A Literature Review on the Foundations and Potentials of Digital Teaching Scenarios for Interprofessional Health Care Education
Abstract
1. Introduction
2. Current Challenges
2.1. Specialization and Interprofessional Collaboration
2.2. Interprofessional Education
- (1)
- Values and ethics. Values and ethics are part of the professional identity of both practitioners and learners. Older approaches to professional identity have been criticized for being selfish and thus tending to create barriers between professions, which is seen as an obstacle to improving health care [29]. Therefore, new patient-oriented and society-centered values are proposed, based on the common goal of improving health care overall. The associated professional ethics thus reflect the shared commitment of different professions to creating safer, more efficient and effective health care systems. This is accompanied by a consistent demonstration of mutual trust and respect in the communication among various professionals [30], whose establishment we already consider to be particularly important for training health care professionals.
- (2)
- Awareness of profession-specific roles, competences, and responsibilities. The roles and responsibilities of the individual professions are defined by legal requirements, but this can vary depending on the specific care situation. Therefore, a concrete understanding of the boundaries of expertise between the professions and knowledge of competences of the professions is crucial and should be practiced and refined in continuous interprofessional education as well as in practice [31,32].
- (3)
- Ability for interprofessional communication. A study by Suter et al. identified the ability of interprofessional communication as a core aspect of interprofessional collaboration [33]. This often faces the challenge that different professions often use different terms, thus preventing effective interprofessional care. In order to guarantee this care, the aim of interprofessional education should be to establish a common interprofessional language, which is trained through appropriate training and practice opportunities.
- (4)
- Ability for interprofessional teamwork. Wherever members of different health care professions work together to achieve common goals for the care of patients, they must demonstrate teamwork skills. Accordingly, they must learn to bring their own expertise into a complex system that achieves better results through individual contributions. Focusing on patient care and dealing openly and constructively with conflicts within the team through effective interprofessional communication and joint problem solving strengthens the ability to work together and form a more effective team.
3. Didactical Approaches
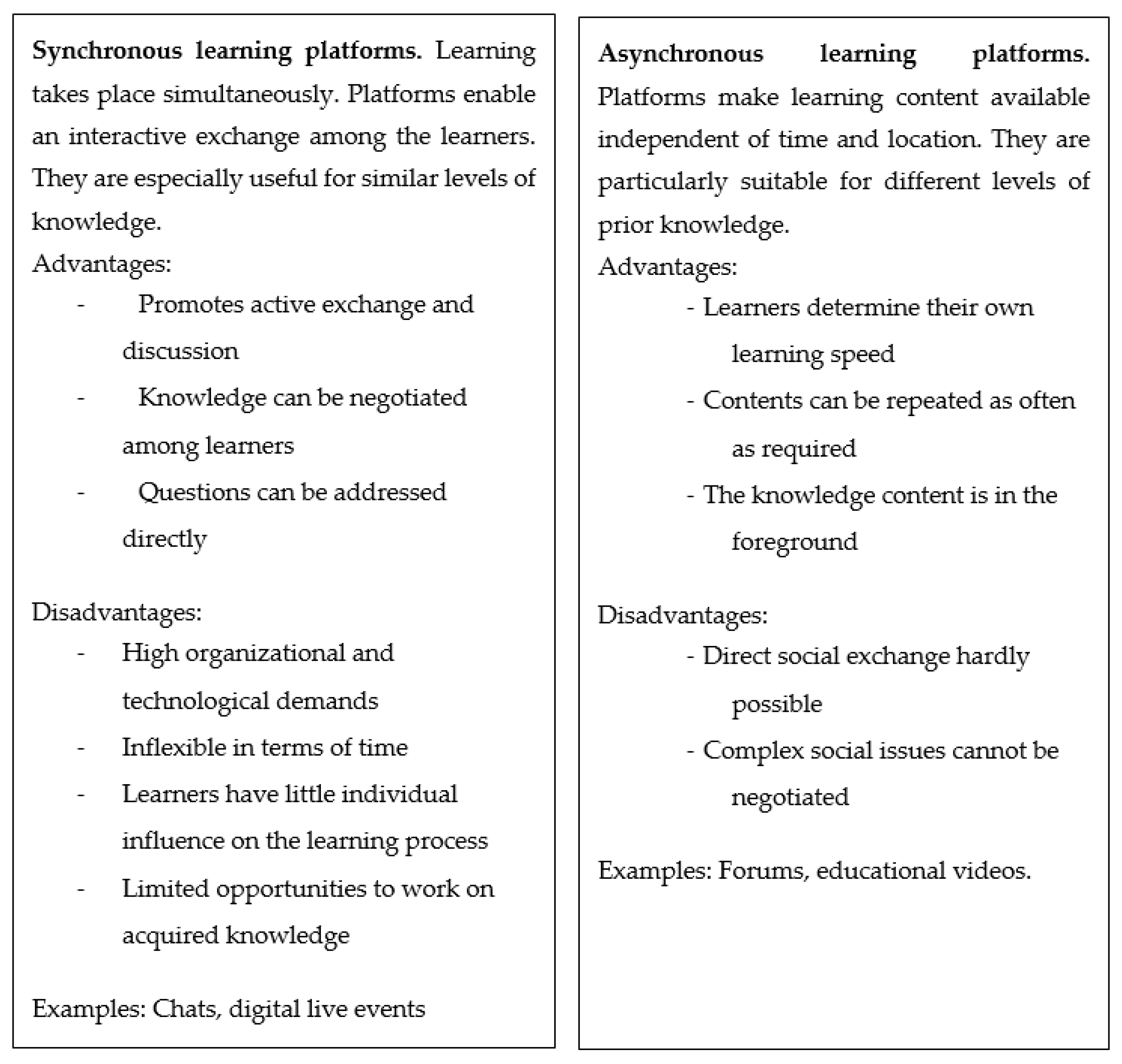
3.1. Digital Interprofessional Teaching: The Application of Learning Platforms
3.2. Digital Interprofessional Teaching: The Application of Videos
4. Conclusions
5. Outlook
