Acute Myocardial Infarction Mortality Rates and Trends in Romania between 1994 and 2017
Abstract
1. Introduction
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
Appendix A
| Year | Women Crude Mortality Rates Per 100,000 Person-Years, by Age Group (Years) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 40–44 | 45–49 | 50–54 | 55–59 | 60–64 | 65–69 | 70–74 | 75–79 | 80–84 | ≥85 | |
| 1994 | 16.8 | 30.3 | 47.5 | 70.5 | 110.2 | 170.3 | 256.9 | 388.4 | 477.3 | 794.8 |
| 1995 | 16.6 | 27.8 | 48.1 | 70.7 | 116.9 | 189.9 | 268.1 | 382.4 | 520.0 | 828.6 |
| 1996 | 18.1 | 32.5 | 54.8 | 76.2 | 126.8 | 181.9 | 267.5 | 411.2 | 618.7 | 984.5 |
| 1997 | 17.1 | 32.5 | 48.7 | 81.0 | 120.3 | 200.0 | 266.4 | 383.5 | 610.7 | 923.3 |
| 1998 | 17.3 | 31.5 | 47.2 | 82.3 | 125.0 | 185.8 | 293.7 | 443.6 | 631.8 | 1029.8 |
| 1999 | 14.5 | 24.1 | 46.9 | 73.6 | 113.5 | 187.0 | 281.4 | 444.0 | 652.0 | 1023.7 |
| 2000 | 14.2 | 22.5 | 38.1 | 71.7 | 110.2 | 165.3 | 260.9 | 398.7 | 578.5 | 1050.2 |
| 2001 | 15.7 | 26.7 | 47.0 | 69.3 | 110.6 | 176.6 | 267.7 | 406.0 | 615.3 | 1027.9 |
| 2002 | 12.9 | 26.9 | 44.3 | 76.4 | 119.5 | 184.2 | 290.4 | 436.8 | 697.8 | 1217.2 |
| 2003 | 15.8 | 25.1 | 38.4 | 76.9 | 109.7 | 170.5 | 284.7 | 421.7 | 619.6 | 1172.8 |
| 2004 | 14.9 | 24.4 | 38.2 | 65.4 | 110.4 | 181.3 | 294.6 | 447.6 | 660.6 | 1344.6 |
| 2005 | 11.5 | 21.4 | 41.4 | 64.8 | 115.9 | 172.0 | 283.6 | 468.4 | 706.8 | 1251.2 |
| 2006 | 10.6 | 21.0 | 38.4 | 64.5 | 101.8 | 169.6 | 284.7 | 439.0 | 661.2 | 1251.3 |
| 2007 | 10.5 | 21.3 | 31.3 | 67.0 | 97.3 | 163.9 | 257.5 | 449.5 | 676.1 | 1249.2 |
| 2008 | 8.4 | 20.1 | 31.8 | 57.0 | 93.8 | 151.1 | 262.6 | 426.4 | 654.1 | 1210.7 |
| 2009 | 9.0 | 18.3 | 30.5 | 57.5 | 96.4 | 146.3 | 245.9 | 407.3 | 608.2 | 1195.1 |
| 2010 | 10.2 | 16.4 | 30.1 | 44.9 | 83.6 | 141.4 | 246.1 | 396.6 | 633.5 | 1199.9 |
