Policymakers’ Perspectives Towards Developing a Guideline to Inform Policy on Fetal Alcohol Spectrum Disorder: A Qualitative Study
Abstract
:1. Introduction
2. Methodology
2.1. Study Setting
2.2. Study Design
2.3. Sampling Procedure
2.4. Data Collection
2.5. Data Analyses
2.6. Trustworthiness and Rigor of the Study
2.7. Ethical Considerations
2.8. Data Management
3. Results
We [(at DOE) do not have any direct policy for FASD but the policy documents I gave you are all part of what we call inclusive education.(DOE2)
We do not have a guideline per se for FASD. We (at DSD) fund non-profit organizations (NPOs) to render services. In our (DSD) annual performance plans, we (at DSD) have indicators as to what we need to achieve as a department.(DSD1)
We (at DOH) do not have any guideline or policy specifically for FASD as such in our Department, so there is nothing to guide any intervention or screening anything specifically.(DOH2)
We [at DOH] do not even have a specific policy for mental health conditions but now it has been combined with clinical conditions, e.g., HIV, AIDS, and mental health are included, that it is [the only] health policy we have for now. We do not have any policy, but we did develop a specific policy last year, but it does not look at FASD condition. It is just into mental illness not into FASD…(DOH2)
We (at DOE) have a policy document on special education needs in terms of education. It is a very broad policy document but Fetal Alcohol Spectrum Disorder is one of the areas that are titled in the policy document… we have the barriers to learning (aspects of the) policies but that includes specific learning barriers, physical barriers (blind, deaf cerebral palsy children). Therefore, FASD is one of the categories …(DOE2)
I am in women’s health and we (at DOH in our division) deal with maternal health. In maternal health, as part of antenatal care, we follow the National Maternity Care guideline and it speaks to the first antenatal booking. There is history taking that we must do and the part that history taking speaks to alcohol use as well.(DOH3)
The FASD is part of a policy (alcohol-related harms reduction policy) but in a certain chapter like health and social services, education awareness and community action group. Therefore, it [FASD policy] is worked into our alcohol-related harms reduction policy, so it (alcohol-related harms reduction policy) is becoming a white paper. It (alcohol-related harm reduction policy) has gone through to the Cabinet and after Cabinet, it (alcohol-related harms reduction policy) could become a white paper—official and then it (white paper) would become policy.(DSD3)
I would really advocate for a separate policy, separate attention given to FASD due to the severity of the problem. Because it is a severe problem in the Western Cape and if you look at communities, people have a greater need for a specialized service when it comes to FASD(DSD2)
Guidelines will definitely be helpful because it will guide appropriate intervention from an early identification point of view. Therefore, if it is identified and properly managed through guidelines, you would probably end up having a more positive result in terms of returning the child to school and not ending up being a dropout.(DOE2)
I believe everyone or anyone would like a specific policy to be developed for a specific issue. However, the first thing that we look at is if it is practical. Can it be implemented? Can the policy address the issue? In addition, can it serve the purpose that it is being developed for? However, for FASD, as I told you, in the beginning, we have schools for the blind, deaf children, schools for cerebral palsy children; we have schools for learners with slow cognitive thinking. We do not have special schools for FASD, but they will be catered for in the special needs schools. You see, as I told you, if there are funding and resources to develop a specific policy that will address this in education, and then I would advocate it. Then, I would say this could smartly be addressed in the department of health or social development, we (at DOE) are just trying to develop them [individuals affected by prenatal alcohol exposure] for the future.(DOE4)
I am not sure if that (separate policy for FASD) is necessary either because in terms of the inclusive policies that child should be identified as having a barrier to learning. Therefore, if you want a policy on that it will cost the management because the teacher needs to know how to address children with those barriers and that may even be university level. I think maybe there is a need to have a module on how to deal with FASD children because they are going (to) be in the classroom.(DOE2)
So, it is basically just general awareness and prevention services when it comes to FASD. It’s an alcohol and drug abuse awareness program. And alcohol and substance abuse or drug abuse has been identified as a special program under Social Development.(DSD2)
We (at DSD) have indicators in terms of what we need to achieve with regard to helping and assisting a patient (with an alcohol problem) or a client with FASD. (We assist the) mother first. We as a department (Social Development) fund organizations to do this.(DSD3)
There is a lot of awareness going on at the clinical level as well as when someone comes to our (Western Cape) local clinics. They (at Western Cape local clinics) do early intervention and try to motivate the client (women) to seek further treatment for the alcohol problem. And then [the Department of Education is running] educational and awareness (programs) at schools, also, the Western Cape Liquor Authority is going to the schools to have road shows and showing school children the pro(s) and cons of drinking [alcohol].(DSD3)
We (at DOH) have a PACK guideline (practical approach care kit), so this is just to help the clinician in the clinic. So, if you look at the women’s health, you screen for any drug [alcohol inclusive] abuse.(DOH1)
