Pre-Existing Disability and Its Risk of Fragility Hip Fracture in Older Adults
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Data Sources and Size
2.3. Participants
2.4. Variables
2.5. Statistical Methods
2.6. Ethics
3. Results
3.1. General Characteristics of Study Participants
3.2. General Characteristics of Patients with Hip Fracture
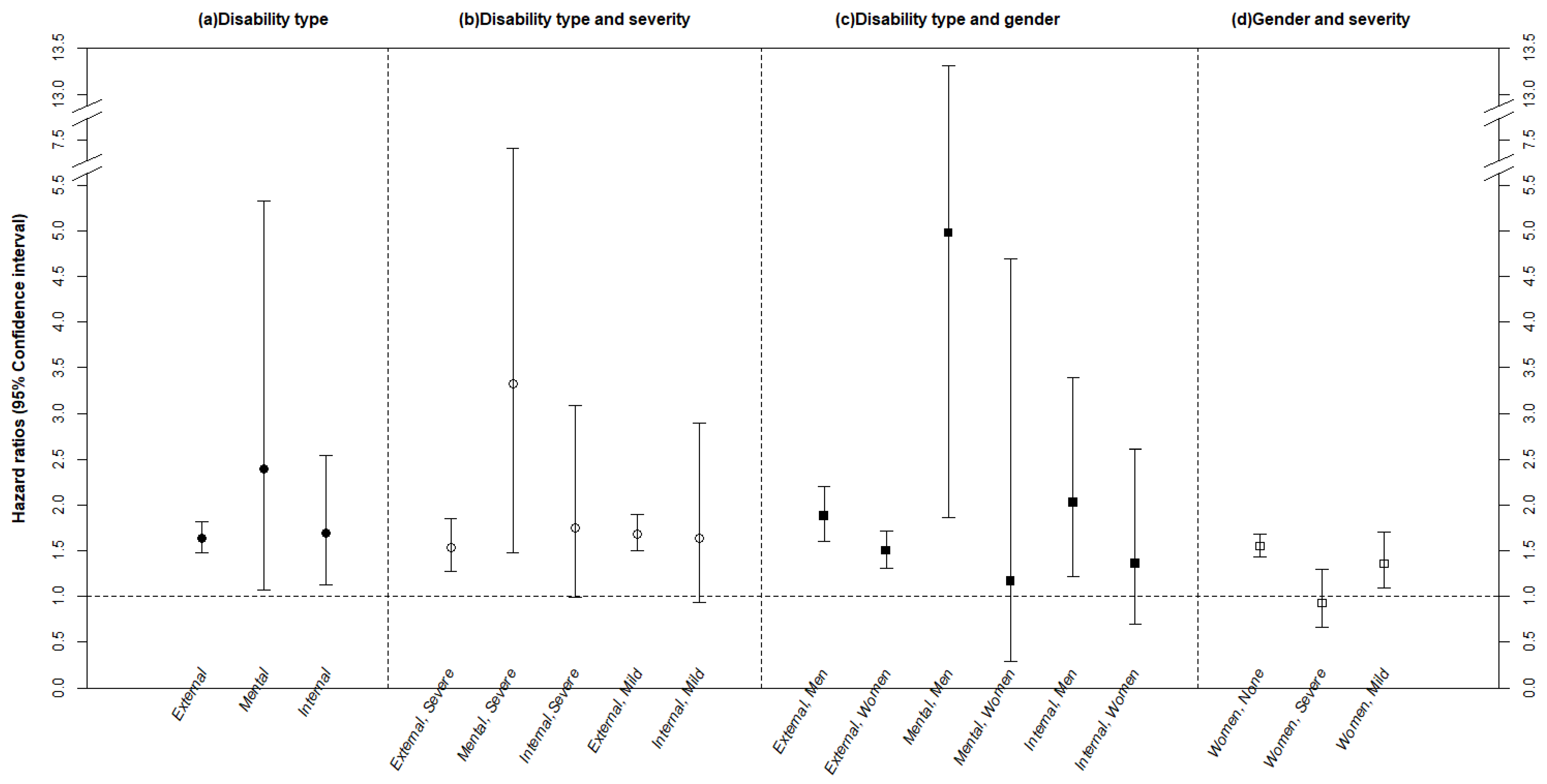
3.3. Hip Fractures: Disability Type And Severity, and Subgroup Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Jiménez-Mola, S.; Calvo-Lobo, C.; Idoate-Gil, J.; Seco-Calvo, J. Functionality, comorbidity, complication and surgery of hip fracture in older adults by age distribution. Rev. Assoc. Méd. Bras. 2018, 64, 420–427. [Google Scholar] [CrossRef] [PubMed]
- Jiménez, S.M.; Calvo-Lobo, C.; Idoate, J.G.; Seco, J.C. Cognitive Impairment Level and Elderly Hip Fracture: Implications in Rehabilitation Nursing. Rehabil. Nurs. Off. J. Assoc. Rehabil. Nur. 2018. [Google Scholar] [CrossRef]
- Smith, A.K.; Cenzer, I.S.; Boscardin, W.J.; Ritchie, C.S.; Wallhagen, M.L.; Covinsky, K.E. Increase in Disability Prevalence Before Hip Fracture. J. Am. Geriatr. Soc. 2015, 63, 2029–2035. [Google Scholar] [CrossRef]
- Kang, H.Y.; Park, S.E.; Kang, D.R.; Kim, J.Y.; Jang, Y.H.; Choi, W.J.; Moon, S.-H.; Yang, K.-H.; Park, J.-Y.; Kwon, S.-Y. Estimating medical expenditure associated with osteoporotic hip fracture in elderly Korean women based on the National Health Insurance Claims Database 2002–2004. Value Health 2009, 12, S93–S96. [Google Scholar] [CrossRef][Green Version]
