Abstract
Computerized and blended treatments seem to be an attractive treatment for adolescents as an alternative to face-to-face treatment, but mental health professionals seem hesitant to use these treatment modalities. This review provides an overview of factors contributing to and withholding from using computerized or blended treatment in routine care. Three databases were searched with terms related to (1) adolescents, (2) depression, (3) computerized or blended, and (4) treatment. Of the 33 articles identified, 10 focused on unguided computerized treatments, six on guided, two on blended, two compared unguided, blended- and face-to-face treatment to no treatment, and eight studies on games. Further, two articles that were focused on an online monitoring tool and three on intervention characteristics or preferred modes of help-seeking. Evidence for effectiveness, adherence, drop-out, and forming therapeutic relations were suspected to be barriers, but are no reason to reject computerized or blended treatment. Improvement in mental health literacy and the possibility to tailor the intervention are facilitators. However, adolescents’ intention to seek help, acceptability of computerized treatment, symptom severity, time spent by therapist, and other facilities are identified as barriers and they need to be taken into account when using computerized or blended interventions. Nevertheless, computerized and blended are promising treatments for depressed youth.
1. Introduction
Depressive disorders are among the most prevalent mental health disorders in youth and they are a major contributor to disability [1,2]. Before the age of 19, more than 15% of youth has suffered from at least one depressive episode in their life [3]. Suffering from depression at a young age increases the risk of social problems, poor academic and professional performance, school drop-out, and health problems, such as substance abuse, comorbid disorders, and suicide [4,5,6]. Besides, a high risk of recurrence and chronicity characterize depressive disorders [7,8]. Given these consequences, treating the disorder effectively at an early age is crucial.
Cognitive Behavioural Therapy (CBT) and Interpersonal Psychotherapy are the first choices of treatment from the current available forms of psychotherapy for depressed youth [9,10,11]. Nevertheless, the average effect size of CBT as compared to a variety of control conditions (i.e., active treatments targeting non-depressive symptoms, active treatment for depression, medication placebo) is small to moderate (ES = 0.34–0.80) [12,13], and only 50% of the treated youth show symptom improvement after psychotherapy [14]. This shows that face-to-face treatment is effective in treating depression, but certainly not for all depressed adolescents. Above all, the number of youth that drop out of treatment is high; approximately 50% (with a range from 17 to 72%) of all adolescent outpatients drop out of treatment according to a meta-analysis [15]. Important barriers for youth seeking help or treatment that are often mentioned are lack of accessibility, for example lack of time, high costs, or no transport [16]. This strongly suggests that more attractive and more suitable treatments are needed, especially for adolescents who do not prefer to visit a mental health professional each week. In doing so, individual outcomes could be improved.
Computerized treatments seem to be an obvious solution to several problems, because of their availability, anonymity, and accessibility [17,18]. Treatment through computer-based programs (for example CD-Roms) and treatment through internet-based programs using online applications (for example email or web-based programs), that are often the most recently developed programs define computerized treatment programs. In this review article, computer-based and internet-based programs will both be conceptualized as computerized programs. Computerized treatments can be unguided, meaning that patients work through the program themselves, or guided, meaning that there is support of a therapist. Characteristic of these guided programs is that communication between patient and support is not synchronized, which means that patients and therapists communicate not at the same time [19]. Treatment programs can also be presented as a game, where the content of the treatment is presented in a gamified manner [20]. Earlier research has demonstrated that computerized treatment is moderately effective in treating depressive disorders in youth when compared to no treatment and waiting list controls [18]. A meta-analysis of treatment effects in depressed adults showed equivalent effects of guided internet-based treatment when compared to face-to-face treatment [21]. However, another meta-analysis has demonstrated that computerized CBT for adults in clinical practice, i.e., outside controlled research settings, has smaller effects and a higher attrition rate when compared to computerized CBT in adults who are recruited for participation in research [22]. A recent development is combining computerized treatment with face-to-face treatment into the so-called blended treatment in order to overcome the downsides of computerized treatment [23]. In blended treatment, patients work independently while using computerized content and receiving guidance by their therapist by means of personal face-to-face contact [23,24]. Blended treatment specifically aims to preserve the therapeutic relation [25]. In such a way, blended treatment contains the benefits of both face-to-face treatment as well as computerized treatment.
Yet, professionals in youth clinical practice still hold a skeptical attitude towards computerized and blended treatments [26,27]. They doubt the effect of these treatment modalities [28] and they assume that there is a high risk of adverse events [19], such as an increase in symptom severity and suicidal ideation, as a consequence of fewer or face-to-face treatment sessions. As a result, professionals are hesitant to use these treatment modalities [29]. The frequently mentioned arguments against solely using computerized or blended treatments include difficulties in monitoring the increase of symptom severity and the risk for suicide [19], no match with the needs of the adolescent, low treatment adherence, and high drop-out. As a consequence, therapists often refrain from using computerized or blended treatments and continue to use face-to-face treatments [28]. However, the evidence for not using these treatments is unclear, since the potentially facilitating factors (i.e., availability, anonymity, accessibility) and barriers (i.e., effect, drop-out) to use computerized or blended treatments in treating depressed youth are not systematically described.
The aim of this review is to provide an overview of the knowledge on factors that could contribute to, or withhold from, using computerized or blended treatment in routine care for adolescents with depression. We will review whether intervention effects, mental health literacy, adherence and drop-out, intention to seek help, tailoring the intervention, symptom severity, risk monitoring, acceptability, treatment engagement, time spent by therapist, therapeutic relation, and other facilities for computerized or blended interventions are facilitators or barriers in the use of treatment of depressed adolescents. Additionally, suggestions for future research are given.
2. Method
2.1. Search Strategy
Databases Medline, PsycInfo, and Embase were systematically searched in January 2019. The search terms were (1) adolescent OR adolescence OR young adult OR teen, AND (2) depression OR depressive OR depressed OR MDD OR mood disorder OR dysthymic OR dysthymia, AND (3) blended OR supported OR guided OR assisted OR computerized OR computerised OR computer-based OR internet-based, AND (4) treatment OR therapy OR intervention OR program.
We identified 1686 studies while using these terms. Besides these, 23 studies were identified through other sources, for example through hand searching reference lists of relevant studies and reviews. In total, we identified 1709 studies. After removing 927 duplicates, 782 studies remained. The first author screened the first, titles, and abstracts to determine whether studies were relevant for the review. The inclusion criteria for the current review were that (1) the presented interventions were computerized or blended, (2) interventions were used as treatment (not as prevention), (3) were directed at depressive symptoms or disorders, (4) were aimed at youth (i.e., aged 12–23 years), (5) were published in peer-reviewed journals in the English or Dutch language, and (6) contained original data. This resulted in excluding 724 studies, because the studies were not about computerized or blended programs (k = 187), did not involve treatment (but were, for example, on online diagnostic tools or online learning environments) (k = 167), were not directed at depressive symptoms or disorders (k = 334), were not aimed at adolescents or youth (k = 18), were not written in the English or Dutch language (k = 4), or did not contain original data (but were, for example, reviews or meta-analyses) (k = 14); as a result, 58 studies remained.