| 2011 | 8.6 | 16.7 | 24.4 | 45.1 | 77.3 | 122.7 | 217.5 | 361.5 | 592.7 | 1083.1 |
| 2012 | 6.0 | 14.4 | 24.3 | 42.2 | 73.6 | 121.6 | 203.8 | 366.3 | 593.0 | 1096.3 |
| 2013 | 7.7 | 9.0 | 27.2 | 42.7 | 73.5 | 118.2 | 207.5 | 337.5 | 568.5 | 1040.4 |
| 2014 | 5.6 | 13.0 | 23.7 | 41.5 | 70.7 | 114.6 | 197.9 | 327.1 | 595.0 | 1049.7 |
| 2015 | 7.4 | 12.0 | 22.9 | 43.7 | 72.0 | 119.3 | 203.3 | 345.4 | 598.8 | 1179.8 |
| 2016 | 6.0 | 10.3 | 18.8 | 39.8 | 63.8 | 111.3 | 181.4 | 311.9 | 540.6 | 977.1 |
| 2017 | 6.1 | 9.6 | 24.2 | 37.7 | 66.6 | 107.1 | 173.4 | 297.9 | 537.0 | 948.7 |
| Year | Men Crude Mortality Rates Per 100,000 Person-Years, by Age Group (Years) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 40–44 | 45–49 | 50–54 | 55–59 | 60–64 | 65–69 | 70–74 | 75–79 | 80–84 | ≥85 | |
| 1994 | 91.5 | 134.5 | 214.9 | 261.0 | 340.0 | 429.4 | 532.3 | 595.3 | 774.3 | 1012.3 |
| 1995 | 88.6 | 136.0 | 211.1 | 272.9 | 342.0 | 427.7 | 541.3 | 661.7 | 811.4 | 1085.3 |
| 1996 | 87.0 | 150.1 | 214.7 | 279.7 | 359.1 | 433.0 | 556.6 | 699.2 | 882.0 | 1170.7 |
| 1997 | 94.7 | 141.9 | 207.4 | 277.0 | 364.5 | 455.9 | 566.0 | 707.2 | 828.1 | 1174.8 |
| 1998 | 80.1 | 129.8 | 196.4 | 268.2 | 335.7 | 430.7 | 547.2 | 691.3 | 935.0 | 1152.4 |
| 1999 | 70.8 | 123.2 | 177.1 | 233.8 | 321.5 | 424.9 | 540.5 | 675.0 | 898.0 | 1319.9 |
| 2000 | 68.3 | 108.4 | 163.8 | 232.8 | 310.2 | 384.9 | 496.1 | 649.1 | 764.2 | 1137.9 |
| 2001 | 61.8 | 114.7 | 165.8 | 245.2 | 332.4 | 405.2 | 521.9 | 676.2 | 767.2 | 1253.3 |
| 2002 | 68.5 | 118.8 | 175.5 | 238.8 | 320.6 | 425.0 | 554.1 | 731.1 | 905.2 | 1453.3 |
| 2003 | 64.1 | 110.4 | 170.5 | 245.3 | 336.0 | 424.7 | 545.2 | 685.6 | 875.8 | 1030.6 |
| 2004 | 63.8 | 105.3 | 171.8 | 240.0 | 319.7 | 435.9 | 534.6 | 718.6 | 948.0 | 1105.6 |
| 2005 | 52.5 | 110.5 | 159.3 | 232.8 | 315.6 | 435.6 | 549.1 | 722.5 | 963.4 | 1252.9 |