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Walton, H.J. World federation for medical education: Proceedings of the world summit on medical education. Med. Educ. 1993, 28, 140–149. [Google Scholar]
- World Health Organization. Learning together to work together for health. In Proceedings of the Report of a WHO Study Group on Multiprofessional Education of Health Personnel: The Team Approach, Geneva, Switzerland, 12–16 October 1987. [Google Scholar]
- Wakefield, A.; Carlisle, C.; Hall, A.; Attree, M. Patient safety investigations: The need for interprofessional learning. Learn. Health Soc. Care 2008, 8, 22–32. [Google Scholar] [CrossRef]
- Larsen, A.; Broberger, E.; Petersson, P. Complex caring needs without simple solutions: The experience of interprofessional collaboration among staff caring for older persons with multimorbidity at home care settings. Scand. J. Caring Sci. 2016, 31, 342–350. [Google Scholar] [CrossRef]
- Rämgård, M.; Blomqvist, K.; Petersson, P. Developing health and social care planning in collaboration. J. Interprof. Care 2015, 29, 354–358. [Google Scholar] [CrossRef]
- Budrionis, A.; Bellika, J.G. The Learning Healthcare System: Where are we now? A systematic review. J. Biomed. Inform. 2016, 64, 87–92. [Google Scholar] [CrossRef]
- Anderson, R.; McDaniel, R.R. Managing health care organizations: Where professionalism meets complexity science. Health Care Manag. Rev. 2000, 25, 83–92. [Google Scholar] [CrossRef]
- Plsek, P.E.; Greenhalgh, T. The challenge of complexity in health care. BMJ. Walton HJ. World federation for medical education: Proceedings of the world summit on medical education. Med. Educ. 1993, 28, 140–149. [Google Scholar]
- Wauben, L.S.G.L.; Dekker-van Doorn, C.M.; van Wijngaarden, J.D.H.; Goossens, R.H.M.; Huijsman, R.; Klein, J.; Lange, J.F. Discrepant perceptions of communication, teamwork and situation awareness among surgical team members. Int. J. Qual Health Care 2011, 23, 159–166. [Google Scholar] [CrossRef] [PubMed]
- O’Leary, K.J.; Ritter, C.D.; Wheeler, H.; Szekendi, M.K.; Brinton, T.S.; Williams, M.V. Teamwork on inpatient medical units: Assessing attitudes and barriers. Qual. Saf. Health Care 2008, 19, 117–121. [Google Scholar] [CrossRef] [PubMed]
- Gehring, K.; Schwappach, D.L.B.; Battaglia, M.; Buff, R.; Huber, F.; Sauter, P.; Wieser, M. Safety climate and its association with office type and team involvement in primary care. Int. J. Qual. Health Care 2013, 25, 396–402. [Google Scholar] [CrossRef] [PubMed]
- Tajfel, H. Social psychology of intergroup relations. Annu. Rev. Psychol. 1982, 33, 1–39. [Google Scholar] [CrossRef]
- Weller, J.; Boyd, M.; Cumin, D. Teams, tribes and patient safety: Overcoming barriers to effective teamwork in healthcare. Postgrad. Med. J. 2014, 90, 149–154. [Google Scholar] [CrossRef]
- Hean, S.; Clark, J.M.; Adams, K.; Humphris, D. Will opposites attract? Similarities and differences in students’ perceptions of the stereotype profiles of other health and social care professional groups. J. Interprof. Care 2006, 20, 162–181. [Google Scholar] [CrossRef] [PubMed]
