Full Radiology Report through Patient Web Portal: A Literature Review
Abstract
1. Introduction
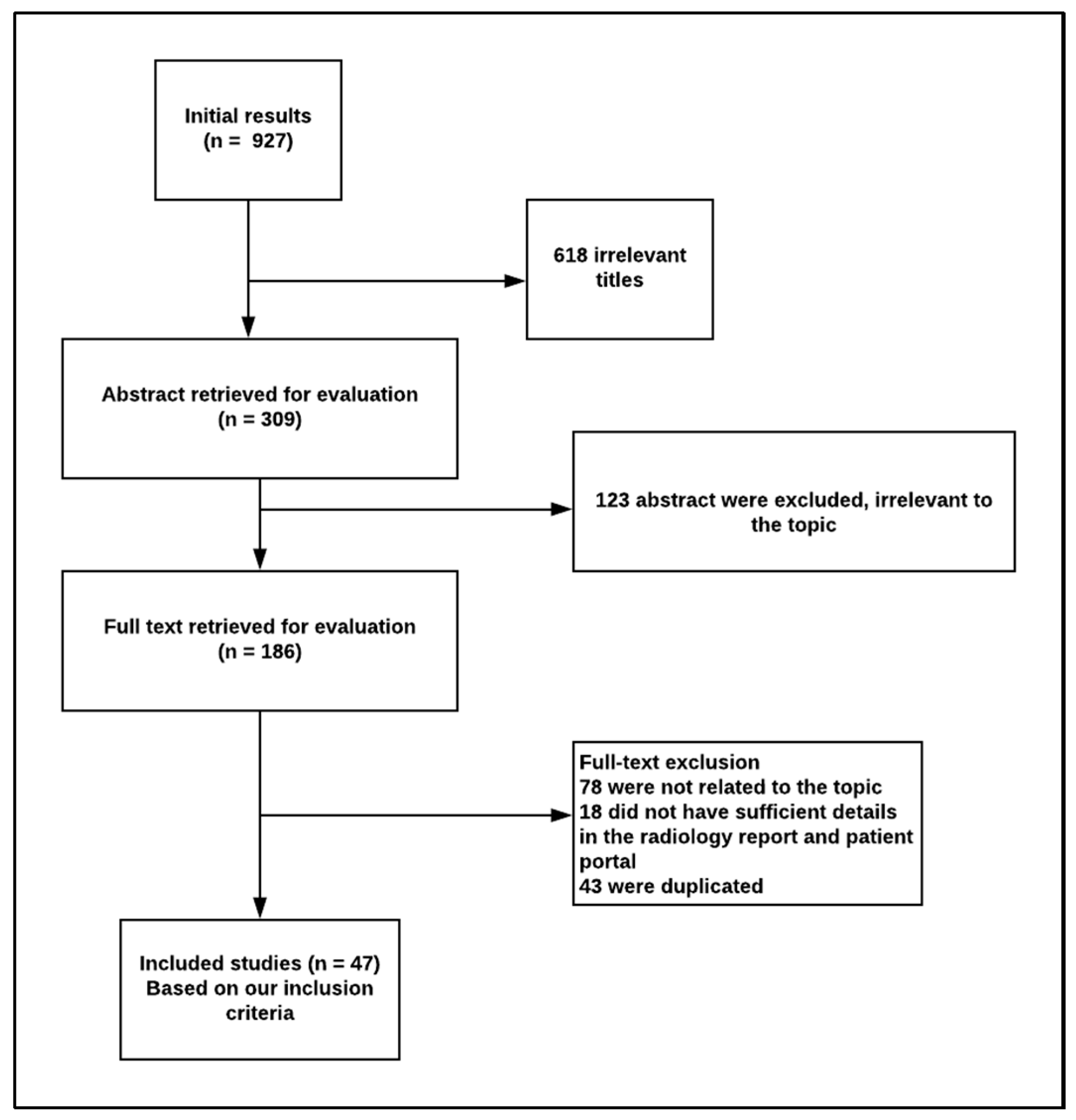
2. Materials and Methods
2.1. Context and Existing Status
2.2. Search Strategy and Criteria
3. Results
3.1. Current Radiological Reports and Patient Portal
3.2. Social Media and Patient Understanding
4. Discussion
4.1. Benefits of a Patient Portal for Patient Engagement
4.2. Impacts of the Health Communications Objectives
4.3. Addressing the Objectives
4.4. Quality Initiatives and Patient Satisfaction
4.5. Patient Portal Platforms
4.6. Limitations in the Patients’ Portal
4.7. Observed Issues
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Henshaw, D.; Okawa, G.; Ching, K.; Garrido, T.; Qian, H.; Tsai, J. Access to radiology reports via an online patient portal: Experiences of referring physicians and patients. J. Am. Coll. Radiol. 2015, 12, 582–586. [Google Scholar] [CrossRef] [PubMed]
- Miles, R.C.; Hippe, D.S.; Elmore, J.G.; Wang, C.L.; Payne, T.H.; Lee, C.I. Patient access to online radiology reports: Frequency and sociodemographic characteristics associated with use. Acad. Radiol. 2016, 23, 1162–1169. [Google Scholar] [CrossRef] [PubMed]
- Patil, S.; Lu, H.; Saunders, C.L.; Potoglou, D.; Robinson, N. Public preferences for electronic health data storage, access, and sharing—Evidence from a pan-European survey. J. Am. Med. Inform. Assoc. 2016, 23, 1096–1106. [Google Scholar] [CrossRef]
- Osborn, C.Y.; Rosenbloom, S.T.; Stenner, S.P.; Anders, S.; Muse, S.; Johnson, K.B. MyHealthAtVanderbilt: Policies and procedures governing patient portal functionality. J. Am. Med. Inform. Assoc. 2011, 18, i18–i23. [Google Scholar] [CrossRef][Green Version]
- Nazi, K.M.; Turvey, C.L.; Klein, D.M.; Hogan, T.P.; Woods, S.S. VA OpenNotes: Exploring the experiences of early patient adopters with access to clinical notes. J. Am. Med. Inform. Assoc. 2014, 22, 380–389. [Google Scholar] [CrossRef]
- Sarkar, U.; Karter, A.J.; Liu, J.Y.; Adler, N.E.; Nguyen, R.; López, A. Social disparities in internet patient portal use in diabetes: Evidence that the digital divide extends beyond access. J. Am. Med. Inform. Assoc. 2011, 18, 318–321. [Google Scholar] [CrossRef] [PubMed]
- McNamara, M.; Arnold, C.; Sarma, K.; Aberle, D.; Garon, E.; Bui, A.A. Patient portal preferences: Perspectives on imaging information. J. Assoc. Inf. Sci. Tech. 2015, 66, 1606–1615. [Google Scholar] [CrossRef] [PubMed]
- Cook, T.S.; Oh, S.C.; Kahn, C.E.J. Patients’ use and evaluation of an online system to annotate radiology reports with lay language definitions. Acad. Radiol. 2017, 24, 1169–1174. [Google Scholar] [CrossRef] [PubMed]
- Garry, K.; Blecker, S.; Saag, H.; Szerencsy, A.; Jones, S.A.; Testa, P. Patient experience with notification of radiology results: A comparison of direct communication and patient portal use. J. Am. Coll. Radiol. 2020. [Google Scholar] [CrossRef]
- Cho, J.K.; Zafar, H.M.; Cook, T.S. Use of an online crowdsourcing platform to assess patient comprehension of radiology reports and colloquialisms. Am. J. Roentgenol. 2020, 214, 1–5. [Google Scholar] [CrossRef]
- Mervak, B.M.; Davenport, M.S.; Flynt, K.A.; Kazerooni, E.A.; Weadock, W.J. What the patient wants: An analysis of radiology-related inquiries from a web-based patient portal. J. Am. Coll. Radiol. 2016, 13, 1311–1318. [Google Scholar] [CrossRef] [PubMed]