| 2006 | 54.8 | 98.0 | 161.5 | 225.9 | 318.8 | 411.0 | 521.4 | 720.0 | 1003.0 | 1199.8 |
| 2007 | 46.3 | 94.3 | 154.7 | 221.4 | 312.5 | 384.9 | 511.3 | 719.1 | 962.9 | 1112.4 |
| 2008 | 40.2 | 87.9 | 157.6 | 217.3 | 286.5 | 369.2 | 514.4 | 673.3 | 863.4 | 1099.4 |
| 2009 | 39.7 | 85.6 | 142.1 | 201.0 | 284.9 | 365.1 | 499.5 | 650.1 | 876.7 | 1062.3 |
| 2010 | 39.3 | 84.5 | 132.3 | 198.4 | 273.2 | 369.7 | 483.0 | 652.5 | 959.9 | 1142.9 |
| 2011 | 35.7 | 69.4 | 127.2 | 184.8 | 265.2 | 316.0 | 458.6 | 597.1 | 876.5 | 1031.0 |
| 2012 | 36.7 | 67.2 | 116.8 | 179.5 | 241.5 | 324.5 | 400.6 | 555.6 | 836.3 | 1291.0 |
| 2013 | 32.0 | 61.9 | 108.1 | 170.3 | 237.6 | 315.2 | 413.3 | 558.7 | 801.0 | 1249.1 |
| 2014 | 28.4 | 59.5 | 110.1 | 173.2 | 236.4 | 309.3 | 411.6 | 576.3 | 806.9 | 1293.6 |
| 2015 | 30.5 | 55.0 | 103.3 | 162.9 | 245.3 | 315.2 | 427.8 | 617.4 | 840.6 | 1286.2 |
| 2016 | 28.7 | 52.1 | 104.6 | 156.0 | 218.1 | 304.1 | 402.1 | 554.8 | 760.9 | 1160.2 |
| 2017 | 25.5 | 54.5 | 104.2 | 155.4 | 228.5 | 314.0 | 396.7 | 523.78 | 736.39 | 1156.8 |
| Year | Women | Men | Total | |||
|---|---|---|---|---|---|---|
| N a | CMR b | Na | CMR b | N a | CMR b | |
| 1994 | 6684 | 57.75 | 13,216 | 118.5 | 19,900 | 87.5 |
| 1995 | 7116 | 61.6 | 13,555 | 121.9 | 20,671 | 91.1 |
| 1996 | 7737 | 67.1 | 14,108 | 127.3 | 21,845 | 96.6 |
| 1997 | 7730 | 67.2 | 14,313 | 129.6 | 22,043 | 97.8 |
| 1998 | 8211 | 71.5 | 13,651 | 124.0 | 21,862 | 97.2 |
| 1999 | 8038 | 70.1 | 13,153 | 119.7 | 21,191 | 94.4 |
| 2000 | 7600 | 66.3 | 12,365 | 112.7 | 19,965 | 89.0 |
| 2001 | 8025 | 70.0 | 13,022 | 118.9 | 21,047 | 93.9 |
| 2002 | 8670 | 78.0 | 13,482 | 127.6 | 22,152 | 102.2 |
| 2003 | 8370 | 75.3 | 13,336 | 126.8 | 21,706 | 100.4 |
| 2004 | 8831 | 79.9 | 13,515 | 129.1 | 22,346 | 103.8 |
| 2005 | 9008 | 82.0 | 13,618 | 130.9 | 22,626 | 105.8 |
