Assessment of Nutritional Status and Dietary Pattern of a Rural Adult Population in Dry Zone, Sri Lanka
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Participant Recruitment
2.2. Data Collection and Tools
2.2.1. Socio-Demographic Data
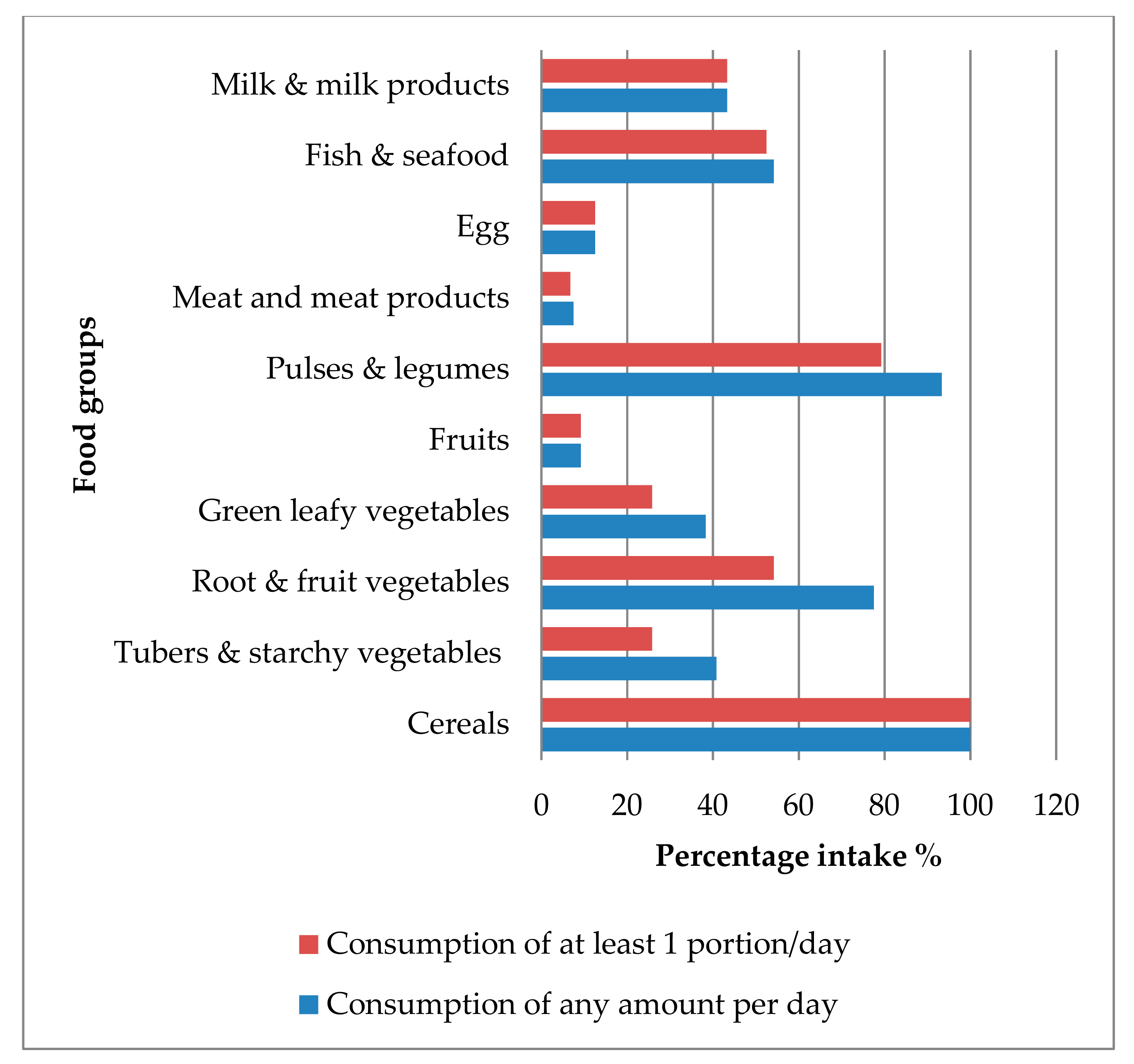
2.2.2. Dietary Data
2.2.3. Physical Activity Data
2.2.4. Anthropometric Measurements
2.3. Nutritional Status Indicators
2.4. Dietary Diversity Indicators
2.5. Statistical Analyses
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Weerahewa, J.W.C.; Babu, S.; Atapattu, N. Food Policies and Nutrition Transition in Sri Lanka: Historical Trends, Political Regimes, and Options for Interventions; International Food Policy Research Institute (IFPRI): Washington, DC, USA, 2018. [Google Scholar]
- Katulanda, P.C.G.; Mahesh, J.G.; Sheriff, R.; Seneviratne, R.D.A.; Wijeratne, S.; Wijesuriya, M.; McCarthy, M.I.; Adler, A.I.; Matthews, D.R. Prevalence and projections of diabetes and pre-diabetes in adults in Sri Lanka—Sri Lanka diabetes, cardiovascular study (SLDCS). Diabet. Med. 2008, 25, 1062–1069. [Google Scholar] [CrossRef] [PubMed]
- Katulanda, P.R.P.; Jayawardena, R.; Sheriff, R.; Matthews, D. Metabolic syndrome among Sri Lankan adults: Prevalence, patterns and correlates. Diabetol. Metab. Syndr. 2012, 4, 24. [Google Scholar] [CrossRef] [PubMed]
- Rajapakse, S.; Shivanthan, M.C.; Selvarajah, M. Chronic kidney disease of unknown etiology in Sri Lanka. Int. J. Occup. Environ. Health 2016, 22, 259–264. [Google Scholar] [CrossRef] [PubMed]
