Prevent Mother-to-Child Transmission (PMTCT) Programs and Enhancement of Maternal Healthcare Infrastructure to Improve Early Detection of Maternal Syphilis in Shanghai, China
Abstract
1. Introduction
2. Materials and Methods
2.1. Definition of Study Periods
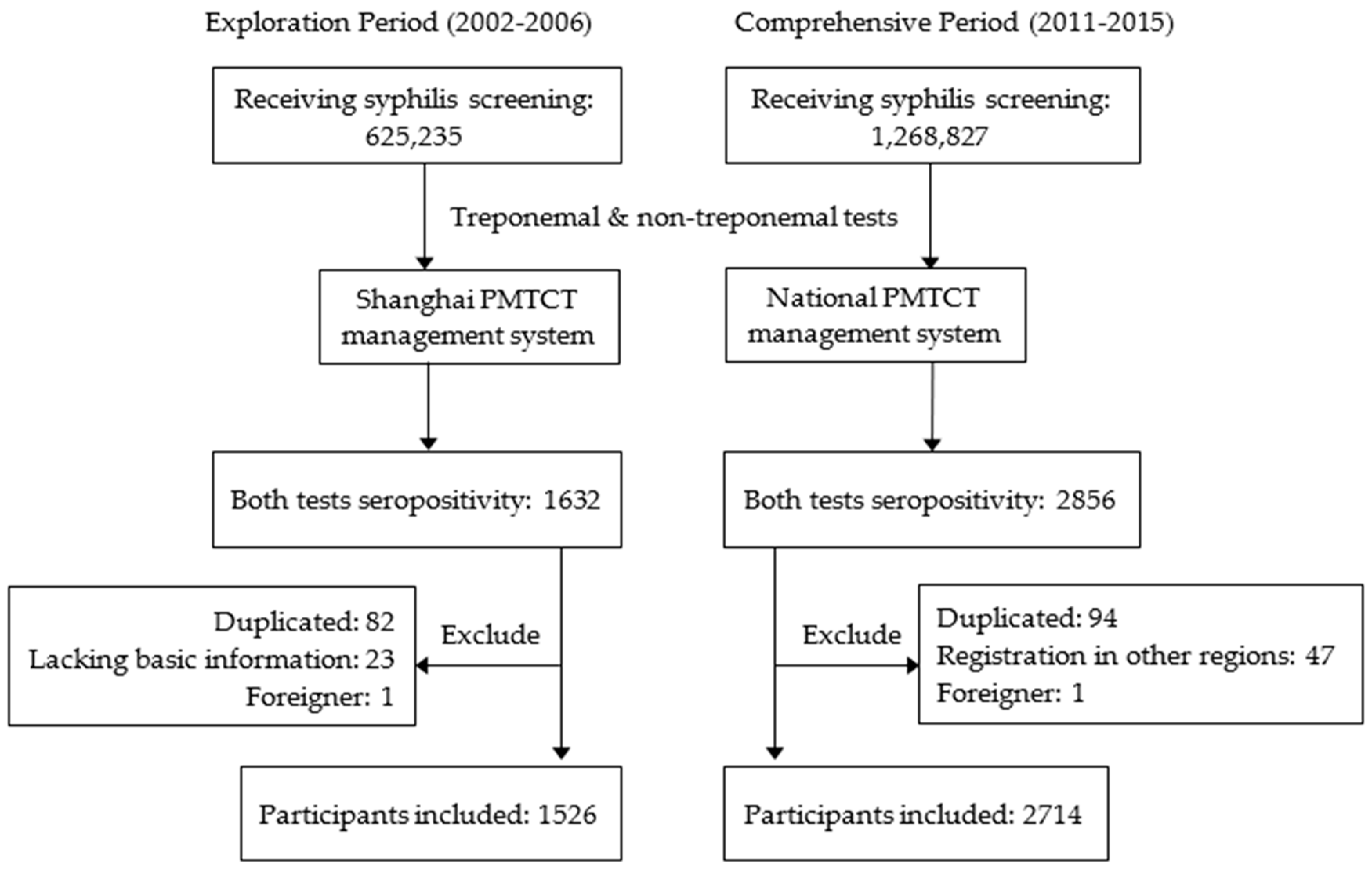
2.2. Study Design and Study Participants
2.3. Screening and Diagnosis of Maternal Syphilis
2.4. Data Collection
2.5. Statistical Analysis
3. Results
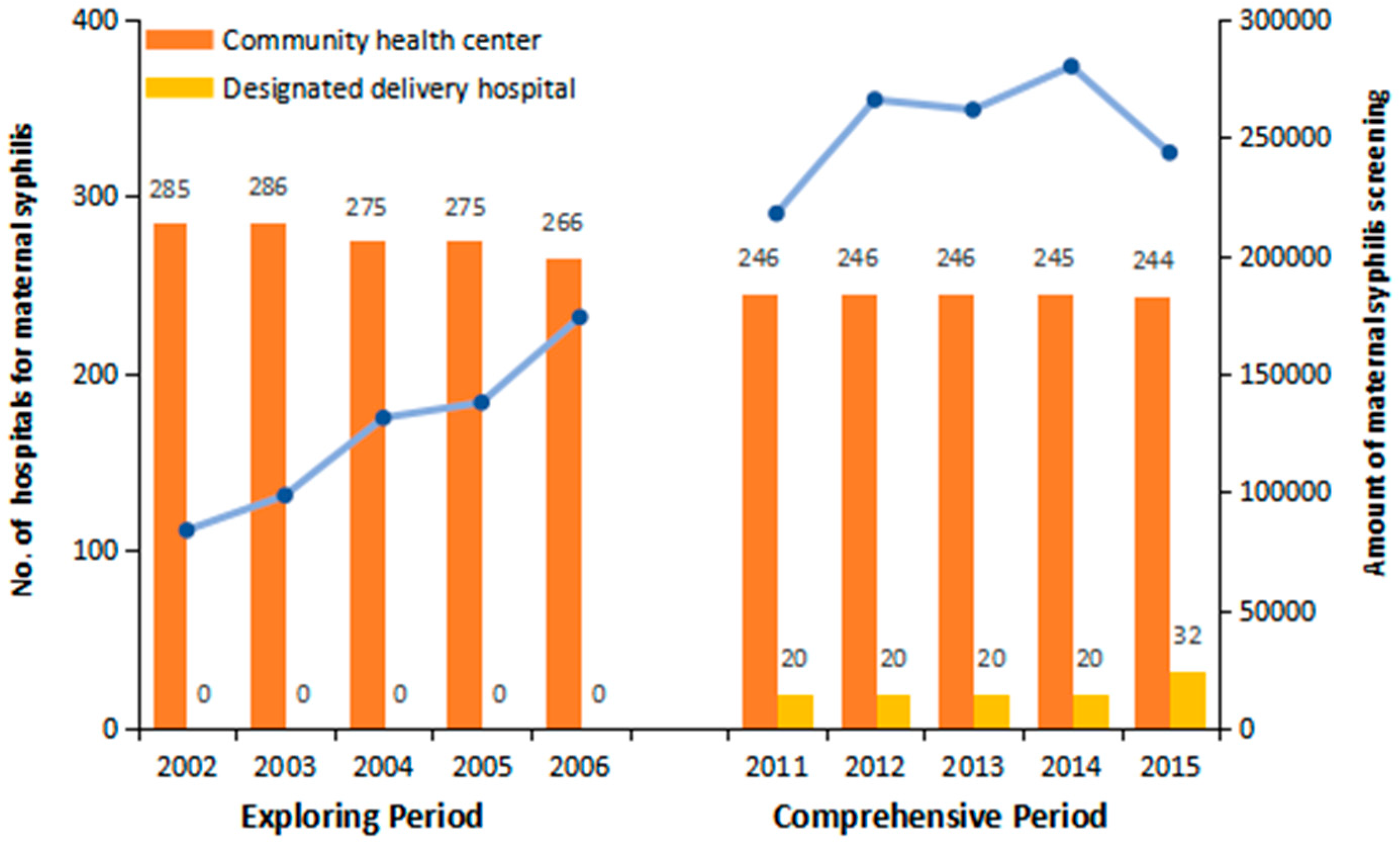
3.1. Enhancement of Health Infrastructure for Maternal Syphilis
3.2. General Characteristics of Study Participants
3.3. Gestational Weeks for Maternal Syphilis Screening
3.4. Gestational Weeks for Maternal Syphilis Diagnosis
3.5. Multivariate Analysis of Factors Affecting the Early Detection of Maternal Syphilis
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Abbreviations
| ANC | Antenatal care |
| APOs | Adverse pregnant outcomes |
| CI | Confidence interval |
| GW | Gestational weeks |
| WHO | World Health Organization |
| HIV | Human immunodeficiency virus |
| HBV | Hepatitis B virus |
| OR | Odds ratio |
| PMTCT | Prevent Mother-to-Child Transmission |
| USA | United States of America |
| STI | Sexually transmitted infection |
References
- World Health Organization. Advancing MDGs 4, 5 and 6: Impact of Congenital Syphilis Elimination. Available online: http://apps.who.int/iris/bitstream/10665/70331/1/ (accessed on 4 June 2016).
