Double Burden of Rural Migration in Canada? Considering the Social Determinants of Health Related to Immigrant Settlement Outside the Cosmopolis
Abstract
1. Introduction
Health Inequities among Immigrant and Rural Populations
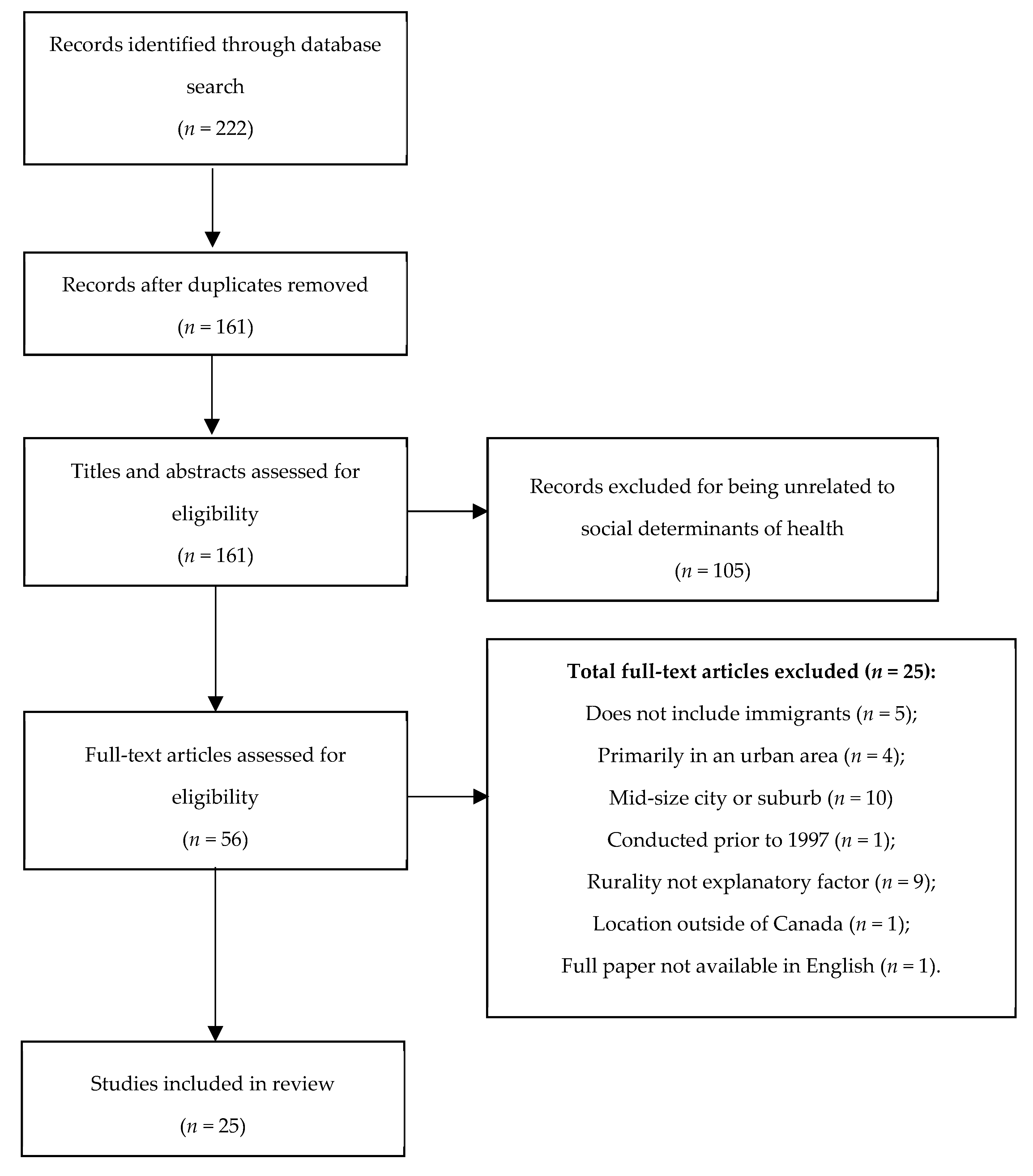
2. Methods
“Societal conditions in which people are born, grow, live, work and age … [including] early years’ experiences, education, economic status, employment and decent work, housing and environment, and effective systems of preventing and treating ill health” [69].