- Jayasumana, C.; Orantes, C.; Herrera, R.; Almaguer, M.; Lopez, L.; Silva, L.C.; Ordunez, P.; Siribaddana, S.; Gunatilake, S.; De Broe, M.E. Chronic interstitial nephritis in agricultural communities: A worldwide epidemic with social, occupational and environmental determinants. Nephrol. Dial. Transplant. Off. Publ. Eur. Dial. Transpl. Assoc.-Eur. Ren. Assoc. 2017, 32, 234–241. [Google Scholar] [CrossRef] [PubMed]
- Jayatilake, N.; Mendis, S.; Maheepala, P.; Mehta, F.R. Chronic kidney disease of uncertain aetiology: Prevalence and causative factors in a developing country. BMC Nephrol. 2013, 14, 180. [Google Scholar] [CrossRef]
- FAO. Conducting Small Scale Nutrition Surveys: A Field Manual; Policy and Nutrition Division: Rome, Italy, 1990. [Google Scholar]
- Katulanda, P.; Jayawardena, M.A.; Sheriff, M.H.; Constantine, G.R.; Matthews, D.R. Prevalence of overweight and obesity in Sri Lankan adults. Obes. Rev. Off. J. Int. Assoc. Study Obes. 2010, 11, 751–756. [Google Scholar] [CrossRef]
- Anne, S.; Paula, B. Household Dietary Diversity Score (HDDS) for Measurement of Household Food Access: Indicator Guide; 20009-5721; Food and Nutrition Technical Assistance Project (FANTA), Academy for educational development: Washington, DC, USA, 2006. [Google Scholar]
- IPAQ. Guidelines for Data Processing and Analysis of the International Physical Activity Questionnaire (IPAQ). 2005. Available online: http://www.ipaq.ki.se/scoring.pdf (accessed on 15 March 2010).