- Newman, L.; Kamb, M.; Hawkes, S.; Gomez, G.; Say, L.; Seuc, A.; Broutet, N. Global estimates of syphilis in pregnancy and associated adverse outcomes: Analysis of multinational antenatal surveillance data. PLoS Med. 2013, 10, e1001396. [Google Scholar] [CrossRef] [PubMed]
- Potter, D.; Goldenberg, R.L.; Read, J.S.; Wang, J.; Hoffman, I.F.; Saathoff, E.; Kafulafula, G.; Aboud, S.; Martinson, F.E.A.; Dahab, M.; et al. Correlates of Syphilis Seroreactivity Among Pregnant Women: The HIVNET 024 Trial in Malawi, Tanzania, and Zambia. Sex. Transm. Dis. 2006, 33, 604–609. [Google Scholar] [CrossRef] [PubMed]
- Kizito, D.; Woodburn, P.W.; Kesande, B.; Ameke, C.; Nabulime, J.; Muwanga, M.; Grosskurth, H.; Elliott, A.M. Uptake of HIV and syphilis testing of pregnant women and their male partners in a programme for prevention of mother-to-child HIV transmission in Uganda. Trop. Med. Int. Health 2008, 13, 680–682. [Google Scholar] [CrossRef] [PubMed]
- Nessa, A.; Islam, M.N.; Ashraf, F.; Islam, F.; Khanam, A.; Sultana, N.; Rashid, M.H.U. Seroprevalence of Treponema Pallidum antibody among pregnant population of Bangladesh. J. Obstet. Gynaecol. Res. 2011, 37, 1625–1630. [Google Scholar] [CrossRef] [PubMed]
- Chen, Z.Q.; Zhang, G.C.; Gong, X.D.; Lin, C.; Gao, X.; Liang, G.J.; Yue, X.L.; Chen, X.S.; Cohen, M.S. Syphilis in China: Results of a national surveillance programme. Lancet 2007, 369, 132–138. [Google Scholar] [CrossRef]
- Hesketh, T.; Zhu, W.X.; Zhou, X.D. Syphilis and social upheaval in China. N. Engl. J. Med. 2010, 363, 1088–1089. [Google Scholar] [PubMed]
- Wang, A.L.; Qiao, Y.P.; Wang, L.H.; Fang, L.W.; Wang, F.; Jin, X.; Qiu, J.; Wang, X.Y.; Wang, Q.; Wu, J.L. Integrated prevention of mother-to-child transmission for human immunodeficiency virus, syphilis and hepatitis B virus in China. Bull. World Health Organ. 2015, 93, 52–56. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. The Global Elimination of Congenital Syphilis: Rationale and Strategy for Action. Available online: http://www.who.int/reproductivehealth/publications/rtis/9789241595858/en/ (accessed on 4 June 2016).