- Broman, K.K.; Oyefule, O.O.; Phillips, S.E.; Baucom, R.B.; Holzman, M.D.; Sharp, K.W. Postoperative care using a secure online patient portal: Changing the (inter) face of general surgery. J. Am. Coll. Surg. 2015, 221, 1057–1066. [Google Scholar] [CrossRef] [PubMed]
- Rosenkrantz, A.B. Differences in perceptions among radiologists, referring physicians, and patients regarding language for incidental findings reporting. Am. J. Roentgenol. 2017, 208, 140–143. [Google Scholar] [CrossRef] [PubMed]
- Gunn, A.J.; Gilcrease-Garcia, B.; Mangano, M.D.; Sahani, D.V.; Boland, G.W.; Choy, G. Journal club: Structured feedback from patients on actual radiology reports: A novel approach to improve reporting practices. Am. J. Roentgenol. 2017, 208, 1262–1270. [Google Scholar] [CrossRef]
- Martin-Carreras, T.; Cook, T.S.; Kahn, C.E.J. Readability of radiology reports: Implications for patient-centered care. Clin. Imaging 2019, 54, 116–120. [Google Scholar] [CrossRef]
- Vitzthum, V.E.; Kitts, A.B.; Swanson, C.; Hanley, M.; Krishnaraj, A. Patient-centered radiology reporting for lung cancer screening. J. Thoracic. Imaging 2020, 35, 85–90. [Google Scholar] [CrossRef]
- Oh, S.C.; Cook, T.S.; Kahn, C.E. PORTER: A prototype system for patient-oriented radiology reporting. J. Digit. Imaging 2016, 29, 450–454. [Google Scholar] [CrossRef]
- Reicher, J.J.; Reicher, M.A. Implementation of certified EHR, patient portal, and “direct” messaging technology in a radiology environment enhances communication of radiology results to both referring physicians and patients. J. Digit. Imaging 2016, 29, 337–340. [Google Scholar] [CrossRef][Green Version]
- Short, R.G.; Middleton, D.; Befera, N.T.; Gondalia, R.; Tailor, T.D. Patient-centered radiology reporting: Using online crowdsourcing to assess the effectiveness of a web-based interactive radiology report. J. Am. Coll. Radiol. 2017, 14, 1489–1497. [Google Scholar] [CrossRef]
- Martin-Carreras, T.; Kahn, C.E.J. Coverage and readability of information resources to help patients understand radiology reports. J. Am. Coll. Radiol. 2018, 15, 1681–1686. [Google Scholar] [CrossRef]
- Qenam, B.; Kim, T.Y.; Carroll, M.J.; Hogarth, M. Text simplification using consumer health vocabulary to generate patient-centered radiology reporting: Translation and evaluation. J. Med. Internet Res. 2017, 19, e417. [Google Scholar] [CrossRef] [PubMed]
- Sadigh, G.; Hertweck, T.; Kao, C.; Wood, P.; Hughes, D.; Henry, T.S. Traditional text-only versus multimedia-enhanced radiology reporting: Referring physicians’ perceptions of value. J. Am. Coll. Radiol. 2015, 12, 519–524. [Google Scholar] [CrossRef]
- Dy, G.W.; Gore, J.L.; Muncey, W.W.; Ellison, J.S.; Merguerian, P.A. Comparative effectiveness of a pilot patient-centered ultrasound report in the management of hydronephrosis. J. Pediatr. Urol. 2018, 14, e1–e7. [Google Scholar] [CrossRef] [PubMed]
- Lye, C.T.; Krumholz, H.M.; Eckroate, J.E.; Daniel, J.G.; DeBronkart, D.; Mann, M.K. Evaluation of the patient request process for radiology imaging in US hospitals. RSNA Radiol. 2019, 292, 409–413. [Google Scholar] [CrossRef] [PubMed]
- Pahade, J.K.; Trout, A.T.; Zhang, B.; Bhambhvani, P.; Muse, V.V.; Delaney, L.R. What patients want to know about imaging examinations: A multiinstitutional us survey in adult and pediatric teaching hospitals on patient preferences for receiving information before radiologic examinations. RSNA Radiol. 2018, 287, 554–562. [Google Scholar] [CrossRef]
- Short, R.G.; Befera, N.T.; Hoang, J.K.; Tailor, T.D. A normal thyroid by any other name: Linguistic analysis of statements describing a normal thyroid gland from noncontrast chest CT reports. J. Am. Coll. Radiol. 2018, 15, 1642–1647. [Google Scholar] [CrossRef]