FASD is more addressed on a local level, at a service delivery level. The actual services that are rendered to the people affected by FASD are included in the generic social work services at grass-root levels in the local offices of the Social Development.(DSD2)
What we (at DOE) have is a commitment to training teachers in the area of the fetal alcohol spectrum disorder. What are the causes? What are their characteristics? In addition, what are the consequences for teaching and learning? Therefore, we have the training sessions across the province for fetal alcohol spectrum disorder.(DOE1)
We (at DOE) are planning a training workshop for our psychologist and I am busy planning for the training with the NPOs, to train our psychologist on early identification and treatment of FASD children. We have asked that the training must [place] emphasis on early identifications. Some have to be according to DSM five (Diagnostic and Statistical Manual of Mental Disorders) because they must diagnose correctly. In addition, the emphasis must also be on how to advise the class teacher on how to teach the child in the classroom.(DOE2)
If a child stays out of school for 10 consecutive days without any reason or explanation, we (at DOE) will call for deregistration and the child is taken out of school. However, the child is not lost; the child will be taken to social development to check if the child does not suffer from whatever special needs. After that, the Department of Social Development will be the parent or guardian for the child.(DOE4)
In schools, teachers are involved in governance. However, when there is a problem and the teacher cannot solve it, the learning support person in the schools or district will help. In addition, if there is a need for (a) psychologist or social worker they will also help. We (at DOE) have outreach teams. They include social workers, psychologist(s), and learning support people; they help an ordinary schoolteacher. Moreover, we have a school-based support team that diagnoses problems in the schools.(DOE1)
The child obviously needs to be channeled into the right schools, be identified at home as well at the school… We as a department (of Social Development) fund organizations to do this.(DSD3)
So, parents’ involvement is crucial; if a child transgresses, his parents are always informed. It is part of the policy (School Acts)(DOE4)
We as a department (Education) are busy rolling out a process for the identification of the child from grade R level. And it is in two, firstly, there is a learner’s profile, which is the biographic details of the learners; some of these details may probably be an indication of FASD. Secondly, there are forms within which the teacher fills in a special needs assessment; form one, two and three.(DOE2)
So, the screening, identification, assessment, and support (SIAS) program is to try to bring the identification down, the education spectrum possible. So, if we (at DOE) can try and pick this up as early as grade R.(DOE3)
Services (for individuals with FASD) are integrated. It (service for individuals with FASD) is dealt with like any other child requiring a service or mother who has a substance problem and requires a specialized health service.(DOH1)
Earlier identification and screening for everybody; not just FASD children, all disabilities. What I am saying if the Department of Health should pick it up in the early years when they are doing the developmental screening and if there could improve communication between the Department(s) of Health and Education. We will address the FASDs issues better.(DOE2)
Yes, early identification… not to put the diagnosis in the hands of the teachers…. I think our biggest problem is that they are not diagnosed. So, the child may be referred to us for concentration problems but actually it’s [an] FASD problem. This is because they are referred to us for behavior (-related issues) but actually, they have a neurological disorder, which we do not know about yet.(DOE3)
What we need first, is the tool to screen and identify, if we are to identify and collect data. Then, from there we can use this evidence to put measures in place…(DOH1)
So, the whole social service sector should really realize that FASD is the problem and that it should be included in all our [social development] social welfare plan(s)… We should look at the whole functioning of the person with FASD in the family [as] very important. So, then we should look at the social, emotional, psychological, educational and inspirational aspects of the person’s life and obviously the person with the FASD within his family environment.(DSD3)
Firstly, in pregnancy, they (women) need assistance with a safe house and referral pathway. (For example), if I am a heavy drinker and I realize today that I am pregnant, but I feel the responsibility to have my child protected, what is in place for me now to stop drinking? If I am living in an abusive relationship, where I am drinking with my husband? What is in place for me if I want to stop drinking today and leave this abusive drinking husband? So, that I can safeguard my child. Also, the referral pathways.(DOH1)
If a child is born and it is determined by the Health Department and Social Development that the child has specific disorders, then the child is going to be referred to a specialized school. This (is) done towards educating the child as far as possible. So that the child can fit into the community or into the work environment if it is possible.(DOE4)
We need remedial interventions early on. We focus a lot on the first thousand days of the brain development, eating and overall care of the child and if the identifying measures can start early on. This might also assist…screening pregnant women and helping other people with intervention.(DOH1)