- Veronese, N.; Maggi, S. Epidemiology and social costs of hip fracture. Injury 2018, 49, 1458–1460. [Google Scholar] [CrossRef]
- Lee, J.; Lee, J.S.; Park, S.H.; Shin, S.A.; Kim, K. Cohort Profile: The National Health Insurance Service-National Sample Cohort (NHIS-NSC), South Korea. Int. J. Epidemiol. 2016, 46, e15. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. The ICD-10 Classification of Mental and Behavioural Disorders: Clinical Descriptions and Diagnostic Guidelines; World Health Organization: Geneva, Switzerland, 1992. [Google Scholar]
- Charlson, M.; Szatrowski, T.P.; Peterson, J.; Gold, J. Validation of a combined comorbidity index. J. Clin. Epidemiol. 1994, 47, 1245–1251. [Google Scholar] [CrossRef]
- Sundararajan, V.; Henderson, T.; Perry, C.; Muggivan, A.; Quan, H.; Ghali, W.A. New ICD-10 version of the Charlson comorbidity index predicted in-hospital mortality. J. Clin. Epidemiol. 2004, 57, 1288–1294. [Google Scholar] [CrossRef]
- Sundararajan, V.; Quan, H.; Halfon, P.; Fushimi, K.; Luthi, J.C.; Burnand, B.; Ghali, W.A. Cross-national comparative performance of three versions of the ICD-10 Charlson index. Med. Care 2007, 45, 1210–1215. [Google Scholar]
- Statistics Korea RoK. Korean Statistical Information Service. 2018; 2015 Census Data in South Korea. Available online: http://kosis.kr/statisticsList/statisticsListIndex.do?menuId=M_01_01&vwcd=MT_ZTITLE&parmTabId=M_01_01#SelectStatsBoxDiv (accessed on 10 June 2018).
