Comparison of Maternal Functioning between Iranian Mothers with and without Depressive Symptoms: A Case-Control Study
Abstract
1. Introduction
2. Material and Methods
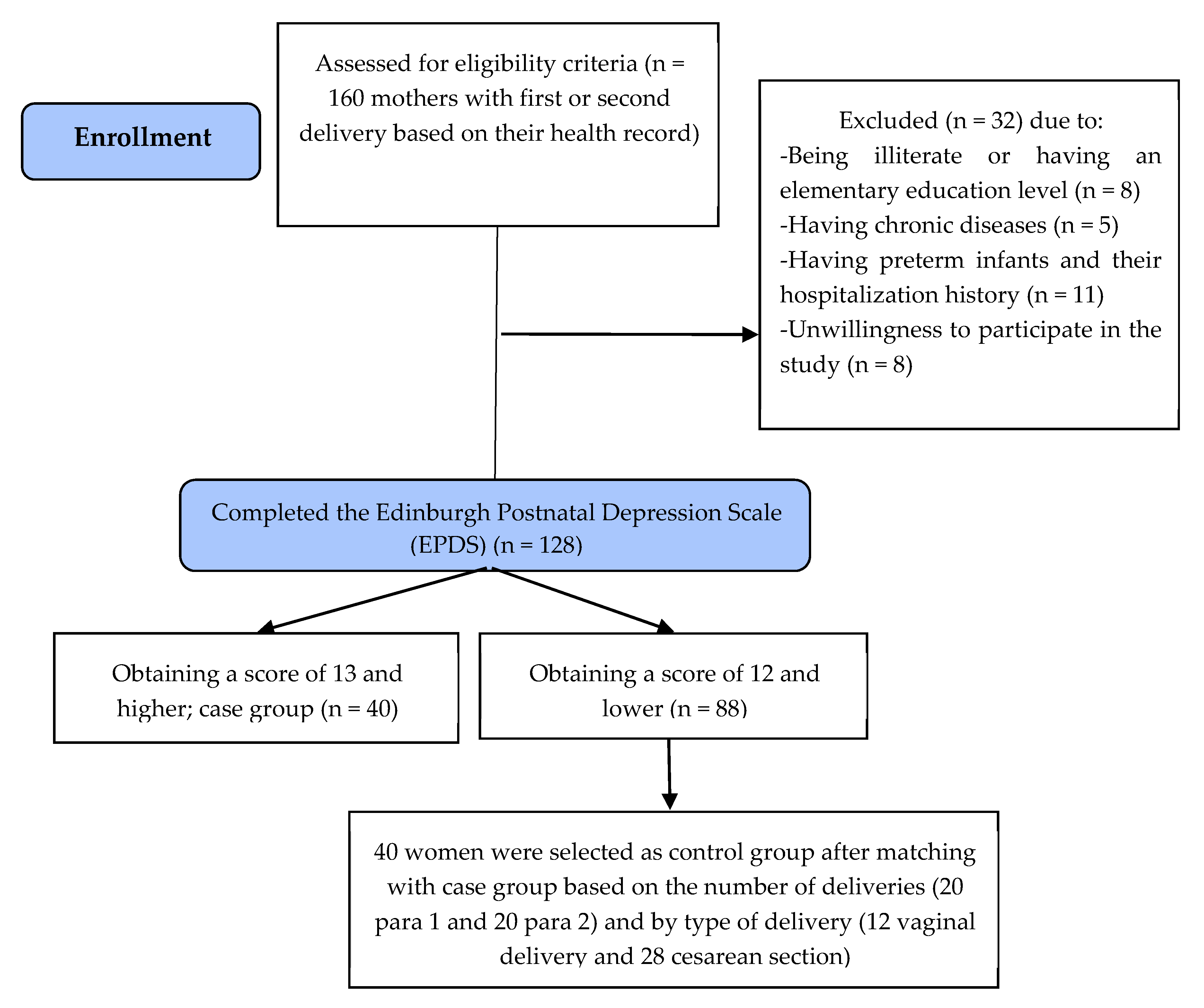
2.1. Participants and Study Design
2.2. Sample Size Calculation
2.3. Sampling
2.4. Data Collection Tools
2.4.1. Sociodemographic and Obstetrics Characteristics Questionnaire
2.4.2. Barkin Index of Maternal Functioning (BIMF)
2.4.3. Edinburgh Postnatal Depression Scale (EPDS)
2.5. Analysis of the Data
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- McGarry, J.; Kim, H.; Sheng, X.; Egger, M.; Baksh, L. Postpartum depression and help-seeking behavior. J. Midwifery Womens Health 2009, 54, 50–56. [Google Scholar] [CrossRef] [PubMed]
- Liu, S.; Yan, Y. Risk factors for postpartum depression among Chinese women: Path model analysis. BMC Pregnancy Childbirth 2017, 17, 133. [Google Scholar] [CrossRef] [PubMed]
- Henshaw, C. Mood disturbance in the early puerperium: A review. Arch. Womens Ment. Health 2003, 6 (Suppl. 2), S33–S42. [Google Scholar] [CrossRef] [PubMed]
- Heron, J.; Craddock, N.; Jones, I. Postnatal euphoria: Are ‘the highs’ an indicator of bipolarity? Bipolar. Disord. 2005, 7, 103–110. [Google Scholar] [CrossRef] [PubMed]
- Stein, A.; Craske, M.G.; Lehtonen, A.; Harvey, A.; Savage-McGlynn, E.; Davies, B.; Goodwin, J.; Murray, L.; Cortina-Borja, M.; Counsell, N. Maternal cognitions and mother-infant interaction in postnatal depression and generalized anxiety disorder. J. Abnorm. Psychol. 2012, 121, 795–809. [Google Scholar] [CrossRef] [PubMed]
- Ali, N.S.; Mahmud, S.; Khan, A.; Ali, B.S. Impact of postpartum anxiety and depression on child’s mental development from two peri-urban communities of Karachi, Pakistan: A quasi-experimental study. BMC Psychiatry 2013, 13, 274. [Google Scholar] [CrossRef]
- Logsdon, M.C.; Wisner, K.; Hanusa, B.H.; Phillips, A. Role functioning and symptom remission in women with postpartum depression after antidepressant treatment. Arch. Psychiatr. Nurs. 2003, 17, 276–283. [Google Scholar] [CrossRef]
- Wisner, K.L.; Parry, B.L.; Piontek, C.M. Clinical practice. Postpartum depression. N. Engl. J. Med. 2002, 347, 194–199. [Google Scholar] [CrossRef]
- Postnatal Depression and Perinatal Mental Health. Available online: https://www.mind.org.uk/information-support/types-of-mental-health-problems/postnatal-depression-and-perinatal-mental-health/postnatal-and-antenatal-depression/ (accessed on 4 April 2020).
- Association, A.P. Diagnostic and Statistical Manual of Mental Disorders (DSM-5®), 5th ed.; American Psychiatric Pub: Washington, DC, USA, 2013; pp. 186–187. [Google Scholar]