- Yi, P.H.; Golden, S.K.; Harringa, J.B.; Kliewer, M.A. Readability of lumbar spine MRI reports: Will patients understand? Am. J. Roentgenol. 2019, 212, 602–606. [Google Scholar] [CrossRef]
- Kemp, J.L.; Mahoney, M.C.; Mathews, V.P.; Wintermark, M.; Yee, J.; Brown, S.D. Patient-centered radiology: Where are we, where do we want to be, and how do we get there? RSNA Radiol. 2017, 285, 601–608. [Google Scholar] [CrossRef]
- Alpert, J.M.; Morris, B.B.; Thomson, M.D.; Matin, K.; Brown, R.F. Implications of patient portal transparency in oncology: Qualitative interview study on the experiences of patients, oncologists, and medical informaticists. JMIR Cancer 2018, 4, e5. [Google Scholar] [CrossRef]
- Mityul, M.I.; Gilcrease-Garcia, B.; Searleman, A.; Demertzis, J.L.; Gunn, A.J. Interpretive differences between patients and radiologists regarding the diagnostic confidence associated with commonly used phrases in the radiology report. Am. J. Roentgenol. 2018, 210, 123–126. [Google Scholar] [CrossRef]
- Choudhry, A.; Hong, J.; Chong, K.; Jiang, B.; Hartman, R.; Chu, E. Patients’ preferences for biopsy result notification in an era of electronic messaging methods. JAMA Dermatol. 2015, 151, 513–521. [Google Scholar] [CrossRef] [PubMed]
- Brook, O.R.; Brook, A.; Vollmer, C.M.; Kent, T.S.; Sanchez, N.; Pedrosa, I. Structured reporting of multiphasic CT for pancreatic cancer: Potential effect on staging and surgical planning. RSNA Radiol. 2015, 274, 464–472. [Google Scholar] [CrossRef] [PubMed]
- Hoang, J.K.; Middleton, W.D.; Farjat, A.E.; Langer, J.E.; Reading, C.C.; Teefey, S.A. Reduction in thyroid nodule biopsies and improved accuracy with American college of radiology thyroid imaging reporting and data system. RSNA Radiol. 2018, 287, 185–193. [Google Scholar] [CrossRef] [PubMed]
- Balthazar, P.; Konstantopoulos, C.; Wick, C.A.; DeSimone, A.K.; Tridandapani, S.; Simoneaux, S. Trainees may add value to patient care by decreasing addendum utilization in radiology reports. Am. J. Roentgenol. 2017, 209, 976–981. [Google Scholar] [CrossRef] [PubMed]
- Rosenkrantz, A.B.; Doshi, A.M. Public transparency web sites for radiology practices: Prevalence of price, clinical quality, and service quality information. Clin. Imaging 2016, 40, 531–534. [Google Scholar] [CrossRef] [PubMed]
- Patmon, F.L.; Gee, P.M.; Rylee, T.L.; Readdy, N.L. Using interactive patient engagement technology in clinical practice: A qualitative assessment of nurses’ perceptions. J. Med. Internet Res. 2016, 18, e298. [Google Scholar] [CrossRef]
- Giardina, T.D.; Modi, V.; Parrish, D.E.; Singh, H. The patient portal and abnormal test results: An exploratory study of patient experiences. Patient Experience J. 2015, 2, 148. [Google Scholar] [CrossRef]
- Cabarrus, M.; Naeger, D.M.; Rybkin, A.; Qayyum, A. Patients prefer results from the ordering provider and access to their radiology reports. J. Am. Coll. Radiol. 2015, 12, 556–562. [Google Scholar] [CrossRef]
- Fang, J.; Boos, J.; Cohen, M.P.; Kruskal, J.B.; Eisenberg, R.; Siewert, B. Radiologists’ experience with patient interactions in the era of open access of patients to radiology reports. J. Am. Coll. Radiol. 2018, 15, 1573–1579. [Google Scholar] [CrossRef]
- Sorondo, B.; Allen, A.; Bayleran, J.; Doore, S.; Fathima, S.; Sabbagh, I. Using a patient portal to transmit patient reported health information into the electronic record: Workflow implications and user experience. eGEMs 2016, 4, 1237. [Google Scholar] [CrossRef]
