Challenges in Infection Epidemiology: On the Underreporting of Norovirus Gastroenteritis Cases in Germany
Abstract
1. Introduction
2. Methods
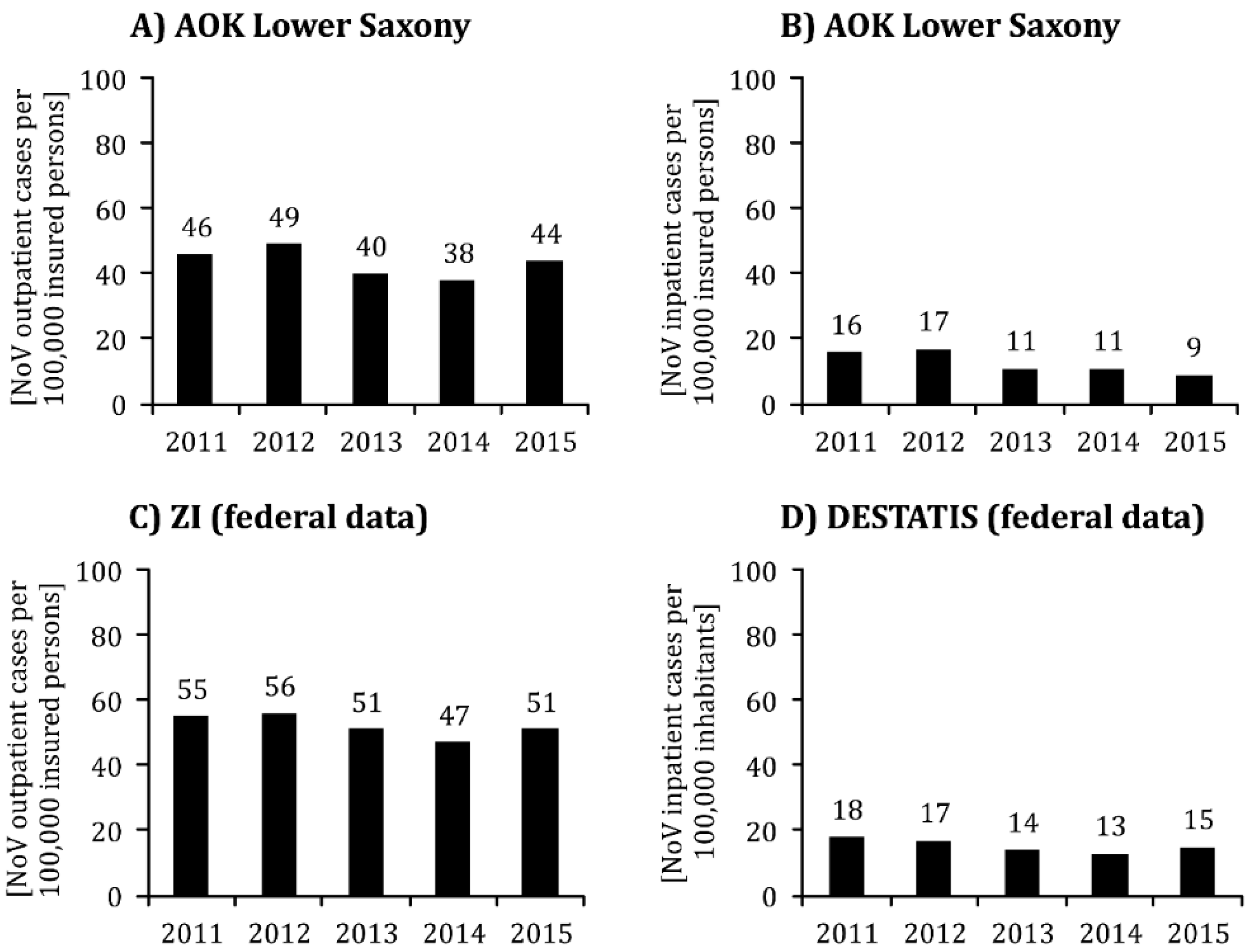
- Billing information data of persons aged 18 to 65 insured through the statutory health insurance ‘Allgemeine Ortskrankenkasse’ in the federal state of Lower Saxony (AOK) whose outpatient or inpatient treatment was coded as ICD10 number A08.1. As the demographic structure (age and gender) of the population insured through the AOK hardly differed from the demographic structure of the population of Lower Saxony as a whole [22], the calculated incidences could be compared with data from the following three sources.