3. Results
3.1. Determinant 1: Social Inclusion
3.2. Determinant 2: Access to Culturally Appropriate Health and Settlement Services
3.3. Determinant 3: Gender
3.4. Determinant 4: Employment
3.5. Determinant 5: Housing
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
Appendix A
| Title | Author(s) | Year | Location Type | Literature Type & Purpose | Theme(s) |
|---|---|---|---|---|---|
| Housing Experiences of Recent Immigrants to Canada’s Small Cities: the Case of North Bay, Ontario | Brown N.R. | 2017 | Small city | Ethnographic study: To better understand newcomers’ ability to attain affordable housing in North Bay |
|
| Attracting immigrants to smaller urban and rural communities: Lessons learned from the Manitoba Provincial Nominee Program | Carter, T., Morrish, M., & Amoyaw, B. | 2008 | Rural communities | Case study: To better understand the changing distribution and settlement of immigrants |
|
| Belonging and Mental Wellbeing Among a Rural Indian-Canadian Diaspora: Navigating Tensions in “Finding a Space of Our Own” | Caxaj, C. Susana; Gill, Navjot K. | 2017 | Rural community | Ethnographic study: To explore sense of belonging in a rural community |
|
| Examining the relationship between social support availability, urban center size, and self-perceived mental health of recent immigrants to Canada: A mixed-methods analysis | Chadwick K.A., Collins P.A. | 2015 | Rural vs. urban communities | Mixed-methods study: To explore the relationship between immigrants’ self-perceived mental health and urban center size |
|
| Eating Chinese: Culture on the menu in small town Canada | Cho, L. | 2010 | Rural community | Narrative: To discuss the Chinese diaspora in rural communities across Canada and understand how their cuisine and entrepreneurship have evolved over time |
|
| Differences in hi-tech immigrant earnings and wages across Canadian cities | Hall, P. V., & Khan, A. J. | 2008 | Rural vs. urban communities | Cross-sectional study: To compare immigrants vs. non-immigrants’ wages across different geographies |
|
| Leading a diverse school during times of demographic change in rural Canada: Reflection, action and suggestions for practice | Hamm L., Doğurga S.-L., Scott A. | 2016 | Rural community | Literature review: To analyze teaching practices in relation to demographic change in rural Canada |
|
| An ethnographic study of communication challenges in maternity care for immigrant women in rural Alberta | Higginbottom G.M.A., Safipour J., Yohani S., O’Brien B., Mumtaz Z., Paton P. | 2015 | Rural community | Ethnographic study: To better understand communication challenges for immigrant women in seeking maternal healthcare in rural Alberta, Canada. |
|
| An ethnographic investigation of the maternity healthcare experience of immigrants in rural and urban Alberta, Canada | Higginbottom G.M., Safipour J., Yohani S., O’Brien B., Mumtaz Z., Paton P., Chiu Y., Barolia R. | 2016 | Rural vs. urban communities | Ethnographic study: To better understand and compare maternity healthcare for immigrant women in rural and urban Canada |
|
| Barriers and facilitators to family planning access in Canada | Hulme J., Dunn S., Guilbert E., Soon J., Norman W. | 2015 | Rural communities | Ethnographic study: To explore barriers to family planning in Canada for vulnerable populations in rural areas |
|
| The dilemma of physician shortage and international recruitment in Canada | Islam, N. | 2014 | Rural communities | Policy brief: To summarize and analyze policies that relate to foreign-trained physicians (rural and urban). |
|
| Sense of community belonging and health in Canada: A regional analysis | Kitchen, P.; Williams, A.; Chowhan, J. | 2012 | Rural vs. urban communities | Cross-sectional study: To look at self-perceived mental health and community belonging across different geographic contexts (urban vs. rural) and different groups of people |
|
| Managing health professional migration from sub-Saharan Africa to Canada: a stakeholder inquiry into policy options | Labonté, R., Packer, C., & Klassen, N. | 2006 | Rural vs. urban communities | Ethnographic study: To better understand the migration of foreign-trained health professionals and its implications for Canada (rural to urban transect). |
|
| The Power of Collaborative Inquiry and Metaphor in Meeting the Health Literacy Needs of Rural Immigrant Women | Lauzon, A.; Farabakhsh, R. | 2014 | Rural community | Ethnographic study: To use a participatory method to understand needs of immigrant women living in a rural Ontarian community |
|