- Laccetti, A.L.; Chen, B.; Cai, J.; Gates, S.; Xie, Y.; Lee, S.J.C. Increase in cancer center staff effort related to electronic patient portal use. J. Oncol. Pract. 2016, 12, e981–e990. [Google Scholar] [CrossRef] [PubMed]
- Woollen, J.; Prey, J.; Wilcox, L.; Sackeim, A.; Restaino, S.; Raza, S.T. Patient experiences using an inpatient personal health record. Appl. Clin. Inform. 2016, 7, 446–460. [Google Scholar] [PubMed]
- Edwards, E.A.; Cote, A.; Phelps, A.S.; Naeger, D.M. Parents of pediatric radiology patients prefer timely reporting and discussing results with referring providers. Acad. Radiol. 2019, 27, 739–743. [Google Scholar] [CrossRef] [PubMed]
- Jung, H.-Y.; Gichoya, J.W.; Vest, J.R. Providers’ access of imaging versus only reports: A system log file analysis. J. Am. Coll. Radiol. 2017, 14, 217–223. [Google Scholar] [CrossRef] [PubMed]
- Zide, M.; Caswell, K.; Peterson, E.; Aberle, D.R.; Bui, A.A.; Arnold, C.W. Consumers’ patient portal preferences and health literacy: A survey using crowdsourcing. JMIR Res. Protoc. 2016, 5, e104. [Google Scholar] [CrossRef] [PubMed]
- Johnson, E.J.; Doshi, A.M.; Rosenkrantz, A.B. Strengths and deficiencies in the content of US radiology private practices’ websites. J. Am. Coll. Radiol. 2017, 14, 431–435. [Google Scholar] [CrossRef]
- Kelly, M.M.; Hoonakker, P.L.; Dean, S.M. Using an inpatient portal to engage families in pediatric hospital care. J. Am. Med. Inform. Assoc. 2017, 24, 153–161. [Google Scholar] [CrossRef]
- Wildenbos, G.A.; Maasri, K.; Jaspers, M.; Peute, L. Older adults using a patient portal: Registration and experiences, one year after implementation. Digit. Health 2018, 4, 2055207618797883. [Google Scholar] [CrossRef]
- Alper, D.P.; Shinagare, A.B.; Hashemi, S.R.; Glazer, D.I.; DiPiro, P.J.; Boland, G.W. Effect of a report template-enabled quality improvement initiative on use of preferred phrases for communicating normal findings in structured abdominal CT and MRI reports. Am. J. Roentgenol. 2020, 214, 835–842. [Google Scholar] [CrossRef]
- Mishra, V.K.; Hoyt, R.E.; Wolver, S.E.; Yoshihashi, A.; Banas, C. Qualitative and quantitative analysis of patients’ perceptions of the patient portal experience with OpenNotes. Appl. Clin. Inform. 2019, 10, 10–18. [Google Scholar] [CrossRef]
- O’Leary, K.J.; Sharma, R.K.; Killarney, A.; O’Hara, L.S.; Lohman, M.E.; Culver, E. Patients’ and healthcare providers’ perceptions of a mobile portal application for hospitalized patients. BMC Med. Inform. Decis. 2016, 16, 123. [Google Scholar] [CrossRef] [PubMed]
- Johnson, A.J.; Frankel, R.M.; Williams, L.S.; Glover, S.; Easterling, D. Patient access to radiology reports: What do physicians think? J. Am. Coll. Radiol. 2010, 7, 281–289. [Google Scholar] [CrossRef] [PubMed]
- Maddock, C.; Lewis, I.; Ahmad, K.; Sullivan, R. Online information needs of cancer patients and their organizations. Ecancermedicalscience 2011, 5, 1–22. [Google Scholar]
- Gephart, S.; Effken, J.; Staggers, N.; Sackett, K.; Hamid, F.; Cline, T. Using health information technology to engage patients in their care. OJNI 2013, 17, 9. [Google Scholar]
- Wells, S.; Rozenblum, R.; Park, A.; Dunn, M.; Bates, D. Personal health records for patients with chronic disease: A major opportunity. Appl. Clin. Inform. 2014, 5, 416–429. [Google Scholar] [PubMed]
