Changing Exposure Perceptions: A Randomized Controlled Trial of an Intervention with Smoking Parents
Abstract
1. Introduction
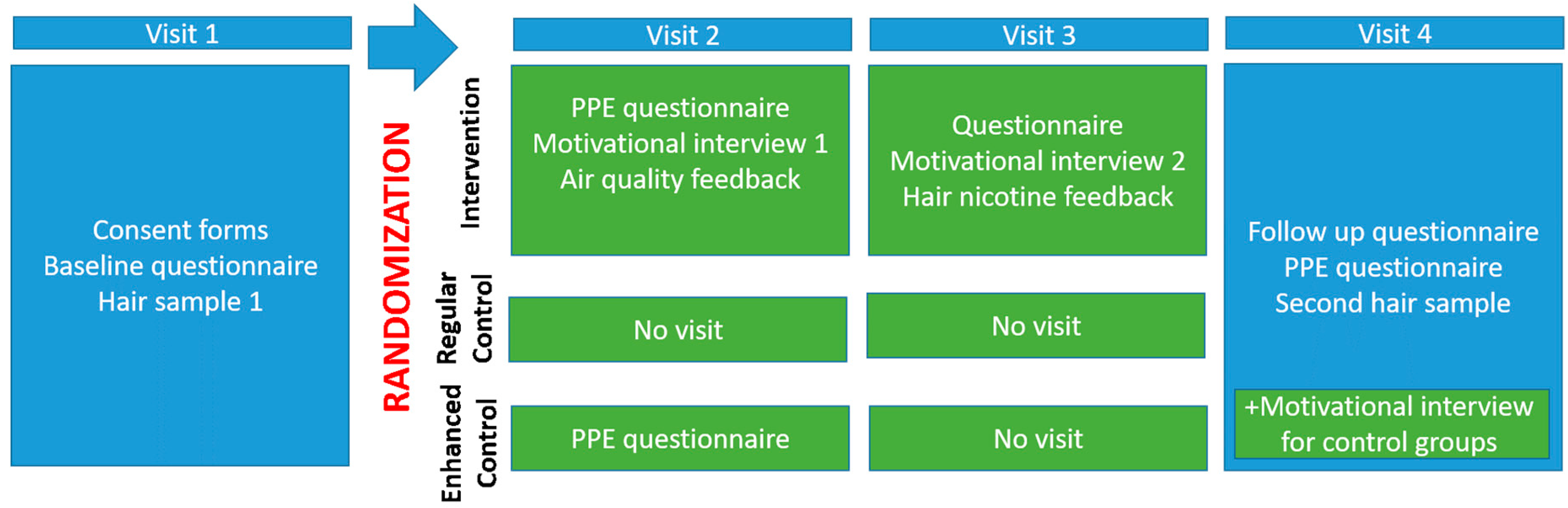
2. Materials and Methods
3. Results
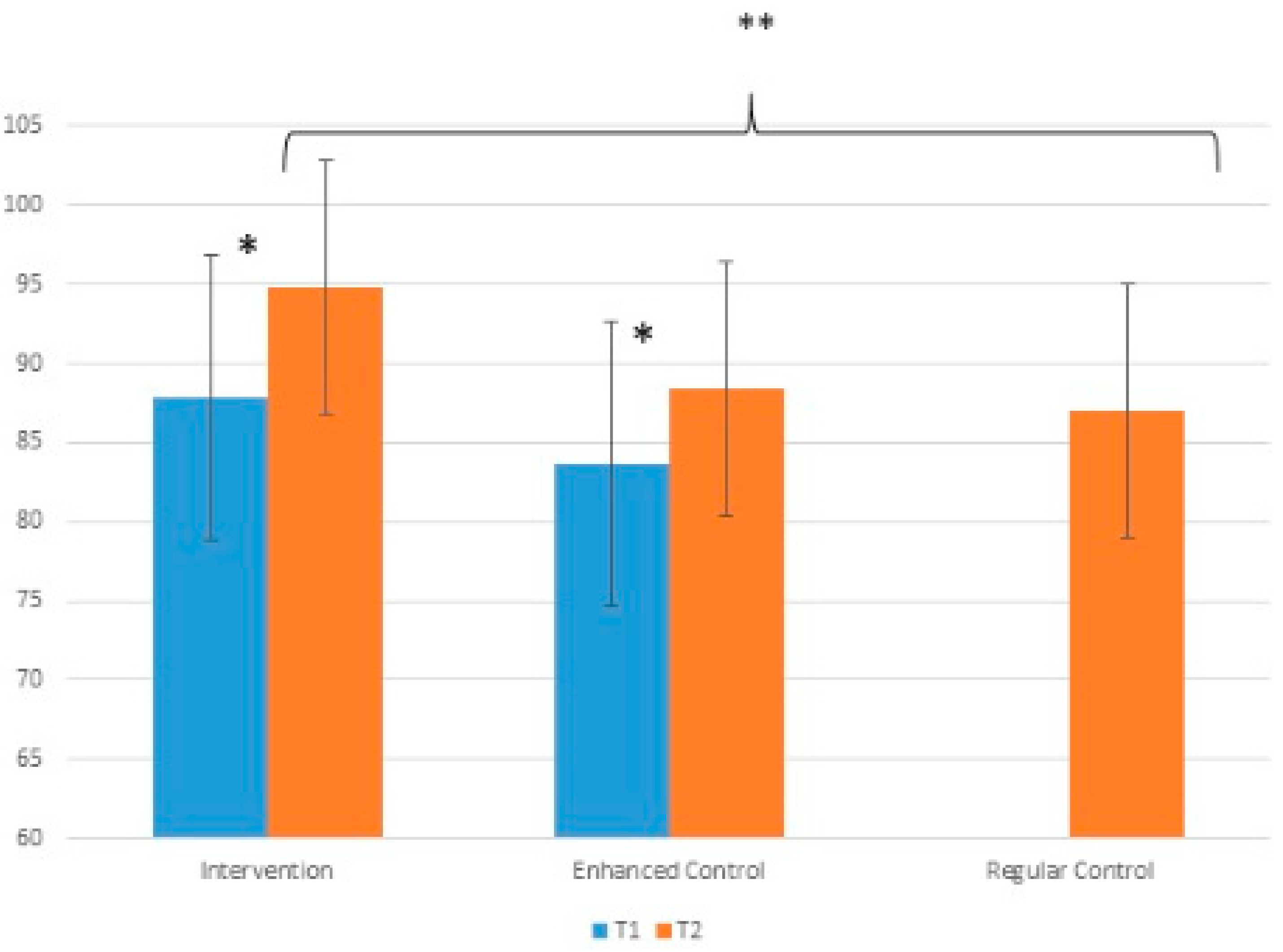
3.1. Parental Perceptions of Exposure (PPE)
3.2. Behavioural Outcomes
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Department of Health and Human Services. The Health Consequences of Involuntary Exposure to Tobacco Smoke: A Report of the Surgeon General; Centers for Disease Control and Prevention Office on Smoking and Health: Atlanta, GA, USA, 2006.
- Raghuveer, G.; White, D.A.; Hayman, L.L.; Woo, J.G.; Villafane, J.; Celermajer, D.; Ward, K.D.; de Ferranti, S.D.; Zachariah, J. Cardiovascular Consequences of Childhood Secondhand Tobacco Smoke Exposure: Prevailing Evidence, Burden, and Racial and Socioeconomic Disparities A Scientific Statement From the American Heart Association. Circulation 2016, 134, e336–e359. [Google Scholar] [CrossRef] [PubMed]
- Oberg, M.; Jaakkola, M.S.; Woodward, A.; Peruga, A.; Pruss-Ustun, A. Worldwide burden of disease from exposure to second-hand smoke: A retrospective analysis of data from 192 countries. Lancet 2011, 377, 139–146. [Google Scholar] [CrossRef]
- Leonardi-Bee, J.; Jere, M.L.; Britton, J. Exposure to parental and sibling smoking and the risk of smoking uptake in childhood and adolescence: A systematic review and meta-analysis. Thorax 2011, 66, 847–855. [Google Scholar] [CrossRef] [PubMed]
- Rosen, L.J.; Lev, E.; Guttman, N.; Tillinger, E.; Rosenblat, S.; Zucker, D.M.; Myers, V. Parental perceptions and misconceptions of child tobacco smoke exposure. Nicotine Tob. Res. 2018, 20, 1369–1377. [Google Scholar] [CrossRef] [PubMed]
- Kegler, M.C.; Haardörfer, R.; Bundy, L.T.; Escoffery, C.; Berg, C.J.; Fernandez, M.; Williams, R.; Hovell, M. Do partial home smoking bans signal progress toward a smoke-free home? Health Educ. Res. 2016, 31, 24–35. [Google Scholar] [CrossRef][Green Version]
- Johansson, A.K.; Hermansson, G.; Ludvigsson, J. How Should Parents Protect Their Children From Environmental Tobacco-Smoke Exposure in the Home? Pediatrics 2004, 113, e291–e295. [Google Scholar] [CrossRef]