Guidelines will definitely be helpful because it will guide appropriate intervention from an early identification point of view. So, if it is identified and properly managed through guidelines, you would probably end up having a more positive result in terms of returning the child to school and not ending up being a dropout. You may say at present, each department works on its own… when you speak about Education, the DSD, and the Health; you need to look at a new guideline [that will make us work together]. (A guideline) that will look at how these three departments will connect in transferring information from one department to another department. This is because it is like, we (at the Department of Education) get the child, and we enroll the child. The child starts in grade R and we have no medical history (of the child). We need to track the multi-development (of the child), we need to track the physical (mental, social and others) development of the child, but now we (at the Department of Education) do not have that.(DOE2)
I think that [inter-departmental collaboration] is definitively the way to go because there are many issues that each Department is dealing with in their own way. This is because if they (departments) can collaborate more and have a relationship with each other, then, it will be better. So, definitely, there is surely a need for multi-sectoral collaboration. Maybe for Social Development, for example, to look at the social need of a child, (Department of) Education looks at educational need and so on. So, to have a conversation between all the departments definitely on how services can be streamlined, it will make it easier to connect them all.(DOH2)
It will not be of any help if the Department of Social Development develops an FASD policy that only applies to our department. So, it (the guideline/policy) needs to cut across all departments and departments follow the same policy or at least we (Departments) fit in into it [the guideline/policy).(DSD2)
Basically, all departments like Department of Community Safety, Department of Health, Department of Education, Department of Rural and Land Reform, the Western Cape Local Authority, the South African Police Services and other key role players like your Municipalities; for example, Cape Town should be involved. For instance, all of them are involved in the alcohol harms reduction policy.(DSD2)
The policy care for people with disabilities…. you will find child care and protection, you will find your FASD empowerment program, you will find current prevention program, you will find youth program. All I am saying is that irrespective of the social program, it must remain accessible to all people including the persons who have disabilities… we (Social Development) will be guided by the integrated service delivery model. Our service delivery, integrated service delivery is divided into four levels. One is awareness, the second is early intervention, the third is statutory and the fourth is reunification.(DSD1)
There is a huge problem related to parental training. It is a massive problem because you would have to train every parent and I am thinking in a lot of cases—individuals with FASDs are coming from lots of areas.(DOE2)
I think we need to advocate for parental training, early diagnosis, and preschool identification. If we are looking at school policy again, early identification allows us to put them into the program early; and teacher training, train teachers to deal with these children because they are in the classroom.(DOE4)
I think it would be contrary to the inclusive education (to have FASD children in special schools). This is because the inclusive education says that we should try to assist the child in the area in which they live. So, we do not want to unnecessarily remove young children from home and place them in a boarding home. So, the inclusive policy, when you read the full services, [the child should be put in] the normal mainstream school in the community, which has additional support.(DOE2)
So, I think the contact of the child for me is so crucial because often we think of just removing the child from one school, placing the child at another but we never discuss it with the child…removing a child from one school to another is traumatic. This is because the child loses his friends, he loses his teacher—a teacher comes with teaching styles, with different teaching styles—he loses his peer, he loses his safe space and then you put the child into a different school. I mean we need to accommodate the interest of the child and we need to communicate and discuss it with the child.(DOE4)
4. Discussion
Strengths and Limitations of the Study
5. Conclusions
Supplementary Materials
Author Contributions
Acknowledgments
Conflicts of Interest
References
- Bailey, B.A.; Sokolo, R.J. Pregnancy and alcohol use: Evidence and recommendations for prenatal care. Clin. Obstet. Gynecol. 2008, 51, 436–444. [Google Scholar] [CrossRef] [PubMed]
- Blackburn, C.; Whitehurst, T. Fetal alcohol spectrum disorders (FASD): Raising awareness in early years settings. Br. J. Spec. Educ. 2010, 37, 122–129. [Google Scholar] [CrossRef]
- WHO. Global Status Report on Alcohol and Health; WHO: Geneva, Switzerland, 2014; pp. 1–100. [Google Scholar]
- Statistics South Africa. Media Release: South Africa Demographic and Health Survey|Statistics South Africa; Statistics South Africa: Pretoria, South Africa, 2016. Available online: http://www.statssa.gov.za/?p=9836 (accessed on 12 January 2018).
- Vellios, N.G.; Van Walbeek, C.P. Self-reported alcohol use and binge drinking in South Africa: Evidence from the National Income Dynamics Study, 2014–2015. S. Afr. Med. J. 2017, 108, 33–39. [Google Scholar] [CrossRef] [PubMed]
- Peltzer, K.; Davids, A.; Njuho, P. Alcohol use and problem drinking in South Africa: Findings from a national population-based survey. Afr. J. Psychiatry 2011, 14, 30–37. [Google Scholar] [CrossRef]
- Chambers, D. Binge-Drinking Is a Huge Problem in SA—But We Can’t Admit It|UCT News. 2018. Available online: https://www.news.uct.ac.za/article/-2018-01-04-binge-drinking-is-a-huge-problem-in-sa-but-we-cant-admit-it (accessed on 1 February 2019).