- Laurance, J.; Henderson, S.; Howitt, P.J.; Matar, M.; Al Kuwari, H.; Edgman, L.S.; Darzi, A. Patient engagement: Four case studies that highlight the potential for improved health outcomes and reduced costs. Health Aff. 2014, 33, 1627–1634. [Google Scholar] [CrossRef]
- Chu, S.K.W.; Huang, H.; Wong, W.N.M.; van Ginneken, W.F.; Wu, K.M.; Hung, M.Y. Quality and clarity of health information on Q&A sites. Libr. Inf. Sci. Res. 2018, 40, 237–244. [Google Scholar]
- Giacco, D.; Mavromara, L.; Gamblen, J.; Conneely, M.; Priebe, S. Shared decision-making with involuntary hospital patients: A qualitative study of barriers and facilitators. BJPsych Open 2018, 4, 113–118. [Google Scholar] [CrossRef]
- Gunderson, J.; Choi-Kain, L.W. Working with patients who self-injure. JAMA Psychiatry 2019, 76, 976–977. [Google Scholar] [CrossRef]
- Bai, R.; Wang, X.; Su, Q. The impact of healthcare information technology on quality and safety of healthcare: A literature review. In Proceedings of the 12th ICSSSM, Guangzhou, China, 22 June 2015. [Google Scholar]
- Hugman, B. Healthcare Communication; Pharmaceutical Press: London, UK, 2009. [Google Scholar]
- Holman, G.T.; Waldren, S.E.; Beasley, J.W.; Cohen, D.J.; Dardick, L.D.; Fox, C.H. Meaningful use’s benefits and burdens for US family physicians. J. Am. Med. Inform. Assoc. 2018, 25, 694–701. [Google Scholar] [CrossRef]
- Devine, T.; Broderick, J.; Harris, L.M.; Wu, H.; Hilfiker, S.W. Making quality health websites a national public health priority: Toward quality standards. J. Med. Internet Res. 2016, 18, e211. [Google Scholar] [CrossRef]
- Peixoto, H.; Domingues, A.; Fernandes, B. Applying Business Intelligence to Clinical and Healthcare Organizations, 1st ed.; IGI Global: Hershey, PA, USA, 2016; pp. 1–23. [Google Scholar]
- Pereira, M.C.A.; Rebehy, P.C.P.W.; Faleiros, F.; Galvao, M.C.B. Handbook of Research on Entrepreneurship and Marketing for Global Reach in the Digital Economy, 1st ed.; IGI Global: Hershey, PA, USA, 2019; pp. 522–537. [Google Scholar]
- Keselman, A.; Logan, R.; Smith, C.A.; Leroy, G.; Zeng-Treitler, Q. Developing informatics tools and strategies for consumer-centered health communication. J. Am. Med. Inform. Assoc. 2008, 15, 473–483. [Google Scholar] [CrossRef]
- Bernstein, M.L.; McCreless, T.; Cote, M.J. Five constants of information technology adoption in healthcare. Hosp. Top. 2007, 85, 17–25. [Google Scholar] [CrossRef] [PubMed]
- Goldzweig, C.L.; Orshansky, G.; Paige, N.M.; Towfigh, A.A.; Haggstrom, D.A.; Miake-Lye, I.; Beroes, J.M.; Shekelle, P.G. Electronic patient portals: Evidence on health outcomes, satisfaction, efficiency, and attitudesa systematic review. Ann. Intern. Med. 2013, 159, 677–687. [Google Scholar] [CrossRef]
- Ramya, A.T.; Khatheeja, S.; Das, M.N.; Sanaboyina, A. Evaluation of benefits and barriers of Electronic Health Records [EHR] with their solutions: A study in multispeciality hospitals. Ann. Glob. Health 2018, 5, 87–96. [Google Scholar] [CrossRef]
- Buntin, M.B.; Damberg, C.; Haviland, A.; Kapur, K.; Lurie, N.; McDevitt, R. Consumer-directed health care: Early evidence about effects on cost and quality. Health Aff. 2006, 25, w516–w530. [Google Scholar] [CrossRef] [PubMed]
- Anvari, M.V. Clinical Staff Communication, Medical Errors, and Patient Satisfaction: A Correlational and Comparative Study. Ph.D. Thesis, University of Phoenix, Phoenix, AZ, USA, 2018. Available online: https://search.proquest.com/openview/187b21a4235704dffed74c9f1522bed5/1?pq-origsite=gscholar&cbl=18750&diss=y (accessed on 1 April 2020).
