cerebral palsy: Parent perspectives. Disabil. Rehabil. 2015, 37, 2164–2173. [Google Scholar] [CrossRef] [PubMed]
- Cleary, S.L.; Taylor, N.F.; Dodd, K.J.; Shields, N. A qualitative evaluation of an aerobic exercise program for young people with cerebral palsy in specialist schools. Dev. Neurorehabil. 2017, 20, 339–346. [Google Scholar] [CrossRef] [PubMed]
- Kelly, M.; Darrah, J. Aquatic exercise for children with cerebral palsy. Dev. Med. Child Neurol. 2005, 47, 838–842. [Google Scholar] [CrossRef] [PubMed]
- Gorter, J.W.; Currie, S.J. Aquatic exercise programs for children and adolescents with cerebral palsy: What do we know and where do we go? Int. J. Pediatr. 2011, 2011, 712165. [Google Scholar] [CrossRef]
- Roostaei, M.; Baharlouei, H.; Azadi, H.; Fragala-Pinkham, M.A. Effects of Aquatic Intervention on Gross Motor Skills in Children with Cerebral Palsy: A Systematic Review. Phys. Occup. Ther. Pediatr. 2017, 37, 496–515. [Google Scholar] [CrossRef]
- Brunton, L.K.; Bartlett, D.J. Description of exercise participation of adolescents with cerebral palsy across a 4-year period. Disabil. Rehabil. 2010, 32, 1501–1508. [Google Scholar] [CrossRef]
- Hurvitz, E.A.; Leonard, C.; Ayyanger, R.; Nelson, V.S. Complementary and alternative medicine use in families of children with cerebral palsy. Dev. Med. Child Neurol. 2003, 45, 364–370. [Google Scholar] [CrossRef]
- Güeita-Rodríguez, J.; García-Muro, F.; Rodríguez-Fernández, Á.L.; Cano-Díez, B.; Chávez-Santacruz, D.; Palacios-Ceña, D. Preliminary Aquatic Physical Therapy Core Sets for Children and Youth with Neurological Disorders: A Consensus Process. Pediatr. Phys. Ther. 2019, 31, 272–278. [Google Scholar] [CrossRef]
- Selb, M.; Escorpizo, R.; Kostanjsek, N.; Stucki, G.; Üstün, B.; Cieza, A. A guide on how to develop an International Classification of Functioning, Disability and Health Core Set. Eur. J. Phys. Rehabil. Med. 2015, 51, 105–117. [Google Scholar] [PubMed]
- Pope, C.; Mays, N. Qualitative Research in Health Care; Blackwell Publishing: Oxford, UK, 2006. [Google Scholar]
- Güeita-Rodríguez, J.; García-Muro, F.; Rodríguez-Fernández, Á.L.; Lambeck, J.; Fernández-de-Las-Peñas, C.; Palacios-Ceña, D. What areas of functioning are influenced by aquatic physiotherapy? Experiences of parents of children with cerebral palsy. Dev. Neurorehabil. 2018, 21, 506–514. [Google Scholar] [CrossRef] [PubMed]
- O’Connor, B.; Kerr, C.; Shields, N.; Adair, B.; Imms, C. Steering towards collaborative assessment: A qualitative study of parents’ experiences of evidence-based assessment practices for their child with cerebral palsy. Disabil. Rehabil. 2019, 23, 1–10. [Google Scholar] [CrossRef]
- Morris, A.; Imms, C.; Kerr, C.; Adair, B. Sustained participation in community-based physical activity by adolescents with cerebral palsy: A qualitative study. Disabil. Rehabil. 2018, 10, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Yin, R.K. Case Study Research: Design and Methods, 5th ed.; Sage: Thousand Oaks, CA, USA, 2014. [Google Scholar]
- Baxter, P.; Jack, S. Qualitative Case Study Methodology: Study Design and Implementation for Novice Researchers. Qual. Rep. 2008, 13, 544–559. [Google Scholar]
- Carpenter, C.; Suto, M. Qualitative Research for Occupational and Physical Therapists: A Practical Guide; Black-Well Publishing: Oxford, UK, 2008. [Google Scholar]
- Carolan, C.M.; Forbat, L.; Smith, A. Developing the DESCARTE Model: The Design of Case Study Research in Health Care. Qual. Health Res. 2016, 26, 626–639. [Google Scholar] [CrossRef] [PubMed]
- Teddlie, C.; Yu, F. Mixed Methods Sampling: A typology with Examples. J. Mix. Methods Res. 2007, 1, 77–100. [Google Scholar] [CrossRef]
- Creswell, J.W.; Poth, C.N. Qualitative inquiry and research design. Choosing Among Five Approaches, 4th ed.; Sage: Thousand Oaks, CA, USA, 2018. [Google Scholar]
- Reeves, S.; Kuper, A.; Hodges, B.D. Qualitative research methodologies: Ethnography. BMJ 2008, 337, a1020. [Google Scholar] [CrossRef]
- McCann, T.; Clark, E. Using unstructured interviews with participants who have schizophrenia. Nurse Res. 2005, 13, 7–18. [Google Scholar] [CrossRef]
- Braun, V.; Clarke, V. Using thematic analysis in psychology. Qual. Res. Psychol. 2006, 3, 77–101. [Google Scholar] [CrossRef]