- Olivier, L.; Curfs, L.M.G.; Viljoen, D.L. Fetal alcohol spectrum disorders: Prevalence rates in South Africa. S. Afr. Med. J. 2016, 106, 103–106. [Google Scholar] [CrossRef] [PubMed]
- Urban, M.; Chersich, M.F.; Fourie, L.-A.; Chetty, C.; Olivier, L.; Viljeon, D. Fetal alcohol syndrome among grade 1 school children in Northern Cape province: Prevalence and risk factors. S. Afr. Med. J. 2008, 98, 877–882. [Google Scholar] [PubMed]
- Urban, M.F.; Olivier, L.; Viljoen, D.; Lombard, C.; Louw, J.G.; Drotsky, L.M.; Temmerman, M.; Chersich, M.F. Prevalence of fetal alcohol syndrome in a South African city with a predominantly black African population. Alcohol Clin. Exp. Res. 2015, 39, 1016–1026. [Google Scholar] [CrossRef] [PubMed]
- May, P.A.; Gossage, J.P.; Marais, A.-S.; Adnams, C.M.; Hoyme, H.E.; Jones, K.L.; Robinson, L.K.; Khaole, N.C.; Snell, C.; Kalberg, W.O.; et al. The epidemiology of fetal alcohol syndrome and partial FAS in a South African community. Drug Alcohol Depend. 2007, 88, 259–271. [Google Scholar] [CrossRef] [PubMed]
- May, P.A.; Blankenship, J.; Marais, A.-S.; Gossage, J.P.; Kalberg, W.O.; Barnard, R.; De Vries, M.; Robinson, L.K.; Adnams, C.M.; Buckley, D.; et al. Approaching the prevalence of the full spectrum of fetal alcohol spectrum disorders in a South African population-based study. Alcohol Clin. Exp. Res. 2013, 37, 818–830. [Google Scholar] [CrossRef] [PubMed]
- May, P.A.; de Vries, M.M.; Marais, A.-S.; Kalberg, W.O.; Adnams, C.M.; Hasken, J.M.; Tabachnick, B.; Robinson, L.K.; Manning, M.A.; Jones, K.L.; et al. The continuum of fetal alcohol spectrum disorders in four rural communities in South Africa: Prevalence and characteristics. Drug Alcohol Depend. 2016, 159, 207–218. [Google Scholar] [CrossRef] [PubMed]
- Jacobs, L.; Steyn, N.; Labadarios, D. ‘Mind the Gap’: Observations in the Absence of Guidelines for Alcohol Abstinence among Expectant Women in South Africa. 2013. Available online: http://repository.hsrc.ac.za/bitstream/handle/20.500.11910/3008/7682.pdf?sequence=1 (accessed on 12 January 2018).
- Fitzpatrick, J.P.; Latimer, J.; Carter, M.; Oscar, J.; Ferreira, M.L.; Olson, H.C.; Lucas, B.R.; Doney, R.; Salter, C.; Try, J.; et al. Prevalence of fetal alcohol syndrome in a population-based sample of children living in remote Australia: The Lililwan project. J. Paediatr. Child. Health 2015, 51, 450–457. [Google Scholar] [PubMed]
- Fitzpatrick, J.P.; Latimer, J.; Olson, H.C.; Carter, M.; Oscar, J.; Lucas, B.R.; Doney, R.; Salter, C.; Try, J.; Hawkes, G.; et al. Prevalence and profile of neurodevelopment and fetal alcohol spectrum disorder (FASD) amongst Australian Aboriginal children living in remote communities. Res. Dev. Disabil. 2017, 65, 114–126. [Google Scholar] [CrossRef] [PubMed]
- Pienaar, K.; Savic, M. Producing alcohol and other drugs as a policy ‘problem’: Acritical analysis of South Africa’s ‘National Drug Master Plan’ (2013–2017). Int. J. Drug Policy 2016, 30, 35–42. [Google Scholar] [CrossRef] [PubMed]
- Mwansa-Kambafwile, J.; Rendall-Mkosi, K.; Jacobs, R.; Nel, E.; London, L. Evaluation of a service provider short course for prevention of fetal alcohol syndrome. J. Stud. Alcohol Drugs 2011, 72, 530–535. [Google Scholar] [CrossRef] [PubMed]
- Chersich, M.F.; Urban, M.; Olivier, L.; Davies, L.A.; Chetty, C.; Viljoen, D. Universal prevention is associated with lower prevalence of fetal alcohol spectrum disorders in Northern Cape, South Africa: A multicentre before-after study. Alcohol Alcohol. 2012, 47, 67–74. [Google Scholar] [CrossRef] [PubMed]
- Rendall-Mkosi, K.; Morojele, N.; London, L.; Moodley, S.; Singh, C.; Girdler-Brown, B. A randomized controlled trial of motivational interviewing to prevent risk for an alcohol-exposed pregnancy in the Western Cape, South Africa. Addiction 2013, 108, 725–732. [Google Scholar] [CrossRef] [PubMed]
- Kirigia, J.M.; Pathe Barry, S. Health challenges in Africa and the way forward. Int. Arch. Med. 2008, 1, 27. [Google Scholar] [CrossRef] [PubMed]
- Adnams, C.M. Fetal alcohol spectrum disorder in Africa. Curr. Opin. Psychiatry 2017, 30, 108–112. [Google Scholar] [CrossRef] [PubMed]
- Rendall-Mkosi, K.; London, L.; Adnams, C.; Morojele, N.; McLoughlin, J.A.; Goldstone, C. Fetal Alcohol Spectrum Disorder in South Africa: Situational and Gap Analysis; UNICEF: Pretoria, South Africa, 2008; Available online: https://www.unicef.org/southafrica/SAF_resources_fetalalcohol.pdf (accessed on 14 September 2017).
- Adebiyi, B.O.; Mukumbang, F.C.; Okop, K.J.; Beytell, A.M. A modified Delphi study towards developing a guideline to inform policy on fetal alcohol spectrum disorders in South Africa: A study protocol. BMJ Open 2018, 8, e019907. [Google Scholar] [CrossRef] [PubMed]
- London, L. The ‘dop’ system, alcohol abuse and social control amongst farm workers in South Africa: A public health challenge. Soc. Sci. Med. 1999, 48, 1407–1414. [Google Scholar] [CrossRef]
- Esper, L.H.; Furtado, E.F. Identifying maternal risk factors associated with Fetal Alcohol Spectrum Disorders: A systematic review. Eur. Child. Adolesc. Psychiatry 2014, 23, 877–889. [Google Scholar] [CrossRef] [PubMed]
- Statistics South Africa. Statistical Release; Statistics South Africa: Pretoria, South Africa, 2017.