- Klainin, P.; Arthur, D.G. Postpartum depression in Asian cultures: A literature review. Int. J. Nurs. Stud. 2009, 46, 1355–1373. [Google Scholar] [CrossRef]
- Barkin, J.L.; Wisner, K.L.; Bromberger, J.T.; Beach, S.R.; Wisniewski, S.R. Assessment of functioning in new mothers. J. Womens Health (Larchmt) 2010, 19, 1493–1499. [Google Scholar] [CrossRef]
- Barkin, J.L.; Wisner, K.L.; Bromberger, J.T.; Beach, S.R.; Terry, M.A.; Wisniewski, S.R. Development of the Barkin Index of Maternal Functioning. J. Womens Health (Larchmt) 2010, 19, 2239–2246. [Google Scholar] [CrossRef] [PubMed]
- Barkin, J.L.; Willis, G.B.; Hawkins, K.C.; Stanfill-Thomas, T.; Beals, L.; Bloch, J.R. Semantic Assessment of the Barkin Index of Maternal Functioning in a Medically Underserved Obstetric Population. Perspect. Psychiatr. Care 2017, 53, 95–103. [Google Scholar] [CrossRef] [PubMed]
- Chamgurdani, F.K.; Barkin, J.L.; Esmaeilpour, K.; Malakouti, J.; Buoli, M.; Mirghafourvand, M. The effect of counseling with a skills training approach on maternal functioning: A randomized controlled clinical trial. BMC Womens Health 2020, 20, 51. [Google Scholar] [CrossRef] [PubMed]
- Barkin, J.L.; Wisner, K.L.; Bromberger, J.T.; Beach, S.R.; Wisniewski, S.R. Factors Associated with Postpartum Maternal Functioning in Women with Positive Screens for Depression. J. Womens Health (Larchmt) 2016, 25, 707–713. [Google Scholar] [CrossRef] [PubMed]
- Barkin, J.L.; McKeever, A.; Lian, B.; Wisniewski, S.R. Correlates of Postpartum Maternal Functioning in a Low-Income Obstetric Population. J. Am. Psychiatr. Nurses Assoc. 2017, 23, 149–158. [Google Scholar] [CrossRef]
- Barkin, J.L.; Stausmire, J.M.; Te, M.N.; Pazik-Huckaby, A.; Serati, M.; Buoli, M.; Harding, R.S.; Bruss, C.A.; Stausmire, K.L. Evaluation of Maternal Functioning in Mothers of Infants Admitted to the Neonatal Intensive Care Unit. J. Womens Health (Larchmt) 2019, 28, 941–950. [Google Scholar] [CrossRef]
- Montazeri, A.; Torkan, B.; Omidvari, S. The Edinburgh Postnatal Depression Scale (EPDS): Translation and validation study of the Iranian version. BMC Psychiatry 2007, 7, 11. [Google Scholar] [CrossRef]
- Posmontier, B. Functional status outcomes in mothers with and without postpartum depression. J. Midwifery Womens Health 2008, 53, 310–318. [Google Scholar] [CrossRef]
- Barkin, J.L.; Wisner, K.L.; Wisniewski, S.R. The psychometric properties of the Barkin Index of Maternal Functioning. J. Obstet. Gynecol. Neonatal. Nurs. 2014, 43, 792–802. [Google Scholar] [CrossRef]
- Barkin, J.L.; Wisner, K.L. The role of maternal self-care in new motherhood. Midwifery 2013, 29, 1050–1055. [Google Scholar] [CrossRef]