- Scott, S.D.; Pollock, C. The role of nursing unit culture in shaping research utilization behaviors. Res. Nurs. Health 2008, 31, 298–309. [Google Scholar] [CrossRef] [PubMed]
- Braithwaite, J.; Clay-Williams, R.; Vecellio, E.; Marks, D.; Hooper, T.; Westbrook, M.; I Westbrook, J.; Blakely, B.; Ludlow, K. The basis of clinical tribalism, hierarchy and stereotyping: A laboratory-controlled teamwork experiment. BMJ Open 2016, 6. [Google Scholar] [CrossRef] [PubMed]
- Braithwaite, J.; Westbrook, M. Rethinking clinical organisational structures: An attitude survey of doctors, nurses and allied health staff in clinical directorates. J. Health Serv. Res. Policy 2005, 10, 10–17. [Google Scholar] [CrossRef]
- Jakobsen, F. An overview of pedagogy and organisation in clinical interprofessional training units in Sweden and Denmark. J. Interprof. Care 2016, 30, 156–164. [Google Scholar] [CrossRef]
- Wilhelmsson, M.; Pelling, S.; Ludvigsson, J.; Hammar, M.; Dahlgren, L.-O.; Faresjö, T. Twenty years experiences of interprofessional education in Linköping—Ground-breaking and sustainable. J. Interprof. Care 2009, 23, 121–133. [Google Scholar] [CrossRef]
- Barr, H.; Freeth, D.; Hammick, M.; Koppel, I.; Reeves, S. The evidence base and recommendations for interprofessional education in health and social care. J. Interprof. Care 2006, 20, 75–78. [Google Scholar] [CrossRef]
- Hammick, M.; Freeth, D.; Koppel, I.; Reeves, S.; Barr, H. A best evidence systematic review of interprofessional education: BEME Guide no. 9. Med. Teach. 2007, 29, 735–751. [Google Scholar] [CrossRef]
- Wissenschaftsrat, D. Empfehlungen zur Weiterentwicklung des Medizinstudiums in Deutschland auf Grundlage einer Bestandsaufnahme der humanmedizinischen Modellstudiengänge; Wissenschaftsrat Dresden: Dresden, Germany, 2014. [Google Scholar]
- Walkenhorst, U.; Mahler, C.; Aistleithner, R.; Hahn, E.G.; Kaap-Fröhlich, S.; Karstens, S.; Reiber, K.; Stock-Schröer, B.; Sottas, B. Positionspapier GMA-Ausschuss–Interprofessionelle Ausbildung in den Gesundheitsberufen. GMS Z. Med. Ausbild. 2015, 32, 95424–95442. [Google Scholar]
- Rudland, J.R.; Mires, G.J. Characteristics of doctors and nurses as perceived by students entering medical school: Implications for shared teaching. Med. Educ. 2005, 39, 448–455. [Google Scholar] [CrossRef] [PubMed]
- Ponzer, S.; Hylin, U.; Kusoffsky, A.; Lauffs, M.; Lonka, K.; Mattiasson, A.-C.; Nordstrom, G. Interprofessional training in the context of clinical practice: Goals and students’ perceptions on clinical education wards. Med. Educ. 2004, 38, 727–736. [Google Scholar] [CrossRef]
- Kayingo, G.; Hass, V.M. The Health Professions Educator: A Practical Guide for New and Established Faculty; Springer Publishing Company: Berlin/Heidelberg, Germany, 2017. [Google Scholar]
- Ateah, C.A.; Snow, W.; Wener, P.; Macdonald, L.; Metge, C.; Davis, P.; Fricke, M.; Ludwig, S.; Anderson, J. Stereotyping as a barrier to collaboration: Does interprofessional education make a difference? Nurse Educ. Today 2011, 31, 208–213. [Google Scholar] [CrossRef]