- Medical Research Council (MRC). Western Cape Mortality Profile 2011; MRC: London, UK, 2014. Available online: www.westerncape.gov.za (accessed on 12 January 2018).
- Petersen Williams, P.; Jordaan, E.; Mathews, C.; Lombard, C.; Parry, C.D. Alcohol and other drug use during pegnancy among women attending midwife obstetric units in the Cape Metropole, South Africa. Adv. Prev. Med. 2014, 2014, 871427. [Google Scholar] [CrossRef] [PubMed]
- Katwan, E.; Adnams, C.; London, L. Childhood behavioural and developmental disorders—Association with maternal alcohol consumption in Cape Town, South Africa. S. Afr. Med. J. 2011, 101, 724–727. [Google Scholar] [PubMed]
- Cloete, L.; Ramugondo, E. ‘I drink’: mothers’ alcohol consumption as both individualised and imposed occupation. S. Afr. J. Occup. Ther. 2015, 45, 34–40. [Google Scholar] [CrossRef]
- Charman, A.; Petersen, L. Comment on the Western Cape Alcohol-Related Harms Reduction Policy Green Paper Charman and Petersen, Sustainable Livelihoods Foundation. 2016. Available online: http://livelihoods.org.za/wp-content/uploads/2016/12/SLF-Comments-on-Western-Cape-Government-Alcohol-Harms-Green-Paper.pdf (accessed on 12 January 2018).
- Glenton, C.; Lewin, S.; Norris, S.; Norris, S. Chapter 15: Using evidence from qualitative research to develop WHO guidelines. In WHO Handbook for Guideline Development; WHO: Geneva, Switzerland, 2014; pp. 183–200. [Google Scholar]
- Creswell, J.; Creswell, J. Research Design: Qualitative, Quantitative, and Mixed Methods Approaches; Sage Publications: Thousand Oaks, CA, USA, 2017. [Google Scholar]
- Bowen, G.A. Naturalistic inquiry and the saturation concept: A research note. Qual. Res. 2008, 8, 137–152. [Google Scholar] [CrossRef]
- Brod, M.; Tesler, L.E.; Christensen, T.L. Qualitative research and content validity: Developing based on science and experience practices. Qual. Life Res. 2009, 18, 1263–1278. [Google Scholar] [CrossRef] [PubMed]
- Gale, N.K.; Heath, G.; Cameron, E.; Rashid, S.; Redwood, S. Using the framework method for the analysis of qualitative data in multi-disciplinary health research. BMC Med. Res. Methodol. 2013, 13, 117. [Google Scholar]
- Miles, M.; Huberman, A. Qualitative Data Analysis: An Expanded Sourcebook; Sage: Thousand Oaks, CA, USA, 1994; Available online: https://books.google.co.za/books?hl=en&lr=&id=U4lU_-wJ5QEC&oi=fnd&pg=PR12&dq=Qualitative+data+analysis:+An+expanded+sourcecbook.&ots=kETI6LOSUR&sig=myBC5ImkUmJHO1z2hizEOBwQzD4 (accessed on 1 March 2018).
- Lincoln, Y.S.; Guba, E.G. Naturalistic Inquiry; Sage Publications: Thousand Oaks, CA, USA, 1985; Available online: https://us.sagepub.com/en-us/nam/naturalistic-inquiry/book842 (accessed on 12 January 2018).