| Social capital, labour markets, and job-finding in urban and rural regions: Comparing paths to employment in prosperous cities and stressed rural communities in Canada | Matthews R., Pendakur R., Young N. | 2009 | Rural vs. urban communities | Mixed-methods study: To compare social capital utilization and employment opportunities between rural and non-rural settings |
|
| The migration decisions of physicians in Canada: the roles of immigrant status and spousal characteristics | McDonald J.T., Worswick C. | 2012 | Rural vs. urban communities | Cross-sectional study: To study mobility patterns of immigrants and non-immigrant physicians (to rural areas). |
|
| Longitudinal trends in mental health among ethnic groups in Canada | Pahwa P., Karunanayake C.P., McCrosky J., Thorpe L. | 2012 | Rural vs. urban communities | Longitudinal study: To examine longitudinal trends between mental health and other demographic factors within ethnic groups |
|
| Democratic citizenship education in rural high schools: Navigating difference and conflict in three Ontario classrooms | Pattison-Meek, J. M. | 2016 | Rural communities | Ethnographic study: To analyze and compare democratic participation in rural and urban high schools |
|
| Experiences of discrimination and discomfort: A comparison of metropolitan and non-metropolitan locations | Ray, B.; Preston, V. | 2013 | Rural vs. urban communities | Cross-sectional study: To examine discrimination among visible vs. non-visible minority groups across varying geographic settings |
|
| Intersectional exposures: Exploring the health effect of Employment with KAAJAL immigrant/refugee women in Grand Erie through Photovoice | Sethi B. | 2013a | Rural vs. urban communities | Cross-sectional study: To survey immigrants’ perception of challenges in relation to health services |
|
| Newcomers health in Brantford and the counties of Brant, Haldimand and Norfolk: Perspectives of newcomers and service providers | Sethi B. | 2013b | Rural communities | Literature review: To demonstrate policy influences over immigrant women’s’ access to health services |
|
| Service delivery on rusty health care wheels: Implications for visible minority women | Sethi, B. | 2014 | Rural/small community | Ethnographic study: To use photovoice to narrate immigrant women’s experiences in relation to employment |
|
| The unequal distribution of occupational health and safety risks among immigrants to Canada compared to Canadian-born labour market participants: 1993–2005 | Smith P.M., Mustard C.A. | 2009 | Rural vs. urban communities | Cross-sectional study: To compare and examine health and safety risks among immigrants vs. non-immigrants |
|
| Understanding the leisure experiences of a minority ethnic group: South Asian teens and young adults in Canada | Tirone, S; Pedlar, A | 2000 | Rural communities | Ethnographic study: To study the effects of leisure activity among ethnic minority students in a small town |
|
| Getting Used to the Quiet: Immigrant Adolescents’ Journey to Belonging in New Brunswick, Canada | Wilson-Forsberg S. | 2012 | Rural communities | Ethnographic study: To examine the inclusion of immigrant adolescents into a small community in New Brunswick, Canada |
|
References
- Canada. Diversity Is Canada’s Strength. Available online: http://pm.gc.ca/eng/news/2015/11/26/diversitycanadas-strength (accessed on 15 December 2018).
- Kennedy, S.; Kidd, M.P.; McDonald, J.T.; Biddle, N. The Healthy Immigrant Effect: Patterns and Evidence from Four Countries. J. Int. Migr. Integr. 2015, 16, 317–332. [Google Scholar] [CrossRef]
- Kitchen, P.; Williams, A.; Chowhan, J. Sense of community belonging and health in Canada: A regional analysis. Soc. Indic. Res. 2012, 107, 103–126. [Google Scholar] [CrossRef]
- Kwak, K. An evaluation of the healthy immigrant effect with adolescents in Canada: Examinations of gender and length of residence. Soc. Sci. Med. 2016, 157, 87–95. [Google Scholar] [CrossRef] [PubMed]
- Antecol, H.; Bedard, K. Unhealthy assimilation: Why do immigrants converge to American health status levels? Demography 2006, 43, 337–360. [Google Scholar] [CrossRef] [PubMed]
- Blair, A.H.; Schneeberg, A. Changes in the “healthy migrant effect” in Canada: Are recent immigrants healthier than they were a decade ago? J. Immigr. Minor. Health 2014, 16, 136–142. [Google Scholar] [CrossRef] [PubMed]
- Hyman, I. Immigration and Health. Available online: http://publications.gc.ca/collections/Collection/H135-01-5E.pdf (accessed on 2 January 2019).
- Newbold, K.B. Self-rated health within the Canadian immigrant population: Risk and the healthy immigrant effect. Soc. Sci. Med. 2005, 60, 1359–1370. [Google Scholar] [CrossRef] [PubMed]
- Ng, E.; Wilkins, R.; Gendron, F.; Berthelot, J.M. Dynamics of Immigrants’ Health in Canada: Evidence from the National Population Health Survey; Catalogue 82-618; Statistics Canada: Ottawa, ON, Canada, 2005.