- Zhang, X.; Loberiza, F.R.; Klein, J.P.; Zhang, M.J. A SAS macro for estimation of direct adjusted survival curves based on a stratified Cox regression model. Comput. Methods Programs Biomed. 2007, 88, 95–101. [Google Scholar] [CrossRef] [PubMed]
- Lobo, E.; Marcos, G.; Santabarbara, J.; Salvador-Roses, H.; Lobo-Escolar, L.; De la Camara, C.; Aso, A.; Lobo-Escolar, A.; Workgroup, Z. Gender differences in the incidence of and risk factors for hip fracture: A 16-year longitudinal study in a southern European population. Maturitas 2017, 97, 38–43. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Tseng, P.T.; Chen, Y.W.; Yeh, P.Y.; Tu, K.Y.; Cheng, Y.S.; Wu, C.K. Bone Mineral Density in Schizophrenia: An Update of Current Meta-Analysis and Literature Review Under Guideline of PRISMA. Medicine 2015, 94, e1967. [Google Scholar] [CrossRef] [PubMed]
- De Hert, M.; Detraux, J.; Stubbs, B. Relationship between antipsychotic medication, serum prolactin levels and osteoporosis/osteoporotic fractures in patients with schizophrenia: A critical literature review. Expert Opin. Drug Saf. 2016, 15, 809–823. [Google Scholar] [CrossRef] [PubMed]
- Gonzalez-Blanco, L.; Greenhalgh, A.M.D.; Garcia-Rizo, C.; Fernandez-Egea, E.; Miller, B.J.; Kirkpatrick, B. Prolactin concentrations in antipsychotic-naive patients with schizophrenia and related disorders: A meta-analysis. Schizophr. Res. 2016, 174, 156–160. [Google Scholar] [CrossRef] [PubMed]
- Kishimoto, T.; De Hert, M.; Carlson, H.E.; Manu, P.; Correll, C.U. Osteoporosis and fracture risk in people with schizophrenia. Curr. Opin. Psychiatry 2012, 25, 415–429. [Google Scholar] [CrossRef]
- Stubbs, B.; Gardner-Sood, P.; Smith, S.; Ismail, K.; Greenwood, K.; Farmer, R.; Gaughran, F. Sedentary behaviour is associated with elevated C-reactive protein levels in people with psychosis. Schizophr. Res. 2015, 168, 461–464. [Google Scholar] [CrossRef] [PubMed]
- Stubbs, B.; De Hert, M.; Sepehry, A.A.; Correll, C.U.; Mitchell, A.J.; Soundy, A.; Detraux, J.; Vancampfort, D. A meta-analysis of prevalence estimates and moderators of low bone mass in people with schizophrenia. Acta Psychiatr. Scand. 2014, 130, 470–486. [Google Scholar] [CrossRef] [PubMed]
- Gomez, L.; Stubbs, B.; Shirazi, A.; Vancampfort, D.; Gaughran, F.; Lally, J. Lower Bone Mineral Density at the Hip and Lumbar Spine in People with Psychosis Versus Controls: A Comprehensive Review and Skeletal Site-Specific Meta-analysis. Curr. Osteoporos. Rep. 2016, 14, 249–259. [Google Scholar] [CrossRef]
- Wu, C.S.; Chang, C.M.; Tsai, Y.T.; Huang, Y.W.; Tsai, H.J. Antipsychotic treatment and the risk of hip fracture in subjects with schizophrenia: A 10-year population-based case-control study. J. Clin. Psychiatry 2015, 76, 1216–1223. [Google Scholar] [CrossRef] [PubMed]
- Da Silva, C.P.; Zuckerman, B.; Olkin, R. Relationship of depression and medications on incidence of falls among people with late effects of polio. Physiother. Theory Pract. 2017, 33, 370–375. [Google Scholar] [CrossRef]
- Verghese, J.; Annweiler, C.; Ayers, E.; Barzilai, N.; Beauchet, O.; Bennett, D.A.; Bennett, D.A.; Bridenbaugh, S.A.; Buchman, A.S.; Callisaya, M.L.; et al. Motoric cognitive risk syndrome: Multicountry prevalence and dementia risk. Neurology 2014, 83, 718–726. [Google Scholar] [CrossRef]
- Callisaya, M.L.; Ayers, E.; Barzilai, N.; Ferrucci, L.; Guralnik, J.M.; Lipton, R.B.; Otahal, P.; Srikanth, V.K.; Verghese, J. Motoric cognitive risk syndrome and falls risk: A multi-center study. J. Alzheimer’s Dis. 2016, 53, 1043–1052. [Google Scholar] [CrossRef]
- Oh, E.S.; Blennow, K.; Bigelow, G.E.; Inouye, S.K.; Marcantonio, E.R.; Neufeld, K.J.; Rosenberg, P.B.; Troncoso, J.C.; Wang, N.-Y.; Zetterberg, H.; et al. Abnormal CSF amyloid-β42 and tau levels in hip fracture patients without dementia. PLoS ONE 2018, 13, e0204695. [Google Scholar] [CrossRef]