- Fleming, M.M.; Liu, F.; Luo, J.; Zhang, Y.; Pei, K.Y. Predictors of 30 d readmission following percutaneous cholecystostomy. J. Surg. Res. 2019, 233, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Luder, H.R.; Frede, S.M.; Kirby, J.A.; Epplen, K.; Cavanaugh, T.; Martin-Boone, J.E. TransitionRx: Impact of community pharmacy postdischarge medication therapy management on hospital readmission rate. J. Am. Pharm. Assoc. 2015, 55, 246–254. [Google Scholar] [CrossRef]
- TGoCoRDiC. Managing patient dose in computed tomography. A report of the International Commission on Radiological Protection. Ann. ICRP 2000, 30, 7. [Google Scholar] [CrossRef]
- Nawfel, R.D.; Chan, K.H.; Wagenaar, D.J.; Judy, P.F. Evaluation of video gray-scale display. Med. Phys. 1992, 19, 561–567. [Google Scholar] [CrossRef]
- Fleury, A.; Vacher, M.; Glasson, H.; Serignat, J.F.; Noury, N. Data Fusion in Health Smart Home: Preliminary Individual Evaluation of Two Families of Sensors; ISG: Pisa, Italy, 2008; p. 135. [Google Scholar]
- Ps, S.K.; Dharun, V. A study of MRI segmentation methods in automatic brain tumor detection. IJET 2016, 8, 2319–8613. [Google Scholar]
- Reiner, B.I.; Siegel, E.L.; Hooper, F.J.; Pomerantz, S.; Dahlke, A.; Rallis, D. Radiologists’ productivity in the interpretation of CT scans: A comparison of PACS with conventional film. Am. J. Roentgenol. 2001, 176, 861–864. [Google Scholar] [CrossRef]
- Hart, J.; McBride, A.; Blunt, D.; Gishen, P.; Strickland, N. Immediate and sustained benefits of a “total” implementation of speech recognition reporting. Br. J. Radiol. 2014, 83, 424–427. [Google Scholar] [CrossRef]

| Citation | Goal / Purpose | Based on Specific Patient Portal y/n | Study Design | Number of Participants | Types of Participants (Patients / Doctors/ Others) | Finding |
|---|---|---|---|---|---|---|
| Cook TS, et al. 2017 [8] | Impacts the annotations in the radiology reports that included patient-oriented definitions, anatomic illustrations, and hyperlinks to improve patient understanding. | No | Survey | 185 | Patients | Increased the understanding. |
| Miles RC, et al. 2016 [2] | To evaluate the frequency with which patients viewed their online radiology reports in relation to in a clinic or laboratory. | Yes | Survey | 129,419 | Patients | More than half of patients with access to online radiology reports viewed them, with higher viewing rates associated with viewing other types of reports. |
| Garry K, et al. 2020 [9] | Comparative study of patient satisfaction and understanding of radiology results when received through an electronic patient portal versus direct communication from providers. | No | Survey | 1005 | Patients | Patients’ understanding of their radiology reports were more through direct provider communication than those who first received their results through the patient portal (26.7% versus 47.8%; p < 0.001). |
| Cho JK, et al. 2020 [10] | To explore patient understanding of the radiology report by using five radiology reporting templates and radiology colloquialisms. | No | Survey | 1369 | Patients | Adding patient summaries in the report can help increase their comprehension of radiology reports. |
| Mervak BM, et al. 2016 [11] | To understand patient preferences in the radiology reports by analysis of patient-initiated messages submitted through a web-based electronic patient portal. | Yes | Survey | 1489 | Patients | Analysis of patient-initiated messages submitted through a patient portal helped to understand the patients’ concerns. |
| Broman KK, et al. 2015 [12] | To evaluate surgeon and patient acceptance of online postoperative care after general surgical operations. | yes | Survey | 50 | Patients, Doctors | In general, online postoperative visits were accepted by surgeons and patients. |
| Rosenkrantz AB, et al. 2017 [13] | Comparing the radiologists, referring physician, and patient interpretations of radiology reports to describe findings of likely low clinical significance. | Yes | Survey | 123 | Patients, Doctors | Ambiguity in radiologists’ language for incidental low-risk findings may contribute to increased patient anxiety and follow-up testing, warranting greater radiologist attention, and potentially new practice or reporting strategies. |
| Gunn AJ, et al. 2017 [14] | Providing actual radiology reports to the patients to evaluate their understanding | Yes | Survey | 104 | Patients | Medical terminologies and longer reports tend to be less well understood. |
| Martin-Carreras T, et al. 2019 [15] | This study looks to assess the readability of radiology reports. | Yes | Data analysis | 108,228 | Reports | Only 4% of all reports were readable at the 8th-grade level, which is the reading level of the average US adult. |
| Vitzthum von Eckstaedt, et al. 2020 [16] | Using the feedback of the patient advisory groups to design a new radiology report for lung cancer. | No | Survey | n/a | Patients | The new report has the potential to serve as a bridge between radiologists and patients, allowing for better patient understanding. |
| Henshaw D, et al. 2015 [1] | The feasibility of releasing reports to patients before the doctor’s appointment. | No | Survey | 508 | Patients | Releasing reports to patients was useful before the doctor’s appointment. |
| Oh SC, et al. 2016 [17] | Will the Prototype System for Patient-Oriented Radiology Reporting (PORTER) improve patients’ understanding of and satisfaction with radiology reports? | No | Survey | 300 | Reports | PORTER improves patients’ understanding of and satisfaction with radiology reports. |