- Tong, A.; Sainsbury, P.; Craig, J. Consolidated criteria for reporting qualitative research (COREQ): A 32-item checklist for interviews and focus groups. Int. J. Qual. Health Care 2007, 19, 349–357. [Google Scholar] [CrossRef] [PubMed]
- Olivier, L.; Urban, M.; Chersich, M.; Temmerman, M.; Viljoen, D. Burden of Fetal Alcohol Syndrome in a rural West Coast area of South Africa. S. Afr. Med. J. 2013, 103, 402–405. [Google Scholar] [CrossRef] [PubMed]
- Crede, S.; Sinanovic, E.; Adnams, C.; London, L. The utilization of health care services by children with fetal alcohol syndrome in the Western Cape, South Africa. Drug Alcohol Depend. 2011, 115, 175–182. [Google Scholar] [CrossRef] [PubMed]
- Popova, S.; Lange, S.; Burd, L.; Urbanoski, K.; Rehm, J. Cost of specialized addiction treatment of clients with fetal alcohol spectrum disorder in Canada. BMC Public Health 2013. [Google Scholar] [CrossRef] [PubMed]
- Popova, S.; Lange, S.; Burd, L.; Rehm, J. Cost attributable to fetal alcohol spectrum disorder in the Canadian correctional system. Int. J. Law Psychiatry 2015, 41, 76–81. [Google Scholar] [CrossRef] [PubMed]
- Stade, B.; Ali, A.; Bennett, D.; Campbell, D.; Johnston, M.; Lens, C.; Tran, S.; Koren, G. The burden of prenatal exposure to alcohol: Revised measurement of cost. Can. J. Clin. Pharmacol. 2009, 16, e91–e102. [Google Scholar]
- Bennett, S.; Glandon, D.; Rasanathan, K. Governing multisectoral action for health in low-income and middle-income countries: Unpacking the problem and rising to the challenge Handling editor Seye Abimbola. BMJ Glob. Health 2018, 3, e000880. [Google Scholar] [CrossRef] [PubMed]
- Rasanathan, K.; Atkins, V.; Mwansambo, C.; Soucat, A.; Bennett, S. Governing multisectoral action for health in low-income and middle-income countries: An agenda for the way forward. BMJ Glob. Health 2018, 3, e000890. [Google Scholar] [CrossRef] [PubMed]
- Pei, J.; Baugh, L.; Andrew, G.; Rasmussen, C. Intervention recommendations and subsequent access to services following clinical assessment for fetal alcohol spectrum disorders. Res. Dev. Disabil. 2017, 60, 176–186. [Google Scholar] [CrossRef] [PubMed]
- Jirikowic, T.; Gelo, J.; Astley, S. Children and youth with fetal alcohol spectrum disorders: Summary of intervention recommendations after clinical diagnosis. Intellect. Dev. Disabil. 2010, 48, 330–344. [Google Scholar] [CrossRef] [PubMed]
- May, P.; De Vries, M.; Marais, A.-S.; Kalberg, W.; Buckley, D.; Adnams, C.; Hasken, J.; Tabachnick, B.; Robinson, L.; Manning, M.; et al. Replication of high fetal alcohol spectrum disorders prevalence rates, child characteristics, and maternal risk factors in a second sample of rural communities in South Africa. Int. J. Environ. Res. Public Health 2017, 14, 522. [Google Scholar] [CrossRef] [PubMed]
- Streissguth, A.P.; Bookstein, F.L.; Barr, H.M.; Sampson, P.D.; O’MALLEY, K.I.E.R.A.N.; Young, J.K. Risk factors for adverse life outcomes in fetal alcohol syndrome and fetal alcohol effects. J. Dev. Behav. Pediatr. 2004, 25, 228–238. [Google Scholar] [CrossRef] [PubMed]
- Cook, J.L.; Green, C.R.; Lilley, C.M.; Anderson, S.M.; Baldwin, M.E.; Chudley, A.E.; Conry, J.L.; LeBlanc, N.; Loock, C.A.; Lutke, J.; et al. Fetal alcohol spectrum disorder: A guideline for diagnosis across the lifespan. CMAJ 2016, 188, 191–197. [Google Scholar] [CrossRef] [PubMed]
- Hoyme, H.E.; Kalberg, W.O.; Elliott, A.J.; Blankenship, J.; Buckley, D.; Marais, A.S.; Manning, M.A.; Robinson, L.K.; Adam, M.P.; Abdul-Rahman, O.; et al. Updated clinical guidelines for diagnosing fetal alcohol spectrum disorders. Pediatrics 2016, 138, e20154256. [Google Scholar] [CrossRef] [PubMed]
- Watkins, R.E.; Elliott, E.J.; Halliday, J.; O’Leary, C.M.; D’Antoine, H.; Russell, E.; Hayes, L.; Peadon, E.; Wilkins, A.; Jones, H.M.; et al. A modified Delphi study of screening for fetal alcohol spectrum disorders in Australia. BMC Pediatr. 2013, 13, 13. [Google Scholar] [CrossRef] [PubMed]
- Reid, N.; Dawe, S.; Shelton, D.; Harnett, P.; Warner, J.; Armstrong, E.; LeGros, K.; O’Callaghan, F. Systematic review of fetal alcohol spectrum disorder interventions across the life span. Alcohol Clin. Exp. Res. 2015, 39, 2283–2295. [Google Scholar] [CrossRef] [PubMed]
- Koren, G.I.; Fantus, E.; Nulman, I. Managing fetal alcohol spectrum disorder in the public school system: A needs assessment pilot. Can. J. Clin. Pharmacol. 2010, 17, e79–e89. [Google Scholar] [PubMed]
- Poole, N.; Schmidt, R.A.; Green, C.; Hemsing, N. Prevention of fetal alcohol spectrum disorder: Current Canadian efforts and analysis of gaps. Subst. Abuse 2016, 10, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Adebiyi, B.O.; Mukumbang, F.C.; Cloete, L.G.; Beytell, A.M. Exploring service providers’ perspectives on the prevention and management of fetal alcohol spectrum disorders in South Africa: A qualitative study. BMC Public Health 2018. [Google Scholar] [CrossRef] [PubMed]
- Public Health Agency of Canada. Fetal Alcohol Spectrum Disorder (FASD): A Framework for Action; Health Canada: Ottawa, ON, Canada, 2003. Available online: https://www.canada.ca/en/public-health/services/reports-publications/fetal-alcohol-spectrum-disorder-fasd-framework-action.html (accessed on 8 August 2018).