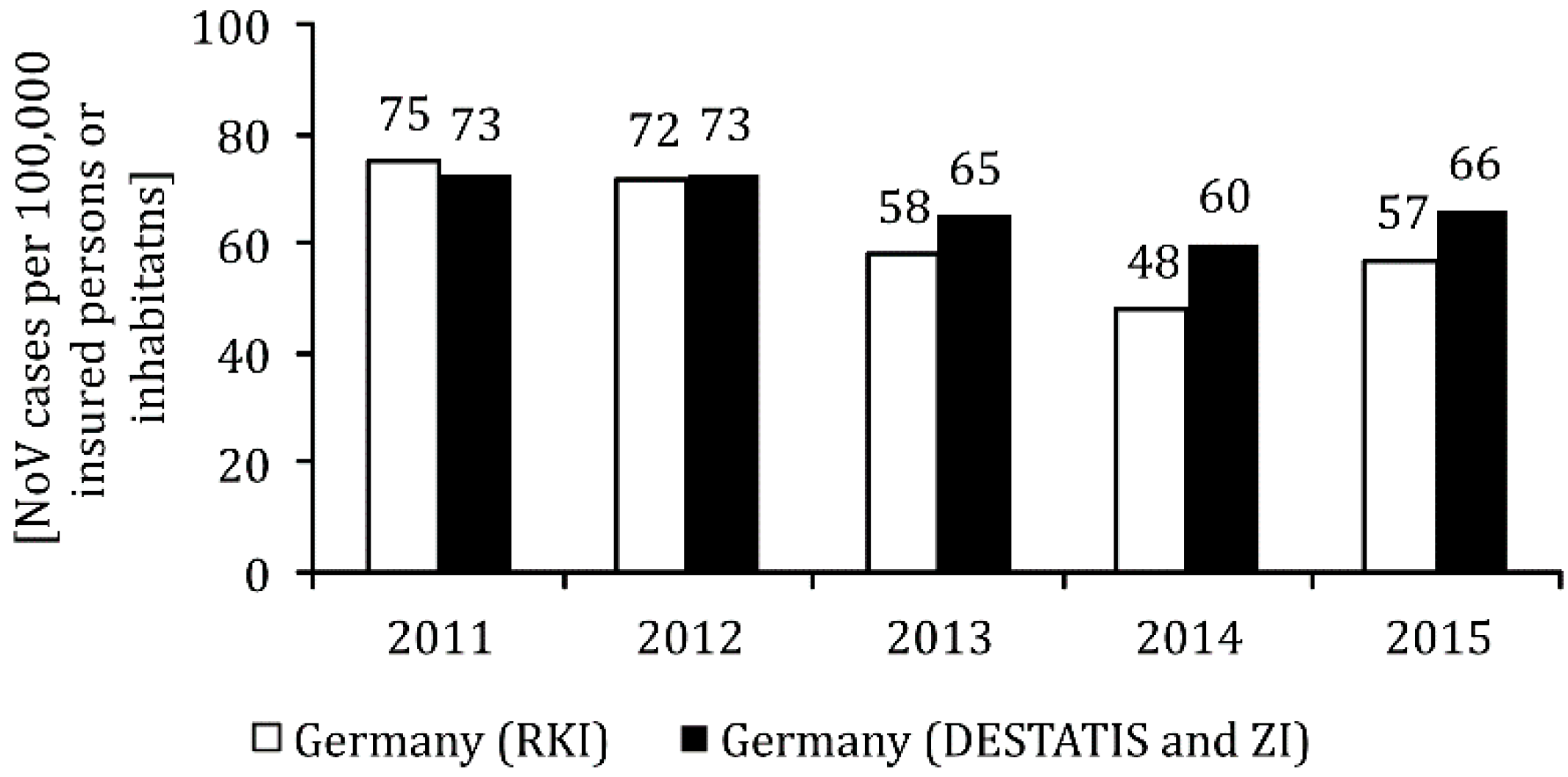
- Billing information data from the Central Institute for Statutory Health Insurance Physician Care (Zentralinstitut für die Kassenärztliche Versorgung; ZI) for all outpatients treated in Germany with statutory health insurance given the diagnosis A08.1. The data for the age group 20–64 years were analyzed to achieve approximate comparability with the incidence of outpatient diagnosis A08.1 reported in the billing data from the AOK.