- WHO. Waist Circumference and Waist–Hip Ratio: Report of a WHO Expert Consultation; WHO Document Production Services: Geneva, Switzerland, 2008. [Google Scholar]
- WHO. Physical status: The use and interpretation of anthropometry. In Report of a WHO Expert Committee; Technical Report Series No. 854; WHO: Geneva, Switzerland, 1995. [Google Scholar]
- Mancia, G.; De Backer, G.; Dominiczak, A.; Cifkova, R.; Fagard, R.; Germano, G.; Grassi, G.; Heagerty, A.M.; Kjeldsen, S.E.; Laurent, S.; et al. 2007 Guidelines for the management of arterial hypertension: The Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). Eur. Heart J. 2007, 28, 1462–1536. [Google Scholar] [CrossRef]
- Shechtman, O.S.B. Grip Strength. In Clinical Assessment Recommendations, 3rd ed.; MacDermid, J., Solomon, G., Valdes, K., Mount Laurel, N.J., American Society of Hand Therapists, Eds.; American Society of Hand Therapists: Bethesda, MD, USA, 2015. [Google Scholar]
- Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet (Lond. Engl.) 2004, 363, 157–163. [CrossRef]
- IDF. The IDF Consensus: Worldwide Definition of the Metabolic Syndrome; IDF: Brussels, Belgium, 2006. [Google Scholar]
- Ashwell, M.; Gibson, S. Waist to height ratio is a simple and effective obesity screening tool for cardiovascular risk factors: Analysis of data from the British National Diet and Nutrition Survey of adults aged 19–64 years. Obes. Facts 2009, 2, 97–103. [Google Scholar] [CrossRef]
- Foote, J.A.; Murphy, S.P.; Wilkens, L.R.; Basiotis, P.P.; Carlson, A. Dietary variety increases the probability of nutrient adequacy among adults. J. Nutr. 2004, 134, 1779–1785. [Google Scholar] [CrossRef]
- Mirmiran, P.; Azadbakht, L.; Azizi, F. Dietary diversity within food groups: An indicator of specific nutrient adequacy in Tehranian women. J. Am. Coll. Nutr. 2006, 25, 354–361. [Google Scholar] [CrossRef] [PubMed]
- Working Group on Infant and Young Child Feeding Indicators. Developing and Validating Simple Indicators of Dietary Quality and Energy Intake of Infants and Young Children in Developing Countries: Summary of Findings from Analysis of 10 Data Sets; Food and Nutrition Technical Assistance Project (FANTA): FHI 360: Washington, DC, USA, August 2006. [Google Scholar]
- Kennedy, G.; Ballard, T.; Dop, M. Guidelines for Measuring Household and Individual Dietary Diversity; EC-FAO: Rome, Italy, 2010. [Google Scholar]
- Swindale, A.; Bilinsky, P. Household Dietary Diversity Score (HDDS) for Measurement of Household Food Access: Indicator Guide; Food and Nutrition Technical Assistance III Project: Washington, DC, USA, 2006. [Google Scholar]
- Nutrition Division: Ministry of Health Care and Nutrition. Food Based Dietary Guidelines for Sri Lanka, 2nd ed.; Nutrition Division: Ministry of Health Care and Nutrition: Colombo, Sri Lanka, 2011.
- Jayawardena, R.; Byrne, N.M.; Soares, M.J.; Katulanda, P.; Yadav, B.; Hills, A.P. High dietary diversity is associated with obesity in Sri Lankan adults: An evaluation of three dietary scores. BMC Public Health 2013, 13, 314. [Google Scholar] [CrossRef] [PubMed]
- Rathnayake, K.M.; Madushani, P.; Silva, K. Use of dietary diversity score as a proxy indicator of nutrient adequacy of rural elderly people in Sri Lanka. BMC Res. Notes 2012, 5, 469. [Google Scholar] [CrossRef] [PubMed]
- Jayawardena, R.; Byrne, N.M.; Soares, M.J.; Katulanda, P.; Hills, A.P. Food consumption of Sri Lankan adults: An appraisal of serving characteristics. Public Health Nutr. 2013, 16, 653–658. [Google Scholar] [CrossRef]
- Department of Census & Statistics-Sri Lanka. Official poverty line by district: January 2019. Available online: http://www.statistics.gov.lk/poverty/monthly_poverty/index.htm (accessed on 3 March 2019).