- Schirinzi, T.; Di Lorenzo, F.; Sancesario, G.M.; Di Lazzaro, G.; Ponzo, V.; Pisani, A.; Nicola Biagio, M.; Giacomo, K.; Alessandro, M. Amyloid-mediated cholinergic dysfunction in motor impairment related to Alzheimer’s Disease. J. Alzheimer’s Dis. 2018, 64, 525–532. [Google Scholar] [CrossRef]
- Pelosin, E.; Ogliastro, C.; Lagravinese, G.; Bonassi, G.; Mirelman, A.; Hausdorff, J.M.; Abbruzzese, G.; Avanzino, L. Attentional control of gait and falls: Is cholinergic dysfunction a common substrate in the elderly and Parkinson’s disease? Front. Aging Neurosci. 2016, 8, 104. [Google Scholar] [CrossRef]
- Kellie, S.E.; Brody, J.A. Sex-specific and race-specific hip fracture rates. Am. J. Public Health 1990, 80, 326–328. [Google Scholar] [CrossRef]
- Farmer, M.E.; White, L.R.; Brody, J.A.; Bailey, K.R. Race and sex differences in hip fracture incidence. Am. J. Public Health 1984, 74, 1374–1380. [Google Scholar] [CrossRef] [PubMed]
- Sogaard, A.J.; Holvik, K.; Omsland, T.K.; Tell, G.S.; Dahl, C.; Schei, B.; Meyer, H.E. Age and Sex Differences in Body Mass Index as a Predictor of Hip Fracture: A NOREPOS Study. Am. J. Epidemiol. 2016, 184, 510–519. [Google Scholar] [CrossRef] [PubMed]
- Ministry of Health and Welfare ROK. The Disabled Person Fact-Finding Survey in 2017; Ministry of Health and Welfare: Sejong, Korea, 2018.
- Johansson, H.; Clark, P.; Carlos, F.; Oden, A.; McCloskey, E.V.; Kanis, J.A. Increasing age- and sex-specific rates of hip fracture in Mexico: A survey of the Mexican Institute of Social Security. Osteoporos. Int. 2011, 22, 2359–2364. [Google Scholar] [CrossRef]
- Fried, L.P.; Tangen, C.M.; Waltson, J.; Newman, A.B.; Hirsch, C.; Gottdiener, J. Cardiovascular Health Study Collaborative Research Group: Cardiovascular Health Study Collaborative Research Group. Frailty in older adults: Evidence for a phenotype. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2001, 56, 146–155. [Google Scholar] [CrossRef]
- Koch, G.; Belli, L.; Giudice, T.L.; Lorenzo, F.D.; Sancesario, G.M.; Sorge, R.; Bernardini, S.; Martorana, A. Frailty among Alzheimer’s disease patients. CNS Neurol. Disord.-Drug Targets (Former. Curr. Drug Targets-CNS Neurol. Disord.) 2013, 12, 507–511. [Google Scholar] [CrossRef]
- Tsai, C.H.; Lin, C.L.; Hsu, H.C.; Chung, W.S. Increased risk of stroke among hip fracture patients: A nationwide cohort study. Osteoporos. Int. 2015, 26, 645–652. [Google Scholar] [CrossRef]
- Ahlborg, H.G.; Rosengren, B.E.; Jarvinen, T.L.; Rogmark, C.; Nilsson, J.A.; Sernbo, I.; Karlsson, M.K. Prevalence of osteoporosis and incidence of hip fracture in women-secular trends over 30 years. BMC Musculoskelet. Disord. 2010, 11, 48. [Google Scholar] [CrossRef] [PubMed]
- Nystrom, H.; Nordstrom, A.; Nordstrom, P. Risk of Injurious Fall and Hip Fracture up to 26 y before the Diagnosis of Parkinson Disease: Nested Case-Control Studies in a Nationwide Cohort. PLoS Med. 2016, 13, e1001954. [Google Scholar] [CrossRef]
- Luan, L.; Li, R.; Wang, Z.; Hou, X.; Gu, W.; Wang, X.; Yan, S.; Xu, D. Stroke increases the risk of hip fracture: A systematic review and meta-analysis. Osteoporos. Int. 2016, 27, 3149–3154. [Google Scholar] [CrossRef] [PubMed]
- Vestergaard, P.; Rejnmark, L.; Mosekilde, L. Fracture risk associated with parkinsonism and anti-Parkinson drugs. Calcif. Tissue Int. 2007, 81, 153–161. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Z.Y.; Hou, X.H.; Xie, G.Y.; Sun, X.W.; Xue, L. Relationship between elderly hip fracture and osteoporosis. Zhonghua Liu Xing Bing Xue Za Zhi 2012, 33, 1293–1295. [Google Scholar]
- National Health Insurance Service RoK. Wonju: National Health Insurance Service. 2018. Available online: http://minwon.nhis.or.kr/menu/retriveMenuSet.xx?menuId=MENU_WBMAB01 (accessed on 30 July 2018).
