An Application of Metabolic Syndrome Severity Scores in the Lifestyle Risk Assessment of Taiwanese Adults
Abstract
1. Introduction
2. Methods
2.1. Data Source
2.2. Study Sample
2.3. Response Variables
2.4. Explanatory Variables
2.5. Statistical Analysis
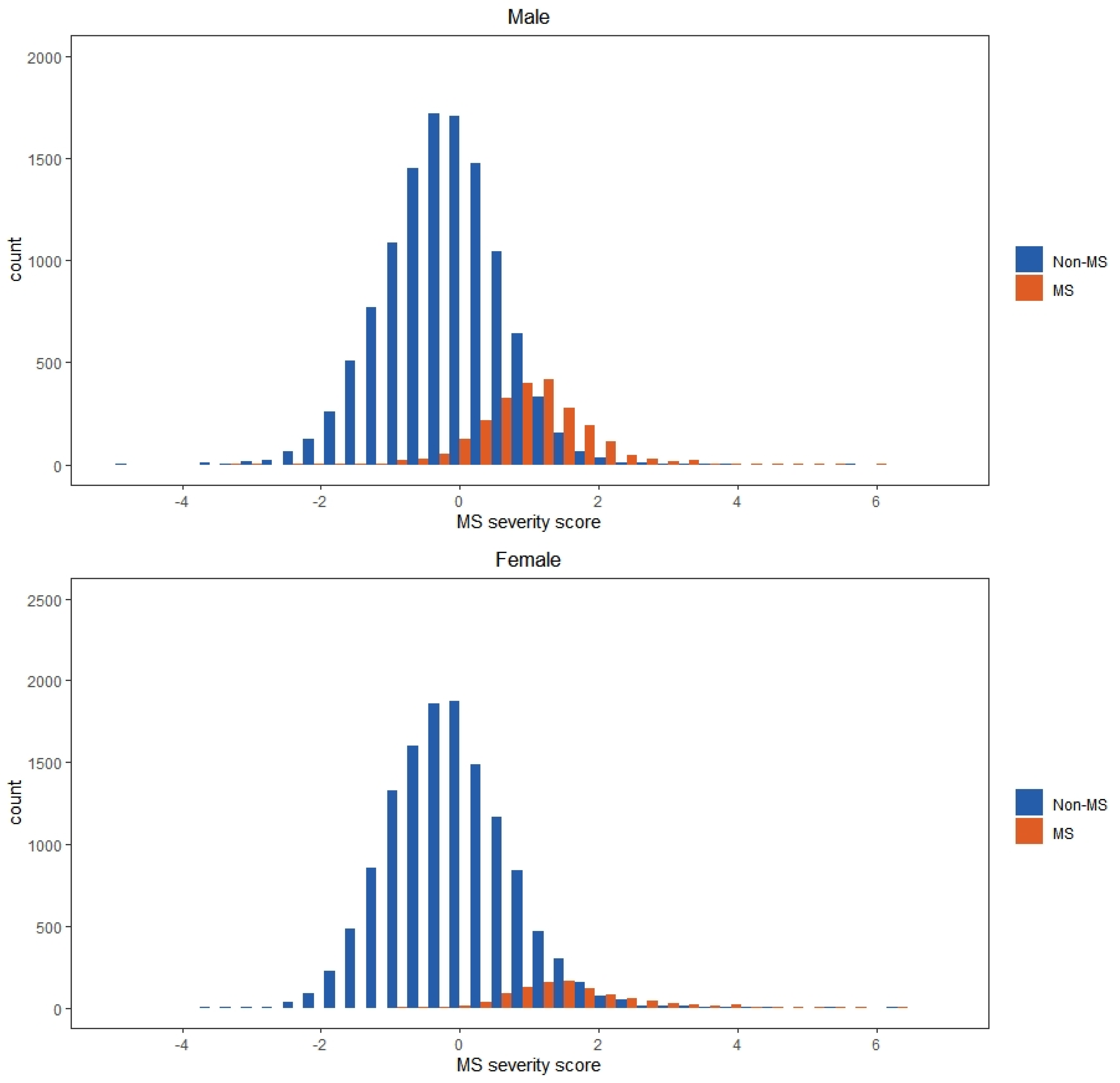
3. Results
4. Discussions
5. Conclusions
Funding
Acknowledgments
Conflicts of Interest
References
- Ranasinghe, P.; Mathangasinghe, Y.; Jayawardena, R.; Hills, A.P.; Misra, A. Prevalence and trends of metabolic syndrome among adults in the Asia-Pacific region: A systematic review. BMC Public Health 2017, 17, 101. [Google Scholar] [CrossRef]
- Zhou, H.; Ma, Z.F.; Lu, Y.; Du, Y.; Shao, J.; Wang, L.; Wu, Q.; Pan, B.; Zhu, W.; Zhao, Q.; et al. Elevated serum uric acid, hyperuricaemia and dietary patterns among adolescents in mainland China. J. Pediatr. Endocrinol. Metab. 2020, 33, 487–493. [Google Scholar] [CrossRef] [PubMed]
- Jahangiry, L.; Shojaeizadeh, D.; Montazeri, A.; Najafi, M.; Mohammad, K.; Farhangi, M.A. Modifiable lifestyle risk factors and metabolic syndrome: Opportunities for a web based preventive program. J. Res. Health Sci. 2014, 14, 303–307. [Google Scholar] [PubMed]
- Racette, S.B.; Deusinger, S.S.; Inman, C.L.; Burlis, T.L.; Highstein, G.R.; Buskirk, T.D.; Steger-May, K.; Peterson, L.R. Worksite Opportunities for Wellness (WOW): Effects on cardiovascular disease risk factors after 1 year. Prev. Med. 2009, 49, 108–114. [Google Scholar] [CrossRef]
- Kim, J.; Choi, Y.H. Physical activity, dietary vitamin C, and metabolic syndrome in Korean adults: The Korea National Health and Nutrition Examination Survey 2008 to 2012. Public Health 2016, 135, 30–37. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Guo, H.; Wu, M.; Liu, M. Serum and dietary antioxidant status is associated with lower prevalence of the metabolic syndrome in a study in Shanghai, China. Asia Pac. J. Clin. Nutr. 2013, 22, 60–68. [Google Scholar] [PubMed]
- Suzuki, K.; Ito, Y.; Inoue, T.; Hamajima, N. Inverse association of serum carotenoids with prevalence of metabolic syndrome among Japanese. Clin. Nutr. 2011, 30, 369–375. [Google Scholar] [CrossRef] [PubMed]