- Ranasinghe, C.; Gamage, P.; Katulanda, P.; Andraweera, N.; Thilakarathne, S.; Tharanga, P. Relationship between Body mass index (BMI) and body fat percentage, estimated by bioelectrical impedance, in a group of Sri Lankan adults: A cross sectional study. BMC Public Health 2013, 13, 797. [Google Scholar] [CrossRef]
- Jin, M.; Du, H.; Zhang, Y.; Zhu, H.; Xu, K.; Yuan, X.; Pan, H.; Shan, G. Characteristics and reference values of fat mass index and fat free mass index by bioelectrical impedance analysis in an adult population. Clin. Nutr. (Edinb. Scotl.) 2018. [Google Scholar] [CrossRef]
- Liu, P.; Ma, F.; Lou, H.; Liu, Y. The utility of fat mass index vs. body mass index and percentage of body fat in the screening of metabolic syndrome. BMC Public Health 2013, 13, 629. [Google Scholar] [CrossRef]
- Wang, D.; Li, Y.; Lee, S.G.; Wang, L.; Fan, J.; Zhang, G.; Wu, J.; Ji, Y.; Li, S. Ethnic differences in body composition and obesity related risk factors: Study in Chinese and white males living in China. PLoS ONE 2011, 6, e19835. [Google Scholar] [CrossRef]
- Norman, K.; Stobaus, N.; Gonzalez, M.C.; Schulzke, J.D.; Pirlich, M. Hand grip strength: Outcome predictor and marker of nutritional status. Clin. Nutr. (Edinb. Scotl.) 2011, 30, 135–142. [Google Scholar] [CrossRef]
- Massy-Westropp, N.M.; Gill, T.K.; Taylor, A.W.; Bohannon, R.W.; Hill, C.L. Hand Grip Strength: Age and gender stratified normative data in a population-based study. BMC Res. Notes 2011, 4, 127. [Google Scholar] [CrossRef]
- Amaral, C.A.; Amaral, T.L.M.; Monteiro, G.T.R.; Vasconcellos, M.T.L.; Portela, M.C. Hand grip strength: Reference values for adults and elderly people of Rio Branco, Acre, Brazil. PLoS ONE 2019, 14, e0211452. [Google Scholar] [CrossRef] [PubMed]
- Mathiowetz, V.; Kashman, N.; Volland, G.; Weber, K.; Dowe, M.; Rogers, S. Grip and pinch strength: Normative data for adults. Arch. Phys. Med. Rehabil. 1985, 66, 69–74. [Google Scholar] [PubMed]
- Tveter, A.T.; Dagfinrud, H.; Moseng, T.; Holm, I. Health-related physical fitness measures: Reference values and reference equations for use in clinical practice. Arch. Phys. Med. Rehabil. 2014, 95, 1366–1373. [Google Scholar] [CrossRef] [PubMed]
- Werle, S.; Goldhahn, J.; Drerup, S.; Simmen, B.R.; Sprott, H.; Herren, D.B. Age- and Gender-Specific Normative Data of Grip and Pinch Strength in a Healthy Adult Swiss Population. J. Hand Surg. (Eur. Vol.) 2009, 84, 76–84. [Google Scholar] [CrossRef] [PubMed]
- Mohammadian, M.; Choobineh, A.; Haghdoost, A.; Hasheminejad, N. Normative data of grip and pinch strengths in healthy adults of Iranian population. Iran. J. Public Health 2014, 43, 1113–1122. [Google Scholar]
- Tsang, R.C.C. Reference Values for 6-Minute Walk Test and Hand-Grip Strength in Healthy Hong Kong Chinese Adults. Hong Kong Physiother. J. 2005, 23, 6–12. [Google Scholar] [CrossRef]
- Nurul Shahida, M.S.; Siti Zawiah, M.D.; Case, K. The relationship between anthropometry and hand grip strength among elderly Malaysians. Int. J. Ind. Ergon. 2015, 50, 17–25. [Google Scholar] [CrossRef]