- Interprofessional Education Collaborative Expert Panel. Core Competencies for Interprofessional Collaborative Practice: Report of an Expert Panel. Acad. Med. 2011, 86, 1351. [Google Scholar] [CrossRef]
- McNair, R. The case for educating health care students in professionalism as the core content of interprofessional education. Med. Educ. 2005, 39, 456–464. [Google Scholar] [CrossRef]
- Way, D.; Jones, L.; Baskerville, B.; Busing, N. Primary health care services provided by nurse practitioners and family physicians in shared practice. CMAJ 2001, 165, 1210–1214. [Google Scholar]
- Edwards, A. Building common knowledge at the boundaries between professional practices: Relational agency and relational expertise in systems of distributed expertise. Int. J. Educ. Res. 2011, 50, 33–39. [Google Scholar] [CrossRef]
- Jakobsen, F.; Hansen, T.B.; Eika, B. Knowing more about the other professions clarified my own profession. J. Interprof. Care 2011, 25, 441–446. [Google Scholar] [CrossRef]
- Suter, E.; Arndt, J.; Arthur, N.; Parboosingh, J.; Taylor, E.; Deutschlander, S. Role understanding and effective communication as core competencies for collaborative practice. J. Interprof. Care 2009, 23, 41–51. [Google Scholar] [CrossRef]
- Quintero, G.A. Medical education and the healthcare system—Why does the curriculum need to be reformed? BMC Med. 2014, 12, 213. [Google Scholar] [CrossRef] [PubMed]
- Kopelman, P. The future of UK medical education curriculum—What type of medical graduates do we need? Future Hosp. J. 2014, 1, 41. [Google Scholar] [CrossRef] [PubMed]
- Guraya, S.Y.; Barr, H. The effectiveness of interprofessional education in healthcare: A systematic review and meta-analysis. Kaohsiung J. Med. Sci. 2018, 34, 160–165. [Google Scholar] [CrossRef] [PubMed]
- Karim, R.; Ross, C. Interprofessional education (IPE) and chiropractic. J. Can. Chiropr. Assoc. 2008, 54, 76–78. [Google Scholar]
- Reeves, S.; Pelone, F.; Harrison, R.; Goldman, J.; Zwarenstein, M. Interprofessional collaboration to improve professional practice and healthcare outcomes. Cochrane Database Syst. Rev. 2017, 2017, CD000072. [Google Scholar] [CrossRef]
- Dombrowski, T.; Dazert, S.; Volkenstein, S. Digitale Strategien in der Lehre. Laryngo Rhino Otol. 2019, 98, S197–S219. [Google Scholar] [CrossRef]
- Kimmerle, J.; Moskaliuk, J.; Oeberst, A.; Cress, U. Learning and Collective Knowledge Construction With Social Media: A Process-Oriented Perspective. Educ. Psychol. 2015, 50, 120–137. [Google Scholar] [CrossRef]
- Cress, U.; Kimmerle, J. Collective Knowledge Construction. In International Handbook of the Learning Sciences; Routledge: New York, NY, USA, 2018; pp. 137–146. [Google Scholar]
- Holtz, P.; Kimmerle, J.; Cress, U. Using big data techniques for measuring productive friction in mass collaboration online environments. Int. J. Comput. Collab. Learn. 2018, 13, 439–456. [Google Scholar] [CrossRef]
- Kimmerle, J.; Fischer, F.; Cress, U. Argumentation and knowledge construction. In International Handbook of Computer-Supported Collaborative Learning; Cress, U., Rosé, W.A., Oshima, J., Eds.; Springer International Publishing: Cham, Switzerland, in press.