- Hawkes, S.; Matin, N.; Broutet, N.; Low, N. Effectiveness of interventions to improve screening for syphilis in pregnancy: A systematic review and meta-analysis. Lancet Infect. Dis. 2011, 11, 684–691. [Google Scholar] [CrossRef]
- National Syphilis Epidemiology Group. Epidemiological Report on Syphilis in 1990: Surveillance Data from 38 Cities in China. Chin. J. Dermatol. 1992, 25, 228–231. [Google Scholar]
- Shanghai Statistic Bureau. 2015 Shanghai Statistic Yearbook. Available online: http://www.stats-sh.gov.cn/ (accessed on 28 December 2016).
- Li, Y.; Zhu, L.; Du, L.; Qu, L.; Jiang, W.; Xu, B. Effects on preventing mother-to-child transmission of syphilis and associated adverse pregnant outcomes: A longitudinal study from 2001 to 2015 in Shanghai, China. BMC Infect. Dis. 2017, 17, 626. [Google Scholar] [CrossRef] [PubMed]
- Tian, X. Sexually transmitted disease among pregnant women in Jilin Province. China Pract. Med. 2011, 6, 255–256. [Google Scholar]
- Zhu, L.; Qing, M.; Shi, H.; Tan, J.; He, L. Primary effect of early warning and management system for high risk pregnancy in Shanghai. Matern. Child Health Care China 2013, 28, 2021–2023. [Google Scholar]
- Zhang, R.L.; Chen, L.P.; Chen, Q.Y.; Wang, X.Y.; Zhang, L.P.; Xiu, X.Y. Epidemiological study on 38 418 syphilis cases during pregnancy. Zhonghua Liu Xing Bing Xue Za Zhi 2007, 28, 749–752. [Google Scholar] [PubMed]
- Qi, Z.; Kulane, A.; Yi, G.; Xu, B. Knowledge and attitude on maternal health care among rural-to-urban migrant women in Shanghai, China. BMC Womens Health 2009, 9, 1–8. [Google Scholar]
- Zhang, Y.; Chen, M.; Lu, J.; Hao, M.; Zhang, C.; Sun, M.; Li, X.; Chang, F. Factors impacting the use of antenatal care and hospital child delivery services: A case study of rural residents in the Enshi Autonomous Prefecture, Hubei Province, China. Int. J. Health Plan. Manag. 2015, 30, 330–345. [Google Scholar] [CrossRef] [PubMed]
- Long, Q.; Zhang, T.H.; Xu, L.; Tang, S.L.; Hemminki, E. Utilisation of maternal health care in western rural China under a new rural health insurance system (New Co-operative Medical System). Trop. Med. Int. Health 2010, 15, 1210–1217. [Google Scholar] [CrossRef] [PubMed]
- Zhao, Q.; Huang, Z.; Yang, S.; Pan, J.; Smith, B.; Xu, B. The utilization of antenatal care among rural-to-urban migrant women in Shanghai: A hospital-based cross-sectional study. BMC Public Health 2012, 12, 1012. [Google Scholar] [CrossRef] [PubMed]
- Song, L. Achievement, challenge and prospective of Preventing Mother to Child Transmission Program of HIV, Syphilis and HBV in China. Chin. J. Health Educ. 2013, 29, 675–676. [Google Scholar]
- Munkhuu, B.; Liabsuetrakul, T.; Chongsuvivatwong, V.; McNeil, E.; Janchiv, R. One-stop service for antenatal syphilis screening and prevention of congenital syphilis in Ulaanbaatar, Mongolia: A cluster randomized trial. Sex. Transm. Dis. 2009, 36, 714–720. [Google Scholar] [CrossRef] [PubMed]
- Kashyap, B.; Sagar, T.; Kaur, I.R. Utility of immunochromatographic assay as a rapid point of care test for screening of antenatal syphilis. Indian J. Sex. Transm. Dis. AIDS 2015, 36, 162–165. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Elimination of Mother-To-Child Transmission (EMTCT) of HIV and Syphilis. Available online: http://cdrwww.who.int/hiv/pub/emtct-validation-guidance (accessed on 4 June 2016).
