Factors Shaping Attitudes of Medical Staff towards Acceptance of the Standard Precautions
Abstract
1. Introduction
2. Material and Methods
- Assessment of the situation—this factor refers to an employee’s decision whether and to what degree it is appropriate to apply SPs in a given situation; this assessment is made independently by the employee and is based on a subjective estimation of the risk related to performing the task (questions 2, 5, 14–16, 23).
- Favourable patterns of behaviour—this factor is associated with social influence on the employees’ behaviour in terms of organisational behaviour favourable for SPs; observing the behaviour of other people causes us to want to modify our own behaviour; we also influence the behaviour of our co-workers through the patterns of our own behaviour, sharing knowledge, giving feedback (questions 1, 3, 7, 9, 10). It is a conscious shaping of the attitudes of others in the direction that we consider to be right, while at the same time, we are convinced we are right and try not to give into the negative influence of other people.
- Negative norms—this factor indicates unfavourable informal rules existing in the organisation, such as group norms, habits and behaviours providing the permission to ignore the need for the application of SPs (questions 11, 12). It is a level of behavioural regulation not disclosed in organisations (usually in organisations we do not speak directly about informal principles or habitually sanctioned norms of behaviour, we rather refer to formal rules and regulations of procedures); this level of behaviour regulation becomes clear when we have to overstep the unwritten, informally existing rules—then, their regulatory force is revealed.
- Unfavourable patterns of behaviour—this factor is associated with social influence on the employees’ behaviours in terms of inconsistent and/or explicitly negative behaviours; if the majority of people behave in a particular way, we are also inclined to behave the same way. With respect to considerations surrounding the application of SPs, if the majority of people in an organisation apply SPs then the workers themselves apply SPs because it is a standard of behaviour in a given organisation; if inconsistent or explicitly negative behaviours occur, the employees will not be as likely to comply with SPs (questions 4, 6, 8, 13, 24).
- Rationalising—this factor describes an employee’s tendency to justify his or her own negative behaviour; the worker is focused on “clearing themselves of accusations”; there is no intention to change the unfavourable behaviour patterns (questions 17–22, 25).
3. Results
4. Discussion
5. Conclusions
Statistical Limitations
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Available online: https://data.worldbank.org/indicator/SH.XPD.CHEX.GD.ZS (accessed on 27 December 2018).
- Haque, M.; Sartelli, M.; McKimm, J.; Bakar, M.A. Health care-associated infections—An overview. Infect. Drug Resist. 2018, 11, 2321–2333. [Google Scholar] [CrossRef] [PubMed]
- LaForce, M. The Control of Infections in Hospitals: 1750 to 1950. In Prevention and Control of Nosocomial Infections; Wenzel, R.P., Ed.; Williams&Wilkins: Baltimore, MD, USA, 1987. [Google Scholar]
- World Health Organization. WHO Guidelines on Hand Hygiene in Health Care. First Part. Global Patient Safety Challenge. Clean Care Is Safer Care. 2009. Available online: http://apps.who.int/iris/bitstream/10665/44102/1/9789241597906_eng.pdf (accessed on 27 December 2018).
- Siegel, J.D.; Rhinehart, E.; Jackson, M.; Chiarello, L. Healthcare Infection Control Practices Advisory Committee: 2007 Guideline for Isolation Precautions: Preventing Transmission of Infectious Agents in Healthcare Settings. Available online: https://www.cdc.gov/infectioncontrol/pdf/guidelines/isolation-guidelines.pdf (accessed on 27 December 2018).