Next, titles, abstracts, and method sections were systematically reviewed and considered for inclusion. Of the 58 remaining studies, 25 studies were excluded because they were not about computerized or blended interventions (k = 3), not aimed at youth (k = 3), were not published in a peer-reviewed journal (but were, for example, conference abstracts) (k = 12), did not contain original data (but were, for example, published study designs) (k = 3), or were not available (k = 4). Figure 1 presents an overview of the final selection of 33 studies. These studies were used in a qualitative analysis on barriers and facilitating factors (including effectiveness) that play a role in using these treatment modalities in the treatment of depressed youth.
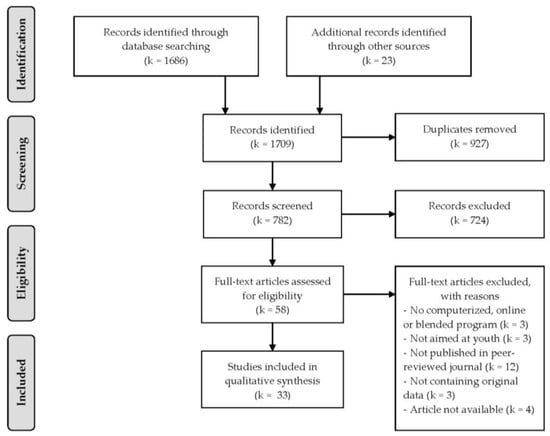
Figure 1.
Flow chart of study selection.
2.2. Data Extraction
The following data could be extracted from the included studies: intervention effects, mental health literacy, adherence and drop-out, intention to seek help, tailoring the intervention, symptom severity, risk monitoring, acceptability, treatment engagement, time spent by therapist, therapeutic relation, and facilities for computerized or blended interventions. For these factors, we will describe whether studies show whether these factors are actual barriers or facilitators in the use of treatment of depressed adolescents.
3. Results
3.1. Description of Studies
Table 1 presents details of the included studies (k = 33). Sixteen studies were aimed at computerized treatments, of which nine were unguided computerized treatments (four computer-based and five internet-based) [30,31,32,33,34,35,36,37,38] and seven studies were guided computerized treatments (one computer-based and six internet-bases) [39,40,41,42,43,44,45], two studies at blended treatment [46,47], two studies compared unguided computerized, blended- and face-to-face treatment to no treatment [48,49], and eight studies were aimed at self-help internet-based games [50,51,52,53,54,55,56,57]. Furthermore, two studies that were focused on the use of an online monitoring tool aimed at registering and monitoring treatment progression [58,59] and three studies were aimed at characteristics of online interventions or studied the preferred modes of help seeking [60,61,62].

Table 1.
Characteristics of the included studies.
Fourteen studies were mainly focused on the evaluation of the effects of the intervention. In these studies, the designs varied between randomized controlled trials (k = 10) [34,35,36,38,39,44,45,49,52,57], pre-post designs with control group (k = 2) [33,42], and pre-post designs without control group (k = 2) [30,40]. Sixteen studies were mainly focused on the feasibility, usability, and acceptability of computerized and blended interventions. The study designs were mixed and they contained qualitative studies with focus groups of patients, healthy adolescents or mental health professionals (k = 6) [41,53,54,56,58,59], randomized controlled trials (k = 3) [43,47,48], pre-post designs without control group (k = 5) [31,46,50,51,55], and cross-sectional studies (k = 2) [32,37]. Three studies were mainly focused on the preferences of patients regarding treatment modalities [32,60,62].
3.2. Intervention Effects
The evidence shows that participants who received unguided computerized CBT (cCBT) less often showed a depressive disorder after receiving the intervention than before [30]. Further, participants showed an increase in perceived control after receiving unguided cCBT [33]. When unguided cCBT was compared to a wait list condition, the findings showed that depressive symptoms decreased significantly more in the unguided CBT condition [34]. The results also showed that the intervention was equally effective for boys and girls [35]. The findings of two studies showed that the decrease of depressive symptoms was larger in the participants in the unguided CBT condition when compared to the participants in the psychoeducational control condition [36,38]. Changes in mental health literacy after unguided computerized treatment were not reported.
After receiving guided cCBT participants showed less depressive symptoms [40]. Depressive symptoms were significantly lower after 10 weeks in the guided cCBT condition when guided cCBT was compared to a waitlist condition [51]. When only including boys, the findings showed no difference in the reduction of depressive symptoms between guided cCBT and psychoeducation [42]. When guided cCBT was compared to treatment as usual, a larger symptom reduction was found in the participants who received guided CBT [43]. Additionally, guided CBT has more benefits for depressed adolescents than the waitlist condition [35,45]. Adolescents showed an increase in literacy and confidence in their knowledge on depression, independent from changes in depressive symptoms after receiving guided cCBT [39].
Blended treatment and treatment as usual showed equal effects in a decrease of depressive symptoms [47]. Moreover, adolescents who received blended CBT for their depressive disorder showed a significant increase in knowledge of CBT concepts after the intervention [47]. Two other studies showed that blended CBT was more effective in treating depressive symptoms, as compared to unguided cCBT alone and face-to-face CBT alone. Nonetheless, participants in all three conditions showed a significant decrease in depressive symptoms when compared to participants without an intervention [48,49]. It needs to be noted that participants in the latter two studies were young adults between 18 and 25, and cannot be seen as a representation of patients in their adolescence.
When the adolescents participated in a self-help CBT-based computer game, their depressive symptoms decreased significantly [55]. However, a decrease of depressive symptoms was not significantly different from adolescents who received treatment as usual [57]. Another study showed that depressive symptoms decrease more after a self-help CBT-based computer game (78%) when compared to a wait list condition (36%) [52]. Two of the online modules of the self-help CBT-based computer game Sparx aimed at improving mental health literacy and the knowledge on depression (e.g., “Learning about depression” in Sparx) were rated as the most useful modules [55].
3.3. Adherence and Drop-Out
Adherence is often considered to be lower and drop-out higher in computerized treatments as compared to face-to-face treatments [62], hence they are considered to be barriers. Between 62% and 94% of the participants completed (almost) the entire unguided cCBT [36,38]. Other findings show that between 0% and 21% of participants dropped out of unguided cCBT [34,38,48].
For guided cCBT, Van der Zanden, Kramer, Gerrits, and Cuijpers [45] reported that only 20% of the participants completed the complete program and attended all sessions, which was exceptionally low when compared to the other studies. However, each session lasted 90 min. and more than half of the participants attended four of the six online sessions. Other studies found that between 61 and 70% completed the full program [40,44]. Johnston, Dear, Gandy, Fogliati, Kayrouz, Sheehan, Rapee, and Titov [40] also reported that 17% of the participants dropped out. It was also mentioned that some individuals did not complete the intervention, but the reason for doing so was not because of dissatisfaction with the intervention [43].