- Lofters, A.K.; Slater, M.; Angl, E.N.; Leung, F.-H. Facebook as a tool for communication, collaboration, and informal knowledge exchange among members of a multisite family health team. J. Multidiscip. Health 2016, 9, 29–34. [Google Scholar] [CrossRef]
- Cress, U.; Kimmerle, J. The interrelations of individual learning and collective knowledge construction: A cognitive-systemic framework. In The Psychology of Digital Learning; Springer: Berlin/Heidelberg, Germany, 2017; pp. 123–145. [Google Scholar]
- Pander, T.; Pinilla, S.; Dimitriadis, K.; Fischer, M.R. The use of Facebook in medical education—A literature review. GMS Z. Med. Ausbild. 2014, 31. [Google Scholar]
- Curran, V.; Matthews, L.; Fleet, L.; Simmons, K.; Gustafson, D.L.; Wetsch, L. A Review of Digital, Social, and Mobile Technologies in Health Professional Education. J. Contin. Educ. Health Prof. 2017, 37, 195–206. [Google Scholar] [CrossRef] [PubMed]
- Vasset, F.; Brynhildsen, S.; Kvilhaugsvik, B. Interprofessional Learning through a Digital Platform. J. Res. Interprof. Pract. Educ. 2019, 9. [Google Scholar] [CrossRef]
- Cain, J.; Chretien, K. Exploring Social Media’s Potential in Interprofessional Education. J. Res. Interprof. Pract. Educ. 2013, 3. [Google Scholar] [CrossRef]
- Kimmerle, J.; Bientzle, M.; Cress, U. Learning communication skills for dealing with different perspectives: Technologies for health sciences education. In Educational Technologies in Medical and Health Sciences Education; Springer: Berlin/Heidelberg, Germany, 2016; pp. 139–157. [Google Scholar]
- Ouadoud, M.; Nejjari, A.; Chkouri, M.Y.; El-Kadiri, K.E. Learning Management System and the Underlying Learning Theories. Int. J. Inform. Sci. Technol. 2018, 2, 25–33. [Google Scholar] [CrossRef]
- Reynolds, R.; Hansen, P. Inter-disciplinary research on inquiry and learning: Information and learning sciences perspectives. In Proceedings of the 2018 Conference on Human Information Interaction & Retrieval, New Brunswick, NJ, USA, 11–15 March 2018; ACM: New York, NY, USA, 2018; pp. 289–292. [Google Scholar] [CrossRef]
- Bientzle, M.; Hircin, E.; Kimmerle, J.; Knipfer, C.; Smeets, R.; Gaudin, R.; Holtz, P.; De Leeuw, R.; Doarn, C. Association of Online Learning Behavior and Learning Outcomes for Medical Students: Large-Scale Usage Data Analysis. JMIR Med. Educ. 2019, 5, e13529. [Google Scholar] [CrossRef]
- Merkt, M.; Schwan, S. Lernen Mit Digitalen Medien aus Studierendenperspektive; Hochschulforum Digitalisierung: Berlin, Germany, 2016. [Google Scholar] [CrossRef]
- Jin, L.; Jeong, A. Learning achieved in structured online debates: Levels of learning and types of postings. Instr. Sci. 2013, 41, 1141–1152. [Google Scholar] [CrossRef]
- Waterston, R. Interaction in online interprofessional education case discussions. J. Interprof. Care 2011, 25, 272–279. [Google Scholar] [CrossRef]
- Ho, K.; Jarvis-Selinger, S.; Norman, C.D.; Li, L.C.; Olatunbosun, T.; Cressman, C.; Nguyen, A. Electronic communities of practice: Guidelines from a project. J. Contin. Educ. Health Prof. 2010, 30, 139–143. [Google Scholar] [CrossRef]
- Coleman, E.; O’Connor, E. The role of WhatsApp® in medical education; a scoping review and instructional design model. BMC Med. Educ. 2019, 19, 279. [Google Scholar] [CrossRef]
- Hean, S.; Craddock, D.; O’Halloran, C. Learning theories and interprofessional education: A user’s guide. Learn. Health Soc. Care 2009, 8, 250–262. [Google Scholar] [CrossRef]
- Hughes, M.; Ventura, S.; Dando, M. On-line interprofessional learning: Introducing constructivism through enquiry-based learning and peer review. J. Interprof. Care 2004, 18, 263–268. [Google Scholar] [CrossRef] [PubMed]
- Pedaste, M.; Mäeots, M.; Leijen, Ä.; Sarapuu, T. Improving Students’ Inquiry Skills through Reflection and Self-Regulation Scaffolds. Technol. Instr. Cogn. Learn. 2012, 9, 81–95. [Google Scholar]
- De Jong, T.; Van Joolingen, W.R. Scientific Discovery learning with computer simulations of conceptual domains. Rev. Educ. Res. 1998, 68, 179–201. [Google Scholar] [CrossRef]