- Nante, N.; Ceriale, E.; Messina, G.; Lenzi, D.; Manzi, P. Effectiveness of ATP bioluminescence to assess hospital cleaning: A review. J. Prev. Med. Hyg. 2017, 58, E177–E183. [Google Scholar] [PubMed]
- Różańska, A.; Romaniszyn, D.; Chmielarczyk, A.; Bulanda, M. Bacteria contamination of touch surfaces in Polish hospital wards. Med. Pracy 2017, 68, 459–467. [Google Scholar] [CrossRef] [PubMed]
- Różańska, A.; Chmielarczyk, A.; Romaniszyn, D.; Sroka-Oleksiak, A.; Bulanda, M.; Walkowicz, M.; Osuch, P.; Knych, T. Antimicrobial Properties of Selected Copper Alloys on Staphylococcus aureus and Escherichia coli in Different Simulations of Environmental Conditions: With vs. without Organic Contamination. Int. J. Environ. Res. Public Health 2017, 14, 813. [Google Scholar] [CrossRef] [PubMed]
- Garus-Pakowska, A.; Sobala, W.; Szatko, F. Observance of hand washing procedures performed by the medical personnel before patient contact. Part I. Int. J. Occup. Med. Environ. Health 2013, 26, 113–121. [Google Scholar] [CrossRef] [PubMed]
- Garus-Pakowska, A.; Sobala, W.; Szatko, F. Observance of hand washing procedures performed by the medical personnel after the patient contact. Part II. Int. J. Occup. Med. Environ. Health 2013, 26, 257–264. [Google Scholar] [CrossRef] [PubMed]
- Garus-Pakowska, A.; Sobala, W.; Szatko, F. The use of protective gloves by medical personnel. Int. J. Occup. Med. Environ. Health 2013, 26, 423–429. [Google Scholar] [CrossRef] [PubMed]
- Baloh, J.; Thom, K.A.; Perencevich, E.; Rock, C.; Robinson, G.; Ward, M.; Herwaldt, L.; Schacht Reisinger, H. Hand hygiene before donning nonsterile gloves: Healthcare workers’ beliefs and practices. Am. J. Infect. Control 2018. [Google Scholar] [CrossRef]
- Ceriale, E.; Vencia, F.; Nante, N.; Sancasciani, S. Hand hygiene compliance in an Italian hospital. Eur. J. Public Health 2016, 26 (Suppl. 1). [Google Scholar] [CrossRef]
- Różańska, A.; Wójkowska-Mach, J.; Bulanda, M. Is the hospital environment friendly for infection control in Poland? Experience after twenty years of modern infection control. J. Hosp. Infect. 2016, 94, 228–229. [Google Scholar] [CrossRef] [PubMed]
- Wałaszek, M.; Kołpa, M.; Wolak, Z.; Różańska, A.; Wójkowska-Mach, J. Poor Hand Hygiene Procedure Compliance among Polish Medical Students and Physicians-The Result of an Ineffective Education Basis or the Impact of Organizational Culture? Int. J. Environ. Res. Public Health 2017, 14, 1026. [Google Scholar] [CrossRef] [PubMed]