- Mirghafourvand, M.; Barkin, J.L.; Asghari Jafarabadi, M.; Karami, F.; Ghanbari-Homayi, S. The psychometric properties of the Barkin index of maternal functioning (BIMF) for the Iranian population. BMC Womens Health 2019, 19, 166. [Google Scholar] [CrossRef] [PubMed]
- Wisner, K.L.; Sit, D.K.Y.; McShea, M.C.; Rizzo, D.M.; Zoretich, R.A.; Hughes, C.L.; Eng, H.F.; Luther, J.F.; Wisniewski, S.R.; Costantino, M.L.; et al. Onset Timing, Thoughts of Self-harm, and Diagnoses in Postpartum Women With Screen-Positive Depression Findings. JAMA Psychiatry 2013, 70, 490–498. [Google Scholar] [CrossRef] [PubMed]
- Kheirabadi, G.R.; Maracy, M.R.; Akbaripour, S.; Masaeli, N. Psychometric properties and diagnostic accuracy of the edinburgh postnatal depression scale in a sample of Iranian women. Iran J. Med. Sci. 2012, 37, 32–38. [Google Scholar] [PubMed]
- Fathi, F.; Mohammad-Alizadeh-Charandabi, S.; Mirghafourvand, M. Maternal self-efficacy, postpartum depression, and their relationship with functional status in Iranian mothers. Women Health 2018, 58, 188–203. [Google Scholar] [CrossRef]
- Barkin, J.L.; Bloch, J.R.; Hawkins, K.C.; Thomas, T.S. Barriers to optimal social support in the postpartum period. J. Obstet. Gynecol. Neonatal. Nurs. 2014, 43, 445–454. [Google Scholar] [CrossRef]
- Logsdon, M.C.; Wisner, K.; Sit, D.; Luther, J.F.; Wisniewski, S.R. Depression treatment and maternal functioning. Depress. Anxiety 2011, 28, 1020–1026. [Google Scholar] [CrossRef]
- Santini, Z.I.; Koyanagi, A.; Tyrovolas, S.; Mason, C.; Haro, J.M. The association between social relationships and depression: A systematic review. J. Affect. Disord. 2015, 175, 53–65. [Google Scholar] [CrossRef]
- Bagherinia, M.; Mirghafourvand, M.; Shafaie, F.S. The effect of educational package on functional status and maternal self-confidence of primiparous women in postpartum period: A randomized controlled clinical trial. J. Matern. Fetal Neonatal Med. 2017, 30, 2469–2475. [Google Scholar] [CrossRef]
| Variable | Case (n = 40) | Control (n = 40) | p-Value |
|---|---|---|---|
| Number (Percent) | Number (Percent) | ||
| Age # | 29.1 (6.0) | 28.0 (5.4) | 0.395 * |
| Husband age # | 33.2 (4.4) | 32.6 (4.8) | 0.562 * |
| Child sex | 0.260 † | ||
| Girl | 20 (50.0) | 15 (37.5) | |
| Boy | 20 (50.0) | 25 (62.5) | |
| Job | 1.000 ‡ | ||
| Housewife | 37 (92.5) | 37 (92.5) | |
| Employed | 3 (7.5) | 3 (7.5) | |
| Husband’s job | 0.916 † | ||
| Worker | 12 (30.0%) | 10 (25.0) | |
| Employee | 9 (22.5) | 9 (22.5) | |
| Shopkeeper | 5 (12.5) | 7 (17.5) | |
| Others | 14 (35.0) | 14 (35.0) | |
| Education | 0.284 § | ||
| Secondary school | 10 (25.0) | 6 (15.0) | |
| High school | 2 (5.0) | 4 (10.0) | |
| Diploma | 20 (50.0) | 18(45.0) | |