- Marquezine, G.F.; Oliveira, C.M.; Pereira, A.C.; Krieger, J.E.; Mill, J.G. Metabolic syndrome determinants in an urban population from Brazil: Social class and gender-specific interaction. Int. J. Cardiol. 2008, 129, 259–265. [Google Scholar] [CrossRef]
- Yoo, S.; Cho, H.J.; Khang, Y.H. General and abdominal obesity in South Korea, 1998–2007: Gender and socioeconomic differences. Prev. Med. 2010, 51, 460–465. [Google Scholar] [CrossRef]
- Kim, J.Y.; Kim, S.H.; Cho, Y.J. Socioeconomic status in association with metabolic syndrome and coronary heart disease risk. Korean J. Fam. Med. 2013, 34, 131–138. [Google Scholar] [CrossRef]
- Gale, E.A. Should we dump the metabolic syndrome?: Yes. BMJ 2008, 336, 640. [Google Scholar] [CrossRef]
- Ragland, D.R. Dichotomizing continuous outcome variables: Dependence of the magnitude of association and statistical power of the cut point. Epidemiology 1992, 3, 434–440. [Google Scholar] [CrossRef]
- Steele, R.M.; Brage, S.; Corder, K.; Wareham, N.J.; Ekelund, U. Physical activity, cardiorespiratory fitness, and the metabolic syndrome in youth. J. Appl. Physiol. 2008, 105, 342–351. [Google Scholar] [CrossRef] [PubMed]
- Kahn, R.; Buse, J.; Ferrannini, E.; Stern, M. The metabolic syndrome: Time for a critical appraisal. Diabetologia 2005, 48, 1684–1699. [Google Scholar] [CrossRef]
- Katzmarzyk, P.T.; Perusse, L.; Malina, R.M.; Bergeron, J.; Despres, J.; Bouchard, C. Stability of indicators of the metabolic syndrome from childhood and adolescence to young adulthood: The Quebec Family Study. J. Clin. Epidemiol. 2001, 54, 190–195. [Google Scholar] [CrossRef]
- Wijndaele, K.; Beunen, G.; Duvigneaud, N.; Matton, L.; Duquet, W.; Thomis, M.; Lefevre, J.; Philippaerts, R.M. A continuous metabolic syndrome risk score: Utility for epidemiological analyses. Diabetes Care 2006, 29, 2329. [Google Scholar] [CrossRef] [PubMed]
- Eisenmann, J.C.; Welk, G.J.; Wickel, E.E.; Blair, S.N. Combined influence of cardiorespiratory fitness and body mass index on cardiovascular disease risk factors among 8–18 year old youth: The Aerobics Center Longitudinal Study. Int. J. Pediatr. Obes. 2007, 2, 66–72. [Google Scholar] [CrossRef]
- Andersen, L.B.; Harro, M.; Sardinha, L.B.; Froberg, K.; Ekelund, U.; Brage, S.; Anderssen, S.A. Physical activity and clustered cardiovascular risk in children: A cross-sectional study (The European Youth Heart Study). Lancet 2006, 368, 299–304. [Google Scholar] [CrossRef]