| 2006 | 9161 | 83.9 | 13,461 | 130.1 | 22,622 | 106.4 |
| 2007 | 8871 | 81.8 | 13,131 | 127.7 | 22,002 | 104.1 |
| 2008 | 8760 | 82.4 | 12,782 | 127.7 | 21,542 | 104.4 |
| 2009 | 8621 | 81.9 | 12,499 | 126.1 | 21,120 | 103.3 |
| 2010 | 8675 | 83.0 | 12,638 | 128.5 | 21,313 | 105.0 |
| 2011 | 8111 | 78.5 | 11,770 | 120.2 | 19,881 | 98.8 |
| 2012 | 8167 | 78.9 | 11,353 | 116.5 | 19,520 | 97.1 |
| 2013 | 8094 | 79.1 | 11,116 | 113.9 | 19,210 | 96.1 |
| 2014 | 8207 | 80.6 | 11,309 | 116.2 | 19,516 | 98.0 |
| 2015 | 8813 | 86.9 | 11,604 | 119.9 | 20,417 | 103.0 |
| 2016 | 7877 | 78.2 | 10,815 | 112.3 | 18,692 | 94.9 |
| 2017 | 7775 | 77.4 | 10,832 | 112.8 | 18,607 | 94.7 |
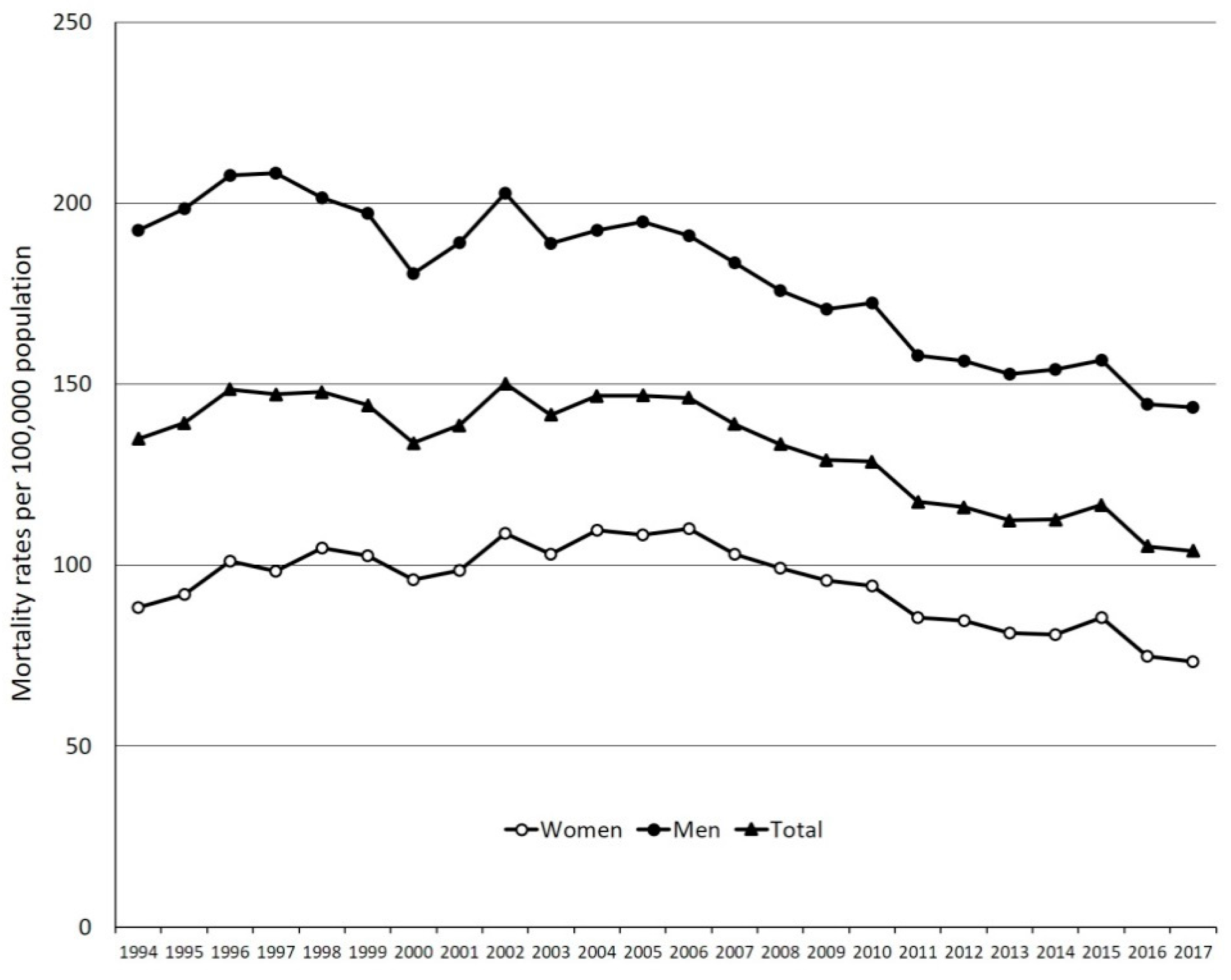
| Year | Women | Men | Total | |||
|---|---|---|---|---|---|---|
| ASMR a | 95% CI | ASMR a | 95% CI | ASMR a | 95% CI | |
| 1994 | 88.3 | 87.6–89.0 | 192.5 | 191.4–193.7 | 134.9 | 134.3–135.6 |
| 1995 | 91.9 | 91.2–92.6 | 198.5 | 197.4–199.7 | 139.3 | 138.7–140.0 |
| 1996 | 101.1 | 100.2–101.7 | 207.7 | 206.5–208.9 | 148.5 | 147.8–149.2 |
| 1997 | 98.4 | 97.7–99.1 | 208.2 | 207.0–209.4 | 147.2 | 146.5–147.8 |
| 1998 | 104.8 | 104.1–105.5 | 201.4 | 200.3–202.6 | 147.8 | 147.1–148.4 |
| 1999 | 102.5 | 101.7–103.2 | 197.2 | 196.1–198.4 | 144.2 | 143.6–144.8 |
| 2000 | 95.9 | 95.2–96.7 | 180.6 | 179.5–181.7 | 133.7 | 133.1–134.3 |
| 2001 | 98.6 | 97.9–99.3 | 189.1 | 188.0–190.2 | 138.6 | 138.0–139.3 |
| 2002 | 108.7 | 107.9–109.4 | 202.8 | 201.7–204.0 | 150.1 | 149.4–150.7 |
| 2003 | 103.0 | 102.3–103.8 | 188.9 | 187.9–190.0 | 141.5 | 140.9–142.1 |
| 2004 | 109.6 | 108.9–110.4 | 192.4 | 191.3–193.4 | 146.7 | 146.1–147.4 |
| 2005 | 108.3 | 107.6–109.1 | 194.9 | 193.8–196.0 | 146.8 | 146.2–147.4 |
| 2006 | 110.1 | 109.4–110.9 | 190.9 | 189.8–192.0 | 146.2 | 145.6–146.8 |
| 2007 | 103.1 | 102.4–103.8 | 183.5 | 182.5–184.5 | 138.9 | 138.3–139.5 |