| Academic | 8 (20.0) | 12 (30.0) | |
| Husband’s education | 0.365 § | ||
| Elementary | 5 (12.5) | 1 (2.5) | |
| Secondary school | 11 (27.5) | 11 (27.5) | |
| High school | 3 (7.5) | 5 (12.5) | |
| Diploma | 10 (25.0) | 11 (27.5) | |
| Academic | 11 (27.5) | 12 (30.0) | |
| Sufficiency of monthly income for living expenses | 0.060 § | ||
| Completely sufficient | 4 (10.0) | 10 (25.0) | |
| Somewhat sufficient | 30 (75.0) | 27 (67.5) | |
| Insufficient | 6 (15.0) | 3 (7.5) | |
| Husband’s support | 0.085 § | ||
| Too much | 11 (27.5) | 14 (35.0) | |
| Much | 9 (22.5) | 14 (35.0) | |
| Medium | 7 (17.5) | 7 (17.5) | |
| Low | 9 (22.5) | 2 (5.0) | |
| Very little | 4 (10.0) | 3 (7.5) | |
| Family’s support | 0.340 § | ||
| Too much | 13 (32.5) | 14 (35.0) | |
| Much | 8 (20.0) | 11 (27.5) | |
| Medium | 6 (15.0) | 7 (17.5) | |
| Low | 7 (17.5) | 4 (10.0) | |
| Very little | 6 (15.0) | 4 (10.0) | |
| Unwanted pregnancy | 0.446 † | ||
| Yes | 12 (30.0) | 9 (22.5) | |
| No | 28 (70.0) | 31 (77.5) | |
| Variable | Case (n = 40) Mean (SD) | Control (n = 40) Mean (SD) | Mean Difference (95% Confidence Interval) | p-Value * |
|---|---|---|---|---|
| Total score of Maternal Functioning (Scale range: 0 to 120) | 63.4 (12.2) | 93.3 (13.0) | −30.0 (−35.6 to −24.3) | <0.001 |
| Self-care (Score range: 0 to 18) | 10.1 (2.8) | 14.3 (3.6) | −3.7 (−5.6 to −2.7) | <0.001 |
| Infant care (Score range: 0 to 12) | 7.8 (1.7) | 10.8 (2.4) | −2.8 (−3.7 to −1.9) | <0.001 |
| Mother-child interaction (Score range: 0 to 18) | 7.0 (1.6) | 6.5 (1.6) | 0.5 (−0.3 to 1.2) | 0.219 |
| Psychological well-being (Score range: 0 to 60) | 29.8 (7.1) | 42.8 (4.4) | −12.9 (−15.5 to −10.3) | <0.001 |
| Social support (Score range: 0 to 18) | 7.9 (3.7) | 14.5 (3.6) | −6.6 (−8.2 to −4.9) | <0.001 |
| Management (Score range: 0 to 36) | 18.4 (4.4) | 25.4 (4.7) | −7.0 (−9.0 to −5.0) | <0.001 |
| Adjustment (Score range: 0 to 12) | 7.5 (1.9) | 10.6 (2.4) | −3.1 (−4.1 to −2.1) | <0.001 |
| Variable | Correlation with Postpartum Depressive Symptoms Score r (p-Value) |
|---|---|
| Total score of Maternal Functioning | −0.79 (<0.001) |
| Self-care | −0.62 (<0.001) |
| Infant care | −0.54 (<0.001) |
| Mother-child interaction | −0.81 (<0.001) |
| Psychological well-being | −0.74 (<0.001) |
| Social support | −0.71 (<0.001) |
| Management | −0.62 (<0.001) |
| Adjustment | −0.57 (<0.001) |
| Variable | B (Confidence Interval 95%) | p-Value |
|---|---|---|
| Groups (Reference: Control) | ||
| Case | −30.1 (−36.8 to −23.4) | <0.001 |
| Age # | −0.0 (−1.0 to 0.9) | 0.976 |
| Husband age # | −0.4 (−1.5 to 0.8) | 0.542 |
| Child sex (Reference: Boy) | ||
| Girl | 2.0 (−5.9 to 10.0) | 0.615 |