- Treatment data on the diagnoses of hospital patients according to the four-digit code of the International Classification of Diseases (ICD, version 10) A08.1 [23,24] kept at the German Federal Statistical Office (Deutsches Statistisches Bundesamt; DESTATIS). According to the definition of the Federal Statistical Office given in the datasets [23,24], hospital cases with several flat-rate case diagnoses were subsumed under the ICD diagnosis that was primarily responsible for inpatient treatment and was considered the discharge diagnosis. For this reason, nosocomial cases are not explicitly reported in the case figures of the Federal Statistical Office. Here, too, the data of 20–64-year-olds were aggregated for comparison purposes.
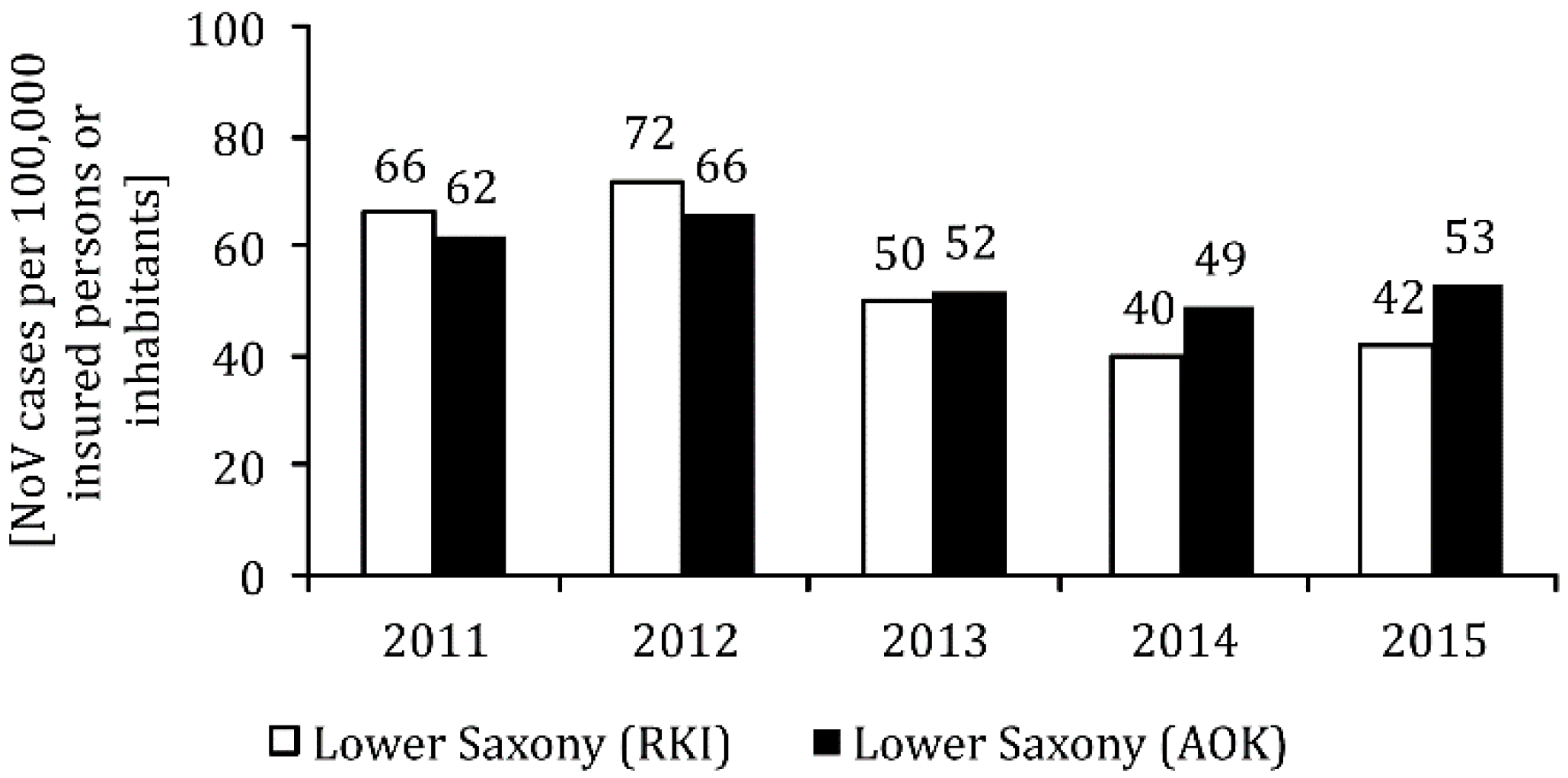
- NoV reporting data from the Robert Koch Institute according to the reference definition ‘clinical laboratory diagnostic’ for Lower Saxony, as well as the entire federal territory of Germany from the Internet portal SurvStat@RKI 2.0 [7].
3. Results
3.1. NoV Diagnoses in the Routine Data of the AOK in Lower Saxony
3.2. Accounting Data of the Central Institute for Statutory Health Insurance Physician Care (ZI)
3.3. Hospital Billing Information Data of the German Federal Statistical Office (DESTATIS)
3.4. Reporting Data of the Robert Koch-Institute
3.5. Reporting Data of the Robert Koch-Institute
4. Discussion