| Reicher JJ, et al. 2016 [18] | The impact of the usage of Meaningful Use-compliant electronic heath record (EHR) technology and direct messaging in radiology practice. | Yes | Data analysis | 752,496 | Messages | It improved radiologist–patient communication. |
| Short RG, et al. 2017 [19] | Comparing the results of using online crowdsourcing to assess the effectiveness of a Web-Based Interactive radiology report. | No | Survey | 193 | Patients | Report understanding scores were significantly higher for the interactive web-based than the standard report group (p < 0.05) |
| Martin-Carreras T, et al. 2018 [20] | Comparing MedlinePlus, RadLex, and the PORTER (Patient-Oriented Radiology Reporter) lay-language radiology glossary for the readability of their definitions and coverage of radiology reports. | Yes | Data analysis | 10,000 | Reports | The readability in PORTER’s glossary definitions was higher than the others. |
| Qenam B, et al. 2017 [21] | Text Simplification by using Consumer Health Vocabulary can help to increase the readability of the radiology report. | No | Data analysis | 792 | Reports | The CHV covered a high number of concepts found in the reports but unmapped concepts are associated with locations that are commonly found in radiology reporting |
| McNamara M, et al. 2015 [7] | To know if the patients prefer to have access to their radiology images or notes. | Yes | Survey | 41 | Patients | The study found that patients prefer to have access to both their radiology images and notes. |
| Sadigh G, et al. 2015 [22] | Doctor’s opinion regarding Traditional Text-Only Versus Multimedia-Enhanced Radiology Reporting. | Yes | Survey | 402 | Doctors | Doctors were satisfied with the format of their current text-only radiology reports and believed that MERR would represent an improvement. |
| Dy GW, et al. 2018 [23] | To evaluate a patient-centered radiology report (PCRR) for renal ultrasounds in children with hydronephrosis. | Yes | Survey | 44 | Patients | The patients showed high confidence in the PCRR. |
| Lye CT, et al. 2019 [24] | To evaluate U.S. hospital compliance with government guidelines and patient straightforward entry to imaging studies. | No | Survey | 81 | Hospitals | All 80 hospitals provided imaging studies on CDs. Only 8% of hospitals by email and three (4%) via an online patient portal. |
| Pahade JK, et al. 2018 [25] | To know what information patients or caregivers found useful before an imaging examination. | No | Survey | 1542 | Patients | Delivery of pre-examination information for imaging examinations is suboptimal, with half of the patients and caregivers seeking information on their own. |
| Short RG, et al. 2018 [26] | To determine the readability of language used in chest Computer Tomography reports to explain a “normal” thyroid gland. | Yes | Data analysis | 11,357 | Chest CT (reports) | The language used by radiologists to explain a normal thyroid gland in chest Computer Tomography reports is complex and variable. |
| Yi PH, et al. 2019 [27] | To evaluate the readability of the lumbar spine in the MRI reports. | Yes | Data analysis | 110 | Lumbar spine (reports) | The study found that the lumbar spine in the MRI reports are written at a level too high for the average person to comprehend. |
| Kemp JL, et al. 2017 [28] | The opinion of radiologists regarding direct communication with their patients. | No | Survey | 694 | Doctors | 89% agreed that they should have direct communication with their patients. |
| Alpert JM, et al. 2018 [29] | To evaluate the current content of oncology in the patient portal. | No | Semi-structured interviews | 60 | Patients, Doctors | Most of the participants were relatively comfortable with this manner of disclosure but still preferred direct communication. |
| Mityul MI, et al. 2018 [30] | To know how patients and radiologists understand the commonly used phrases within the radiology report. | No | Survey | 113 | Patients, Doctors | There is a huge difference between patients and doctors in terms of understanding the medical terms in the radiologic report. |
| Choudhry A, et al. 2015 [31] | To evaluate the current content of the Biopsy Result in the patient portal. | Yes | Survey | 301 | Patients | Most of the patients preferred to have direct communication with their doctors by telephone. |
| Brook OR, et al. 2015 [32] | To compare structured radiology reports versus nanostructured reporting and the effects of both reports on subjective assessment of resectability. | No | Survey | 120 | Reports | Surgeons were more confident in regards to the structured radiology reports. |
| Hoang JK, et al. 2018 [33] | The affective of applying American College of Radiology Thyroid Imaging Reporting and Data System (ACR TI-RADS) criteria in the number of thyroid nodules recommended for biopsy. | Yes | Survey | 100 | Thyroid nodules (reports) | ACR TI-RADS criteria decreased the number of thyroid nodules recommended for biopsy. |
| Balthazar P, et al. 2017 [34] | To study the impact of trainee involvement and any factors on addendum rates in radiologic reports. | Yes | Data analysis | 129,033 | Reports | Trainees helped to decrease the addendum rates in radiology report. |
| Rosenkrantz AB, et al. 2016 [35] | To evaluate information about radiology practices on public transparency Web sites. | Yes | Data analysis | 8 | Web sites | Transparency Web sites had a lesser extent of service quality and information. |
| Patmon FL, et al. 2016 [36] | To evaluate using interactive patient engagement technologies (iPET) by nurses. | Yes | Survey | 38 | Nurses | Nurses who received sufficient training on the iPET system were more comfortable with iPET. |