| 2008 | 99.2 | 98.6–99.9 | 175.8 | 174.8–176.8 | 133.4 | 132.8–134.0 |
| 2009 | 95.8 | 95.1–96.4 | 170.7 | 169.7–171.6 | 129.0 | 128.5–129.6 |
| 2010 | 94.2 | 93.5–94.8 | 172.4 | 171.4–173.3 | 128.6 | 128.1–129.2 |
| 2011 | 85.4 | 84.8–86.0 | 158.0 | 157.0–158.9 | 117.5 | 117.0–118.0 |
| 2012 | 84.6 | 84.0–85.1 | 156.4 | 155.4–157.3 | 116.0 | 115.5–116.5 |
| 2013 | 81.3 | 80.7–81.8 | 152.8 | 151.9–153.7 | 112.4 | 111.9–112.9 |
| 2014 | 80.7 | 80.1–81.2 | 154.1 | 153.2–155.0 | 112.6 | 112.1–113.1 |
| 2015 | 85.5 | 84.9–86.0 | 156.7 | 155.8–157.6 | 116.6 | 116.1–117.1 |
| 2016 | 74.8 | 74.3–75.3 | 144.5 | 143.6–145.4 | 105.2 | 104.7–105.6 |
| 2017 | 73.3 | 72.8–73.8 | 143.5 | 142.7–144.4 | 103.9 | 103.5–104.4 |
References
- Roth, G.A.; Abate, D.; Abate, K.H.; Abay, S.M.; Abbafati, C.; Abbasi, N.; Abbastabar, H.; Abd-Allah, F.; Abdela, J.; Abdelalim, A.; et al. Global, regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 2018, 392, 1736–1788. [Google Scholar] [CrossRef]
- Tatu-Chitoiu, G.; Cinteza, M.; Dorobantu, M.; Udeanu, M.; Manfrini, O.; Pizzi, C.; Vintila, M.; Ionescu, D.D.; Craiu, E.; Burghina, D.; et al. In-hospital case fatality rates for acute myocardial infarction in Romania. CMAJ 2009, 180, 1207–1213. [Google Scholar] [CrossRef] [PubMed]
- Bordejevic, D.A.; Caruntu, F.; Mornos, C.; Olariu, I.; Petrescu, L.; Tomescu, M.C.; Citu, I.; Mavrea, A.; Pescariu, S. Prognostic impact of blood pressure and heart rate at admission on in-hospital mortality after primary percutaneous intervention for acute myocardial infarction with ST-segment elevation in western romania. Ther. Clin. Risk Manag. 2017, 13, 1061–1068. [Google Scholar] [CrossRef] [PubMed]
- UNdata | Record View | Population by Age, Sex and Urban/Rural Residence. Available online: http://data.un.org/Data.aspx?d=POP&f=tableCode%3A22 (accessed on 12 December 2019).