- Australian Government. Title: National Fetal Alcohol Spectrum Disorder Strategic Action Plan; Australian Government: Canberra, Australia, 2018. Available online: http://www.dpmc.gov.au/government/commonwealth-coat-arms (accessed on 2 February 2019).
- Williams, D.R.; Costa, M.V.; Odunlami, A.O.; Mohammed, S.A. Moving upstream: How interventions that address the social determinants of health can improve health and reduce disparities. J. Public Health Manag. Pract. 2008, 14, S8–S17. [Google Scholar] [CrossRef] [PubMed]
- Sanders, J.; Currie, C.L. Looking further upstream to prevent fetal alcohol spectrum disorder in Canada. Can. J. Public Health 2014, 105, e450–e452. [Google Scholar] [CrossRef] [PubMed]
| Characteristics | Participants (N = 10) |
|---|---|
| Number of interviews per department | |
| Department of Education | 4 |
| Department of Health | 3 |
| Department of Social Development | 3 |
| Gender | |
| Male | 4 |
| Female | 6 |
| Profession | |
| Allied health | 5 |
| Others | 5 |
| Working Experience (Years) | |
| 5–10 | 3 |
| 11–20 | 3 |
| 21–30 | 2 |
| 31–40 | 1 |
| 41–50 | 1 |
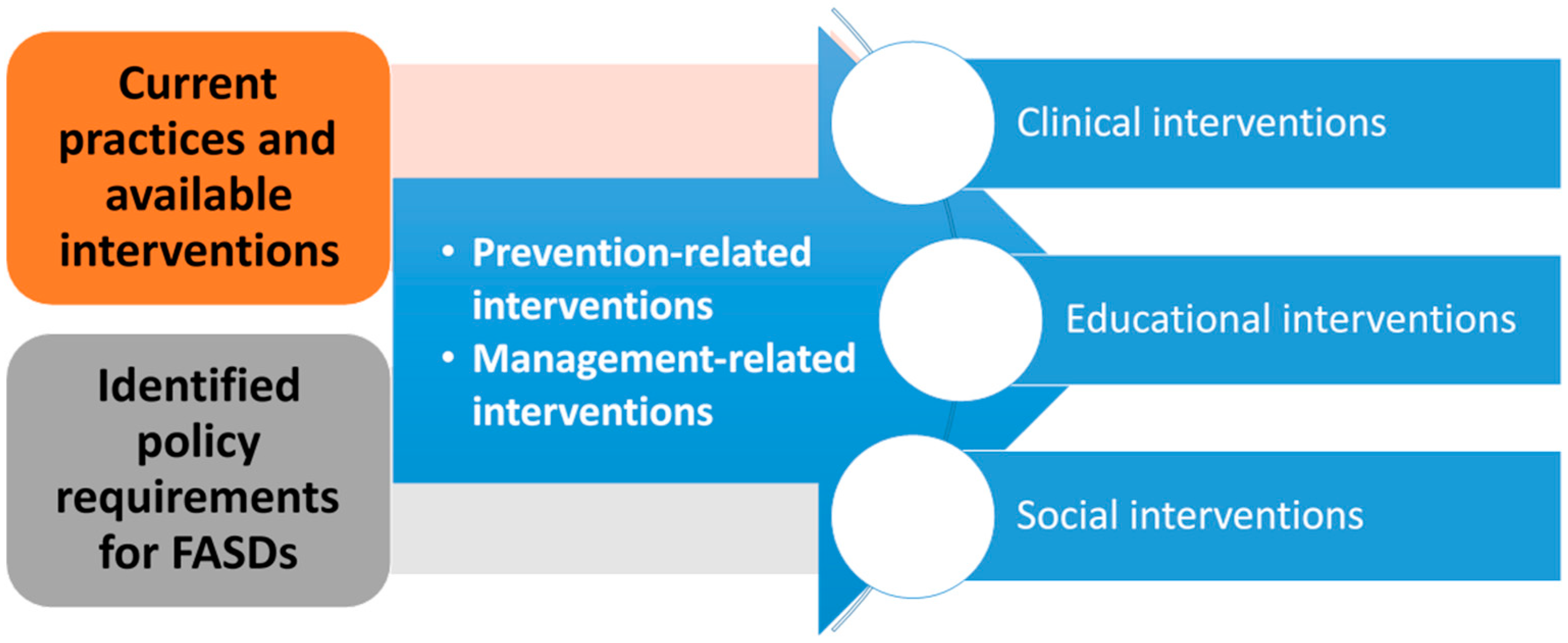
| Prevention practices and interventions | Clinical | Use of non-profit organizations [NPOs] to assist pregnant women with a drinking problem |
| Referring women with an alcohol problem to DSD | ||
| Taking alcohol history during antenatal booking | ||
| Health promotion on alcohols for women in clinics | ||
| Customized message on the risk of alcohol consumption | ||
| Multi-sectoral collaboration for alcohol abuse prevention | ||
| Motivational counseling to stop drinking | ||
| Alcohol screening for high-risk women | ||
| Educational | Prevention awareness in schools on alcohol | |
| Social | Funding NPOs to carry out FASD prevention program | |
| Awareness and prevention of alcohol abuse at a local level | ||
| Motivating women to participate in an alcohol program | ||
| Awareness schools and clinics on the danger of drinking alcohol | ||
| Alcohol/drug abuse awareness program in the community | ||
| Management practices and interventions | Clinical | General developmental screening for children |
| Use of NPOs to carry out a diagnosis for children | ||
| Multi-sectoral collaboration for management | ||
| Educational | Educating children with FASD and preparing them for the future | |
| Parent involvement in the management of a child with FASD | ||
| Commitment to training teachers and members of the support team on the identification and management of a child with FASD | ||
| Availability of outreach team to support teachers and learners | ||
| Adaptation of curriculum for an individual with FASD | ||
| Screening, identification, assessment, and support for children | ||
| Provision of specialized education for individuals with FASD | ||
| Specialized support for individuals with FASD within the mainstream school | ||
| Availability of policy that addressed curriculum, behavior, and governance | ||
| Social | Early intervention and aftercare assistance for children | |
| Availability of protective workshops for adults with a disability | ||
| Availability of daycare service for children with disability | ||
| Availability of residential services for children with disability | ||
| Funding NPOs to provide residential care for children with FASD |
| Prevention policy requirements | Clinical | Need for multi-sectoral collaboration for prevention |
| Facilitate local initiates to solve alcohol problems | ||
| Establishment of a working group for policy development | ||
| Emphasis on no alcohol is safe during pregnancy | ||
| Need to screen women for alcohol and drug abuse | ||
| Need for a prevention program for the women, the family, and the community | ||
| Educational | Put a law in place to deter people from abusing alcohol | |