- Wałaszek, M.; Kołpa, M.; Różańska, A.; Wolak, Z.; Bulanda, M.; Wójkowska-Mach, J. Practice of hand hygiene and use of protective gloves: Differences in the perception between patients and medical staff. Am. J. Infect. Control 2018. [Google Scholar] [CrossRef] [PubMed]
- Wałaszek, M.; Kołpa, M.; Wolak, Z.; Różańska, A.; Wójkowska-Mach, J. Patient as a Partner in Healthcare-Associated Infection Prevention. Int. J. Environ. Res. Public Health 2018, 15, 624. [Google Scholar] [CrossRef] [PubMed]
- Wałaszek, M.; Kołpa, M.; Jagiencarz-Starzec, B.; Wolak, Z.; Wójkowska-Mach, J. Nail microbial colonization following hand disinfection: A qualitative pilot study. J. Hosp. Infect. 2018. [Google Scholar] [CrossRef] [PubMed]
- Edwards, L.A. Social Desirability Variable in Personality Assessment and Research; Dryden: New York, NY, USA, 1957. [Google Scholar]
- Paulhus, D.L.; Reid, D.B. Enhancement and denial in socially desirable responding. J. Personal. Soc. Psychol. 1991, 60, 307–317. [Google Scholar] [CrossRef]
- Izdebski, P.; Żbikowska, K.; Kotyśko, M. Review of theories of social approval. Acta Universitatis Lodziensis Folia Psychologica 2013, 17, 5–20. [Google Scholar]
- Cialdini, R.B. Wywieranie Wpływu na Ludzi; Gdańskie Wydawnictwo Psychologiczne: Gdańsk, Poland, 2016. [Google Scholar]
- Aronson, E.; Wilson, T.D.; Akert, R.M. Psychologia Społeczna; Serce i umysł, Zysk i S-ka Wydawnictwo: Poznań, Poland, 1997. [Google Scholar]
| Variable | Characteristics of the Study Group | ||
|---|---|---|---|
| Average Age, Years (SD) | Average Seniority, Years (SD) | Average Support for SPs Index Sum * (SD) | |
| Gender | |||
| female, n = 456 | 42.6 (9.07) | 20.1 (10.21) | 90.8 (11.10) |
| male, n = 39 | 32.1 (8.90) | 7. 6 (7.33) | 88.1 (11.97) |
| nd, n = 1 | 50.0 (n/a) | 30.0 (n/a) | 63.0 (n/a) |
| Place of work | |||
| medical wards, n = 184 | 42.1 (9.06) | 19.7 (10.38) | 88.7 (12.32) |
| intensive care units, n = 62 | 42.2 (8.96) | 19.2 (10.11) | 89.2 (12.36) |
| surgical wards, n = 160 | 42.2 (8.50) | 19.8 (9.33) | 92.7 (9.50) |
| emergency department, n = 45 | 36.2 (12.29) | 12.7 (13.01) | 92.2 (9.04) |
| others, n = 6 | 26.0 (n/a) | 4.0 (n/a) | 87.0 (n/a) |
| nd, n = 48 | 46.0 (7.78) | 23.5 (9.52) | 91.1 (11.88) |
| Occupation | |||
| nurses, n = 442 | 43.2 (8.50) | 20.8 (9.67) | 90.8 (11.32) |
| physicians, n = 19 | 39.1 (10.10) | 13.3 (9.96) | 92.5 (10.51) |
| paramedics, n = 32 | 27.4 (5.45) | 3.6 (3.78) | 89.1 (9.44) |
| others, n = 20 | 26.0 (n/a) | 4.0 (n/a) | 87.0 (n/a) |
| nd, n = 5 | 37.8 (9.15) | 14.2 (9.58) | 76.0 (14.46) |
| Total, N = 505 | 41.8 (9.47) | 19.2 (10.57) | 90.5 (11.24) |
| Variable | Support for SPs Index Sum | ||