- Keane, S.; Lincoln, M.; Smith, T. Retention of allied health professionals in rural new south Wales: A thematic analysis of focus groups discussions. BMC Health Serv. Res. 2012, 12, 175. [Google Scholar] [CrossRef] [PubMed]
- Miles, M.B.; Huberman, A.M.; Saldaña, J. Qualitative Data Analysis. A Methods Sourcebook, 3rd ed.; Sage: Thousand Oaks, CA, USA, 2014. [Google Scholar]
- Tong, A.; Sainsbury, P.; Craig, J. Consolidated criteria for reporting qualitative research (COREQ): A 32-item checklist for interviews and focus groups. Int. J. Qual. Health Care. 2007, 19, 349–357. [Google Scholar] [CrossRef] [PubMed]
- Shenton, A.K. Strategies for ensuring trustworthiness in qualitative research projects. Educ. Inf. 2004, 22, 63–75. [Google Scholar] [CrossRef]
- Houghton, C.; Casey, D.; Shaw, D.; Murphy, K. Rigourin qualitative case-study research. Nurs. Res. 2013, 20, 12–17. [Google Scholar] [CrossRef] [PubMed]
- World Medical Association. World Medical Association Declaration of Helsinki: Ethical principles for medical research involving human subjects. JAMA 2013, 310, 2191–2194. [Google Scholar] [CrossRef] [PubMed]
- Lai, C.J.; Liu, W.Y.; Yang, T.F.; Chen, C.L.; Wu, C.Y.; Chan, R.C. Pediatric Aquatic Therapy on Motor Function and Enjoyment in Children Diagnosed with Cerebral Palsy of Various Motor Severities. J. Child Neurol. 2015, 30, 200–208. [Google Scholar] [CrossRef]
- Sato, D.; Onishi, H.; Yamashiro, K.; Iwabe, T.; Shimoyama, Y.; Maruyama, A. Water immersion to the femur level affects cerebral cortical activity in humans: Functional near-infrared spectroscopy study. Brain Topogr. 2012, 25, 220–227. [Google Scholar] [CrossRef]
- Sato, D.; Yamashiro, K.; Onishi, H.; Shimoyana, Y.; Yoshida, T.; Maruyama, A. The effect of water immersion on short-latency somatosensory evoked potentials in human. BMC Neurosci. 2012, 13, 13. [Google Scholar] [CrossRef]
- Chrysagis, N.; Douka, A.; Nikopoulos, M.; Apostolopoulou, F.; Koutsouki, D. Effects of an aquatic program on gross motorfunction of children with spastic cerebral palsy. J. Biol. Exerc. 2009, 5, 13–25. [Google Scholar]
- Ballington, S.J.; Naidoo, R. The carry-over effect of an aquatic-based intervention in children with cerebral palsy. Afr. J. Disabil. 2018, 7, 361. [Google Scholar] [CrossRef]
- Akinola, B.I.; Gbiri, C.A.; Odebiyi, D.O. Effect of a 10-Week Aquatic Exercise Training Program on Gross Motor Function in Children with Spastic Cerebral Palsy. Glob. Pediatric Health 2019, 6, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Getz, M.; Hutzler, Y.; Vermeer, A. The relationship between aquatic independence and gross motor functionin children with neuro-motor impairments. Adapt Phys. Act. Q. 2006, 23, 339–355. [Google Scholar]
- Fragala-Pinkham, M.; Haley, S.M.; O’Neil, M.E. Group aquatic aerobic exercise for children with disabilities. Dev. Med. Child Neurol. 2008, 50, 822–827. [Google Scholar] [CrossRef] [PubMed]
- Becker, B.E. Aquatic therapy: Scientific foundations and clinical rehabilitation applications. PM R 2009, 1, 859–872. [Google Scholar] [CrossRef]
- Sato, D.; Yamashiro, K.; Yamazaki, Y.; Ikarashi, K.; Onishi, H.; Baba, Y.; Maruyama, A. Priming Effects of Water Immersion on Paired Associative Stimulation-Induced Neural Plasticity in the Primary Motor Cortex. Int. J. Env. Res. Public Health 2019, 17, 215. [Google Scholar] [CrossRef]
| Participants | Sociodemographic Data |
|---|---|
| Students | Participants: 14 (5 women) |
| Mean age (years): 10.90 (SD +/− 3.77) | |
| School attendance (years): 5.90 (SD +/− 3.91) | |
| Number of years receiving aquatic therapy: 4.45 (SD +/− 3.20) | |
| % GMFCS: II (28.5%), III (14.2%), IV (14.2%), V (42.8%) | |
| Parents | Participants: 8 (7 women) |
| Mean age: 46 (SD +/− 6) | |
| Health care professionals | Participants: 3 (3 women) |
| Mean age: 39 (SD +/− 3.5) | |
| Years of experience in CP: 12 (SD +/− 4.96) | |
| Education professionals | Participants: 2 (2 women) |
| Mean age: 36.5 (SD +/− 0.5) | |
| Years of experience in CP: 14.5 (SD +/− 2.5) |
| Participants | Data Collection Tool | Number of Participants | Setting | Time | Study Phase |
|---|---|---|---|---|---|
| Children context | |||||