- Raitakari, O.T.; Porkka, K.V.; Rasanen, L.; Ronnemaa, T.; Viikari, J.S. Clustering and six year cluster-tracking of serum total cholesterol, HDL-cholesterol and diastolic blood pressure in children and young adults: The Cardiovascular Risk in Young Finns Study. J. Clin. Epidemiol. 1994, 47, 1085–1093. [Google Scholar] [CrossRef]
- Gurka, M.J.; Ice, C.L.; Sun, S.S.; DeBoer, M.D. A confirmatory factor analysis of the metabolic syndrome in adolescents: An examination of sex and racial/ethnic differences. Cardiovasc. Diabetol. 2012, 11, 128. [Google Scholar] [CrossRef]
- Eisenmann, J.C. On the use of a continuous metabolic syndrome score in pediatric research. Cardiovasc. Diabetol. 2008, 7, 17. [Google Scholar] [CrossRef] [PubMed]
- Jung, K.J.; Jee, Y.H.; Jee, S.H. Metabolic risk score and vascular mortality among Korean adults: The Korean Metabolic Syndrome Mortality Study. Asia. Pac. J. Public Health 2017, 29, 122–131. [Google Scholar] [CrossRef] [PubMed]
- Huh, J.H.; Lee, J.H.; Moon, J.S.; Sung, K.C.; Kim, J.Y.; Kang, D.R. Metabolic syndrome severity score in Korean adults: Analysis of the 2010–2015 Korea National Health and Nutrition Examination Survey. J. Korean Med. Sci. 2019, 34, e48. [Google Scholar] [CrossRef] [PubMed]
- Low, S.; Khoo, K.C.J.; Wang, J.; Irwan, B.; Sum, C.F.; Subramaniam, T.; Lim, S.C.; Wong, T.K.M. Development of a metabolic syndrome severity score and its association with incident diabetes in an Asian population—Results from a longitudinal cohort in Singapore. Endocrine 2019, 65, 73–80. [Google Scholar] [CrossRef]
- Yang, X.; Tao, Q.; Sun, F.; Zhan, S. The impact of socioeconomic status on the incidence of metabolic syndrome in a Taiwanese health screening population. Int. J. Public Health 2012, 57, 551–559. [Google Scholar] [CrossRef]
- Liao, C.M.; Lin, C.M. Life course effects of socioeconomic and lifestyle factors on metabolic syndrome and 10-year risk of cardiovascular disease: A longitudinal study in Taiwan adults. Int. J. Environ. Res. Public Health 2018, 15, 2178. [Google Scholar] [CrossRef]
- Taiwan National Health Promotion Administration. 2007 Criteria of Metabolic Syndrome in Adults. Available online: https://www.hpa.gov.tw/Pages/Detail.aspx?nodeid=639&pid=1219 (accessed on 5 March 2019).