- Adedoyin, R.A.; Ogundapo, F.A.; Mbada, C.E.; Adekanla, B.A.; Johnson, O.E.; Onigbinde, T.A.; Emechete, A.A.I. Reference Values for Handgrip Strength Among Healthy Adults in Nigeria. Hong Kong Physiother. J. 2009, 27, 21–29. [Google Scholar] [CrossRef]
- Bansal, N. Hand Grip Strength: Normative Data for Young Adults. Indian J. Phys. Occup. Ther. Int. J. 2008, 2, 29–33. [Google Scholar]
- Kamarul, T.; Ahmad, T.S.; Loh, W.Y. Hand grip strength in the adult Malaysian population. J. Orthop. Surg. (Hong Kong) 2006, 14, 172–177. [Google Scholar] [CrossRef]
- Katulanda, P.; Dissanayake, H.A.; De Silva, S.D.N.; Katulanda, G.W.; Liyanage, I.K.; Constantine, G.R.; Sheriff, R.; Matthews, D.R. Prevalence, patterns, and associations of dyslipidemia among Sri Lankan adults-Sri Lanka Diabetes and Cardiovascular Study in 2005-2006. J. Clin. Lipidol. 2018, 12, 447–454. [Google Scholar] [CrossRef] [PubMed]
- De Silva, A.P.; De Silva, S.H.; Haniffa, R.; Liyanage, I.K.; Jayasinghe, K.S.; Katulanda, P.; Wijeratne, C.N.; Wijeratne, S.; Rajapakse, L.C. A cross sectional survey on social, cultural and economic determinants of obesity in a low middle income setting. Int. J. Equity Health 2015, 14, 6. [Google Scholar] [CrossRef] [PubMed]
- Jayawardana, N.; Jayalath, W.; Madhujith, W.M.T.; Ralapanawa, U.; Jayasekera, R.S.; Alagiyawanna, S.; Bandara, A.; Kalupahana, N.S. Aging and obesity are associated with undiagnosed hypertension in a cohort of males in the Central Province of Sri Lanka: A cross-sectional descriptive study. BMC Cardiovasc. Disord. 2017, 17, 165. [Google Scholar] [CrossRef] [PubMed]
- Wijewardene, K.; Mohideen, M.; Mendis, S.; Fernando, D.; Kulathilaka, T.; Weerasekara, D.; Uluwitta, P. Prevalence of hypertension, diabetes and obesity: Baseline findings of a population based survey in four provinces in Sri Lanka. Ceylon Med. J. 2005, 50, 62–70. [Google Scholar] [CrossRef]
- Arambepola, C.; Allender, S.; Ekanayake, R.; Fernando, D. Urban living and obesity: Is it independent of its population and lifestyle characteristics? Trop. Med. Int. Health 2008, 13, 448–457. [Google Scholar] [CrossRef]
- Rathnayake, K.M.; Roopasingam, T.; Dibley, M.J. High carbohydrate diet and physical inactivity associated with central obesity among premenopausal housewives in Sri Lanka. BMC Res. Notes 2014, 7, 564. [Google Scholar] [CrossRef][Green Version]
- Jayawardana, R.; Ranasinghe, P.; Sheriff, M.H.; Matthews, D.R.; Katulanda, P. Waist to height ratio: A better anthropometric marker of diabetes and cardio-metabolic risks in South Asian adults. Diabetes Res. Clin. Pr. 2013, 99, 292–299. [Google Scholar] [CrossRef]
- Jayawardena, R.; Byrne, N.M.; Soares, M.J.; Katulanda, P.; Hills, A.P. Body weight perception and weight loss practices among Sri Lankan adults. Obes. Res. Clin. Pract. 2014, 8, e192–e200. [Google Scholar] [CrossRef]
- Jayatissa, R.; Moazzem Hossain, S.M.; Gunawardana, S.; Ranbanda, J.M.; Gunathilaka, M.; De Silva, P.C. Prevalence and associations of overweight among adult women in Sri Lanka: A national survey. Sri Lanka J. Diabetes Endocrinol. Metab. 2012, 2, 61–68. [Google Scholar] [CrossRef]