Adherence was not reported for blended interventions. The drop-out varied between studies: De Vos, Tromp, Bodden, and Stikkelbroek [46] reported that 13% of the patients dropped out, Kobak, Mundt, and Kennard [47] reported 10%, while Sethi [48] reported no drop-outs.
For games, it was found that between 60% and 81% of the participants completed the entire self-help CBT-based computer game Sparx [55,57]. Another 9 to 26% completed four to six modules of the game. However, when the self-help CBT-based computer game was used for adolescent inpatients, only 10% completed the intervention [50]. Fleming, Dixon, Frampton, and Merry [52] reported that there was no difference in proportion of drop-outs between a self-help CBT-based computer game condition and the waitlist condition.
3.4. Intention to Seek Help
In general, a low intention to seek help characterizes depressed adolescents [52]. Indeed, it was found that depressed adolescents are more inclined to avoid seek help than to get face-to-face or computerized treatment [60]. After following an unguided computerized program for depression, adolescents are more intended to seek additional mental health treatment [33,60]. Higher mental health literacy indirectly predicted the intention to seek computerized or face-to-face treatment. Although computerized programs (i.e., unguided or guided) seem to be more available and accessible due to more privacy for example, adolescents report that they need to be motivated to use computerized programs and need to be aware of the existence of computerized treatments and where to find them [31].
3.5. Tailoring the Intervention
The possibility to adapt an intervention to the individual preferences, needs, and goals is called tailoring interventions [63]. Computerized interventions are often considered easier to tailor, and this can be seen as a facilitator of computerized interventions. Adolescents reported that computerized interventions are accessible at any time and place and can, therefore, be easily tailored to individual preferences [31]. Moreover, a study reported that study participants found it appealing that several computerized programs allowed for patients to tailor exercises and create their own treatment goals, for example by creating their own behavioral activation plan [32].
3.6. Symptom Severity
The severity of depressive symptoms or having a severe depressive disorder has been described as a barrier to use computerized treatment. The perception of mental health professionals is that online interventions, regardless of being unguided, guided, or blended, are not adequate for adolescents with severe depressive symptoms or a major depressive disorder, because the computerized support system is not suitable [41]. Additionally, during computerized treatment, the severity of depressive symptoms can be a barrier for proceeding. An increase in depressive symptoms during the intervention was a reason to change the computerized intervention into a face-to-face treatment, because mental health professionals believed that the online intervention was inappropriate when the depression became too severe [61].
Additionally, it was found that the use of this app decreased when mental health improved in testing the feasibility of an online application aimed at registering and monitoring treatment progression and to access crisis plans. The app became less useful when treatment was finished or almost finished, because the need to access crisis plans and update treatment progression was smaller [58].
3.7. Risk Monitoring
The concern of mental health professionals is that they are not able to monitor risk of self-harm and suicidal ideation in the computerized treatment of depressive disorders [59]. Mental health professionals reported that it was difficult to decide which notifications were actually alarming in the adolescent’s condition and needed interference when guided computerized interventions were used [41].
Another concern is that treatment activity of the patient is often not synchronous with the activity of the therapist. Consequently, the therapist is not always able to monitor progress and risk. Clinicians participating in a qualitative study suggested that other people in mental service could check for alerting messages [59].
3.8. Acceptability
Participants that used unguided cCBT rated the program as useful and helpful [32]. Most of the participants would recommend it to others [33,36]. One study asked participants to rate the actual website. The participants were positive and they reported that it was easy to use and relatable [33]. Unguided cCBT allows for privacy, which participants rated as very important [31]. The strongest predictor for use and non-use appeared to be gender, as females are more likely to use unguided cCBT [37]. Guided cCBT was evaluated by participants as useful and ‘worth their time’ [40]. Most of the participants were satisfied [40,43] and they rated the treatment as acceptable and would recommend it to friends [40].
Blended CBT was rated as flexible, helpful, and easy to use at a location the adolescent choose, which is important, because adolescents prefer not to visit mental health services for face-to-face treatment [46,47]. However, more than half of the participants would not recommend it to others. Improvements in depressive symptoms were attributed to the face-to-face sessions and not to the computerized program [46]. Further, adolescents reported that the therapists’ messages were useful and motivating [46].
Participants reported that the computer game Sparx was acceptable, useful, and feasible as intervention [50,53,55]. They also reported that the program was appealing for young people [55,57], although the generic version of Sparx did not specifically address topics for sexual minority youth (i.e., youth attracted to the same sex, both sexes, or not sure of their sexual attraction) [54]. The majority of adolescents would recommend Sparx to others [55,57]. Privacy can be easily guaranteed [55] and, for members from a small community, it seems to be a promising way to seek help [51,56]. Nonetheless, internet safety needs to be considered by the users [56].
Adolescents were positive about an online application aimed at registering and monitoring to enhance the effects of cCBT, because it was easier to contact mental health professionals [59]. Patients and mental health professionals were both positive about the possibilities of an online monitoring tool for treatment progression and access crisis plans to fit well with the treatment [58].
Besides the acceptability of specific interventions, registered in earlier mentioned studies, two studies explicitly focused on modalities of treatment delivery and preferences of adolescents and young adults. The first study revealed that only a minority (16%) of the Australian adolescents preferred computerized treatment. Two-thirds of the adolescents preferred face-to-face treatment; however, the highest percentage of adolescents had no intention to seek help at all [60]. Another study revealed that the majority of patients of 18 years and older preferred face-to-face treatment, and there was also preference of a combination of face-to-face and computerized treatment (blended) over complete computerized treatment [62]. It needs to be noted that participants in this latter study are aged 18 and older, and cannot be seen as a representation of patients in their adolescence.
3.9. Treatment Engagement
The low treatment engagement of youth in computerized programs is often mentioned as a barrier. Patients and mental health professionals reported that an online application (a so-called electronic personal health record) aimed at registering and monitoring treatment progression was stimulating adolescents’ engagement in a hospital-based outpatient treatment [58]. In addition, an online behavioral activation tool was assessed by youth to have a motivational effect on treatment engagement [32]. No studies reported results on treatment engagement of adolescents or therapists for computerized treatment (unguided or guided), blended treatment, or self-help game.
3.10. Time Spent by Therapist
The time investment of therapists is seen as a facilitator in using computerized treatment, because it is often estimated that the time spent by therapists for guided computerized treatment or blended treatment is less than for face-to-face treatment [64,65]. One of the studies included in this review registered the time that mental health professionals spent on each patient who received guided cCBT. On average, they spent more than 45 min. per week per patient. Besides the chat sessions, approximately 30 messages were sent to each patient [44]. Mental health professionals reported that an online monitoring tool (to monitor mood, risk, and treatment adherence of adolescents completing a cCBT program) was not fully integrated in the treatment and they perceived the monitoring tool as an additional task. The monitoring took more time than anticipated and not all professionals used it [59].