- Pace, M.; Cayotte, E.; Agafitei, L.; Zupanic, T.; Wojtyniak, B.; Gissler, M. 2013 Edition Revision of the European Standard Population Report of Eurostat’s Task Force; Methodologies and Working papers; Publications Office of the European Union: Luxembourg, 2013. [Google Scholar]
- Cretu, D.E.; Udroiu, C.A.; Stoicescu, C.I.; Tatu-Chitoiu, G.; Vinereanu, D. Predictors of in-Hospital Mortality of ST-Segment Elevation Myocardial Infarction Patients Undergoing Interventional Treatment. An Analysis of Data from the RO-STEMI Registry. Maedica 2015, 10, 295–303. [Google Scholar] [PubMed]
- Puymirat, E.; Battler, A.; Birkhead, J.; Bueno, H.; Clemmensen, P.; Cottin, Y.; Fox, K.A.; Gorenek, B.; Hamm, C.; Huber, K.; et al. Euro Heart Survey 2009 Snapshot: Regional variations in presentation and management of patients with AMI in 47 countries. Eur. Hear. J. Acute Cardiovasc. Care 2013, 2, 359–370. [Google Scholar] [CrossRef]
- Widimsky, P.; Wijns, W.; Fajadet, J.; de Belder, M.; Knot, J.; Aaberge, L.; Andrikopoulos, G.; Antonio Baz, J.; Betriu, A.; Claeys, M.; et al. Reperfusion therapy for ST elevation acute myocardial infarction in Europe: Description of the current situation in 30 countries. Eur. Heart J. 2010, 31, 943–957. [Google Scholar] [CrossRef]
- Tatu-Chitoiu, G.; Arafat, R.; Deleanu, D.; Vinereanu, D.; Udroiu, C.; Petris, A. Impact of the Romanian national programme for interventional therapy in ST-elevation myocardial infarction. EuroIntervention 2012, 8, P126–P132. [Google Scholar] [CrossRef]
- Tubaro, M.; Danchin, N.; Goldstein, P.; Filippatos, G.; Hasin, Y.; Heras, M.; Jansky, P.; Norekval, T.M.; Swahn, E.; Thygesen, K.; et al. Pre-hospital treatment of STEMI patients. A scientific statement of the Working Group Acute Cardiac Care of the European Society of Cardiology. Acute Card. Care 2011, 13, 56–67. [Google Scholar] [CrossRef]
- Townsend, N.; Wilson, L.; Bhatnagar, P.; Wickramasinghe, K.; Rayner, M.; Nichols, M. Cardiovascular disease in Europe: Epidemiological update 2016. Eur. Heart J. 2016, 37, 3232–3245. [Google Scholar] [CrossRef]
- Rahimi, K.; Duncan, M.; Pitcher, A.; Emdin, C.A.; Goldacre, M.J. Mortality from heart failure, acute myocardial infarction and other ischaemic heart disease in England and Oxford: A trend study of multiple-cause-coded death certification. J. Epidemiol. Community Health 2015, 69, 1000–1005. [Google Scholar] [CrossRef]
- Orozco-Beltran, D.; Cooper, R.S.; Gil-Guillen, V.; Bertomeu-Martinez, V.; Pita-Fernandez, S.; Durazo-Arvizu, R.; Carratala-Munuera, C.; Cea-Calvo, L.; Bertomeu-Gonzalez, V.; Seoane-Pillado, T.; et al. Trends in Mortality From Myocardial Infarction. A Comparative Study Between Spain and the United States: 1990–2006. Rev. Española Cardiol. (Engl. Ed. ) 2012, 65, 1079–1085. [Google Scholar] [CrossRef] [PubMed]
- Benjamin, E.J.; Blaha, M.J.; Chiuve, S.E.; Cushman, M.; Das, S.R.; Deo, R.; De Ferranti, S.D.; Floyd, J.; Fornage, M.; Gillespie, C.; et al. Heart Disease and Stroke Statistics’2017 Update: A Report from the American Heart Association. Circulation 2017, 135, e146–e603. [Google Scholar] [CrossRef] [PubMed]
- Simionescu, N.; Niculescu, L.S.; Sanda, G.M.; Stancu, C.S.; Popescu, A.C.; Popescu, M.R.; Simionescu, M.; Dimulescu, D.R.; Vlad, A.; Sima, A.V. MiR-486 and miR-92a identified in HDL subfractions discriminate between stable and vulnerable coronary artery disease patients. FEBS J. 2015, 282, 217–218. [Google Scholar]
- Mihai, M.; Giurcãneanu, C.; Popa, L.; Nitipir, C.; Popa, M. Controversies and challenges of chronic wound infection diagnosis and treatment. Mod. Med. 2015, 22, 375–381. [Google Scholar]