- Newbold, K.B. Chronic conditions and the healthy immigrant effect: Evidence from Canadian immigrants. J. Ethn. Migr. Stud. 2006, 32, 765–784. [Google Scholar] [CrossRef]
- Asanin, J.; Wilson, K. “I spent nine years looking for a doctor”: Exploring access to health care among immigrants in Mississauga, Ontario, Canada. Soc. Sci. Med. 2008, 66, 1271–1283. [Google Scholar] [CrossRef] [PubMed]
- Crooks, V.A.; Schuurman, N. Interpreting the results of a modified gravity model: Examining access to primary health care physicians in five Canadian provinces and territories. BMC Health Serv. Res. 2012, 12, 230. [Google Scholar] [CrossRef] [PubMed]
- Curtis, L.J.; MacMinn, W.J. Health care utilization in Canada: Twenty-five years of evidence. Can. Public Policy 2008, 34, 65–87. [Google Scholar] [CrossRef]
- Edge, S.; Newbold, K.B.; McKeary, M. Exploring socio-cultural factors that mediate, facilitate, & constrain the health and empowerment of refugee youth. Soc. Sci. Med. 2014, 117, 34–41. [Google Scholar] [CrossRef] [PubMed]
- Edge, S.; Newbold, B. Discrimination and the Health of Immigrants & Refugees: Exploring Canada’s Evidence Base and Directions for Future Research in Newcomer Receiving Countries. J. Immigr. Minor. Health 2013, 15, 141–148. [Google Scholar] [CrossRef] [PubMed]
- Rosenberg, M. Health Geography III: Old ideas, new ideas or new determinisms? Prog. Hum. Geogr. 2017, 41, 832–842. [Google Scholar] [CrossRef]
- Saposnik, G.; Redelmeier, D.A.; Lu, H.; Fuller-Thomson, E.; Lonn, E.; Ray, J.G. Myocardial infarction associated with recency of immigration to Ontario. QJM Int. J. Med. 2010, 103, 253–258. [Google Scholar] [CrossRef] [PubMed]
- Statistics Canada. Census Profile; 2016 Census (Catalogue no. 98-316-X2016001); Statistics Canada: Ottawa, ON, Canada, 2016. Available online: www12.statcan.gc.ca/census-recensement/2016/dp-pd/prof/index.cfm?Lang=E (accessed on 12 November 2018).
- Statistics Canada. Population Growth: Migratory Increase Overtakes Natural Increase; Statistics Canada: Ottawa, ON, Canada. Available online: www.statcan.gc.ca/pub/11-630-x/11-630-x2014001-eng.htm (accessed on 12 November 2018).
- Dibase, S.; Bauder, H. Immigrant settlement in Ontario: Location and local labour markets. Can. Ethn. Stud. 2005, 37, 114–136. [Google Scholar]
- Hiebert, D.; Schuurman, N.; Smith, H. Multiculturalism “On the Ground”: The Social Geography of Immigrant and Visible Minority Populations in Montreal, Toronto, and Vancouver; Centre of Excellence for Research on Immigration and Diversity: Vancouver, BC, Canada, 2007. [Google Scholar]
- Lung-Amam, W. Malls of meaning: Building Asian America in Silicon Valley suburbia. J. Am. Ethn. Hist. 2015, 34, 18–53. [Google Scholar] [CrossRef]
- Wilson, J.; Singer, A. Immigrants in 2010 Metropolitan America: A Decade of Change; Metropolitan Policy Program, Brookings Institution: Washington, DC, USA, 2011. [Google Scholar]
- Abu-Ayyash, C.; Brochu, P. The uniqueness of the immigrant experience across Canada: A closer look at the region of Waterloo. Our Divers. Cities 2006, 2, 20–26. [Google Scholar]
- Carter, T.; Morrish, M.; Amoyaw, B. Attracting immigrants to smaller urban and rural communities: Lessons learned from the Manitoba Provincial Nominee Program. J. Int. Migr. Integr. Rev. De L’integration Et De La Migr. Int. 2008, 9, 161–183. [Google Scholar] [CrossRef]
- Tirone, S.; Pedlar, A. Understanding the leisure experiences of a minority ethnic group: South Asian teens and young adults in Canada. Loisir Et. Soc. Soc. Leis. 2000, 23, 145–169. [Google Scholar] [CrossRef]
- Walton-Roberts, M. Regional Immigration and Dispersal: Lessons from Small- and Medium-Sized Urban Centres in British Columbia. Can. Ethn. Stud. 2005, 37, 12–34. [Google Scholar]
- Ehrensaft, P.; Beeman, J. Distance and Diversity in Nonmetropolitan Economies in Rural and Small Town Canada; Thompson Educational Publishing: Toronto, ON, USA, 1992; pp. 193–224. ISBN 978-155-077-041-4. [Google Scholar]
- Newcomer Centre of Peel. Rural Employment Initiative. Available online: http://www.ncpeel.ca/services/look-for-employment (accessed on 20 February 2017).