3.11. Therapeutic Relation
Mental health professionals often express their concerns regarding the quality of the therapeutic relation when solely using a computerized treatment, hence making it a barrier to use computerized treatment programs. They were concerned whether using a computerized program could establish the same relationship as having face-to-face sessions [59]. However, mental health professionals who already used a computerized program, more specifically guided cCBT, reported that it did not negatively impact their therapeutic relationship with the depressed adolescent [43,44,59]. Guided computerized treatment could even support the therapeutic interaction, because the adolescents learn how to express themselves in the computerized program [47,61]. An online application that was aimed at registering and monitoring treatment progression and accessing crisis plans was reported to facilitate communication. This resulted in a positive relation between therapist and patient, because the communication during the face-to-face sessions was focused on treatment techniques and not on monitoring [58].
3.12. Facilities for Computerized Interventions
Another important barrier for using guided or blended interventions is a lack of training in the computerized part of the treatment protocol. Mental health professionals did not receive any training or the training did not met their needs [61]. Further, it was mentioned that the internet connection was to slow for the use of internet interventions, especially in clinical settings [61].
4. Discussion
The aim of this review was to provide an overview of the knowledge of factors that could contribute to, or withhold from, using computerized or blended treatment in routine care for adolescents with depression. We expected that acceptability, low intention to seek help, the possibility to tailor the intervention, and time investment of therapist are considered as facilitators for the use of computerized interventions. On the other hand, we expected that limited evidence for effectiveness, low mental health literacy, low adherence, high drop-out, high severity of symptoms, difficulty in risk monitoring, low treatment engagement, difficulties in establishing a therapeutic relation, and limited facilities for computerized treatment are considered as barriers.
Overall, the findings of this review suggest that adolescents receiving unguided cCBT, guided cCBT, blended CBT, or self-help CBT-based computer game show a decrease in depressive symptoms after the intervention. Studies showed that symptom reduction was larger after unguided cCBT when compared to psychoeducation, larger in guided cCBT as compared to treatment as usual, and larger in blended CBT when compared to guided cCBT and face-to-face CBT [48,49]. These findings suggest that depressive symptoms reduce with all forms of cCBT including blended CBT. However, these findings need to be interpreted with caution, because they are based on a low number of studies; some without comparison to a control condition. Additionally, it needs to be taken into account that effects, especially of the unguided treatment, can be slightly overestimated due to the influence of research activities (e.g., administrative contact about questionnaires or therapist contact about severity of symptoms). It is known from earlier research in adults that effect sizes of computerized treatment increase when there is more support [66,67]. Especially in the treatment forms in which there is usually none to very little contact with therapist, this might have influenced the effects.
Intervention adherence to unguided cCBT (i.e., 62–94%), guided cCBT (i.e., 61–70%), blended CBT (i.e., 90%), and self-help CBT-based computer game (i.e., 60–81%) was comparable. The drop-out rates were also comparable between interventions, that is, 0–21% in unguided CBT, 17% in guided CBT, 0–13% in blended CBT. These percentages are comparable to the 14.2% drop-out of face-to-face psychotherapy for depressed adolescents reported by Watanabe, Hunot, Omori, Churchill, and Furukawa [14]. Again, we need to consider the impact of research activities, because it is known that drop-out in adult treatment is lower when there is more support during computerized treatment [66]. Therefore, the drop-out number might be an underestimation, especially in unguided computerized programs.
Mental health professionals reported that the therapeutic relation with adolescents was not negatively impacted when treatment is computerized. This is corresponds to earlier findings that online communication is an easy way for youth to connect to others and form new relationships [68,69]. However, mental health professionals qualified computerized interventions, whether or not guided or blended, as inadequate for adolescents with severe depression. The major concern is that mental health professionals are not able to monitor risk on self-harm or suicidal ideation. The intensive monitoring of risks is in accordance with the treatment guidelines for depression in youth [70]. Mental health professionals are supposed to make a safety plan when a patient suffers from suicidal ideation and this might, therefore, lead to a strong preference for face-to-face treatment in mental health professionals.
When considering acceptability, computerized and blended treatment were rated by participants as useful, helpful, easy to use, relatable, worth the time, and participants were satisfied. Privacy was mentioned as a benefit of unguided CBT. The participants attributed the improvements after blended CBT to the face-to-face sessions.
The results show that depressed adolescents have low intention to seek help; they are more intended to not seek help than to get any form of treatment. A minority of adolescents would prefer computerized treatment. However, higher mental health literacy increased the intention to seek help. Adolescents stated that especially online interventions are accessible at any time and place, and give the possibility to be more easily tailored to their preferences. Further, studies show that mental health literacy increased in adolescents who received guided cCBT, blended CBT, or self-help CBT-based computer game. This indicates that computerized treatment might be an important part in a stepped care approach, where the adolescents first receive computerized treatment to increase mental health literacy, move on to blended treatment when symptoms remain, and only move to a more intensive face-to-face treatment if necessary, as was suggested before by Van Straten, et al. [71]. This approach offers accessible and efficient mental health support for depressed adolescents in an effective way.
Further, training for therapists in the computerized part of the protocol is an important necessity according to therapists. However, a study among psychologists regarding the use of internet-based therapeutic interventions showed that psychologists have little interest in using or receiving training in computerized therapy [29]. This discrepancy between knowing that training is important, and low interest in receiving training might explain the low use of computerized treatment in treating depressed youth.
Summarizing, evidence for effectiveness, mental health literacy, adherence, drop-out, the possibility to tailor the intervention, and forming a therapeutic relation can be seen as facilitators in using computerized treatment. The intention to seek help, symptom severity, acceptability, and facilities of computerized treatment can be seen as barriers. Risk monitoring is not possible in unguided treatment, but it can be done in guided or blended treatment. Time that is spent by therapists is nonexistent in unguided treatment. However, in guided or blended treatment, the time that is spent by therapist is comparable to face-to-face treatment. This shows that adolescents’ acceptability for computerized treatment and time that is spent by the therapist, both often mentioned as facilitators, appear to be barriers based on our research findings. Further, evidence of effectiveness, adherence, drop-out, and therapeutic relation were thought to be barriers for computerized treatment, and our findings showed that they are facilitating computerized and blended treatment.
4.1. Strengths and Limitations
This study has important limitations that need to be taken into account when interpreting the results. First, the studies included in this review were not selected on the study design, which resulted in studies with pre-post design with or without control condition, randomized controlled trials, cross-sectional studies, and studies with a qualitative study design. The quality of the designs is sometimes insufficient for examining effectiveness. However, not all included studies were aimed at effectiveness and, therefore, they give insight in other factors that could contribute to or withhold from using computerized or blended treatment in routine care. Second, findings are based on a small number of studies. Additionally, most participants were actively recruited to participate in the study, therefore characteristics, symptom level, and severity differed largely across the included studies. It is uncertain whether findings will hold when computerized or blended treatments are implemented in routine care [72,73]. Therefore, the findings need to be interpreted with caution and conclusions need to be carefully drawn. Third, we noticed that the terms guided computerized treatment and blended treatment were not used consistently across different studies. We choose to define treatment as blended only when treatment existed of computerized content through which patients work independently and patients receive guidance by their therapist by means of personal face-to-face contact, in line with the definition of Mathiasen, Andersen, Riper, Kleiboer, and Roessler [23] and Erbe, Eichert, Riper, and Ebert [24].