- Amarasinghe, S.; Sandrasegarampillai, B.; Arasaratnam, V. Metabolic syndrome among Jaffna Tamil community, Sri Lanka. Indian J. Endocrinol. Metab. 2015, 19, 663–666. [Google Scholar] [CrossRef]
- Owolabi, E.O.; Ter Goon, D.; Adeniyi, O.V. Central obesity and normal-weight central obesity among adults attending healthcare facilities in Buffalo City Metropolitan Municipality, South Africa: A cross-sectional study. J. HealthPopul. Nutr. 2017, 36. [Google Scholar] [CrossRef] [PubMed]
- Thaikruea, L.; Thammasarot, J. Prevalence of normal weight central obesity among Thai healthcare providers and their association with CVD risk: A cross-sectional study. Sci. Rep. 2016, 6, 37100. [Google Scholar] [CrossRef] [PubMed]
- Zhang, P.; Wang, R.; Gao, C.; Jiang, L.; Lv, X.; Song, Y.; Li, B. Prevalence of Central Obesity among Adults with Normal BMI and Its Association with Metabolic Diseases in Northeast China. PLoS ONE 2016, 11, e0160402. [Google Scholar] [CrossRef] [PubMed]
- Katulanda, P.; Jayawardena, M.A.; Sheriff, M.H.; Matthews, D.R. The distance between the lower edge of the xiphisternum and the center of the umbilicus as an indicator of abdominal obesity and cardiovascular disease risk. Obes Facts 2010, 3, 201–204. [Google Scholar] [CrossRef] [PubMed]
- Kasturiratne, A.; Warnakulasuriya, T.; Pinidiyapathirage, J.; Kato, N.; Wickremasinghe, R.; Pathmeswaran, A. P2-130 Epidemiology of hypertension in an urban Sri Lankan population. J. Epidemiol. Community Health 2011, 65, A256. [Google Scholar] [CrossRef][Green Version]
- Katulanda, P.; Ranasinghe, P.; Jayawardena, R.; Constantine, G.R.; Rezvi Sheriff, M.H.; Matthews, D.R. The prevalence, predictors and associations of hypertension in Sri Lanka: A cross-sectional population based national survey. Clin. Exp. Hypertens. 2014, 36, 484–491. [Google Scholar] [CrossRef] [PubMed]
- Gamage, A.; Seneviratne, R.; Hanna, F. Ps 17-23 physical inactivity as a predictor of hypertension among employees in Sri Lanka: a cross-sectional study. J. Hypertens. 2016, 34, e480. [Google Scholar] [CrossRef]
- Rathnayake, K.M.; Wimalathunga, M.; Weech, M.; Jackson, K.G.; Lovegrove, J.A. High prevalence of undernutrition and low dietary diversity in institutionalised elderly living in Sri Lanka. Public Health Nutr. 2015, 18, 2874–2880. [Google Scholar] [CrossRef]
- Siriwardhana, E.R.I.; Perera, P.A.; Sivakanesan, R.; Abeysekara, T.; Nugegoda, D.B.; Weerakoon, K.G. Is the staple diet eaten in Medawachchiya, Sri Lanka, a predisposing factor in the development of chronic kidney disease of unknown etiology?-A comparison based on urinary β2-microglobulin measurements. BMC Nephrol. 2014, 15, 103. [Google Scholar] [CrossRef]
- Jayawardena, R.; Thennakoon, S.; Byrne, N.; Soares, M.; Katulanda, P.; Hills, A. Energy and nutrient intakes among Sri Lankan adults. Int. Arch. Med. 2014, 7, 34. [Google Scholar] [CrossRef]
- Human energy requirements: Report of a joint FAO/ WHO/UNU Expert Consultation. Food Nutr. Bull. 2005, 26, 166.
- Diet, nutrition and the prevention of chronic diseases. World Health Organ. Tech. Rep. Ser. 2003, 916, 1–149.