- Gurka, M.J.; Lilly, C.L.; Oliver, M.N.; DeBoer, M.D. An examination of sex and racial/ethnic differences in the metabolic syndrome among adults: A confirmatory factor analysis and a resulting continuous severity score. Metabolism 2014, 63, 218–225. [Google Scholar] [CrossRef]
- Sattar, N.; Forouhi, N.G. Metabolic syndrome criteria: Ready for clinical prime time or work in progress? Eur. Heart J. 2005, 26, 1249–1251. [Google Scholar] [CrossRef][Green Version]
- Kastelein, J. Cardiovascular risk—Through the ages. Atheroscler. Suppl. 2004, 5, 1–2. [Google Scholar] [CrossRef]
- Simmons, R.K.; Alberti, K.G.M.M.; Gale, E.A.M.; Colagiuri, S.; Tuomilehto, J.; Qiao, Q.; Ramachandran, A.; Tajima, N.; Mirchov, I.B.; Ben-Nakhi, A.; et al. The metabolic syndrome: Useful concept or clinical tool? Report of a WHO Expert Consultation. Diabetologia 2010, 53, 600–605. [Google Scholar] [CrossRef]
- Tuomilehto, J. Impact of age on cardiovascular risk: Implications for cardiovascular disease management. Atheroscler. Suppl. 2004, 5, 9–17. [Google Scholar] [CrossRef]
- Guseman, E.H.; Eisenmann, J.C.; Laurson, K.R.; Cook, S.R.; Stratbucker, W. Calculating a continuous metabolic syndrome score using nationally representative reference values. Acad. Pediatr. 2018, 18, 589–592. [Google Scholar] [CrossRef] [PubMed]
- Cook, S.; Auinger, P.; Huang, T.T.K. Growth curves for cardio-metabolic risk factors in children and adolescents. J. Pediatr. 2009, 155, S6.e15–S6.e26. [Google Scholar] [CrossRef] [PubMed]
- Kang, G.D.; Guo, L.; Guo, Z.R.; Hu, X.S.; Wu, M.; Yang, H.T. Continuous metabolic syndrome risk score for predicting cardiovascular disease in the Chinese population. Asia. Pac. J. Clin. Nutr. 2012, 21, 88. [Google Scholar] [PubMed]
- Berry, J.D.; Lloyd-Jones, D.M.; Garside, D.B.; Greenland, P. Framingham risk score and prediction of coronary heart disease death in young men. Am. Heart J. 2007, 154, 80–86. [Google Scholar] [CrossRef] [PubMed]
- Hemann, B.A.; Bimson, W.F.; Taylor, A.J. The Framingham Risk Score: An appraisal of its benefits and limitations. Am. Heart Hosp. J. 2007, 5, 91–96. [Google Scholar] [CrossRef]
- Khanna, R.; Kapoor, A.; Kumar, S.; Tewari, S.; Garg, N.; Goel, P.K. Metabolic syndrome and Framingham risk score: Observations from a coronary angiographic study in Indian patients. Indian J. Med. Res. 2013, 137, 295. [Google Scholar]
| Groups | T | MS (%) | WC | FPG | TG | HDL-C | SBP | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | |||