- It is possible that the hospital stay of a patient was billed with the main diagnosis A08.1, although the outpatient diagnosis A08.1 had already been made for this patient in advance. Thus, this patient was included in the ZI and DESTATIS data as both an outpatient and an inpatient case, whereas it was not entered more than once in the RKI database. This effect, with an artificial increase in NoV incidence, must also be taken into account when interpreting the insured person data of the AOK. On the other hand, the DESTATIS data for the years 2011 to 2015 did not include any nosocomial NoV cases, which is why the actual number of NoV cases in German hospitals may have been higher than suggested by the DESTATIS data. To what extent these contradictory effects have led to a reduction in data quality that cannot be answered here. Irrespective of this, it can be stated that different case definitions or a lack of harmonization of the secondary data we are looking to represent a limitation of our study. A further limitation is that the ZI/DESTATIS data is only available nationwide and a direct comparison between these and AOK data of a federal state is not possible. As can already be seen in the RKI statistics, reporting compliance in the eastern German states is higher than in most western German states, and thus influences the incidence rates [15].
- The discrepancy may indicate that NoV cases were not recorded in the register of residents of the RKI during the last two years of observation among patients treated by SHI physicians, which would constitute a violation of the reporting obligation under §7(1) No. 36 IfSG. To what extent this effect plays a role cannot be clarified without further studies.