|---|---|---|---|
| Power of Impact | p-Value | ||
| Age | −0.10 | 0.24 | |
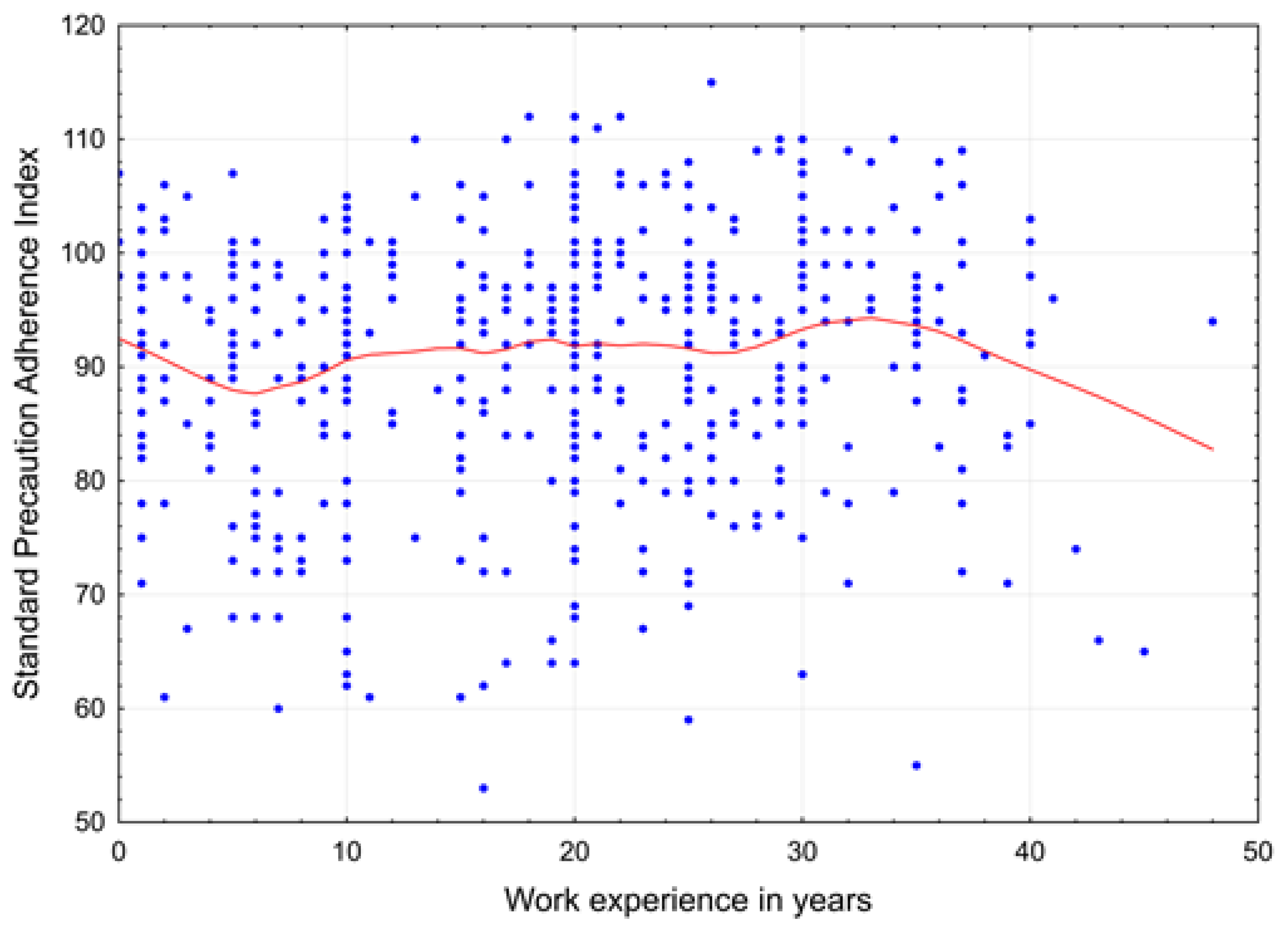
| Seniority | 0.17 | 0.02 | |
| Sex | female | 3.44 | 0.31 |
| male | 0.22 | 0.95 | |
| Profession | nurses | 1.12 | 0.70 |
| physicians | 5.15 | 0.13 | |
| paramedics | −0.36 | 0.92 | |
| Place of work | medical wards | −2.47 | 0.01 |
| intensive care units (ICUs) | −2.48 | 0.05 | |
| surgical wards | 1.47 | 0.13 | |
| emergency department (ED) | 3.76 | 0.04 | |
| Variable | Test of Significance of Differentiation of Support for SPs, Index Sum | ||
|---|---|---|---|
| degrees of Freedom | MS—Strength of Contribution | p-Value | |
| Age | 1 | 4.30 | 0.84 |
| Seniority | 1 | 77.45 | 0.39 |
| Sex | 2 | 126.94 | 0.30 |
| Profession | 4 | 92.42 | 0.48 |
| Place of work | 4 | 632.15 | <0.001 |
| Partial sums | Statistically significant dependent variables of influence |
|---|---|
| (1) Rationalising | non-surgical wards (−) ED (+) |
| (2) Favourable patterns of behaviour | men (−) physicians (+), non-surgical wards (−) surgical wards (+) |
| (3) Negative norms | ED (−) |
| (4) Unfavourable patterns of behaviour | seniority (+), surgical wards (+) |
| (5) Assessment of the situation | No impact |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rosiński, J.; Różańska, A.; Jarynowski, A.; Wójkowska-Mach, J.; of Hospital Infections Team, P.S. Factors Shaping Attitudes of Medical Staff towards Acceptance of the Standard Precautions. Int. J. Environ. Res. Public Health 2019, 16, 1050. https://doi.org/10.3390/ijerph16061050
Rosiński J, Różańska A, Jarynowski A, Wójkowska-Mach J, of Hospital Infections Team PS. Factors Shaping Attitudes of Medical Staff towards Acceptance of the Standard Precautions. International Journal of Environmental Research and Public Health. 2019; 16(6):1050. https://doi.org/10.3390/ijerph16061050
Chicago/Turabian StyleRosiński, Jerzy, Anna Różańska, Andrzej Jarynowski, Jadwiga Wójkowska-Mach, and Polish Society of Hospital Infections Team. 2019. "Factors Shaping Attitudes of Medical Staff towards Acceptance of the Standard Precautions" International Journal of Environmental Research and Public Health 16, no. 6: 1050. https://doi.org/10.3390/ijerph16061050
APA StyleRosiński, J., Różańska, A., Jarynowski, A., Wójkowska-Mach, J., & of Hospital Infections Team, P. S. (2019). Factors Shaping Attitudes of Medical Staff towards Acceptance of the Standard Precautions. International Journal of Environmental Research and Public Health, 16(6), 1050. https://doi.org/10.3390/ijerph16061050