| Variable | Frequency | Percentage (%) |
|---|---|---|
| Age | ||
| 18–29 | 17 | 14.2 |
| 30–39 | 38 | 31.7 |
| 40–49 | 19 | 15.8 |
| 50–59 | 15 | 12.5 |
| 60–70 | 22 | 18.3 |
| >70 | 9 | 7.5 |
| Education level | ||
| No proper education | 13 | 10.8 |
| Primary | 78 | 65 |
| Secondary | 25 | 20.8 |
| Tertiary | 4 | 3.3 |
| Marital status | ||
| Married | 108 | 90 |
| Divorced | 1 | 0.8 |
| Widowed | 6 | 5 |
| Unmarried | 5 | 4.2 |
| Number of family members | ||
| 1–2 | 13 | 10.8 |
| 3–5 | 66 | 55 |
| >5 | 41 | 34.2 |
| Monthly income (SLR) | ||
| <5000 | 8 | 6.7 |
| 5001–10,000 | 8 | 6.7 |
| 10,001–20,000 | 28 | 23.3 |
| 20,001–30,000 | 53 | 44.2 |
| 30,001–50,000 | 16 | 13.3 |
| >50,000 | 7 | 5.8 |
| On treatment for NCDs | ||
| Hypertension | 26 | 21.7 |
| Diabetes mellitus | 13 | 10.8 |
| Hypercholesterolemia | 15 | 12.5 |
| Coronary heart diseases | 4 | 3.3 |
| Chronic respiratory diseases | 9 | 7.5 |
| Health-related habits | ||
| Smoking cigarettes | 11 | 9.2 |
| Betel chewing | 47 | 39.2 |
| Drinking alcohol | 12 | 10 |
| Variable | Men (N = 38) | Women (N = 82) | Total (N = 120) | p-Value * | |||
|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | ||
| Age | 50.11 | 14.66 | 43.50 | 15.85 | 45.59 | 15.73 | 0.032 |
| SBP (mmHg) | 150.16 | 25.27 | 142.49 | 20.81 | 144.92 | 22.50 | 0.082 |
| DBP (mmHg) | 97.39 | 15.58 | 93.89 | 13.91 | 95.00 | 14.49 | 0.219 |
| Weight (kg) | 57.67 | 9.87 | 55.05 | 11.28 | 55.88 | 10.88 | 0.221 |
| Height (cm) | 161.39 | 6.08 | 153.04 | 7.23 | 155.68 | 7.89 | <0.001 |
| BMI (kg/m2) | 22.20 | 3.97 | 23.46 | 4.26 | 23.06 | 4.20 | 0.125 |
| % Body fat | 26.05 | 8.49 | 34.79 | 4.92 | 32.02 | 7.45 | <0.001 |
| % Body muscle | 30.38 | 4.93 | 24.93 | 2.32 | 26.65 | 4.21 | <0.001 |
| MUAC (cm) | 27.74 | 3.70 | 28.40 | 3.60 | 28.19 | 3.63 | 0.352 |
| WC (cm) | 84.79 | 9.38 | 85.96 | 9.53 | 85.59 | 9.46 | 0.529 |
| HC (cm) | 87.63 | 8.96 | 91.32 | 8.79 | 90.15 | 8.98 | 0.036 |
| WHR | 0.97 | 0.04 | 0.94 | 0.05 | 0.95 | 0.05 | 0.002 |
| WHtR | 0.53 | 0.06 | 0.56 | 0.07 | 0.55 | 0.07 | 0.005 |
| FMI (kg/m2) | 6.06 | 2.69 | 8.33 | 2.58 | 7.61 | 2.81 | <0.001 |
| HGS-L (kg) | 31.17 | 11.27 | 22.96 | 7.01 | 25.56 | 9.36 | <0.001 |
| HGS-R (kg) | 30.05 | 11.26 | 23.67 | 7.07 | 25.69 | 9.08 | 0.002 |
| Variable | Men n (%) | Women n (%) | Total n (%) | p-Value * |
|---|---|---|---|---|
| BMI category † | ||||
| Underweight | 7 (18.4) | 7 (8.5) | 14 (11.7) | 0.321 |
| Normal | 14 (36.8) | 33 (40.2) | 47 (39.2) | |
| Overweight | 14 (36.8) | 29 (35.4) | 43 (35.8) | |
| Obese | 3 (7.9) | 13 (15.9) | 16 (13.3) | |
| CO ‡ | ||||
| By WC | 12 (31.6) | 59 (72) | 71 (59.2) | <0.001 |
| By WHR | 37 (97.4) | 80 (97.6) | 117 (97.5) | 0.950 |
| By WHtR | 22 (57.9) | 67 (81.7) | 89 (74.2) | 0.006 |
| NWCO | ||||
| By WC | 1 (2.6) | 16 (19.5) | 17 (14.2) | 0.014 |
| By WHR | 13 (34.2) | 31 (37.8) | 44 (36.7) | 0.704 |
| By WHtR | 8 (21.1) | 21 (25.6) | 29 (24.2) | 0.588 |
| PA level | ||||
| Low | 12 (31.6) | 8 (9.8) | 20 (16.7) | 0.003 |
| Moderate | 5 (13.2) | 29 (35.4) | 34 (28.3) | |