- Mihai, M.M.; Dima, M.B.; Dima, B.; Holban, A.M. Nanomaterials for Wound Healing and Infection Control. Materials 2019, 12, 2176. [Google Scholar] [CrossRef]
- Dorobantu, M.; Tautu, O.F.; Dimulescu, D.; Sinescu, C.; Gusbeth-Tatomir, P.; Arsenescu-Georgescu, C.; Mitu, F.; Lighezan, D.; Pop, C.; Babes, K.; et al. Perspectives on hypertension’s prevalence, treatment and control in a high cardiovascular risk East European country: Data from the SEPHAR III survey. J. Hypertens. 2018, 36, 690–700. [Google Scholar] [CrossRef]
- Dorobanţu, M.; Darabont, R.; Ghiorghe, S.; Arsenescu-Georgescu, C.; Macarie, C.; Mitu, F.; Lighezan, D.; Musetescu, R.; Pop, C.; Ardeleanu, E.; et al. Hypertension prevalence and control in Romania at a seven-year interval. Comparison of SEPHAR I and II surveys. J. Hypertens. 2014, 32, 39–47. [Google Scholar] [CrossRef]
- Mota, M.; Popa, S.G.; Mota, E.; Mitrea, A.; Catrinoiu, D.; Cheta, D.M.; Guja, C.; Hancu, N.; Ionescu-Tirgoviste, C.; Lichiardopol, R.; et al. Prevalence of diabetes mellitus and prediabetes in the adult Romanian population: PREDATORR study. J. Diabetes 2016, 8, 336–344. [Google Scholar] [CrossRef]
- Popa, S.; Moţa, M.; Popa, A.; Moţa, E.; Serafinceanu, C.; Guja, C.; Catrinoiu, D.; Hâncu, N.; Lichiardopol, R.; Bala, C.; et al. Prevalence of overweight/obesity, abdominal obesity and metabolic syndrome and atypical cardiometabolic phenotypes in the adult Romanian population: PREDATORR study. J. Endocrinol. Invest. 2016, 39, 1045–1053. [Google Scholar] [CrossRef]
- Ioacara, S.; Guja, C.; Fica, S.; Ionescu-Tirgoviste, C. The dynamics of life expectancy over the last six decades in elderly people with diabetes. Diabetes Res. Clin. Pract. 2013, 99, 217–222. [Google Scholar] [CrossRef]
- Ioacara, S.; Guja, C.; Ionescu-Tirgoviste, C.; Martin, S.; Tiu, C.; Fica, S. Rates and Causes of Death among Adult Diabetes Patients in Romania. Endocr. Res. 2019, 44, 81–86. [Google Scholar] [CrossRef] [PubMed]
- Ioacara, S.; Sava, E.; Georgescu, O.; Sirbu, A.; Fica, S. Recent diabetes-related mortality trends in Romania. Acta Diabetol. 2018, 55, 821–826. [Google Scholar] [CrossRef] [PubMed]
- Ioacara, S.; Tiu, C.; Panea, C.; Nicolae, H.; Sava, E.; Martin, S.; Fica, S. Stroke Mortality Rates and Trends in Romania, 1994–2017. J. Stroke Cerebrovasc. Dis. 2019, 28, 104431. [Google Scholar] [CrossRef] [PubMed]
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ioacara, S.; Popescu, A.C.; Tenenbaum, J.; Dimulescu, D.R.; Popescu, M.R.; Sirbu, A.; Fica, S. Acute Myocardial Infarction Mortality Rates and Trends in Romania between 1994 and 2017. Int. J. Environ. Res. Public Health 2020, 17, 285. https://doi.org/10.3390/ijerph17010285
Ioacara S, Popescu AC, Tenenbaum J, Dimulescu DR, Popescu MR, Sirbu A, Fica S. Acute Myocardial Infarction Mortality Rates and Trends in Romania between 1994 and 2017. International Journal of Environmental Research and Public Health. 2020; 17(1):285. https://doi.org/10.3390/ijerph17010285
Chicago/Turabian StyleIoacara, Sorin, Andreea C. Popescu, Joseph Tenenbaum, Doina R. Dimulescu, Mihaela R. Popescu, Anca Sirbu, and Simona Fica. 2020. "Acute Myocardial Infarction Mortality Rates and Trends in Romania between 1994 and 2017" International Journal of Environmental Research and Public Health 17, no. 1: 285. https://doi.org/10.3390/ijerph17010285
APA StyleIoacara, S., Popescu, A. C., Tenenbaum, J., Dimulescu, D. R., Popescu, M. R., Sirbu, A., & Fica, S. (2020). Acute Myocardial Infarction Mortality Rates and Trends in Romania between 1994 and 2017. International Journal of Environmental Research and Public Health, 17(1), 285. https://doi.org/10.3390/ijerph17010285