| Men | 13823 | 16.7 | 82.54 | 8.39 | 101.35 | 14.09 | 124.46 | 76.2 | 53.29 | 12.05 | 119.91 | 13.79 |
| 20–34 YRS | 4816 | 11.3 | 81.37 | 9.17 | 97.8 | 10.29 | 109.26 | 69.93 | 53.99 | 12.02 | 119.39 | 12.52 |
| 35–49 YRS | 4803 | 18.7 | 83.1 | 8.02 | 101.51 | 13.61 | 136.19 | 79.78 | 51.87 | 11.33 | 119.15 | 13.34 |
| 50–64 YRS | 4204 | 20.6 | 83.23 | 7.7 | 105.23 | 17.05 | 128.46 | 76.03 | 54.11 | 12.72 | 121.36 | 15.46 |
| Women | 13925 | 7 | 70.85 | 7.39 | 96.14 | 12.32 | 87.04 | 52.89 | 66.42 | 15.21 | 109.49 | 15.07 |
| 20–34 YRS | 4583 | 2.1 | 68.18 | 7.14 | 92.42 | 8.28 | 71.57 | 37.28 | 67.42 | 15.09 | 104.59 | 11.53 |
| 35–49 YRS | 5073 | 5.8 | 70.59 | 6.69 | 95.53 | 9.76 | 85.19 | 53.63 | 65.41 | 14.78 | 107.91 | 13.62 |
| 50–64 YRS | 4269 | 14.2 | 74.02 | 7.22 | 100.84 | 16.46 | 105.85 | 60.02 | 66.55 | 15.76 | 116.63 | 17.26 |
| Indices/Loadings | Men | Women | ||||
|---|---|---|---|---|---|---|
| 20–34 YRS | 35–49 YRS | 50–64 YRS | 20–34 YRS | 35–49 YRS | 50–64 YRS | |
| Indices | ||||||
| Chi-square | 85.353 | 96.288 | 88.174 | 23.355 | 65.790 | 31.043 |
| AIC | 107.353 | 118.288 | 110.174 | 45.355 | 87.790 | 53.043 |
| RMSEA | 0.065 | 0.069 | 0.071 | 0.032 | 0.055 | 0.040 |
| SRMR | 0.027 | 0.029 | 0.033 | 0.015 | 0.023 | 0.016 |
| GF1 | 0.993 | 0.992 | 0.992 | 0.998 | 0.995 | 0.997 |
| NFI | 0.947 | 0.962 | 0.958 | 0.988 | 0.978 | 0.988 |
| Factor loading | ||||||
| WC | 0.82 | 0.76 | 0.81 | 0.74 | 0.73 | 0.70 |
| FPG | 0.35 | 0.28 | 0.31 | 0.39 | 0.46 | 0.38 |
| Ln-TG | 0.52 | 0.49 | 0.42 | 0.44 | 0.50 | 0.50 |
| HDL-C | 0.40 | 0.36 | 0.38 | 0.35 | 0.38 | 0.41 |
| SBP | 0.41 | 0.35 | 0.24 | 0.38 | 0.37 | 0.36 |
| Sex-age Groups | Equation |
|---|---|
| Men | |
| 20–34 YRS | −10.6959 + 0.0844 × WC + 0.0119 × FPG + 0.3680 × Ln-TG − 0.0082 × HDL-C + 0.0121 × SBP |
| 35–49 YRS | −12.1104 + 0.0960 × WC + 0.0094 × FPG + 0.4556 × Ln-TG − 0.0097 × HDL-C + 0.0127 × SBP |
| 50–64 YRS | −11.3783 + 0.1089 × WC + 0.0073 × FPG + 0.2835 × Ln-TG − 0.0086 × HDL-C + 0.0055 × SBP |
| Women | |
| 20–34 YRS | −12.6514 + 0.1032 × WC + 0.0253 × FPG + 0.5074 × Ln-TG − 0.0100 × HDL-C + 0.0175 × SBP |
| 35–49 YRS | −12.3220 + 0.0972 × WC + 0.0246 × FPG + 0.5251 × Ln-TG − 0.0089 × HDL-C + 0.0131 × SBP |
| 50–64 YRS | −11.1397 + 0.0902 × WC + 0.0127 × FPG + 0.5491 × Ln-TG − 0.0093 × HDL-C + 0.0112 × SBP |
| Lifestyle Habit | MS | MS Severity Score | Total | ||
|---|---|---|---|---|---|
| n | % | Mean (SD) | Median | ||
| Smoking | |||||