- Pedaste, M.; Mäeots, M.; Siiman, L.A.; De Jong, T.; Van Riesen, S.A.; Kamp, E.T.; Manoli, C.C.; Zacharia, Z.; Tsourlidaki, E. Phases of inquiry-based learning: Definitions and the inquiry cycle. Educ. Res. Rev. Neth. 2015, 14, 47–61. [Google Scholar] [CrossRef]
- Kamin, A.-M. Anforderungen an interprofessionell Pflegende. In Beruflich Pflegende als Akteure in Digital Unterstützten Lernwelten; Springer: Berlin, Germany, 2013. [Google Scholar] [CrossRef]
- Evans, S.; Ward, C.; Reeves, S. Online interprofessional education facilitation: A scoping review. Med. Teach. 2018, 41, 215–222. [Google Scholar] [CrossRef]
- Ammenwerth, E.; Hackl, W.O.; Felderer, M.; Hörbst, A. Wie gelingt gemeinsames Lernen in asynchronen Lernumgebungen? Pflegezeitschrift 2017, 70, 38–42. [Google Scholar] [CrossRef]
- Cress, U.; Kimmerle, J. Successful knowledge building needs group awareness: Interaction analysis of a 9th grade CSCL Biology lesson. In Productive Multivocality in the Analysis of Group Interactions; Springer: Berlin/Heidelberg, Germany, 2013; pp. 495–509. [Google Scholar] [CrossRef]
- Cartwright, J.; Franklin, D.; Forman, D.; Freegard, H. Promoting collaborative dementia care via online interprofessional education. Australas. J. Ageing 2015, 34, 88–94. [Google Scholar] [CrossRef]
- Öztok, M.; Zingaro, D.; Brett, C.; Hewitt, J. Exploring asynchronous and synchronous tool use in online courses. Comput. Educ. 2013, 60, 87–94. [Google Scholar] [CrossRef]
- Hallin, K.; Kiessling, A.; Waldner, A.; Henriksson, P. Active interprofessional education in a patient based setting increases perceived collaborative and professional competence. Med. Teach. 2009, 31, 151–157. [Google Scholar] [CrossRef]
- Barnett, S.; Jones, S.C.; Bennett, S.; Iverson, D.; Bonney, A. General practice training and virtual communities of practice - a review of the literature. BMC Fam. Pract. 2012, 13, 87. [Google Scholar] [CrossRef]
- Volkers, N. Bridging the Professional Divide: Along with clear benefits, interprofessional collaboration can bring misunderstandings. Six bridge-builders share their strategies. ASHA Lead. 2016, 21, 40–50. [Google Scholar] [CrossRef]
- Gergerich, E.; Boland, D.; Scott, M.A. Hierarchies in interprofessional training. J. Interprof. Care 2019, 33, 528–535. [Google Scholar] [CrossRef] [PubMed]
- McLoughlin, C.; Patel, K.D.; O’Callaghan, T.; Reeves, S. The use of virtual communities of practice to improve interprofessional collaboration and education: Findings from an integrated review. J. Interprof. Care 2017, 32, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Van Es, E.A.; Tunney, J.; Goldsmith, L.T.; Seago, N. A framework for the facilitation of teachers’ analysis of video. J. Teach. Educ. 2014, 65, 340–356. [Google Scholar] [CrossRef]
- Custers, E.J.F.M.; Regehr, G.; McCulloch, W.; Peniston, C.; Reznick, R. The Effects of Modeling on Learning a Simple Surgical Procedure: See One, Do One or See Many, Do One? Adv. Health Sci. Educ. 1999, 4, 123–143. [Google Scholar] [CrossRef] [PubMed]
- Custers, E.J.F.M.; Regehr, G.; McCulloch, W.; Peniston, C.; Reznick, R. Enhancing technical skill learning through interleaved mixed-model observational practice. Adv. Health Sci. Educ. 1999, 4, 123–143. [Google Scholar] [CrossRef]
- Domuracki, K.; Wong, A.; Olivieri, L.; Grierson, L.E.M. The impacts of observing flawed and flawless demonstrations on clinical skill learning. Med. Educ. 2015, 49, 186–192. [Google Scholar] [CrossRef]
- Rapp, A.K.; Healy, M.G.; Charlton, M.E.; Keith, J.N.; Rosenbaum, M.E.; Kapadia, M.R. YouTube is the Most Frequently Used Educational Video Source for Surgical Preparation. J. Surg. Educ. 2016, 73, 1072–1076. [Google Scholar] [CrossRef]
- Mayer, R.E. Cognitive theory of multimedia learning. In The Cambridge Handbook of Multimedia Learning, 2nd ed.; Cambridge University Press (CUP): Cambridge, UK, 2014; pp. 43–71. [Google Scholar] [CrossRef]
- Baddeley, A. Working memory: Looking back and looking forward. Nat. Rev. Neurosci. 2003, 4, 829–839. [Google Scholar] [CrossRef]