- Spencer, N.; Blackburn, C.; Bonas, S.; Coe, C.; Dolan, A. Parent reported home smoking bans and toddler (18–30 month) smoke exposure: A cross-sectional survey. Arch. Dis. Child. 2005, 90, 670–674. [Google Scholar] [CrossRef]
- Hovell, M.; Zakarian, J.; Matt, G.E.; Liles, S.; Jones, J.A.; Hofstetter, C.R.; Larson, S.N.; Benowitz, N.L. Counseling to reduce children’s secondhand smoke exposure and help parents quit smoking: A controlled trial. Nicotine Tob. Res. 2009, 11, 1383–1394. [Google Scholar] [CrossRef]
- Irvine, L.; Crombie, I.K.; Clark, R.A.; Slane, P.W.; Feyerabend, C.; Goodman, K.E.; Cater, J.I. Advising parents of asthmatic children on passive smoking: Randomised controlled trial. Br. Med. J. 1999, 318, 1456–1459. [Google Scholar] [CrossRef]
- Wilson, S.R.; Farber, H.J.; Knowles, S.B.; Lavori, P.W. A randomized trial of parental behavioral counseling and cotinine feedback for lowering environmental tobacco smoke exposure in children with asthma: Results of the LET’S Manage Asthma trial. Chest 2011, 139, 581–590. [Google Scholar] [CrossRef]
- Fossum, B.; Arborelius, E.; Bremberg, S. Evaluation of a counseling method for the prevention of child exposure to tobacco smoke: An example of client-centered communication. Prev. Med. 2004, 38, 295–301. [Google Scholar] [CrossRef] [PubMed]
- Yilmaz, G.; Karacan, C.; Yoney, A.; Yilmaz, T. Brief intervention on maternal smoking: A randomized controlled trial. Child Care Health Dev. 2006, 32, 73–79. [Google Scholar] [CrossRef]
- Zakarian, J.M.; Hovell, M.F.; Sandweiss, R.D.; Hofstetter, C.R.; Matt, G.E.; Bernert, J.T.; Pirkle, J.; Hammond, S.K. Behavioral counseling for reducing children’s ETS exposure: Implementation in community clinics. Nicotine Tob. Res. 2004, 6, 1061–1074. [Google Scholar] [CrossRef] [PubMed]
- McIntosh, N.A.; Clark, N.M.; Howatt, W.F. Reducing tobacco smoke in the environment of the child with asthma: A cotinine-assisted, minimal-contact intervention. J. Asthma 1994, 31, 453–462. [Google Scholar] [CrossRef] [PubMed]
- Hovell, M.F.; Meltzer, S.B.; Wahlgren, D.R.; Matt, G.E.; Hofstetter, C.R.; Jones, J.A.; Meltzer, E.O.; Bernert, J.T.; Pirkle, J.L. Asthma management and environmental tobacco smoke exposure reduction in Latino children: A controlled trial. Pediatrics 2002, 110, 946–956. [Google Scholar] [CrossRef]