| Job (Reference: Employed) | ||
| Housewife | −10.0 (−24.3 to 4.4) | 0.169 |
| Husband’s job (Reference: Others) | ||
| Worker | −1.1 (−10.2 to 8.0) | 0.806 |
| Employee | −3.6 (−16.2 to 8.9) | 0.566 |
| Shopkeeper | −5.1 (−15.6 to 5.3) | 0.331 |
| Education (Reference: Academic) | ||
| Secondary school | −1.2 (−14.5 to 12.0) | 0.850 |
| High school | −7.2 (−23.1 to 8.8) | 0.371 |
| Diploma | 3.6 (−6.4 to 13.7) | 0.471 |
| Husband’s education (Reference: Academic) | ||
| Elementary | 3.4 (−15.0 to 21.7) | 0.714 |
| Secondary school | 8.0 (−6.4 to 22.4) | 0.271 |
| High school | 1.3 (−14.2 to 16.7) | 0.869 |
| Diploma | 4.2 (−8.5 to 16.9) | 0.508 |
| Sufficiency of monthly income for living expenses (Reference: Insufficient) | ||
| Completely sufficient | 5.2 (−8.7 to 19.1) | 0.456 |
| Somewhat sufficient | 2.6 (−9.4 to 14.6) | 0.666 |
| Husband’s support (Reference: Very little) | ||
| Too much | −1.6 (−22.3 to 19.2) | 0.880 |
| Much | −8.8 (−27.5 to 9.8) | 0.346 |
| Medium | −11.5 (−29.0 to 6.1) | 0.195 |
| Low | −6.0 (−24.9 to 13.0) | 0.530 |
| Family’s support (Reference: Very little) | ||
| Too much | −0.6 (−20.0 to 18.7) | 0.947 |
| Much | 9.0 (−9.5 to 27.5) | 0.333 |
| Medium | 7.2 (−10.8 to 25.2) | 0.427 |
| Low | 4.3 (−11.8 to 20.3) | 0.596 |
| Unwanted pregnancy (Reference: No) | ||
| Yes | 3.9 (−5.0 to 12.7) | 0.383 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Karami Chamgurdani, F.; Barkin, J.L.; Curry, C.L.; Mirghafourvand, M. Comparison of Maternal Functioning between Iranian Mothers with and without Depressive Symptoms: A Case-Control Study. Int. J. Environ. Res. Public Health 2020, 17, 3350. https://doi.org/10.3390/ijerph17103350
Karami Chamgurdani F, Barkin JL, Curry CL, Mirghafourvand M. Comparison of Maternal Functioning between Iranian Mothers with and without Depressive Symptoms: A Case-Control Study. International Journal of Environmental Research and Public Health. 2020; 17(10):3350. https://doi.org/10.3390/ijerph17103350
Chicago/Turabian StyleKarami Chamgurdani, Fatemeh, Jennifer L. Barkin, Carolann L. Curry, and Mojgan Mirghafourvand. 2020. "Comparison of Maternal Functioning between Iranian Mothers with and without Depressive Symptoms: A Case-Control Study" International Journal of Environmental Research and Public Health 17, no. 10: 3350. https://doi.org/10.3390/ijerph17103350
APA StyleKarami Chamgurdani, F., Barkin, J. L., Curry, C. L., & Mirghafourvand, M. (2020). Comparison of Maternal Functioning between Iranian Mothers with and without Depressive Symptoms: A Case-Control Study. International Journal of Environmental Research and Public Health, 17(10), 3350. https://doi.org/10.3390/ijerph17103350