- Großer, J.; Janczyk, M. The fate of previously focused working memory content: Decay or/and inhibition. Cogn. Process. 2014, 15, 41–42. [Google Scholar]
- Eggeling, M.; Bientzle, M.; Shiozawa, T.; Cress, U.; Kimmerle, J. The Impact of Visualization Format and Navigational Options on Laypeople’s Perception and Preference of Surgery Information Videos: Randomized Controlled Trial and Online Survey. J. Particip. Med. 2018, 10, e12338. [Google Scholar] [CrossRef]
- Bandura, A. Social Foundations of Thought and Action: A Social Cognitive Theory/Albert Bandura; Prentice-Hall: Englewood Cliffs, NJ, USA, 1986. [Google Scholar]
- Bandura, A. Social cognitive theory: An agentic perspective. Annu. Rev. Psychol. 2001, 52, 1–26. [Google Scholar] [CrossRef] [PubMed]
- Grosser, J.; Bientzle, M.; Shiozawa, T.; Hirt, B.; Kimmerle, J. Observing inter-professional videos: Impact of collaboration between physicians and psychologists on attitude and knowledge acquisition. 2020; Manuscript submitted for publication. [Google Scholar]
- Mahler, C.; Berger, S.; Pollard, K.; Krisam, J.; Karstens, S.; Szecsenyi, J.; Krug, K. Translation and psychometric properties of the German version of the University of the West of England Interprofessional Questionnaire (UWE-IP). J. Interprof. Care 2017, 31, 105–109. [Google Scholar] [CrossRef] [PubMed]
- Pollard, K.; Miers, M.E.; Gilchrist, M. Second year scepticism: Pre-qualifying health and social care students’ midpoint self-assessment, attitudes and perceptions concerning interprofessional learning and working. J. Interprof. Care 2005, 19, 251–268. [Google Scholar] [CrossRef]
- Jang, H.W.; Kim, K.-J. Use of online clinical videos for clinical skills training for medical students: Benefits and challenges. BMC Med. Educ. 2014, 14, 56. [Google Scholar] [CrossRef] [PubMed]
- Azer, S.A. Mechanisms in cardiovascular diseases: How useful are medical textbooks, eMedicine, and YouTube? Adv. Physiol. Educ. 2014, 38, 124–134. [Google Scholar] [CrossRef] [PubMed]
- Kardas, M.; O’Brien, E. Easier Seen Than Done: Merely Watching Others Perform Can Foster an Illusion of Skill Acquisition. Psychol. Sci. 2018, 29, 521–536. [Google Scholar] [CrossRef]
- Atkinson, R.K.; Derry, S.J.; Renkl, A.; Wortham, D. Learning from examples: Instructional principles from the worked examples research. Rev. Educ. Res. 2000, 70, 181–214. [Google Scholar] [CrossRef]
- Renkl, A. Toward an instructionally oriented theory of example-based learning. Cogn. Sci. 2014, 38, 1–37. [Google Scholar] [CrossRef]
- König, L. Podcasts in higher education: Teacher enthusiasm increases students’ excitement, interest, enjoyment, and learning motivation. Educ. Stud. 2020. [Google Scholar] [CrossRef]
- Cohen, L. Student Identification with a Profession. Educ. Res. 1969, 12, 41–45. [Google Scholar] [CrossRef]
- Selle, K.M.; Salamon, K.; Boarman, R.; Sauer, J. Providing interprofessional learning through interdisciplinary collaboration: The role of “modelling”. J. Interprof. Care 2008, 22, 85–92. [Google Scholar] [CrossRef] [PubMed]
- Beekes, W.A. The ’Millionaire’ method for encouraging participation. Act. Learn. High. Educ. 2006, 7, 25–36. [Google Scholar] [CrossRef]
- Voelkel, S.; Bennett, D. New uses for a familiar technology: Introducing mobile phone polling in large classes. Innov. Educ. Teach. Int. 2013, 51, 46–58. [Google Scholar] [CrossRef]
- O’Bannon, B.W.; Thomas, K.M. Mobile phones in the classroom: Preservice teachers answer the call. Comput. Educ. 2015, 85, 110–122. [Google Scholar] [CrossRef]
- Florenthal, B. Student perceptions of and satisfaction with mobile polling technology: An exploratory study. J. Adv. Mark. Educ. 2018, 26, 44–57. [Google Scholar]
- Beaumont, A.; Gousseau, M.; Sommerfeld, C.; Leitao, D.; Gooi, A. Mobile audience response systems at a continuing medical education conference. Stud. Health Technol. Inform. 2017. [Google Scholar] [CrossRef]
- Corbridge, S.J.; Corbridge, T.; Tiffen, J.; Carlucci, M. Implementing team-based learning in a nurse practitioner curriculum. Nurse Educ. 2013, 38, 202–205. [Google Scholar] [CrossRef]