| Variants | Exploring Period | Comprehensive Period | Total | t/χ2 | p-Value |
|---|---|---|---|---|---|
| Age (mean ± SD) | 27.78 ± 4.83 | 28.69 ± 5.41 | 28.36 ± 5.23 | 31.625 | <0.001 a |
| Residence | |||||
| Local resident | 504 (33.0) | 722 (26.6) | 1226 (28.9) | 19.616 | <0.001 b |
| Non-resident | 1022 (67.0) | 1992 (73.4) | 3014 (71.1) | ||
| Education | |||||
| Primary school | 298 (19.5) | 242 (8.9) | 540 (12.7) | 151.501 | <0.001 c |
| Secondary school | 1109 (72.7) | 1824 (67.2) | 2933 (69.2) | ||
| College or above | 106 (6.9) | 474 (17.5) | 580 (13.7) | ||
| Unknown | 13 (0.9) | 174 (6.4) | 187 (4.4) | ||
| Marriage | |||||
| Unmarried | 68 (4.5) | 220 (8.1) | 288 (6.8) | 28.721 | <0.001 b |
| Married | 1439 (94.3) | 2484 (91.5) | 3923 (92.5) | ||
| Divorced/unknown | 19 (1.2) | 10 (0.4) | 29 (0.7) | ||
| Occupation | |||||
| Employed | 627 (41.1) | 830 (30.6) | 1457 (34.4) | 47.797 | <0.001 b |
| Unemployed | 899 (58.9) | 1884 (69.4) | 2783 (65.6) | ||
| Previous Delivery | |||||
| Yes | 745 (48.8) | 1213 (44.7) | 1958 (46.2) | 6.691 | 0.010 b |
| No | 781 (51.2) | 1501 (55.3) | 2282 (53.8) |
| Variants | Gestational Weeks (n, %) | χ2 | p-Value | |||
|---|---|---|---|---|---|---|
| ≤12 | 13–18 | 19–27 | ≥28 | |||
| Period | ||||||
| Exploring | 165 (10.8) | 300 (19.7) | 411 (26.9) | 650 (42.6) | 99.192 | <0.001 a |
| Comprehensive | 380 (14.0) | 934 (34.4) | 582 (21.4) | 818 (30.1) | ||
| Exploring year | ||||||
| 2002 | 24 (11.7) | 37 (18.0) | 60 (29.3) | 84 (41.0) | 0.298 | 0.585 b |
| 2003 | 30 (12.7) | 43 (18.2) | 70 (29.7) | 93 (39.4) | ||
| 2004 | 36 (11.8) | 53 (17.4) | 87 (28.6) | 128 (42.1) | ||
| 2005 | 40 (9.5) | 86 (20.5) | 95 (22.7) | 198 (47.3) | ||
| 2006 | 35 (9.7) | 81 (22.4) | 99 (27.3) | 147 (40.6) | ||
| Comprehensive year | ||||||
| 2011 | 43 (9.4) | 144 (31.5) | 123 (26.9) | 147 (32.2) | 23.274 | <0.001 b |
| 2012 | 72 (13.1) | 170 (30.9) | 124 (22.5) | 185 (33.6) | ||
| 2013 | 97 (14.7) | 229 (34.7) | 133 (20.2) | 201 (30.5) | ||
| 2014 | 79 (14.1) | 208 (37.1) | 122 (21.7) | 152 (27.1) | ||
| 2015 | 89 (18.4) | 183 (37.7) | 80 (16.5) | 133 (27.4) | ||
| Variants | Gestational Weeks (n, %) | χ2 | p-Value | |||
|---|---|---|---|---|---|---|
| ≤12 | 13–18 | 19–27 | ≥28 | |||
| Period | ||||||
| Exploring | 111 (7.3) | 240 (15.7) | 397 (26.0) | 778 (51.0) | 233.110 | <0.001 a |
| Comprehensive | 362 (13.3) | 914 (33.7) | 617 (22.7) | 821 (30.3) | ||
| Exploring year | ||||||
| 2002 | 18 (8.8) | 25 (12.2) | 61 (29.8) | 101 (49.3) | 0.000 | 0.983 b |
| 2003 | 20 (8.5) | 36 (15.3) | 57 (24.2) | 123 (52.1) | ||
| 2004 | 21 (6.9) | 49 (16.1) | 78 (25.7) | 156 (51.3) | ||
| 2005 | 28 (6.7) | 71 (16.9) | 96 (22.9) | 225 (53.5) | ||
| 2006 | 24 (6.6) | 59 (16.3) | 105 (29.0) | 174 (48.1) | ||
| Comprehensive year | ||||||
| 2011 | 46 (10.1) | 146 (31.9) | 124 (27.1) | 141 (30.9) | 15.072 | 0.002 b |