4.2. Suggestions for Future Research
There is some evidence regarding the effectiveness of computerized treatments for depressed youth, but evidence on effectiveness on blended treatment is scarce. Both treatment forms need to be examined in routine care to study whether the effects hold when they are implemented in routine care. Especially studies on the effectiveness of computerized and blended treatment in routine care can contribute to increase knowledge of mental health professionals and lower the threshold to use computerized, blended, or face-to-face treatment.
Furthermore, there is a gap of knowledge regarding the cost-effectiveness of computerized as well as blended treatment; hence, more research in this area is warranted. It has been suggested that blended care could reduce costs in comparison to face-to-face treatment. To our knowledge, only a limited number of studies assessed cost-effectiveness of blended treatment for depressed adults [74,75] and one review with 12 included studies was performed on the cost-effectiveness of internet and mobile-based interventions for treatment and the prevention of depression in adults [76]. However, no studies have been done on cost-effectiveness for depressed youth.
Lastly, the adherence rates and drop-out rates were found to be equal for computerized and face-to-face treatment [14]. Possibly, the adherence and drop-out rates might improve when individual patients are offered their preferred treatment. Moreover, studies on personalized treatment have shown that treatment effects can be improved when patients are assigned to treatment that is optimal for their characteristics (e.g., symptoms severity, life events, comorbidity) based on prediction models (e.g., [77,78]).
5. Conclusions
Based on this review, we conclude that computerized and blended treatments seem promising as treatments for depressed youth in terms of effectiveness, adherence, drop-out, and forming a therapeutic relation. Additionally, the improvement in mental health literacy and the possibility to tailor the intervention can be seen as facilitators in using computerized treatment. However, adolescents’ intention to seek help, symptom severity, and facilities of computerized treatment can be seen as barriers. Further, adolescents’ acceptability for computerized treatment and time spent by therapist were thought to be facilitators, both often mentioned as facilitators, appear to be barriers that are based on our research findings. Highlighting the importance to monitor risks of severe depressive symptoms and possible suicidal ideation, unguided computerized treatment might be more appropriate for patients with mild to moderate depressive symptoms, where blended treatment could serve as a following step in the stepped care approach. Nonetheless, it needs to be noted that further research needs to be done to strengthen evidence for the use of computerized and blended treatment in routine care.
Author Contributions
S.P.A.R. was responsible for the literature search and reporting the study results. S.P.A.R. was responsible for preparing the manuscript, which was revised by S.P.A.R., Y.A.J.S. and D.H.M.B. All authors have read and agreed to the published version of the manuscript.
Funding
This research and the APC was funded by the Dutch Organisation for Health research and Development ZonMW (grant number 70-72900-98-16144).
Conflicts of Interest
The authors declare that they have no conflict of interest.
References
- Gore, F.M.; Bloem, P.J.N.; Patton, G.C.; Ferguson, J.; Joseph, V.; Coffey, C.; Sawyer, S.M.; Mathers, C.D. Global burden of disease in young people aged 10–24 years: A systematic analysis. Lancet 2011, 377, 2093–2102. [Google Scholar] [CrossRef]
- Ferrari, A.J.; Somerville, A.J.; Baxter, A.J.; Norman, R.; Patten, S.B.; Vos, T.; Whiteford, H.A. Global variation in the prevalence and incidence of major depressive disorder: A systematic review of the epidemiological literature. Psychol. Med. 2013, 43, 471–481. [Google Scholar] [CrossRef] [PubMed]
- Ormel, J.; Raven, D.; Van Oort, F.; Hartman, C.A.; Reijneveld, S.A.; Veenstra, R.; Vollebergh, W.A.M.; Buitelaar, J.; Verhulst, F.C.; Oldehinkel, A.J. Mental health in Dutch adolescents: A TRAILS report on prevalence, severity, age of onset, continuity and co-morbidity of DSM disorders. Psychol. Med. 2015, 45, 345–360. [Google Scholar] [CrossRef] [PubMed]
- Verboom, C.E.; Sijtsema, J.J.; Verhulst, F.C.; Penninx, B.W.J.H.; Ormel, J. Longitudinal associations between depressive problems, academic performance, and social functioning in adolescent boys and girls. Dev. Psychol. 2014, 50, 247. [Google Scholar] [CrossRef]
- Aalto-Setälä, T.; Marttunen, M.; Tuulio-Henriksson, A.; Poikolainen, K.; Lönnqvist, J. Depressive symptoms in adolescence as predictors of early adulthood depressive disorders and maladjustment. Am. J. Psychiatry 2002, 159, 1235–1237. [Google Scholar] [CrossRef]
- Portzky, G.; Van Heeringen, C. Suïcide bij jongeren. Psychol. Gezondh. 2009, 37, 75–89. [Google Scholar] [CrossRef]
- Birmaher, B.; Brent, D.A.; AACAP Work Group on Quality Issues. Practice parameter for the assessment and treatment of children and adolescents with depressive disorders. J. Am. Acad. Child Adolesc. Psychiatry 2007, 46, 1503–1526. [Google Scholar] [CrossRef]
- Ryan, N.D. Treatment of depression in children and adolescents. Lancet 2005, 366, 933–940. [Google Scholar] [CrossRef]
- Guideline Development Panel for the Treatment of Depressive Disorders. Clinical Practice Guideline for the Treatment of Depression Across Three Age Cohorts; APA: Washington, DC, USA, 2019. [Google Scholar]
- Weisz, J.R.; Doss, A.J.; Hawley, K.M. Youth psychotherapy outcome research: A review and critique of the evidence base. Annu. Rev. Psychol. 2005, 56, 337–363. [Google Scholar] [CrossRef]