| None | 1939 | 9.9% | −0.024 (0.974) | −0.079 | 19,590 |
| Second-hand smoke | 118 | 11.0% | 0.058 (1.126) | −0.044 | 1069 |
| Quit | 281 | 17.0% | 0.038 (0.970) | −0.011 | 1652 |
| Casual intake | 135 | 13.8% | 0.017 (1.003) | −0.032 | 978 |
| Daily intake | 641 | 18.3% | 0.080 (1.015) | 0.032 | 3495 |
| Missing data | 168 | 17.4% | 0.108 (1.301) | 0.038 | 964 |
| Drinking | |||||
| None | 2297 | 10.7% | −0.004 (0.987) | −0.066 | 21,384 |
| Quit | 67 | 13.3% | 0.027 (0.973) | 0.008 | 502 |
| 1–2 times/wk | 400 | 15.3% | −0.001 (0.982) | −0.039 | 2608 |
| 3–4 times/wk | 150 | 17.5% | −0.057 (1.002) | −0.068 | 858 |
| >4 times/wk | 58 | 19.1% | −0.026 (0.957) | −0.054 | 304 |
| Missing data | 310 | 14.8% | 0.082 (1.154) | 0.025 | 2092 |
| Chewing betel nut | |||||
| None | 2728 | 10.9% | −0.015 (0.981) | −0.067 | 25,105 |
| Quit | 24 | 40.7% | 0.166 (1.043) | 0.105 | 840 |
| 1–2 times/wk | 70 | 27.9% | 0.352 (1.199) | 0.341 | 251 |
| 3–4 times/wk | 194 | 23.1% | 0.567 (1.045) | 0.612 | 59 |
| >4 times/wk | 24 | 25.8% | 0.189 (0.978) | 0.026 | 93 |
| Missing data | 242 | 17.3% | 0.096(1.215) | 0.003 | 1400 |
| Sleeping (hrs/day) | |||||
| <4 | 45 | 13.8% | 0.082 (1.052) | −0.034 | 327 |
| 4.0–5.9 | 719 | 12.1% | 0.029 (1.010) | −0.034 | 5959 |
| 6.0–6.9 | 1592 | 12.0% | −0.012 (0.974) | −0.059 | 13,267 |
| 7.0–7.9 | 681 | 10.7% | −0.016 (0.985) | −0.063 | 6349 |
| ≥8 | 104 | 10.1% | −0.029 (1.004) | −0.113 | 1031 |
| Missing data | 141 | 17.3% | 0.165 (1.353) | 0.078 | 815 |
| Physical activity (level) | |||||
| None | 2311 | 11.9% | 0.030 (0.998) | −0.024 | 19,344 |
| Light | 588 | 11.1% | −0.069 (0.937) | −0.120 | 5313 |
| Moderate | 120 | 8.4% | −0.230 (0.897) | −0.259 | 1426 |
| Heavy | 42 | 11.6% | 0.039 (1.066) | −0.031 | 363 |
| Missing data | 221 | 17.0% | 0.109 (1.277) | 0.006 | 1302 |
| Physical activity (times/wk) | |||||
| None | 881 | 12.0% | −0.011 (1.038) | −0.080 | 7340 |
| 1 | 497 | 11.9% | −0.059 (0.950) | −0.086 | 4189 |
| 2–3 | 644 | 10.7% | −0.057 (0.960) | −0.104 | 6003 |
| 7 | 812 | 11.2% | 0.009 (1.016) | −0.054 | 7265 |
| >7 | 129 | 12.9% | 0.049 (0.978) | −0.011 | 997 |
| Missing data | 319 | 16.3% | 0.117 (1.187) | 0.027 | 1954 |
| Physical activity (hrs/day) | |||||
| <0.5 | 948 | 11.4% | 0.027 (0.993) | −0.031 | 8305 |
| 0.5–1 | 1162 | 11.4% | −0.006 (0.991) | −0.052 | 10,198 |
| 1–2 | 576 | 10.9% | −0.055 (0.964) | −0.118 | 5267 |
| >2 | 223 | 13.3% | −0.021 (0.959) | −0.053 | 1679 |