| 2012 | 76 (13.8) | 154 (27.9) | 132 (24.0) | 189 (34.3) | ||
| 2013 | 88 (13.3) | 227 (34.4) | 146 (22.1) | 199 (30.2) | ||
| 2014 | 67 (11.9) | 207 (36.9) | 131 (23.4) | 156 (27.8) | ||
| 2015 | 85 (17.5) | 180 (37.1) | 84 (17.3) | 136 (28.0) | ||
| Variants | Compare Group | Control Group | Screening within 12 GWs | Diagnosis within 16 GWs | ||
|---|---|---|---|---|---|---|
| OR (95% CI) | p-Value | OR (95% CI) | p-Value | |||
| Policy period | Comprehensive | Exploring | 1.28 (1.04~1.58) | 0.020 | 2.76 (2.33~3.27) | <0.001 |
| Age (years) | 1.01 (0.99~1.03) | 0.178 | 1.03 (1.01~1.05) | <0.001 | ||
| Residence | Local resident | Non-resident | 1.69 (1.38~2.07) | <0.001 | 1.59 (1.36~1.87) | <0.001 |
| Education | Secondary school | Primary school | 1.82 (1.22~2.70) | 0.003 | 2.35 (1.75~3.17) | <0.001 |
| College or above | 3.00 (1.91~4.71) | <0.001 | 4.12 (2.91~5.84) | <0.001 | ||
| Unknown | 1.16 (0.61~2.22) | 0.650 | 1.83 (1.18~2.84) | 0.007 | ||
| Marriage | Unmarried | Married | 0.87 (0.58~1.30) | 0.485 | 0.71 (0.53~0.97) | 0.030 |
| Divorced/unknown | 1.39 (0.47~4.10) | 0.548 | 1.26 (0.52~3.05) | 0.609 | ||
| Occupation | Unemployed | Employed | 0.80 (0.65~0.97) | 0.022 | 0.68 (0.59~0.80) | <0.001 |
| Previous delivery | Yes | No | 0.68 (0.56~0.84) | <0.001 | 0.55 (0.47~0.64) | <0.001 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Du, L.; Li, Y.; Jin, H.; Huang, C.; Gu, Y.; Zhu, L.; Xu, B. Prevent Mother-to-Child Transmission (PMTCT) Programs and Enhancement of Maternal Healthcare Infrastructure to Improve Early Detection of Maternal Syphilis in Shanghai, China. Int. J. Environ. Res. Public Health 2019, 16, 1002. https://doi.org/10.3390/ijerph16061002
Du L, Li Y, Jin H, Huang C, Gu Y, Zhu L, Xu B. Prevent Mother-to-Child Transmission (PMTCT) Programs and Enhancement of Maternal Healthcare Infrastructure to Improve Early Detection of Maternal Syphilis in Shanghai, China. International Journal of Environmental Research and Public Health. 2019; 16(6):1002. https://doi.org/10.3390/ijerph16061002
Chicago/Turabian StyleDu, Li, Yang Li, Hui Jin, Cheng Huang, Yibin Gu, Liping Zhu, and Biao Xu. 2019. "Prevent Mother-to-Child Transmission (PMTCT) Programs and Enhancement of Maternal Healthcare Infrastructure to Improve Early Detection of Maternal Syphilis in Shanghai, China" International Journal of Environmental Research and Public Health 16, no. 6: 1002. https://doi.org/10.3390/ijerph16061002
APA StyleDu, L., Li, Y., Jin, H., Huang, C., Gu, Y., Zhu, L., & Xu, B. (2019). Prevent Mother-to-Child Transmission (PMTCT) Programs and Enhancement of Maternal Healthcare Infrastructure to Improve Early Detection of Maternal Syphilis in Shanghai, China. International Journal of Environmental Research and Public Health, 16(6), 1002. https://doi.org/10.3390/ijerph16061002