- Government of Canada. Provincial Nominee Program: Who Can Apply. Available online: https://www.canada.ca/en/immigration-refugees-citizenship/services/immigrate-canada/provincial-nominees/eligibility.html (accessed on 20 September 2018).
- Statistics Canada. Immigration and Ethnocultural Diversity: Key Results from the 2016 Census. Available online: http://www.statcan.gc.ca/daily-quotidien/171025/dq171025b-eng.htm (accessed on 15 December 2018).
- Sanez, R.; Donato, K.; Gouveia, L.; Torres, C. Latinos in the South: A glimpse of ongoing trends and research South. Rural Sociol. 2003, 19, 1–19. [Google Scholar]
- Hamm, L.; Doğurga, S.L.; Scott, A. Leading a diverse school during times of demographic change in rural Canada: Reflection, action and suggestions for practice. Citizsh. Teach. Learn. 2016, 11, 211–230. [Google Scholar] [CrossRef]
- Caldwell, W.; Labute, B.; Khan, B.; D’souza Rea, N. Attracting and Retaining Newcomers in Rural Communities and Small Towns; University of Guelph: Guelph, ON, Canada, 2007. [Google Scholar]
- Matthews, R.; Pendakur, R.; Young, N. Social capital, labour markets, and job-finding in urban and rural regions: Comparing paths to employment in prosperous cities and stressed rural communities in Canada. Sociol. Rev. 2009, 57, 306–330. [Google Scholar] [CrossRef]
- Sibley, L.M.; Weiner, J.P. An evaluation of access to health care services along the rural-urban continuum in Canada. BMC Health Serv. Res. 2011, 11, 20. [Google Scholar] [CrossRef] [PubMed]
- Walton-Roberts, M.W. Immigration, the university and the welcoming second tier city. J. Int. Migr. Integr. 2001, 12, 453–473. [Google Scholar] [CrossRef]
- Mcintyre, S.; Ellaway, A.; Cummins, S. Place effects on health: How can we conceptualise, operationalise and measure them? Soc. Sci. Med. 2002, 55, 125–139. [Google Scholar] [CrossRef]
- World Health Organization. Closing the Gap in a Generation: Health Equity through Action on Social Determinants of Health. Available online: https://apps.who.int/iris/bitstream/handle/10665/43943/9789241563703_eng.pdf;jsessionid=E648C26F2E8A5D9713591D371B7A6EEB?sequence=1 (accessed on 6 February 2019).
- Sanmartin, C.; Ross, N. Experiencing difficulties accessing first-contact health services in Canada. Healthc. Policy 2006, 1, 103–109. [Google Scholar] [CrossRef] [PubMed]
- Constant, A.F.; García-Muñoz, T.; Neuman, S.; Neuman, T. A “healthy immigrant effect” or a “sick immigrant effect”? Selection and policies matter. Eur. J. Health Econ. 2018, 19, 103–121. [Google Scholar] [CrossRef] [PubMed]
- McDonald, J.T.; Kennedy, S. Insights into the ‘healthy immigrant effect’: Health status and health service use of immigrants to Canada. Soc. Sci. Med. 2004, 59, 1613–1627. [Google Scholar] [CrossRef] [PubMed]
- Harrington, D.W.; Wilson, K.; Rosenberg, M.W. Waiting for a specialist consultation for a new condition in Ontario: Impacts on patients’ lives. Healthc. Policy 2014, 9, 90. [Google Scholar] [CrossRef] [PubMed]
- Asanin, D.J.; Wilson, K. “Education? It is irrelevant to my job now and it makes me very depressed…”: Exploring the health impacts of under/unemployment among highly-skilled recent immigrants in Canada. Ethn. Health 2009, 14, 185–204. [Google Scholar] [CrossRef]
- Asanin, D.J.; Wilson, K. “My health has improved because I always have everything I need here…”: A qualitative exploration of health improvement and decline among immigrants. Soc. Sci. Med. 2010, 70, 1219–1228. [Google Scholar]
- Yu, J.; Teschke, K. The healthy immigrant effect and active commuting. J. Transp. Health 2018, 10, 253–261. [Google Scholar] [CrossRef]
- Harrington, D.W.; Wilson, K.; Rosenberg, M.; Bell, S. Access granted! Barriers endure: Determinants of difficulties accessing specialist care when required in Ontario, Canada. BMC Health Serv. Res. 2013, 13, 146. [Google Scholar] [CrossRef] [PubMed]
- Pattison-Meek, J.M. Democratic Citizenship Education in Rural High Schools: Navigating Difference and Conflict in Three Ontario Classrooms. Ph.D. Dissertation, University of Toronto, Toronto, ON, Canada, 2016. [Google Scholar]
- Labonté, R.; Packer, C.; Klassen, N. Managing health pofessional migration from sub-Saharan Africa to Canada: A stakeholder inquiry into policy options. Hum. Resour. Health 2006, 4, 22. [Google Scholar] [CrossRef] [PubMed]
- Wilson-Forsberg, S. Getting Used to the Quiet: Immigrant Adolescents’ Journey to Belonging in New Brunswick, Canada; McGill-Queen’s University Press: Montreal, QC, Canada, 2012. [Google Scholar]
- Caldwell, W.J.; Kraehling, P.; Huff, J.; Kaptur, S. Healthy Rural Communities: Strategies and Models of Practice. Available online: https://www.publichealthontario.ca/en/ServicesAndTools/Documents/LDCP/HealthyRuralCommunitiesToolKit%20compressed.pdf (accessed on 10 November 2018).