- Furthermore, insufficient coding quality on the part of general practitioners (GP) is possible [10]. It is conceivable, for example, that the treatment of possible NoV cases was invoiced with the ICD10 diagnosis A08.1, although no reliable laboratory evidence was available. According to §7(1) No. 36 IfSG, laboratories must notify the responsible health authority of every person for whom an NoV-positive stool sample is available by patient name [3]. This notification is then forwarded by the health authorities to the competent state authority, which finally reports these figures to the RKI [8]. According to personal reports from individual representatives of the Public Health Service (7.2. and 19.2.2019), however, NoV cases are not reported by the laboratories only in exceptional cases. Accordingly, the NoV case numbers reported by the laboratories should be regarded as resilient.
- a subjectively different experience of NoV symptoms may lead affected persons, whose infections are not confirmed in the context of an outbreak, to seek help from a doctor to varying degrees or (partly contrary to the official recommendations) stay away from work for varying lengths of time [10];
- a varying diagnostic behavior of doctors, on the other hand, and thus a varying degree of willingness to arrange for an appropriate laboratory test if relevant symptoms are present. If physicians estimate the burden of NoV patients as low due to the temporary character of the disease, whereby a larger number of potential NoV cases may then be accounted for with the ICD10 diagnosis A08.4 ‘Virus-induced intestinal infection, not specified in more detail’ [10];
- a varying capacity of local health authorities to press for laboratory diagnostic evidence to clarify the causative agent of infection in the event of outbreaks of gastroenteritis in community establishments [10]. In this context, we have unpublished data on gastroenteritis outbreaks in the catchment area of two health authorities. With the exception of outbreaks in hospitals and nursing homes for the elderly, insufficient laboratory diagnostic evidence was available from community institutions, especially day-care centers. However, as these are only two case studies, this trend cannot be generalized.
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Niendorf, S.; Jacobsen, S.; Faber, M. Increase of norovirus infections in winter season 2016/2017. [Vermehrter Anstieg der Norovirus-Infektionen in der Winter-Saison 2016/2017]. Epid. Bull. 2017, 7, 67–70. [Google Scholar] [CrossRef]
- Pringle, K.; Lopman, B.; Vega, E.; Vinje, J.; Parashar, U.D.; Hall, A.J. Noroviruses: Epidemiology, immunity and prospects for prevention. Future Microbiol. 2015, 10, 53–67. [Google Scholar] [CrossRef]
- Robert Koch-Institut. Norovirus Gastroenteritis. [Norovirus Gastroenteritis: RKI-Ratgeber (26.07.2008)]. Available online: https://www.rki.de/DE/Content/Infekt/EpidBull/Merkblaetter/Ratgeber_Noroviren.html;jsessionid=E426AA0DCB8F17DF505D090BB36CC2F6.2_cid290#doc2374562bodyText16 (accessed on 21 August 2019).
- Schwartz, S.; Vergoulidou, M.; Schreier, E.; Loddenkemper, C.; Reinwald, M.; Schmidt-Hieber, M.; Flegel, W.A.; Thiel, E.; Schneider, T. Norovirus gastroenteritis causes severe and lethal complications after chemotherapy and hematopoietic stem cell transplantation. Blood 2011, 117, 5850–5856. [Google Scholar] [CrossRef]
- Lindsay, L.; Wolter, J.; De Coster, I.; Van Damme, P.; Verstraeten, T. A decade of norovirus disease risk among older adults in upper-middle and high income countries: A systematic review. BMC Infect. Dis. 2015, 15, 425. [Google Scholar] [CrossRef]
- Riera-Montes, M.; O’Ryan, M.; Verstraeten, T. Norovirus and rotavirus disease severity in children: Systematic review and meta-analysis. Pediatr. Infect. Dis. J. 2018, 37, 501–505. [Google Scholar] [CrossRef] [PubMed]
- Robert Koch-Institut. SurvStat@RKI 2.0. Web-Based Query of Reporting Data According to Infection Protection Law. [Web-Basierte Abfrage der Meldedaten Gemäß Infektionsschutzgesetz (IfSG)]. Available online: https://survstat.rki.de (accessed on 10 January 2019).