- Weisz, J.R.; Kuppens, S.; Eckshtain, D.; Ugueto, A.M.; Hawley, K.M.; Jensen-Doss, A. Performance of evidence-based youth psychotherapies compared with usual clinical care: A multilevel meta-analysis. JAMA Psychiatry 2013, 70, 750–761. [Google Scholar] [CrossRef]
- Klein, J.B.; Jacobs, R.H.; Reinecke, M.A. Cognitive-behavioral therapy for adolescent depression: A meta-analytic investigation of changes in effect-size estimates. J. Am. Acad. Child Adolesc. Psychiatry 2007, 46, 1403–1413. [Google Scholar] [CrossRef] [PubMed]
- Zhou, X.; Hetrick, S.E.; Cuijpers, P.; Qin, B.; Barth, J.; Whittington, C.J.; Cohen, D.; Del Giovane, C.; Liu, Y.; Michael, K.D. Comparative efficacy and acceptability of psychotherapies for depression in children and adolescents: A systematic review and network meta-analysis. World Psychiatry 2015, 14, 207–222. [Google Scholar] [CrossRef] [PubMed]
- Watanabe, N.; Hunot, V.; Omori, I.M.; Churchill, R.; Furukawa, T.A. Psychotherapy for depression among children and adolescents: A systematic review. Acta Psychiatr. Scand. 2007, 116, 84–95. [Google Scholar] [CrossRef] [PubMed]
- De Haan, A.M.; Boon, A.E.; De Jong, J.T.V.M.; Hoeve, M.; Vermeiren, R.R.J.M. A meta-analytic review on treatment dropout in child and adolescent outpatient mental health care. Clin. Psychol. Rev. 2013, 33, 698–711. [Google Scholar] [CrossRef] [PubMed]
- Gulliver, A.; Griffiths, K.M.; Christensen, H. Perceived barriers and facilitators to mental health help-seeking in young people: A systematic review. BMC Psychiatry 2010, 10, 113. [Google Scholar] [CrossRef] [PubMed]
- Calear, A.L.; Christensen, H. Review of internet-based prevention and treatment programs for anxiety and depression in children and adolescents. Med. J. Aust. 2010, 192, S12–S14. [Google Scholar] [CrossRef] [PubMed]
- Ebert, D.D.; Zarski, A.-C.; Christensen, H.; Stikkelbroek, Y.; Cuijpers, P.; Berking, M.; Riper, H. Internet and computer-based cognitive behavioral therapy for anxiety and depression in youth: A meta-analysis of randomized controlled outcome trials. PLoS ONE 2015, 10, e0119895. [Google Scholar] [CrossRef]
- Andersson, G.; Titov, N. Advantages and limitations of Internet-based interventions for common mental disorders. World Psychiatry 2014, 13, 4–11. [Google Scholar] [CrossRef]
- Fleming, T.M.; Bavin, L.; Stasiak, K.; Hermansson-Webb, E.; Merry, S.N.; Cheek, C.; Lucassen, M.; Lau, H.M.; Pollmuller, B.; Hetrick, S.E. Serious games and gamification for mental health: Current status and promising directions. Front. Psychiatry 2017, 7, 215. [Google Scholar] [CrossRef]
- Carlbring, P.; Andersson, G.; Cuijpers, P.; Riper, H.; Hedman-Lagerlöf, E. Internet-based vs. face-to-face cognitive behavior therapy for psychiatric and somatic disorders: An updated systematic review and meta-analysis. Cogn. Behav. Ther. 2018, 47, 1–18. [Google Scholar] [CrossRef]
- So, M.; Yamaguchi, S.; Hashimoto, S.; Sado, M.; Furukawa, T.A.; McCrone, P. Is computerised CBT really helpful for adult depression? A meta-analytic re-evaluation of CCBT for adult depression in terms of clinical implementation and methodological validity. BMC Psychiatry 2013, 13, 113. [Google Scholar] [CrossRef] [PubMed]
- Mathiasen, K.; Andersen, T.E.; Riper, H.; Kleiboer, A.A.M.; Roessler, K.K. Blended CBT versus face-to-face CBT: A randomised non-inferiority trial. BMC Psychiatry 2016, 16, 432. [Google Scholar] [CrossRef] [PubMed]
- Erbe, D.; Eichert, H.C.; Riper, H.; Ebert, D.D. Blending face-to-face and internet-based interventions for the treatment of mental disorders in adults: Systematic review. J. Med. Internet Res. 2017, 19, e306. [Google Scholar] [CrossRef] [PubMed]
- Kenter, R.M.F.; Van de Ven, P.M.; Cuijpers, P.; Koole, G.; Niamat, S.; Gerrits, R.S.; Willems, M.; Van Straten, A. Costs and effects of Internet cognitive behavioral treatment blended with face-to-face treatment: Results from a naturalistic study. Internet Interv. 2015, 2, 77–83. [Google Scholar] [CrossRef]
- Perle, J.G.; Langsam, L.C.; Nierenberg, B. Controversy clarified: An updated review of clinical psychology and tele-health. Clin. Psychol. Rev. 2011, 31, 1247–1258. [Google Scholar] [CrossRef] [PubMed]
- Donovan, C.L.; Poole, C.; Boyes, N.; Redgate, J.; March, S. Australian mental health worker attitudes towards cCBT: What is the role of knowledge? Are there differences? Can we change them? Internet Interv. 2015, 2, 372–381. [Google Scholar] [CrossRef]
- Waller, R.; Gilbody, S. Barriers to the uptake of computerized cognitive behavioural therapy: A systematic review of the quantitative and qualitative evidence. Psychol. Med. 2009, 39, 705–712. [Google Scholar] [CrossRef]
- Mora, L.; Nevid, J.; Chaplin, W. Psychologist treatment recommendations for Internet-based therapeutic interventions. Comput. Hum. Behav. 2008, 24, 3052–3062. [Google Scholar] [CrossRef]
- Abeles, P.; Verduyn, C.; Robinson, A.; Smith, P.; Yule, W.; Proudfoot, J. Computerized CBT for adolescent depression (“stressbusters”) and its initial evaluation through an extended case series. Behav. Cogn. Psychother. 2009, 37, 151–165. [Google Scholar] [CrossRef]
- Bradley, K.L.; Robinson, L.M.; Brannen, C.L. Adolescent help-seeking for psychological distress, depression, and anxiety using an internet program. Int. J. Ment. Health Promot. 2012, 14, 23–34. [Google Scholar] [CrossRef]
- Davidson, T.M.; Yuen, E.K.; Felton, J.W.; McCauley, J.; Gros, K.S.; Ruggiero, K.J. Feasibility assessment of a brief, web-based behavioral activation intervention for adolescents with depressed mood. Int. J. Psychiatry Med. 2014, 48, 69–82. [Google Scholar] [CrossRef] [PubMed]
- Logsdon, C.M.; Myers, J.; Rushton, J.; Gregg, J.L.; Josephson, A.M.; Davis, D.W.; Brothers, K.; Baisch, K.; Carabello, A.; Vogt, K.; et al. Efficacy of an Internet-based depression intervention to improve rates of treatment in adolescent mothers. Arch. Womens Ment. Health 2018, 21, 273–285. [Google Scholar] [CrossRef] [PubMed]