- Baxi, R.; Sharma, M.; Roseby, R.; Baxi, R.; Webster, P. Family and carer smoking control programmes for reducing children’s exposure to environmental tobacco smoke. Cochrane Database Syst. Rev. 2014, 1, CD001746. [Google Scholar] [CrossRef]
- Rosen, L.J.; Myers, V.; Hovell, M.; Zucker, D.; Ben Noach, M. Meta-analysis of parental protection of children from tobacco smoke exposure. Pediatrics 2014, 133, 698–714. [Google Scholar] [CrossRef]
- Myers, V.; Shiloh, S.; Rosen, L.J. Parental perceptions of children’s exposure to tobacco smoke: Development and validation of a new measure. BMC Public Health 2018, 18, 1031. [Google Scholar] [CrossRef]
- Myers, V.; Zucker, D.; Rosen, L.J.; Shiloh, S. Parental perceptions of children’s exposure to tobacco smoke and parental smoking behaviour. Int. J. Environ. Res. Public Health 2020, 17. [Google Scholar]
- Godin, G.; Sheeran, P.; Conner, M.; Delage, G.; Germain, M.; Bélanger-Gravel, A.; Naccache, H. Which survey questions change behavior? Randomized controlled trial of mere measurement interventions. Health Psychol. 2010, 29, 636–644. [Google Scholar] [CrossRef]
- Petrie, K.J.; Weinman, J. Patients’ Perceptions of Their Illness: The Dynamo of Volition in Health Care. Curr. Dir. Psychol. Sci. 2012, 21, 60–65. [Google Scholar] [CrossRef]
- McCambridge, J. From question-behaviour effects in trials to the social psychology of research participation. Psychol. Health 2015, 30, 72–84. [Google Scholar] [CrossRef]
- Rodrigues, A.M.; O’Brien, L.; French, D.P.; Glidewell, L.; Sniehotta, F.F. The Question–Behavior Effect: Genuine Effect or Spurious Phenomenon? A Systematic Review of Randomized Controlled Trials with Meta-Analyses. Health Psychol. 2015, 34, 61–78. [Google Scholar] [CrossRef] [PubMed]
- Chandon, P.; Morwitz, V.G.; Reinartz, W.J. Do Intentions Really Predict Behavior? Self-Generated Validity Effects in Survey Research. J. Market. 2005, 69, 1–14. [Google Scholar] [CrossRef]
- French, D.P.; Sutton, S. Reactivity of measurement in health psychology: How much of a problem is it? What can be done about it? Br. J. Health Psychol. 2010, 15, 453–468. [Google Scholar] [CrossRef]
- Morwitz, V.G.; Johnson, E.; Schmittlein, D. Does Measuring Intent Change Behavior? J. Consum. Res. 1993, 20, 46–61. [Google Scholar] [CrossRef]
- Morwitz, V.G.; Fitzsimons, G.J. The Mere-Measurement Effect: Why Does Measuring Intentions Change Actual Behavior? J. Consum. Psychol. 2004, 14, 64–74. [Google Scholar] [CrossRef]