| Missing data | 373 | 16.2% | 0.093 (1.156) | −0.009 | 2299 |
| Vegetarian diet | |||||
| No | 3145 | 11.7% | −0.002 (0.989) | −0.057 | 26,804 |
| Yes | 98 | 12.8% | 0.043 (1.085) | −0.026 | 766 |
| Missing data | 39 | 21.9% | 0.389 (1.794) | 0.348 | 178 |
| Drinking sweetened beverages (cups/wk) | |||||
| None | 1236 | 12.2% | −0.023 (0.986) | −0.066 | 10,167 |
| 1–3 | 364 | 10.5% | 0.017 (0.991) | −0.043 | 3464 |
| 4–6 | 403 | 10.8% | 0.020 (0.942) | −0.031 | 3727 |
| 7 | 999 | 11.7% | −0.022 (0.969) | −0.070 | 8508 |
| >7 | 172 | 13.7% | 0.044 (1.150) | −0.069 | 1260 |
| Missing data | 108 | 17.4% | 0.142 (1.418) | 0.007 | 622 |
| Taking vitamin C supplements | |||||
| No | 2927 | 12.2% | 0.013 (1.004) | −0.042 | 23,983 |
| Yes | 355 | 9.4% | −0.073 (0.967) | −0.116 | 3765 |
| Taking vitamin E supplements | |||||
| No | 3096 | 11.9% | 0.006 (1.003) | −0.049 | 26,121 |
| Yes | 186 | 11.4% | −0.058 (0.951) | −0.105 | 1627 |
| Taking fish oil supplements | |||||
| No | 3063 | 11.7% | 0.001 (0.999) | −0.055 | 26,172 |
| Yes | 219 | 13.9% | 0.037 (1.010) | −0.019 | 1576 |
| Lifestyle Habit | Logistic Regression | Ordinal Regression | Linear Regression | |||
|---|---|---|---|---|---|---|
| AOR | p-Value | AOR | p-Value | β | p-Value | |
| Smoking (vs. None) | ||||||
| Second-hand smoke | 1.100 | 0.452 | 1.002 | 0.782 | 0.060 | 0.113 |
| Quit | 1.104 | 0.684 | 1.132 | 0.027 | 0.071 | 0.022 |
| Intake casually | 1.077 | 0.731 | 1.110 | 0.129 | 0.065 | 0.092 |
| Intake everyday | 1.136 | 0.505 | 1.112 | 0.019 | 0.068 | 0.007 |
| Drink (vs. None) | ||||||
| Quit | 0.819 | 0.228 | 0.832 | 0.062 | −0.122 | 0.027 |
| 1–2 times/wk | 0.951 | 0.502 | 0.914 | 0.045 | −0.048 | 0.053 |
| 3–4 times/wk | 0.956 | 0.757 | 0.830 | 0.013 | −0.134 | 0.001 |
| >4 times/wk | 0.854 | 0.414 | 0.752 | 0.023 | −0.191 | 0.008 |
| Chewing betel nut (vs. None) | ||||||
| Quit | 1.272 | 0.033 | 1.106 | 0.213 | −0.163 | 0.250 |
| 1–2 times/wk | 1.859 | 0.001 | 1.561 | 0.002 | 0.083 | 0.061 |
| 3–4 times/wk | 2.973 | 0.004 | 3.216 | 0.001 | 0.122 | 0.437 |
| >4 times/wk | 1.060 | 0.869 | 1.375 | 0.208 | 0.323 | 0.165 |
| Sleep (vs. ≥8hrs/day) | ||||||
| <4hrs/day | 1.034 | 0.888 | 1.141 | 0.348 | 0.025 | 0.761 |
| 4.0–5.9 hrs/day | 0.959 | 0.759 | 1.108 | 0.153 | 0.027 | 0.692 |
| 6.0–6.9 hrs/day | 0.982 | 0.891 | 1.107 | 0.325 | 0.038 | 0.114 |
| 7.0–7.9 hrs/day | 0.896 | 0.416 | 1.105 | 0.491 | −0.014 | 0.672 |
| Physical activity level (vs. None) | ||||||