| Giardina TD, et al. 2015 [37] | Opinions of patients who have chronic diseases regarding their results in the patient portal. | Yes | Interview | 13 | Patients | They have several concerns that affected their experience. |
| Cabarrus M, et al. 2015 [38] | To know patients’ preferences for receiving their radiologic report results. | Yes | Survey | 617 | Patients | 64% of patients want to have copy of their results or online access. |
| Fang J, et al. 2018 [39] | To know doctor’s experiences with patient interactions in the era of open access of patients to imaging reports. | Yes | Survey | 128 | Staff and trainee doctors | Most of the respondents found interactions with patients to be a satisfying experience. |
| Sorondo B, et al. 2016 [40] | To evaluate the patient self-reported screening tool in a patient portal and user experience in primary care. | Yes | Survey | 72 | Patients | Patients can effectively use their portals to complete the patient report. |
| Laccetti AL, et al. 2016 [41] | To examine patterns of use of patient portals by clinic employees at a National Cancer Institute-designated comprehensive cancer center. | Yes | Data analysis | 289 | Nurses, Ancillary staff, Clerical/managerial staff, Doctors, Advanced practice providers | All the staff efforts that related to a patient portal has improved markedly over time, especially among nursing staff. |
| Woollen J, et al. 2016 [42] | To investigate patient experience with browsing their laboratory test results and radiology reports on a tablet or computer from the patient portal. | Yes | Semi-structured interviews | 14 | Patients | Providing a tablet computer may enhance satisfaction, lower anxiety, and increase understanding of their health conditions. |
| Edwards EA, et al. 2019 [43] | To know parent preferences for pediatric radiology patients. | Yes | Survey | n/a | Parents | The majority of parents prefer to receive the radiology report from a radiologist in-person. |
| Jung HY, et al. 2017 [44] | This article examined differences in access to text-only reports compared with radiology images through a health information exchange system by health care professionals. | Yes | Data analysis | 1670 | Doctors and non-doctors | Radiologists, orthopedists, pulmonary disease specialists, and surgeons accessed imaging more often than text-based reports only. |
| Zide M, et al. 2016 [45] | The effect of patient health literacy in radiology on perceived portal usability. | No | Survey | 500 | Patients | Those who have more medical conditions have a greater preference for patient portals. |
| Johnson EJ, et al. 2017 [46] | To evaluate the content of the private practice radiology facilities in the USA. | Yes | Survey | 50 | Private practice radiology facility | The quality of the content was low. |
| Kelly MM, et al. 2017 [47] | To know the parent’s opinion of using the inpatient portal application on a tablet computer that presents information about a child’s hospital stay. | Yes | Survey | 296 | Parents | In general, parents were satisfied with the inpatient portal. |
| Wildenbos GA, et al. 2018 [48] | To know the opinion of the older adult patients using a patient portal. | No | Survey | 10,679 | Older adult patients | The majority indicated that they prefer to review their medical information and appointments by the portal. |
| Alper DP, et al. 2020 [49] | To assess the impact of a reports template quality improvement (QI) initiative on the use of preferred phrases for connecting normal findings in structured abdominal CT and MRI reports. | Yes | Data analysis | 44,680 | Radiology reports | A QI intervention decreased the use of equivocal terms and increased the use of preferred phrases when connecting normal findings in abdominal MRI and CT reports. |
| Mishra VK, et al. 2019 [50] | To analyze the patient’s perceptions after being given access to specialist’s notes and primary care via the patient portal. | No | Survey | 6439 | Patients | The study confirms that the patients who have access to their specialists’ online medical records and primary care perceived benefits of OpenNotes. |
| O’Leary KJ, et al. 2016 [51] | To evaluate health care provider and patient perceptions of a patient portal and identify opportunities to enhance the current design. | Yes | Semi-structured interviews | 18 | Patients | Optimizing the patient portal will require attention to the format of information provided, including type and timing. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alarifi, M.; Patrick, T.; Jabour, A.; Wu, M.; Luo, J. Full Radiology Report through Patient Web Portal: A Literature Review. Int. J. Environ. Res. Public Health 2020, 17, 3673. https://doi.org/10.3390/ijerph17103673
Alarifi M, Patrick T, Jabour A, Wu M, Luo J. Full Radiology Report through Patient Web Portal: A Literature Review. International Journal of Environmental Research and Public Health. 2020; 17(10):3673. https://doi.org/10.3390/ijerph17103673
Chicago/Turabian StyleAlarifi, Mohammad, Timothy Patrick, Abdulrahman Jabour, Min Wu, and Jake Luo. 2020. "Full Radiology Report through Patient Web Portal: A Literature Review" International Journal of Environmental Research and Public Health 17, no. 10: 3673. https://doi.org/10.3390/ijerph17103673
APA StyleAlarifi, M., Patrick, T., Jabour, A., Wu, M., & Luo, J. (2020). Full Radiology Report through Patient Web Portal: A Literature Review. International Journal of Environmental Research and Public Health, 17(10), 3673. https://doi.org/10.3390/ijerph17103673