| High | 21 (55.3) | 45 (54.9) | 66 (55) |
| Food Group | Mean Intake (SD) (Portion/Day) | National Recommendation [23] (Portion/Day) | % Meets National Recommendation |
|---|---|---|---|
| Cereals and equivalents | 10.90 (2.36) | 6–11 | 100 |
| Vegetables | 1.38 (1.07) | 3–5 | 8.3 |
| Fruits | 0.1 (0.35) | 2–3 | 1.7 |
| Fruits and vegetables | 1.48 (1.11) | ≥5 | 0.8 |
| Meat, fish, eggs and/or pulses | 2.76 (1.68) | 3–4 | 44.2 |
| Milk or milk products | 0.52 (0.65) | 1–2 | 43.3 |
| Added sugar | 3.08 (2.19) | Sparingly | 13.3 |
| Energy and Nutrient Intake | Male (N = 38) | Female (N = 82) | Total (N = 120) | p * | |||||
|---|---|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Min | Max | Mean | SD | ||
| Energy (kcal/day) | 1384.0 | 418.55 | 1415.56 | 396.49 | 677.40 | 2943.20 | 1430.18 | 387.63 | 0.555 |
| Energy (kcal/kg per day) | 26.11 | 7.78 | 26.13 | 8.36 | 11.55 | 47.88 | 26.14 | 8.66 | 0.986 |
| Protein (g/day) | 37.93 | 16.58 | 38.21 | 15.99 | 10.70 | 91.30 | 38.35 | 15.82 | 0.896 |
| Protein (g/kg per day) | 0.03 | 0.006 | 0.03 | 0.007 | 0.01 | 0.05 | 0.03 | 0.008 | 0.846 |
| Fat (g/day) | 32.39 | 21.87 | 29.75 | 19.68 | 1.30 | 100.10 | 28.52 | 18.59 | 0.318 |
| Carbohydrate (g/day) | 232.68 | 70.29 | 250.67 | 65.29 | 135.80 | 507.00 | 259.0 | 61.5 | 0.039 |
| Energy from protein (%) | 10.79 | 2.53 | 10.62 | 2.53 | 5.00 | 18.00 | 10.54 | 2.54 | 0.613 |
| Energy from fat (%) | 19.53 | 9.3 | 17.2 | 8.35 | 2.00 | 40.00 | 16.12 | 7.7 | 0.037 |
| Energy from carbohydrates (%) | 69.68 | 9.81 | 72.18 | 9.41 | 50.00 | 91.00 | 73.34 | 9.05 | 0.047 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Abeywickrama, H.M.; Wimalasiri, K.M.S.; Koyama, Y.; Uchiyama, M.; Shimizu, U.; Chandrajith, R.; Nanayakkara, N. Assessment of Nutritional Status and Dietary Pattern of a Rural Adult Population in Dry Zone, Sri Lanka. Int. J. Environ. Res. Public Health 2020, 17, 150. https://doi.org/10.3390/ijerph17010150
Abeywickrama HM, Wimalasiri KMS, Koyama Y, Uchiyama M, Shimizu U, Chandrajith R, Nanayakkara N. Assessment of Nutritional Status and Dietary Pattern of a Rural Adult Population in Dry Zone, Sri Lanka. International Journal of Environmental Research and Public Health. 2020; 17(1):150. https://doi.org/10.3390/ijerph17010150
Chicago/Turabian StyleAbeywickrama, Hansani Madushika, K. M. Swarna Wimalasiri, Yu Koyama, Mieko Uchiyama, Utako Shimizu, Rohana Chandrajith, and Nishantha Nanayakkara. 2020. "Assessment of Nutritional Status and Dietary Pattern of a Rural Adult Population in Dry Zone, Sri Lanka" International Journal of Environmental Research and Public Health 17, no. 1: 150. https://doi.org/10.3390/ijerph17010150
APA StyleAbeywickrama, H. M., Wimalasiri, K. M. S., Koyama, Y., Uchiyama, M., Shimizu, U., Chandrajith, R., & Nanayakkara, N. (2020). Assessment of Nutritional Status and Dietary Pattern of a Rural Adult Population in Dry Zone, Sri Lanka. International Journal of Environmental Research and Public Health, 17(1), 150. https://doi.org/10.3390/ijerph17010150