| Children | Participant observation | 11 students | APACE School (Classrooms, hall, playground, dining room, speech therapy room, pool, dressing room, occupational therapy room, bathroom, dancing activity → hall, weaving workshop → classroom, physiotherapy room, corridors, social skills workshop with psychotherapist → classroom, storyteller activity → classroom) | 59 h (3540 min) | During period of intervention (October/June) |
| Minimum 40 min before aquatic intervention + minimum 40 min after aquatic intervention | |||||
| Semi-structured interviews | 3 students | APACE Classroom | 210 min | During intervention, after school | |
| (range: 63 to 77 min) | |||||
| Parents | Focus group | 8 parents | APACE School dining room | 73 min | During intervention, after school |
| Therapy context | Semi-structured interviews | 3 health professionals | Assistant → APACE Classroom | 249 min | During intervention, during breaks after school |
| Speech therapist → APACE Speech therapy room | |||||
| Physiotherapist → APACE Physiotherapy room | (range: 77 to 92 min) | ||||
| Informal interviews | 2 health professionals | APACE school | 40 min | During period of intervention | |
| Educational context | Semi-structured interviews | 2 teachers | Director → APACE Classroom | 123 min | During intervention, after school |
| Teacher → APACE Classroom | (range: 55 to 68 min) | ||||
| Informal interviews | 1 teacher | APACE school | 22 min | During period of intervention |
| Criteria | Techniques Performed and Application Procedures |
|---|---|
| Credibility | Investigator triangulation: each interview was analyzed by two researchers. Thereafter, team meetings were performed in which the analyses were compared and themes were identified. |
| Triangulation of data collection methods: interviews were conducted, and researcher field notes were kept. | |
| Participant validation: this consisted of asking the participants to confirm the data obtained during the data collection and analysis stages. | |
| Transferability | In-depth descriptions of the study were performed, providing details of the characteristics of researchers, participants, contexts, sampling strategies, and the data collection and analysis procedures. |
| Dependability | Audit by an external researcher: an external researcher assessed the study research protocol, focusing on aspects concerning the methods applied and study design. |
| Confirmability | Investigator triangulation, participant triangulation, data collection triangulation. |
| Researcher reflexivity was encouraged via the completion of reflexive reports and by describing the rationale for the study. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Muñoz-Blanco, E.; Merino-Andrés, J.; Aguilar-Soto, B.; García, Y.C.; Puente-Villalba, M.; Pérez-Corrales, J.; Güeita-Rodríguez, J. Influence of Aquatic Therapy in Children and Youth with Cerebral Palsy: A Qualitative Case Study in a Special Education School. Int. J. Environ. Res. Public Health 2020, 17, 3690. https://doi.org/10.3390/ijerph17103690
Muñoz-Blanco E, Merino-Andrés J, Aguilar-Soto B, García YC, Puente-Villalba M, Pérez-Corrales J, Güeita-Rodríguez J. Influence of Aquatic Therapy in Children and Youth with Cerebral Palsy: A Qualitative Case Study in a Special Education School. International Journal of Environmental Research and Public Health. 2020; 17(10):3690. https://doi.org/10.3390/ijerph17103690
Chicago/Turabian StyleMuñoz-Blanco, Elisa, Javier Merino-Andrés, Beatriz Aguilar-Soto, Yolanda Castillo García, Marta Puente-Villalba, Jorge Pérez-Corrales, and Javier Güeita-Rodríguez. 2020. "Influence of Aquatic Therapy in Children and Youth with Cerebral Palsy: A Qualitative Case Study in a Special Education School" International Journal of Environmental Research and Public Health 17, no. 10: 3690. https://doi.org/10.3390/ijerph17103690
APA StyleMuñoz-Blanco, E., Merino-Andrés, J., Aguilar-Soto, B., García, Y. C., Puente-Villalba, M., Pérez-Corrales, J., & Güeita-Rodríguez, J. (2020). Influence of Aquatic Therapy in Children and Youth with Cerebral Palsy: A Qualitative Case Study in a Special Education School. International Journal of Environmental Research and Public Health, 17(10), 3690. https://doi.org/10.3390/ijerph17103690