- Bast, B.A.; Greenwald, B.D. Preventing hip fracture after stroke. Top. Stroke Rehabil. 2007, 14, 67–79. [Google Scholar] [CrossRef]
| Variables | Category | Total | Fracture Experience |
|---|---|---|---|
| N (%) | N (%) | ||
| Total 1 | 90,012 (100.0) | 3943 (4.4) | |
| Hip fracture incidence rate 2 (per 100,000) | — | 4612 | |
| Gender | Men | 35,426 (39.4) | 1066 (3.0) |
| Women | 54,586 (60.6) | 2877 (5.3) | |
| Age group | 65–69 | 35,417 (39.3) | 899 (2.5) |
| 70–74 | 24,348 (27.0) | 970 (4.0) | |
| 75–79 | 15,424 (17.1) | 1004 (6.5) | |
| 80–84 | 9183 (10.2) | 702 (7.6) | |
| 85+ | 5640 (6.3) | 368 (6.5) | |
| Type of health security | Health insurance | 80,670 (89.6) | 3639 (4.5) |
| Medical aid | 9342 (10.4) | 304 (3.3) | |
| Household Income 1 | Low | 23,624 (26.2) | 970 (4.1) |
| Middle | 27,957 (31.1) | 1206 (4.3) | |
| High | 38,431 (42.7) | 1767 (4.6) | |
| Severity of disability | Non-disabled | 81,945 (91.0) | 3492 (4.3) |
| Severe | 2601 (2.9) | 135 (5.2) | |
| Mild | 5466 (6.1) | 316 (5.8) | |
| Type of disability | |||
| External disability | Limb disability | 3990 (4.4) | 237 (5.9) |
| Brain disability | 1308 (1.5) | 83 (6.3) | |
| Visual disability | 981 (1.1) | 47 (4.8) | |
| Auditory impairment | 1157 (1.3) | 54 (4.7) | |
| Mental disability | Mental retardation | 57 (0.1) | 3 (5.3) |
| Mental disease | 40 (0.0) | 3 (7.5) | |
| Internal organ disability etc. | Renal impairment | 161 (0.2) | 8 (5.0) |
| Other disability | 373 (0.4) | 16 (4.3) | |
| Underlying diseases | Stroke | 6604 (7.3) | 371 (5.6) |
| Parkinson | 413 (0.5) | 28 (6.8) | |
| Osteoporosis | 11,622 (12.9) | 713 (6.1) | |
| Charlson comorbidity index | 0 | 59,712 (66.3) | 2522 (4.2) |
| 1–2 | 27,723 (30.8) | 1293 (4.7) | |
| 3+ | 2577 (2.9) | 128 (5.0) | |
| Follow-uptime (day), mean (SD, standard deviation) | 2861.4 (953.9) | 1939.0 (941.9) | |
| Variables | Category | Overall, N (%) | Gender, N (%) | Disability, N (%) | ||||
|---|---|---|---|---|---|---|---|---|
| Men | Women | X2 or t-test (p-Value) | Disabled | Non-Disabled | X2 or t-test (p-Value) | |||
| Total 1 | 3943 (100.0) | 1066 (27.0) | 2877 (73.0) | 451 (11.4) | 3492 (88.6) | X2 = 3943.00 (<0.0001) | ||
| Gender | Men | 1066 (27.0) | – | – | 205 (19.2) | 861 (80.8) | X2 = 87.59 (<0.0001) | |
| Women | 2877 (73.0) | – | – | 246 (8.6) | 2631 (91.4) | |||
| Age group | 65–69 | 899 (22.8) | 346 (38.5) | 553 (61.5) | X2 = 78.13 (<0.0001) | 179 (19.9) | 720 (80.1) | X2 = 115.14(<0.0001) |
| 70–74 | 970 (24.6) | 275 (28.4) | 695 (71.6) | 125 (12.9) | 845 (87.1) | |||
| 75–79 | 1004 (25.5) | 225 (22.4) | 779 (77.6) | 94 (9.4) | 910 (90.6) | |||