- Chan, E.A.; Chi, S.P.M.; Ching, S.; Lam, S.K. Interprofessional education: The interface of nursing and social work. J. Clin. Nurs. 2010, 19, 168–176. [Google Scholar] [CrossRef]
- Carpenter, J.; Dickinson, H. Interprofessional Education and Training, 2nd ed.; Interprofessional Education and Training; The Policy Press: Bristol, UK, 2008. [Google Scholar]
- Foster, R.; Macleod Clark, J. Moderating the stereotypical views of health and social care students: The role of interprofessional education. J. Interprof. Care 2014, 29, 34–40. [Google Scholar] [CrossRef]
- Pettigrew, T.F.; Tropp, L.R. How does intergroup contact reduce prejudice? Meta-analytic tests of three mediators. Eur. J. Soc. Psychol. 2008, 38, 922–934. [Google Scholar] [CrossRef]
- MacKay, C.; Davis, A.M.; Mahomed, N.; Badley, E.M. Expanding roles in orthopaedic care: A comparison of physiotherapist and orthopaedic surgeon recommendations for triage. J. Eval. Clin. Pract. 2009, 15, 178–183. [Google Scholar] [CrossRef] [PubMed]
- Hamilton, J. Two birds with one stone: Addressing interprofessional education aims and objectives in health profession curricula through interdisciplinary cultural competency training. Med. Teach. 2011, 33, 199–203. [Google Scholar] [CrossRef]
- Hirt, B.; Shiozawa, T.; Herlan, S.; Wagner, H.-J.; Küppers, E. Surgical prosection in a traditional anatomical curriculum—Tübingens’ Sectio chirurgica. Ann. Anat. Anat. Anz. 2010, 192, 349–354. [Google Scholar] [CrossRef] [PubMed]
- Shiozawa, T.; Butz, B.; Herlan, S.; Kramer, A.; Hirt, B. Interactive anatomical and surgical live stream lectures improve students’ academic performance in applied clinical anatomy. Anat. Sci. Educ. 2016, 10, 46–52. [Google Scholar] [CrossRef] [PubMed]
- Grosser, J.; Bientzle, M.; Shiozawa, T.; Hirt, B.; Kimmerle, J. Acquiring clinical knowledge from an online video platform: A randomized controlled experiment on the relevance of integrating anatomical information and clinical practice. Anat. Sci. Educ. 2018, 12, 478–484. [Google Scholar] [CrossRef]
- Atack, L.; Parker, K.; Rocchi, M.; Maher, J.; Dryden, T. The impact of an online interprofessional course in disaster management competency and attitude towards interprofessional learning. J. Interprof. Care 2009, 23, 586–598. [Google Scholar] [CrossRef]
- Schichtel, M. Core-competence skills in e-mentoring for medical educators: A conceptual exploration. Med. Teach. 2010, 32, e248–e262. [Google Scholar] [CrossRef]
| Assessment Criteria | Social Interaction | Individual Knowledge Acquisition | Entertainment | Vividness of the Material | Organizational Effort | Flexibility | Costs | |
|---|---|---|---|---|---|---|---|---|
| Text-based | Asynchronous | − | + | ~ | − | − | + | − |
| Synchronous | + | − | ~ | − | − | − | ~ | |
| Video-based | Asynchronous | − | + | + | + | + | + | ~ |
| Synchronous | + | − | + | + | + | − | + | |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Grosser, J.; Bientzle, M.; Kimmerle, J. A Literature Review on the Foundations and Potentials of Digital Teaching Scenarios for Interprofessional Health Care Education. Int. J. Environ. Res. Public Health 2020, 17, 3410. https://doi.org/10.3390/ijerph17103410
Grosser J, Bientzle M, Kimmerle J. A Literature Review on the Foundations and Potentials of Digital Teaching Scenarios for Interprofessional Health Care Education. International Journal of Environmental Research and Public Health. 2020; 17(10):3410. https://doi.org/10.3390/ijerph17103410
Chicago/Turabian StyleGrosser, Johannes, Martina Bientzle, and Joachim Kimmerle. 2020. "A Literature Review on the Foundations and Potentials of Digital Teaching Scenarios for Interprofessional Health Care Education" International Journal of Environmental Research and Public Health 17, no. 10: 3410. https://doi.org/10.3390/ijerph17103410
APA StyleGrosser, J., Bientzle, M., & Kimmerle, J. (2020). A Literature Review on the Foundations and Potentials of Digital Teaching Scenarios for Interprofessional Health Care Education. International Journal of Environmental Research and Public Health, 17(10), 3410. https://doi.org/10.3390/ijerph17103410