- Hauri, A.M.; Westbrock, H.J.; Claus, H.; Geis, S.; Giernat, S.; Forssbohm, M.; Uphoff, H. Electronic outbreak surveillance in Germany: A first evaluation for nosocomial norovirus outbreaks. PLoS ONE 2011, 6, e17341. [Google Scholar] [CrossRef] [PubMed]
- Bernard, H.; Werber, D.; Höhle, M. Estimating the under-reporting of norovirus illness in Germany utilizing enhanced awareness of diarrhoea during a large outbreak of Shiga toxin-producing E. coli O104:H4 in 2011—A time series analysis. BMC Infect. Dis. 2014, 14, 116. [Google Scholar] [CrossRef] [PubMed]
- Hofmann, F.; Michaelis, M.; Stößel, U. Norovirus gastroenteritis—An underestimated infectious disease? Considerations on the quality of institutional data. [Norovirus-Gastroenteritis—Eine unterschätzte Infektionskrankheit? Überlegungen zur Qualität institutioneller Daten]. In Arbeitsmedizin im Gesundheitsdienst; Tagungsband 30 des Freiburger Symposiums Arbeitsmedizin im Gesundheitsdienst; Hofmann, F., Reschauer, G., Stößel, U., Eds.; FFAS: Freiburg, Germany, 2017; pp. 118–130. [Google Scholar]
- Robert Koch-Institut. Revised case definitions for the transmission of evidence of dengue virus and norovirus and cases of disease or death to dengue fever and norovirus gastroenteritis. [Überarbeitete Falldefinitionen zur Übermittlung von Nachweisen von Denguevirus und Norovirus und Erkrankungs-oder Todesfällen an Denguefieber und an Norovirus-Gastroenteritis]. Bundesgesundheitsbl. Gesundh. Gesundh. 2011, 54, 246–250. [Google Scholar] [CrossRef]
- Diercke, M.; Benzler, J.; Schöneberg, I.; Mücke, I.; Altmann, D.; Claus, H.; Gilsdorf, A.; Mitarbeiter der Abteilung für Infektionsepidemiologie. Case definitions for the surveillance of notifiable infectious diseases in Germany. [Falldefinitionen für die Surveillance meldepflichtiger Infektionskrankheiten in Deutschland, Ausgabe 2015]. Bundesgesundheitsbl. Gesundheitsforsch. Gesundheitsschutz 2014, 57, 1107–1110. [Google Scholar] [CrossRef][Green Version]
- Public Health England. Hospital Norovirus Outbreak Reporting System. User Guidance. Available online: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/836362/Hospital_Norovirus_Outbreak_Reporting_System_User_Guide.pdf (accessed on 29 November 2019).
- Edelstein, M.; Wallensten, A.; Zetterquist, I.; Hulth, A. Detecting the norovirus season in Sweden using search engine data—Meeting the needs of hospital infection control teams. PLoS ONE 2014, 9, e100309. [Google Scholar] [CrossRef]
- Robert Koch-Institut. Epidemiological Yearbook of Notifiable Infectious Diseases for 2017. [Infektionsepidemiologisches Jahrbuch Meldepflichtiger Krankheiten für 2017]. Available online: https://www.rki.de/DE/Content/Infekt/Jahrbuch/Jahrbuch_2017.pdf?__blob=publicationFile (accessed on 28 November 2018).