| Light | 0.792 | <0.001 | 0.837 | <0.001 | −0.088 | <0.001 |
| Moderate | 0.572 | <0.001 | 0.653 | <0.001 | −0.236 | <0.001 |
| Heavy | 0.669 | 0.251 | 0.742 | 0.066 | −0.221 | 0.016 |
| Physical activity frequency (vs. None) | ||||||
| 1 time/wk | 0.793 | 0.075 | 0.935 | 0.366 | −0.003 | 0.873 |
| 2–3 times/wk | 0.853 | 0.210 | 0.876 | 0.003 | −0.038 | 0.091 |
| 7 times/wk | 0.899 | 0.395 | 0.940 | 0.125 | −0.085 | 0.001 |
| >7 times/wk | 0.977 | 0.853 | 0.988 | 0.744 | −0.055 | 0.178 |
| Physical activity duration (vs. <0.5 hrs/day) | ||||||
| 0.5–1 hrs/day | 1.044 | 0.491 | 1.027 | 0.439 | 0.024 | 0.453 |
| 1–2 hrs/day | 0.966 | 0.649 | 0.914 | 0.355 | 0.038 | 0.347 |
| >2 hrs/day | 0.935 | 0.511 | 0.943 | 0.317 | −0.014 | 0.490 |
| Vegetarian diet (vs. No) | ||||||
| Yes | 1.003 | 0.983 | 0.989 | 0.889 | −0.007 | 0.800 |
| Drinking sweetened beverages (vs. None) | ||||||
| 1–3 cups/wk | 1.115 | 0.057 | 1.024 | 0.450 | 0.038 | 0.032 |
| 4–6 cups/wk | 1.004 | 0.961 | 1.060 | 0.150 | 0.032 | 0.146 |
| 7 cups/wk | 0.983 | 0.822 | 0.984 | 0.704 | −0.006 | 0.780 |
| >7 cups/wk | 1.080 | 0.479 | 0.985 | 0.813 | 0.052 | 0.037 |
| Taking vitamin C supplements (vs. No) | ||||||
| Yes | 0.849 | 0.036 | 0.883 | 0.001 | −0.067 | 0.002 |
| Taking vitamin E supplements (vs. No) | ||||||
| Yes | 1.046 | 0.671 | 0.945 | 0.332 | −0.039 | 0.225 |
| Taking fish oil supplements (vs. No) | ||||||
| Yes | 1.204 | 0.048 | 1.095 | 0.110 | 0.071 | 0.022 |
© 2020 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lin, C.-M. An Application of Metabolic Syndrome Severity Scores in the Lifestyle Risk Assessment of Taiwanese Adults. Int. J. Environ. Res. Public Health 2020, 17, 3348. https://doi.org/10.3390/ijerph17103348
Lin C-M. An Application of Metabolic Syndrome Severity Scores in the Lifestyle Risk Assessment of Taiwanese Adults. International Journal of Environmental Research and Public Health. 2020; 17(10):3348. https://doi.org/10.3390/ijerph17103348
Chicago/Turabian StyleLin, Chih-Ming. 2020. "An Application of Metabolic Syndrome Severity Scores in the Lifestyle Risk Assessment of Taiwanese Adults" International Journal of Environmental Research and Public Health 17, no. 10: 3348. https://doi.org/10.3390/ijerph17103348
APA StyleLin, C.-M. (2020). An Application of Metabolic Syndrome Severity Scores in the Lifestyle Risk Assessment of Taiwanese Adults. International Journal of Environmental Research and Public Health, 17(10), 3348. https://doi.org/10.3390/ijerph17103348