| Awareness about the danger of drinking alcohol | ||
| Targeted intervention in high incidence area | ||
| Social | Advocating for the right of individuals with FASD | |
| The inclusion of the needs of individuals with FASD in the social welfare plan | ||
| Skill building for individuals with FASD | ||
| Alcohol pricing and tavern regulation | ||
| Create a local alcohol action committee | ||
| Consultation with relevant implementation stakeholders | ||
| Management policy requirements | Clinical | Identification of the needs of individuals with FASD |
| Need for a safe house for pregnant women and referral pathways | ||
| Need for seamless connection with services on FASD problems | ||
| Need for helpline that people can call for information on FASD | ||
| Need for multi-sectoral collaboration for managing FASD | ||
| Educational | Interdepartmental involvement (South African Police Services [SAPS], churches, and non-profit organizations [NPOs]) | |
| Need for specialist care for individuals with FASD | ||
| Need for a structured and dedicated program for FASD | ||
| Training of teachers, social workers, and psychologist on FASD | ||
| Need for inclusive education for individuals with FASD | ||
| Classroom management guideline for FASD | ||
| Pharmacological management of FASD | ||
| Parents should create a care mechanism for their children. | ||
| Early diagnosis and preschool identification for children | ||
| Need for early intervention for an individual with FASD | ||
| Need for school curriculum adaptation and functional curriculum for an individual with FASD | ||
| Need for additional support within the mainstream school FASD children | ||
| Need for medical assistant in schools for FASD children | ||
| Early identification and prevention | ||
| Clear roles and responsibilities of the different departments of management of FASD | ||
| Appropriate child placement for FASD children | ||
| Clear channels of communication among departments | ||
| Proper communication to the parent about their children | ||
| Communication with FASD children | ||
| Social | Need for specified and appropriate intervention for different ages | |
| Training of caregivers, social service practitioners, and volunteers | ||
| Promoting independent living | ||
| Build residential facilities and daycare | ||
| Care for individuals with FASD and their families | ||
| Funding NPOs to provide personalized services for FASD |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Adebiyi, B.O.; Mukumbang, F.C.; Cloete, L.G.; Beytell, A.-M. Policymakers’ Perspectives Towards Developing a Guideline to Inform Policy on Fetal Alcohol Spectrum Disorder: A Qualitative Study. Int. J. Environ. Res. Public Health 2019, 16, 945. https://doi.org/10.3390/ijerph16060945
Adebiyi BO, Mukumbang FC, Cloete LG, Beytell A-M. Policymakers’ Perspectives Towards Developing a Guideline to Inform Policy on Fetal Alcohol Spectrum Disorder: A Qualitative Study. International Journal of Environmental Research and Public Health. 2019; 16(6):945. https://doi.org/10.3390/ijerph16060945
Chicago/Turabian StyleAdebiyi, Babatope O., Ferdinand C. Mukumbang, Lizahn G. Cloete, and Anna-Marie Beytell. 2019. "Policymakers’ Perspectives Towards Developing a Guideline to Inform Policy on Fetal Alcohol Spectrum Disorder: A Qualitative Study" International Journal of Environmental Research and Public Health 16, no. 6: 945. https://doi.org/10.3390/ijerph16060945
APA StyleAdebiyi, B. O., Mukumbang, F. C., Cloete, L. G., & Beytell, A.-M. (2019). Policymakers’ Perspectives Towards Developing a Guideline to Inform Policy on Fetal Alcohol Spectrum Disorder: A Qualitative Study. International Journal of Environmental Research and Public Health, 16(6), 945. https://doi.org/10.3390/ijerph16060945