| 80–84 | 702 (17.8) | 144 (20.5) | 558 (79.5) | 39 (5.6) | 663 (94.4) | |||
| 85+ | 368 (9.3) | 76 (20.7) | 292 (79.3) | 14 (3.8) | 354 (96.2) | |||
| Type of health security | Health insurance | 3639 (92.3) | 995 (27.3) | 2644 (72.7) | X2 = 2.26 (0.1326) | 397 (10.9) | 3242 (89.1) | X2 = 13.00 (0.0003) |
| Medical aid | 304 (7.7) | 71 (23.4) | 233 (76.6) | 54 (17.8) | 250 (82.2) | |||
| Household income 2 | Low | 970 (24.6) | 248 (25.6) | 722 (74.4) | X2 = 2.83 (0.2432) | 126 (13.0) | 844 (87.0) | X2 = 3.10 (0.2118) |
| Middle | 1206 (30.6) | 346 (28.7) | 860 (71.3) | 130 (10.8) | 1076 (89.2) | |||
| High | 1767 (44.8) | 472 (26.7) | 1295 (73.3) | 195 (11.0) | 1572 (89.0) | |||
| Type of disability 1 | External physical disability | 421 (10.7) | 186 (44.2) | 235 (55.8) | – | – | – | – |
| Mental disability | 6 (0.2) | 4 (66.7) | 2 (33.3) | – | – | – | – | |
| Internal organ or other disability | 24 (0.6) | 15 (62.5) | 9 (37.5) | – | – | – | – | |
| Severity of disability | Severe | 135 (3.4) | 67 (49.6) | 68 (50.4) | X2 = 1.35 (0.2445) | 135 (100.0) | – | – |
| Mild | 316 (8.0) | 138 (43.7) | 178 (56.3) | 316 (100.0) | – | |||
| Underlying diseases | Stroke | 371 (9.4) | 134 (36.1) | 237 (63.9) | X2 = 17.13 (<0.0001) | 84 (22.6) | 287 (77.4) | X2 = 50.75 (<0.0001) |
| Parkinson | 28 (0.7) | 8 (28.6) | 20 (71.4) | X2 = 0.03 (0.8543) | 4 (14.3) | 24 (85.7) | X2 = 0.23 (0.6347) | |
| Osteoporosis | 713 (18.1) | 60 (8.4) | 653 (91.6) | X2 = 152.98 (<0.0001) | 84 (11.8) | 629 (88.2) | X2 = 0.10 (0.7504) | |
| Charlson comorbidity index3 | 0 | 2522 (64.0) | 610 (24.2) | 1912 (75.8) | X2 = 46.06 (<0.0001) | 262 (10.4) | 2260 (89.6) | X2 = 17.82 (0.0001) |
| 1–2 | 1293 (32.8) | 395 (30.5) | 898 (69.5) | 161 (12.5) | 1132 (87.5) | |||
| 3+ | 128 (3.2) | 61 (47.7) | 67 (52.3) | 28 (21.9) | 100 (78.1) | |||
| Follow-uptime (day), mean (SD) | 1939.0 (941.9) | 1587.3 (952.6) | 1969.3 (936.3) | t = −3.32 (0.0009) | 1770.4 (932.9) | 1960.8 (941.0) | t = 4.05 (<0.0001) | |
| Variable | Category | Total Hazard Ratio (95% CI) | Gender, Hazard Ratio (95% CI) | Disability, Hazard Ratio (95% CI) | ||
|---|---|---|---|---|---|---|
| Men | Women | Disabled | Non-Disabled | |||
| Gender | Men | 1.00 | – | – | 1.00 | 1.00 |
| Women | 1.49 (1.39–1.61) | – | – | 1.28 (1.05–1.56) | 1.54 (1.42–1.67) | |
| Age | 65–69 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| 70–74 | 1.67 (1.52–1.83) | 1.43 (1.22–1.68) | 1.81 (1.62–2.02) | 1.11 (0.88–1.40) | 1.81 (1.64–2.00) | |
| 75–79 | 3.04 (2.77–3.32) | 2.32 (1.96–2.75) | 3.41 (3.06–3.81) | 1.51 (1.18–1.94) | 3.41 (3.09–3.77) | |