- Rickhi, B.; Kania-Richmond, A.; Moritz, S.; Cohen, J.; Paccagnan, P.; Dennis, C.; Liu, M.; Malhotra, S.; Steele, P.; Toews, J. Evaluation of a spirituality informed e-mental health tool as an intervention for major depressive disorder in adolescents and young adults–a randomized controlled pilot trial. BMC Complement. Altern. Med. 2015, 15, 450. [Google Scholar] [CrossRef] [PubMed]
- Smith, P.; Scott, R.; Eshkevari, E.; Jatta, F.; Leigh, E.; Harris, V.; Robinson, A.; Abeles, P.; Proudfoot, J.; Verduyn, C.; et al. Computerised CBT for depressed adolescents: Randomised controlled trial. Behav. Res. Ther. 2015, 73, 104–110. [Google Scholar] [CrossRef] [PubMed]
- Stasiak, K.; Hatcher, S.; Frampton, C.M.A.; Merry, S.N. A pilot double blind randomized placebo controlled trial of a prototype computer-based cognitive behavioural therapy program for adolescents with symptoms of depression. Behav. Cogn. Psychother. 2014, 42, 385–401. [Google Scholar] [CrossRef] [PubMed]
- Vangberg, H.C.B.; Lillevoll, K.R.; Waterloo, K.; Eisemann, M. Does Personality Predict Depression and Use of an Internet-Based Intervention for Depression among Adolescents? Depress. Res. Treat. 2012, 2012, 593068. [Google Scholar] [CrossRef]
- Wright, B.; Tindall, L.; Littlewood, E.; Allgar, V.; Abeles, P.; Trépel, D.; Ali, S. Computerised cognitive-behavioural therapy for depression in adolescents: Feasibility results and 4-month outcomes of a UK randomised controlled trial. BMJ Open 2017, 7, e012834. [Google Scholar] [CrossRef]
- Berg, M.; Rozental, A.; Johansson, S.; Liljethörn, L.; Radvogin, E.; Topooco, N.; Andersson, G. The role of knowledge in internet-based cognitive behavioural therapy for adolescent depression: Results from a randomised controlled study. Internet Interv. 2019, 15, 10–17. [Google Scholar] [CrossRef]
- Johnston, L.; Dear, B.F.; Gandy, M.; Fogliati, V.J.; Kayrouz, R.; Sheehan, J.; Rapee, R.M.; Titov, N. Exploring the efficacy and acceptability of internet-delivered cognitive behavioural therapy for young adults with anxiety and depression: An open trial. Aust. N. Z. J. Psychiatry 2014, 48, 819–827. [Google Scholar] [CrossRef]
- Kurki, M.; Anttila, M.; Koivunen, M.; Marttunen, M.; Välimäki, M. Nurses’ experiences of the use of an Internet-based support system for adolescents with depressive disorders. Inf. Health Soc. Care 2018, 43, 234–247. [Google Scholar] [CrossRef]
- O’Kearney, R.; Gibson, M.; Christensen, H.; Griffiths, K.M. Effects of a cognitive-behavioural internet program on depression, vulnerability to depression and stigma in adolescent males: A school-based controlled trial. Cogn. Behav. Ther. 2006, 35, 43–54. [Google Scholar] [CrossRef] [PubMed]
- Stallard, P.; Richardson, T.; Velleman, S.; Attwood, M. Computerized CBT (Think, Feel, Do) for depression and anxiety in children and adolescents: Outcomes and feedback from a pilot randomized controlled trial. Behav. Cogn. Psychother. 2011, 39, 273–284. [Google Scholar] [CrossRef] [PubMed]
- Topooco, N.; Berg, M.; Johansson, S.; Liljethörn, L.; Radvogin, E.; Vlaescu, G.; Nordgren, L.B.; Zetterqvist, M.; Andersson, G. Chat- and internet-based cognitive-behavioural therapy in treatment of adolescent depression: Randomised controlled trial. BJPsych Open 2018, 4, 199–207. [Google Scholar] [CrossRef] [PubMed]
- Van der Zanden, R.; Kramer, J.; Gerrits, R.; Cuijpers, P. Effectiveness of an online group course for depression in adolescents and young adults: A randomized trial. J. Med. Internet Res. 2012, 14, 296–309. [Google Scholar] [CrossRef] [PubMed]
- De Vos, R.; Tromp, N.; Bodden, D.; Stikkelbroek, Y. Therapeut onmisbaar bij ‘blended therapie’tegen depressie. Kind Adolesc. Prakt. 2017, 16, 6–13. [Google Scholar] [CrossRef]
- Kobak, K.A.; Mundt, J.C.; Kennard, B. Integrating technology into cognitive behavior therapy for adolescent depression: A pilot study. Ann. Gen. Psychiatry 2015, 14, 37. [Google Scholar] [CrossRef]
- Sethi, S. Treating youth depression and anxiety: A randomised controlled trial examining the efficacy of computerised versus face-to-face cognitive behaviour therapy. Aust. Psychol. 2013, 48, 249–257. [Google Scholar] [CrossRef]
- Sethi, S.; Campbell, A.J.; Ellis, L.A. The use of computerized self-help packages to treat adolescent depression and anxiety. J. Technol. Hum. Serv. 2010, 28, 144–160. [Google Scholar] [CrossRef]
- Bobier, C.; Stasiak, K.; Mountford, H.; Merry, S.N.; Moor, S. When ‘e’ therapy enters the hospital: Examination of the feasibility and acceptability of SPARX (a cCBT programme) in an adolescent inpatient unit. Adv. Ment. Health 2013, 11, 286–292. [Google Scholar] [CrossRef]
- Cheek, C.; Bridgman, H.; Fleming, T.M.; Cummings, E.; Ellis, L.; Lucassen, M.F.G.; Shepherd, M.J.; Skinner, T. Views of Young People in Rural Australia on SPARX, a Fantasy World Developed for New Zealand Youth With Depression. JMIR Serious Games 2014, 2, e3. [Google Scholar] [CrossRef]
- Fleming, T.M.; Dixon, R.; Frampton, C.M.A.; Merry, S.N. A pragmatic randomized controlled trial of computerized CBT (SPARX) for symptoms of depression among adolescents excluded from mainstream education. Behav. Cogn. Psychother. 2012, 40, 529–541. [Google Scholar] [CrossRef]
- Lucassen, M.F.G.; Hatcher, S.; Fleming, T.M.; Stasiak, K.; Shepherd, M.J.; Merry, S.N. A qualitative study of sexual minority young people’s experiences of computerised therapy for depression. Australas. Psychiatry 2015, 23, 268–273. [Google Scholar] [CrossRef] [PubMed]
- Lucassen, M.F.G.; Hatcher, S.; Stasiak, K.; Fleming, T.M.; Shepherd, M.J.; Merry, S.N. The views of lesbian, gay and bisexual youth regarding computerised self-help for depression: An exploratory study. Adv. Ment. Health 2013, 12, 22–33. [Google Scholar] [CrossRef]