- Abdullah, A.S.; Mak, Y.W.; Loke, A.Y.; Lam, T.H. Smoking cessation intervention in parents of young children: A randomised controlled trial. Addiction 2005, 100, 1731–1740. [Google Scholar] [CrossRef]
- Eriksen, W.; Sorum, K.; Bruusgaard, D. Effects of information on smoking behaviour in families with preschool children. Acta Pediatr. 1996, 85, 209–212. [Google Scholar] [CrossRef]
- Petrie, K.J.; Cameron, L.D.; Ellis, C.J.; Buick, D.; Weiman, J. Changing Illness Perceptions After Myocardial Infarction: An Early Intervention Randomized Controlled Trial. Psychosom. Med. 2002, 64, 580–586. [Google Scholar] [CrossRef]
- Siemonsma, P.C.; Stuive, I.; Roorda, L.D.; Vollebregt, J.A.; Walker, M.F.; Lankhorst, G.J.; Lettinga, A.T. Cognitive treatment of illness perceptions in patients with chronic low back pain: A randomized controlled trial. Phys. Ther. 2013, 93, 435–448. [Google Scholar] [CrossRef] [PubMed]
- Meyer, D.; Leventhal, H.; Gutmann, M. Common-sense models of illness: The example of hypertension. Health Psychol. 1985, 4, 115–135. [Google Scholar] [CrossRef] [PubMed]
- Conrad, P. Who comes to work-site wellness programs? A preliminary review. J. Occup. Med. 1987, 29, 317–320. [Google Scholar] [PubMed]
| Total (n = 159) | Intervention (n = 69) | Enhanced Control (n = 20) | Regular Control (n = 70) | F Value ANOVA (df) | p Value | ||
| Child age (months) Mean (SD) | 37.46 (23.01) | 40.68 (22.98) | 39.15 (23.18) | 33.80 (22.80) | 1.742 (2155) | 0.179 | |
| Parental cigarettes/day Mean (SD) | 15.02 (9.59) | 14.56 (10.01) | 16.75 (8.13) | 14.97 (9.62) | 0.403 (2156) | 0.669 | |
| Total (n = 159) | Intervention (n = 69) | Enhanced control (n = 20) | Regular control (n = 70) | Chi square | p Value | ||
| Child gender | Female | 82 (51.6%) | 40 (58.0%) | 12 (60.0%) | 30 (42.9%) | 3.829 | 0.147 |
| Mother’s education | No academic degree | 50 (30.8%) | 26 (38.0%) | 6 (30.0%) | 18 (26.1%) | 2.205 | 0.332 |
| Academic degree | 106 (67.9%) | 42 (61.8%) | 14 (70.0%) | 50 (73.5%) | |||
| Father’s education | No academic degree | 82 (51.9%) | 38 (56.0%) | 11 (55.0%) | 32 (45.7%) | 0.876 | 0.645 |
| Academic degree | 69 (43.9%) | 28 (41.8%) | 8 (40.0%) | 33 (47.1%) | |||
| Socioeconomic status (self-reported family income) | Above average | 68 (43.0%) | 32 (47.1%) | 7 (35.0%) | 29 (41.4%) | 7.311 | 0.293 |