- Zingg, W.; Colombo, C.; Jucker, T.; Bossart, W.; Ruef, C. Impact of an outbreak of norovirus infection on hospital resources. Infect. Control. Hosp. Epidemiol. 2005, 26, 263–267. [Google Scholar] [CrossRef] [PubMed]
- Johnston, C.P.; Qiu, H.; Ticehurst, J.R.; Dickson, C.; Rosenbaum, P.; Lawson, P.; Stokes, A.B.; Lowenstein, C.J.; Kaminsky, M.; Cosgrove, S.E.; et al. Outbreak Management and Implications of a Nosocomial Norovirus Outbreak. Clin. Infect. Dis. 2007, 45, 534–540. [Google Scholar] [CrossRef] [PubMed]
- Hofmann, F.; Michaelis, M.; Nübling, M.; Stößel, U. Norovirus gastroenteritis: How high is the number of unreported cases? Study design of a method mix study. [Norovirus-Gastroenteritis: Wie hoch ist die Dunkelziffer? Studiendesign einer Methodenmix-Studie] (P166). In Proceedings of the 56th Scientific Annual Meeting of the German Society for Occupational and Environmental Medicine (DGAUM), München, Germany, 9–11 March 2016. [Google Scholar]
- Michaelis, M.; Hofmann, F.M.; Stößel, U.; Hofmann, F. Norovirus outbreaks and cooperation between occupational health physicians and hygiene personnel in hospitals. Results of a survey among congress participants. [Norovirusausbrüche und Kooperation zwischen Hygienepersonal und Betriebsärzten im Krankenhaus. Ergebnisse einer Umfrage bei Kongressteilnehmern]. Zent. Arb. Arb. Ergon. 2017, 67, 309–313. [Google Scholar] [CrossRef]
- Michaelis, M.; Olawumi, E.; Stößel, U.; Hofmann, F.; Schulz-Stübner, S. Cooperation with company doctors duringnorovirus outbreaks in hospitals at the interfaces of occupational safety and patient safety. Results of a survey of hygiene specialists. [Kooperation mit Betriebsärzten bei Norovirusausbrüchen im Krankenhaus an den Schnittstellen des Arbeits-und Patientenschutzes. Ergebnisse einer Umfrage von Hygienefachpersonal]. Umweltmed. Hyg. Arbeitsmed. 2019, 24, 119–126. [Google Scholar]
- Swart, E.; Bitzer, E.; Gothe, H.; Harling, M.; Hoffmann, F.; Horenkamp-Sonntag, D.; Maier, B.; March, S.; Petzold, T.; Röhrig, R.; et al. Standardized reporting routine for secondary data analysis (STROSA)—A consensus reporting standard for Germany. [Publication in German: STandardisierte BerichtsROutine für Sekundärdaten Analysen (STROSA)—Ein konsentierter Berichtsstandard für Deutschland, Version 2]. Das Gesundh. 2016, 78, e145–e160. [Google Scholar] [CrossRef]
- Jaunzeme, J.; Eberhard, S.; Geyer, S. How ‘representative’ are the data from statutory health insurances? [Wie ‘repräsentativ’ sind GKV-Daten?]. Bundesgesundheitsbl. Gesundh. Gesundh. 2013, 56, 447–454. [Google Scholar] [CrossRef]
- Statistisches Bundesamt. In-Depth Diagnostic Data of Hospital Patients (Data Record Structure). [Tiefgegliederte Diagnosedaten der Krankenhauspatientinnen und-Patienten (Datensatzstruktur—Ältere Ausgaben 2019]. Available online: https://www.destatis.de/DE/Publikationen/Thematisch/Gesundheit/AlteAusgaben/TiefgegliederteDiagnosedatenAlt.html (accessed on 15 February 2019).
- Statistische Ämter des Bundes und der Länder. In-Depth Diagnostic Data of Hospital Patients 2019. [Gesundheit/Tiefgegliederte Diagnosedaten der Krankenhauspatientinnen und-Patienten]. Available online: https://www.destatis.de/GPStatistik/receive/DESerie_serie_00000950 (accessed on 15 February 2019).