- Lucassen, M.F.G.; Merry, S.N.; Hatcher, S.; Frampton, C.M.A. Rainbow SPARX: A novel approach to addressing depression in sexual minority youth. Cogn. Behav. Prac. 2015, 22, 203–216. [Google Scholar] [CrossRef]
- Lucassen, M.F.G.; Samra, R.; Iacovides, I.; Fleming, T.M.; Shepherd, M.J.; Stasiak, K.; Wallace, L. How LGBT+ Young People Use the Internet in Relation to Their Mental Health and Envisage the Use of e-Therapy: Exploratory Study. JMIR Serious Games 2018, 6, e11249. [Google Scholar] [CrossRef]
- Merry, S.N.; Stasiak, K.; Shepherd, M.J.; Frampton, C.M.A.; Fleming, T.M.; Lucassen, M.F.G. The effectiveness of SPARX, a computerised self help intervention for adolescents seeking help for depression: Randomised controlled non-inferiority trial. BMJ 2012, 344, e2598. [Google Scholar] [CrossRef]
- Forchuk, C.; Reiss, J.; Eichstedt, J.; Singh, D.; Collins, K.; Rudnick, A.; Walsh, J.; Ethridge, P.; Kutcher, S.; Fisman, S. The youth-mental health engagement network: An exploratory pilot study of a smartphone and computer-based personal health record for youth experiencing depressive symptoms. Int. J. Ment. Health 2016, 45, 205–222. [Google Scholar] [CrossRef]
- Sundram, F.; Hawken, S.J.; Stasiak, K.; Lucassen, M.F.G.; Fleming, T.M.; Shepherd, M.J.; Greenwood, A.; Osborne, R.; Merry, S.N. Tips and Traps: Lessons From Codesigning a Clinician E-Monitoring Tool for Computerized Cognitive Behavioral Therapy. JMIR Ment. Health 2017, 4, e3. [Google Scholar] [CrossRef]
- Bradford, S.; Rickwood, D. Adolescent’s preferred modes of delivery for mental health services. Child Adolesc. Ment. Health 2014, 19, 39–45. [Google Scholar] [CrossRef]
- Kurki, M.; Koivunen, M.; Anttila, M.; Hätönen, H.; Välimäki, M. Usefulness of internet in adolescent mental health outpatient care. J. Psychiatr. Ment. Health Nurs. 2011, 18, 265–273. [Google Scholar] [CrossRef]
- Lokkerbol, J.; Geomini, A.; Van Voorthuijsen, J.; Van Straten, A.; Tiemens, B.; Smit, F.; Risseeuw, A.; Hiligsmann, M. A discrete-choice experiment to assess treatment modality preferences of patients with depression. J. Med. Econ. 2018, 22, 178–186. [Google Scholar] [CrossRef]
- Lauver, D.R.; Ward, S.E.; Heidrich, S.M.; Keller, M.L.; Bowers, B.J.; Brennan, P.F.; Kirchhoff, K.T.; Wells, T.J.J. Patient-centered interventions. Res. Nurs. Health 2002, 25, 246–255. [Google Scholar] [CrossRef]
- Fairburn, C.G.; Patel, V. The impact of digital technology on psychological treatments and their dissemination. Behav. Res. Ther. 2017, 88, 19–25. [Google Scholar] [CrossRef]
- Topooco, N.; Riper, H.; Araya, R.; Berking, M.; Brunn, M.; Chevreul, K.; Cieslak, R.; Ebert, D.D.; Etchmendy, E.; Herrero, R. Attitudes towards digital treatment for depression: A European stakeholder survey. Internet Interv. 2017, 8, 1–9. [Google Scholar] [CrossRef]
- Richards, D.; Richardson, T. Computer-based psychological treatments for depression: A systematic review and meta-analysis. Clin. Psychol. Rev. 2012, 32, 329–342. [Google Scholar] [CrossRef]
- Johansson, R.; Andersson, G. Internet-based psychological treatments for depression. Expert Rev. Neurother. 2012, 12, 861–870. [Google Scholar] [CrossRef]
- Wolak, J.; Mitchell, K.J.; Finkelhor, D. Escaping or connecting? Characteristics of youth who form close online relationships. J. Adolesc. 2003, 26, 105–119. [Google Scholar] [CrossRef]
- Gross, E.F. Adolescent Internet use: What we expect, what teens report. J. Appl. Dev. Psychol. 2004, 25, 633–649. [Google Scholar] [CrossRef]
- Landelijke Stuurgroep Multidisciplinaire Richtlijnontwikkeling in de GGZ. Guidelines for Youth Depression Richtlijn Voor Depressie Bij Jeugd, Addendum; Trimbos Institute: Utrecht, The Netherlands, 2009. [Google Scholar]
- Van Straten, A.; Seekles, W.; Van ‘t Veer-Tazelaar, N.J.; Beekman, A.T.F.; Cuijpers, P. Stepped care for depression in primary care: What should be offered and how? Med. J. Aust. 2010, 192, S36–S39. [Google Scholar] [CrossRef]
- Weisz, J.R.; Weiss, B.; Donenberg, G.R. The lab versus the clinic: Effects of child and adolescent psychotherapy. Am. Psychol. 1992, 47, 1578. [Google Scholar] [CrossRef]
- Gibbons, C.J.; Fournier, J.C.; Stirman, S.W.; DeRubeis, R.J.; Crits-Christoph, P.; Beck, A.T. The clinical effectiveness of cognitive therapy for depression in an outpatient clinic. J. Affect. Disord. 2010, 125, 169–176. [Google Scholar] [CrossRef]
- Littlewood, E.; Duarte, A.; Hewitt, C.; Knowles, S.; Palmer, S.; Walker, S.; Andersen, P.; Araya, R.; Barkham, M.; Bower, P. A randomised controlled trial of computerised cognitive behaviour therapy for the treatment of depression in primary care: The Randomised Evaluation of the Effectiveness and Acceptability of Computerised Therapy (REEACT) trial. Health Technol. Assess. 2015, 19, 1. [Google Scholar] [CrossRef]
- Hollinghurst, S.; Peters, T.J.; Kaur, S.; Wiles, N.; Lewisand, G.; Kessler, D. Cost-effectiveness of therapist-delivered online cognitive–behavioural therapy for depression: Randomised controlled trial. Br. J. Psychiatry 2010, 197, 297–304. [Google Scholar] [CrossRef]
- Paganini, S.; Teigelkoetter, W.; Buntrock, C.; Baumeister, H. Economic evaluations of internet-and mobile-based interventions for the treatment and prevention of depression: A systematic review. J. Affect. Disord. 2018, 225, 733–755. [Google Scholar] [CrossRef]
- Simon, G.E.; Perlis, R.H. Personalized medicine for depression: Can we match patients with treatments? Am. J. Psychiatry 2010, 167, 1445–1455. [Google Scholar] [CrossRef]
- Huibers, M.J.H.; Cohen, Z.D.; Lemmens, L.H.J.M.; Arntz, A.; Peeters, F.P.M.L.; Cuijpers, P.; DeRubeis, R.J. Predicting optimal outcomes in cognitive therapy or interpersonal psychotherapy for depressed individuals using the personalized advantage index approach. PLoS ONE 2015, 10, e0140771. [Google Scholar] [CrossRef]
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).