| Average | 49 (31.0%) | 20 (29.4%) | 5 (25.0%) | 24 (34.3%) | |||
| Below average | 36 (22.8%) | 12 (17.6%) | 7 (35.0%) | 17 (24.3%) | |||
| PPE at T1 | PPE at T2 | Mean PPE Change | Paired t Test (df) | p Value | |
|---|---|---|---|---|---|
| Intervention (n = 69) | 88.13 ± 18.35 (n = 67) | 94.76 ± 17.55 (n = 62) | 7.02 (17.81) (n = 61) | −3.077 (60) | 0.003 |
| Enhanced Control (n = 20) | 84.40 ± 21.39 (n = 15) | 89.44 ± 18.98 (n = 16) | 13.58 (15.42) (n = 12) | −3.052 (11) | 0.011 |
| Regular control (n = 70) | - | 87.00 ± 19.52 (n = 66) | - | - | |
| Total with repeated PPE measures (n = 73) | 86.51 ± 19.34 | 94.60 ± 17.60 | 8.10 (17.51) | −3.950 (72) | <0.001 |
| Intervention | Control | Enhanced Control | |
|---|---|---|---|
| Home smoking ban | 4 (5.8%) | 1 (1.4%) | 0 |
| Car smoking ban | 1 (1.4%) | 0 | 0 |
| Quit smoking | 9 (13.0%) | 5 (7.1%) | 0 |
| Reduced smoking | 2 (2.9%) | 5 (7.1%) | 1 (5.0%) |
| Smoke less around children/close balcony door when smoking | 11 (15.9%) | 1 (1.4%) | 1 (5.0%) |
| Any positive change | 39.1% | 17.1% | 10.0% |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Myers, V.; Shiloh, S.; Zucker, D.M.; Rosen, L.J. Changing Exposure Perceptions: A Randomized Controlled Trial of an Intervention with Smoking Parents. Int. J. Environ. Res. Public Health 2020, 17, 3349. https://doi.org/10.3390/ijerph17103349
Myers V, Shiloh S, Zucker DM, Rosen LJ. Changing Exposure Perceptions: A Randomized Controlled Trial of an Intervention with Smoking Parents. International Journal of Environmental Research and Public Health. 2020; 17(10):3349. https://doi.org/10.3390/ijerph17103349
Chicago/Turabian StyleMyers, Vicki, Shoshana Shiloh, David M. Zucker, and Laura J. Rosen. 2020. "Changing Exposure Perceptions: A Randomized Controlled Trial of an Intervention with Smoking Parents" International Journal of Environmental Research and Public Health 17, no. 10: 3349. https://doi.org/10.3390/ijerph17103349
APA StyleMyers, V., Shiloh, S., Zucker, D. M., & Rosen, L. J. (2020). Changing Exposure Perceptions: A Randomized Controlled Trial of an Intervention with Smoking Parents. International Journal of Environmental Research and Public Health, 17(10), 3349. https://doi.org/10.3390/ijerph17103349