- Stößel, U.; Michaelis, M.; Olawumi, E.; Hofmann, F. Norovirus gastroenteritis—A significant infectious disease in occupational health? [Norovirus-Gastroenteritis—Eine arbeitsmedizinisch bedeutsame Infektionskrankheit?]. In Arbeitsmedizin im Gesundheitsdienst: Tagungsband 31 des Freiburger Symposiums Arbeitsmedizin im Gesundheitsdienst; Hofmann, F., Reschauer, G., Stößel, U., Eds.; FFAS: Freiburg, Germany, 2018; pp. 114–124. [Google Scholar]
- Bernard, H.; Faber, M.; Wilking, H.; Haller, S.; Höhle, M.; Schielke, A.; Ducomble, T.; Siffczyk, C.; Merbecks, S.S.; Fricke, G.; et al. Large multistate outbreak of norovirus gastroenteritis associated with frozen strawberries, Germany, 2012. Euro Surveill 2014, 19, 20719. [Google Scholar] [CrossRef][Green Version]
- Niedersächsisches Landesgesundheitsamt. Noroviruses—Review of the 2012/2013 Season. [Noroviren—Rückblick auf die Saison 2012/2013]. Available online: https://www.nlga.niedersachsen.de/download/78607 (accessed on 21 August 2019).
- Ebner, W.; Meyer, E. Noroviren. Krankenh. Up2date 2007, 2, 9–19. [Google Scholar] [CrossRef]
- Schimmelpfennig, M.; Walter-Dohmes, M.; Aue, T.; Gesundheitsamt, K.; Uphoff, H.; Fitzenberger, J.; Hauri, A.M. Noroviruses: A food-borne outbreak among visitors to a public canteen. [Noroviren: Zu einem lebensmittelbedingten Ausbruch unter Besuchern einer öffentlichen Kantine]. Epidemiol. Bull. 2009, 9, 80–81. Available online: https://www.rki.de/DE/Content/Infekt/EpidBull/Archiv/2009/09/Art_02.html (accessed on 21 August 2019).
- Michaelis, M.; Olawumi, E.; Stößel, U.; Hofmann, F. Norovirus gastroenteritis in nursing care. [Norovirus-Gastroenteritis in der Pflege]. Schwest. Pfleg. 2018, 57, 60–63. [Google Scholar]
- Schmutz, C.; Bless, P.J.; Mäusezahl, D.; Jost, M.; Mäusezahl-Feuz, M.; Swiss Sentinel Surveillance Network. Acute gastroenteritis in primary care: A longitudinal study in the Swiss Sentinel Surveillance Network, Sentinella. Infection 2017, 45, 811–824. [Google Scholar] [CrossRef] [PubMed]
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hofmann, F.M.; Olawumi, E.; Michaelis, M.; Hofmann, F.; Stößel, U. Challenges in Infection Epidemiology: On the Underreporting of Norovirus Gastroenteritis Cases in Germany. Int. J. Environ. Res. Public Health 2020, 17, 314. https://doi.org/10.3390/ijerph17010314
Hofmann FM, Olawumi E, Michaelis M, Hofmann F, Stößel U. Challenges in Infection Epidemiology: On the Underreporting of Norovirus Gastroenteritis Cases in Germany. International Journal of Environmental Research and Public Health. 2020; 17(1):314. https://doi.org/10.3390/ijerph17010314
Chicago/Turabian StyleHofmann, Felix Martin, Edward Olawumi, Martina Michaelis, Friedrich Hofmann, and Ulrich Stößel. 2020. "Challenges in Infection Epidemiology: On the Underreporting of Norovirus Gastroenteritis Cases in Germany" International Journal of Environmental Research and Public Health 17, no. 1: 314. https://doi.org/10.3390/ijerph17010314
APA StyleHofmann, F. M., Olawumi, E., Michaelis, M., Hofmann, F., & Stößel, U. (2020). Challenges in Infection Epidemiology: On the Underreporting of Norovirus Gastroenteritis Cases in Germany. International Journal of Environmental Research and Public Health, 17(1), 314. https://doi.org/10.3390/ijerph17010314