| 80–84 | 4.17 (3.77–4.60) | 3.15 (2.59–3.84) | 4.68 (4.16–5.27) | 1.57 (1.11–2.23) | 4.75 (4.27–5.28) | |
| 85+ | 4.09 (3.62–4.62) | 3.91 (3.04–5.02) | 4.30 (3.73–4.97) | 1.43 (0.82–2.47) | 4.63 (4.07–5.26) | |
| Type of health security | Health insurance | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Medical aid | 0.52 (0.45–0.59) | 0.61 (0.46–0.81) | 0.50 (0.43–0.58) | 0.51 (0.35–0.73) | 0.52 (0.45–0.61) | |
| Household income 1 | High | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Low | 1.00 (0.92–1.09) | 1.17 (0.98–1.39) | 0.94 (0.84–1.04) | 1.14 (0.87–1.49) | 0.98 (0.89–1.07) | |
| Middle | 0.98 (0.91–1.06) | 1.08 (0.94–1.24) | 0.94 (0.86–1.02) | 0.96 (0.77–1.20) | 0.98 (0.90–1.06) | |
| Severity of disability | Non-disabled | 1.00 | 1.00 | 1.00 | – | – |
| Severe | 1.59 (1.33–1.89) | 2.02 (1.57–2.61) | 1.28 (1.01–1.64) | – | – | |
| Mild | 1.68 (1.49–1.88) | 1.78 (1.48–2.13) | 1.60 (1.38–1.87) | – | – | |
| Charlson comorbidity index | 0 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| 1–2 | 1.10 (1.02–1.18) | 1.10 (0.96–1.27) | 1.10 (1.01–1.20) | 0.99 (0.78–1.25) | 1.11 (1.03–1.20) | |
| 3+ | 1.24 (1.03–1.49) | 1.45 (1.10–1.92) | 1.10 (0.85–1.42) | 1.00 (0.64–1.55) | 1.27 (1.03–1.56) | |
| Underlying diseases | Stroke (ref = none) | 1.27 (1.13–1.43) | 1.35 (1.11–1.65) | 1.24 (1.08–1.44) | 1.48 (1.11–1.98) | 1.19 (1.04–1.35) |
| Parkinson (ref = none) | 1.51 (1.04–2.19) | 1.42 (0.70–2.85) | 1.56 (1.01–2.43) | 0.89 (0.33–2.39) | 1.75 (1.17–2.62) | |
| Osteoporosis (ref = none) | 1.35 (1.24–1.46) | 1.76 (1.36–2.29) | 1.30 (1.19–1.42) | 1.47 (1.14–1.90) | 1.34 (1.22–1.47) | |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, J.; Jang, S.-N.; Lim, J.-Y. Pre-Existing Disability and Its Risk of Fragility Hip Fracture in Older Adults. Int. J. Environ. Res. Public Health 2019, 16, 1237. https://doi.org/10.3390/ijerph16071237
Kim J, Jang S-N, Lim J-Y. Pre-Existing Disability and Its Risk of Fragility Hip Fracture in Older Adults. International Journal of Environmental Research and Public Health. 2019; 16(7):1237. https://doi.org/10.3390/ijerph16071237
Chicago/Turabian StyleKim, Jayeun, Soong-Nang Jang, and Jae-Young Lim. 2019. "Pre-Existing Disability and Its Risk of Fragility Hip Fracture in Older Adults" International Journal of Environmental Research and Public Health 16, no. 7: 1237. https://doi.org/10.3390/ijerph16071237
APA StyleKim, J., Jang, S.-N., & Lim, J.-Y. (2019). Pre-Existing Disability and Its Risk of Fragility Hip Fracture in Older Adults. International Journal of Environmental Research and Public Health, 16(7), 1237. https://doi.org/10.3390/ijerph16071237