- Hartley, D. Rural health disparities, population health, and rural culture. Am. J. Public Health 2004, 94, 1675–1678. [Google Scholar] [CrossRef] [PubMed]
- Jackson, R.J. The impact of the built environment on health: An emerging field. Am. J. Public Health 2003, 93, 1382–1384. [Google Scholar] [CrossRef] [PubMed]
- Pampalon, R.; Hamel, D.; Gamache, P. Health inequalities in urban and rural Canada: Comparing inequalities in survival according to an individual and area-based deprivation index. Health Place 2010, 16, 416–420. [Google Scholar] [CrossRef] [PubMed]
- DesMeules, M.; Pong, R.; Lagacé, C.; Heng, D.; Manuel, D.; Pitblado, R.; Bollman, R.; Guernsey, J.; Kazanjian, A.; Koren, I. How Healthy Are Rural Canadians? An Assessment of Their Health Status and Health Determinants; Canadian Institute for Health Information: Ottawa, ON, Canada, 2006; ISBN 101-553-928-814. [Google Scholar]
- Pong, R.W.; DesMeules, M.; Lagacé, C. Rural–urban disparities in health: How does Canada fare and how does Canada compare with Australia? Aust. J. Rural Health 2009, 17, 58–64. [Google Scholar] [CrossRef] [PubMed]
- Bruner, M.W.; Lawson, J.; Pickett, W.; Boyce, W.; Janssen, I. Rural Canadian adolescents are more likely to be obese compared with urban adolescents. Int. J. Pediatr. Obes. 2008, 3, 205–211. [Google Scholar] [CrossRef] [PubMed]
- Karunanayake, C.P.; Rennie, D.C.; Hagel, L.; Lawson, J.; Janzen, B.; Pickett, W.; Dosman, J.A.; Phawa, P.; Saskatchewan Rural Health Study Group. Access to specialist care in rural Saskatchewan: The Saskatchewan rural health study. Healthcare 2015, 3, 84–99. [Google Scholar] [CrossRef] [PubMed]
- Public Health Ontario. Healthy Rural Communities Tool Kit: A Guide for Rural Municipalities. Available online: https://www.publichealthontario.ca/en/ServicesAndTools/Documents/LDCP/HealthyRuralCommunitiesToolKit%20compressed.pdf (accessed on 13 December 2018).
- Lynam, M.J.; Cowley, S. Understanding marginalization as a social determinant of health. Crit. Public Health 2002, 17, 137–149. [Google Scholar] [CrossRef]
- Rodrigues, P.; Dean, J.; Kirkpatrick, S.; Berbary, L.; Scott, S. Exploring experiences of the food environment among immigrants living in the Region of Waterloo, Ontario. Can. J. Public Health 2016, 107, 53–59. [Google Scholar] [CrossRef] [PubMed]
- Alter, D.A.; Austin, P.C.; Tu, J.V. Canadian Cardiovascular Outcomes Research Team. Community factors, hospital characteristics and inter-regional outcome variations following acute myocardial infarction in Canada. Can. J. Cardiol. 2005, 21, 247–255. [Google Scholar] [PubMed]
- Frank, L.; Engelke, P.; Schmid, T. Health and Community Design: The Impact of the Built Environment on Physical Activity; Island Press: Washington, DC, USA, 2003; ISBN 978-155-963-917-0. [Google Scholar]
- Frumkin, H. Urban sprawl and public health. Public Health Rep. 2016, 117, 201. [Google Scholar] [CrossRef]
- Newman, L.; Baum, F.; Javanparast, S.; O’Rourke, K.; Carlon, L. Addressing social determinants of health inequities through settings: A rapid review. Health Promot. Int. 2015, 30, 126–143. [Google Scholar] [CrossRef] [PubMed]
- Arksey, H.; O’Malley, L. Scoping studies: Towards a methodological framework. Int. J. Soc. Res. Methodol. 2005, 8, 19–32. [Google Scholar] [CrossRef]
- Levac, D.; Colquhoun, H.; O’Brien, K.K. Scoping studies: Advancing the methodology. Implement. Sci. 2010, 5, 69. [Google Scholar] [CrossRef] [PubMed]
- Sanou, D.; O’Reilly, E.; Ngnie-Teta, I.; Batal, M.; Mondain, N.; Andrew, C.; Newbold, B.K.; Bourgeault, I.L. Acculturation and nutritional health of immigrants in Canada: A scoping review. J. Immigr. Minor. Health 2014, 16, 24–34. [Google Scholar] [CrossRef] [PubMed]
- Marmot, M.; Wilkinson, R. Social Determinants of Health: The Solid Facts. Available online: http://www.euro.who.int/__data/assets/pdf_file/0005/98438/e81384.pdf (accessed on 15 December 2018).
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; Prisma Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef] [PubMed]
- Silverman, R.M.; Patterson, K.L. Qualitative Research Methods for Community Development; Routledge: New York, NY, USA, 2015; ISBN 978-041-574-036-4. [Google Scholar]
- Brown, N.R. Housing Experiences of Recent Immigrants to Canada’s Small Cities: The Case of North Bay, Ontario. J. Int. Migr. Integr. 2017, 18, 719–747. [Google Scholar] [CrossRef]
- Caxaj, C.S.; Gill, N.K. Belonging and Mental Wellbeing Among a Rural Indian-Canadian Diaspora: Navigating Tensions in “Finding a Space of Our Own”. Qual. Health Res. 2017, 27, 1119–1132. [Google Scholar] [CrossRef] [PubMed]
- Chadwick, K.A.; Collins, P.A. Examining the relationship between social support availability, urban center size, and self-perceived mental health of recent immigrants to Canada: A mixed-methods analysis. Soc. Sci. Med. 2015, 128, 220–230. [Google Scholar] [CrossRef] [PubMed]
- Cho, L. Eating Chinese: Culture on the Menu in Small Town Canada; University of Toronto Press: Toronto, ON, Canada, 2010; ISBN 978-144-261-040-8. [Google Scholar]
- Higginbottom, G.M.; Safipour, J.; Yohani, S.; O’Brien, B.; Mumtaz, Z.; Paton, P. An ethnographic study of communication challenges in maternity care for immigrant women in rural Alberta. Midwifery 2015, 31, 297–304. [Google Scholar] [CrossRef] [PubMed]
- Higginbottom, G.M.; Safipour, J.; Yohani, S.; O’Brien, B.; Mumtaz, Z.; Paton, P.; Chiu, Y.; Barolia, R. An ethnographic investigation of the maternity healthcare experience of immigrants in rural and urban Alberta, Canada. BMC Pregnancy Childbirth 2016, 16, 20. [Google Scholar] [CrossRef] [PubMed]
- Hulme, J.; Dunn, S.; Guilbert, E.; Soon, J.; Norman, W. Barriers and facilitators to family planning access in Canada. Healthc. Policy 2015, 10, 48. [Google Scholar] [CrossRef] [PubMed]
- Lauzon, A.; Farabakhsh, R. The Power of Collaborative Inquiry and Metaphor in Meeting the Health Literacy Needs of Rural Immigrant Women: A Case of Parent Education. In Handbook of Research on Adult and Community Health Education: Tools, Trends, and Methodologies; IGI Global: Hershey, PA, USA, 2014; pp. 51–67. [Google Scholar] [CrossRef]
- Pahwa, P.; Karunanayake, C.P.; McCrosky, J.; Thorpe, L. Longitudinal trends in mental health among ethnic groups in Canada. Chronic Dis. Inj. Can. 2012, 32, 164–176. [Google Scholar] [PubMed]
- Sethi, B. Intersectional Exposures: Exploring the Health Effect of Employment with KAAJAL Immigrant/Refugee Women in Grand Erie through Photovoice. Ph.D. Dissertation, Laurier University, Waterloo, ON, Canada, 2014. [Google Scholar]
- Sethi, B. Newcomers health in Brantford and the counties of Brant, Haldimand and Norfolk: Perspectives of newcomers and service providers. J. Immigr. Minor. Health 2013, 15, 925–931. [Google Scholar] [CrossRef] [PubMed]
- Sethi, B. Service delivery on rusty health care wheels: Implications for visible minority women. J. Evid.-Based Soc. Work 2013, 10, 522–532. [Google Scholar] [CrossRef] [PubMed]
- Hall, P.V.; Khan, A.J. Differences in hi-tech immigrant earnings and wages across Canadian cities. Can. Geogr. Le Géographe Can. 2008, 52, 271–290. [Google Scholar] [CrossRef]
- Smith, P.M.; Mustard, C.A. The unequal distribution of occupational health and safety risks among immigrants to Canada compared to Canadian-born labour market participants: 1993–2005. Saf. Sci. 2010, 48, 1296–1303. [Google Scholar] [CrossRef]
- Islam, N. The dilemma of physician shortage and international recruitment in Canada. Int. J. Health Policy Manag. 2014, 3, 29. [Google Scholar] [CrossRef] [PubMed]
- McDonald, J.T.; Worswick, C. The migration decisions of physicians in Canada: The roles of immigrant status and spousal characteristics. Soc. Sci. Med. 2012, 75, 1581–1588. [Google Scholar] [CrossRef] [PubMed]
- Dion, K.L. Immigrants’ perceptions of housing discrimination in Toronto: The Housing New Canadians project. J. Soc. Issues 2001, 57, 523–539. [Google Scholar] [CrossRef]
- Hulchanski, J.D. Immigrants and access to housing: How welcome are newcomers to Canada. In Proceedings of the Metropolis Year II Conference, Montreal, QC, Canada, 23–26 November 1997; University of Toronto: Toronto, ON, Canada, 1997; Volume 4, p. 2006. [Google Scholar]
- Zhuang, Z.C. Rethinking Multicultural Planning: An Empirical Study of Ethnic Retailing. Can. J. Urban Res. 2013, 22, 90–116. [Google Scholar]
- OPHA. Health in Cities: The Role for Public Health. Available online: http://www.opha.on.ca/OPHA/media/Resources/Position-Papers/2003-01_pp.pdf?ext=.pdf (accessed on 13 December 2018).
- Government of Ontario. Community Immigrant Retention in Rural Ontario. Available online: https://www.ontario.ca/page/community-immigrant-retention-rural-ontario-program (accessed on 15 December 2018).
| Review Step | Application |
|---|---|
| Step 1: Identifying research question | The research question guiding this study is: “How do rural settlement patterns influence health and social determinants of health for immigrant populations in Canada?” |
| Step 2: Identifying relevant studies | The following data sources were to be used for this study: PsycInfo, PubMed, Web of Science, and Scopus. Inclusion criteria
|
| Step 3: Selecting studies | The team used an iterative approach to eliminate studies based on exclusion criteria and contents that do not address the research question or fulfill our objectives. |
| Step 4: Charting data | A descriptive summary table was used to highlight characteristics found in articles (refer to Table A1 in Appendix). A common framework was used to collect data from all articles to track themes found in the data. |
| Step 5: Summarizing and reporting the results | This article summarizes the results of this study and provides discussion of existing literature and its effect on future research on this topic. |
| Step 6: Consultation | Approximately 17 key informants were interviewed across Canada on this topic from multiple sectors of practice. Findings from the consultation will be elaborated in a forthcoming article. |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Patel, A.; Dean, J.; Edge, S.; Wilson, K.; Ghassemi, E. Double Burden of Rural Migration in Canada? Considering the Social Determinants of Health Related to Immigrant Settlement Outside the Cosmopolis. Int. J. Environ. Res. Public Health 2019, 16, 678. https://doi.org/10.3390/ijerph16050678
Patel A, Dean J, Edge S, Wilson K, Ghassemi E. Double Burden of Rural Migration in Canada? Considering the Social Determinants of Health Related to Immigrant Settlement Outside the Cosmopolis. International Journal of Environmental Research and Public Health. 2019; 16(5):678. https://doi.org/10.3390/ijerph16050678
Chicago/Turabian StylePatel, Asiya, Jennifer Dean, Sara Edge, Kathi Wilson, and Effat Ghassemi. 2019. "Double Burden of Rural Migration in Canada? Considering the Social Determinants of Health Related to Immigrant Settlement Outside the Cosmopolis" International Journal of Environmental Research and Public Health 16, no. 5: 678. https://doi.org/10.3390/ijerph16050678
APA StylePatel, A., Dean, J., Edge, S., Wilson, K., & Ghassemi, E. (2019). Double Burden of Rural Migration in Canada? Considering the Social Determinants of Health Related to Immigrant Settlement Outside the Cosmopolis. International Journal of Environmental Research and Public Health, 16(5), 678. https://doi.org/10.3390/ijerph16050678





