Cardiovascular Disease Healthcare Utilization in Sub-Saharan Africa: A Scoping Review
Abstract
1. Introduction
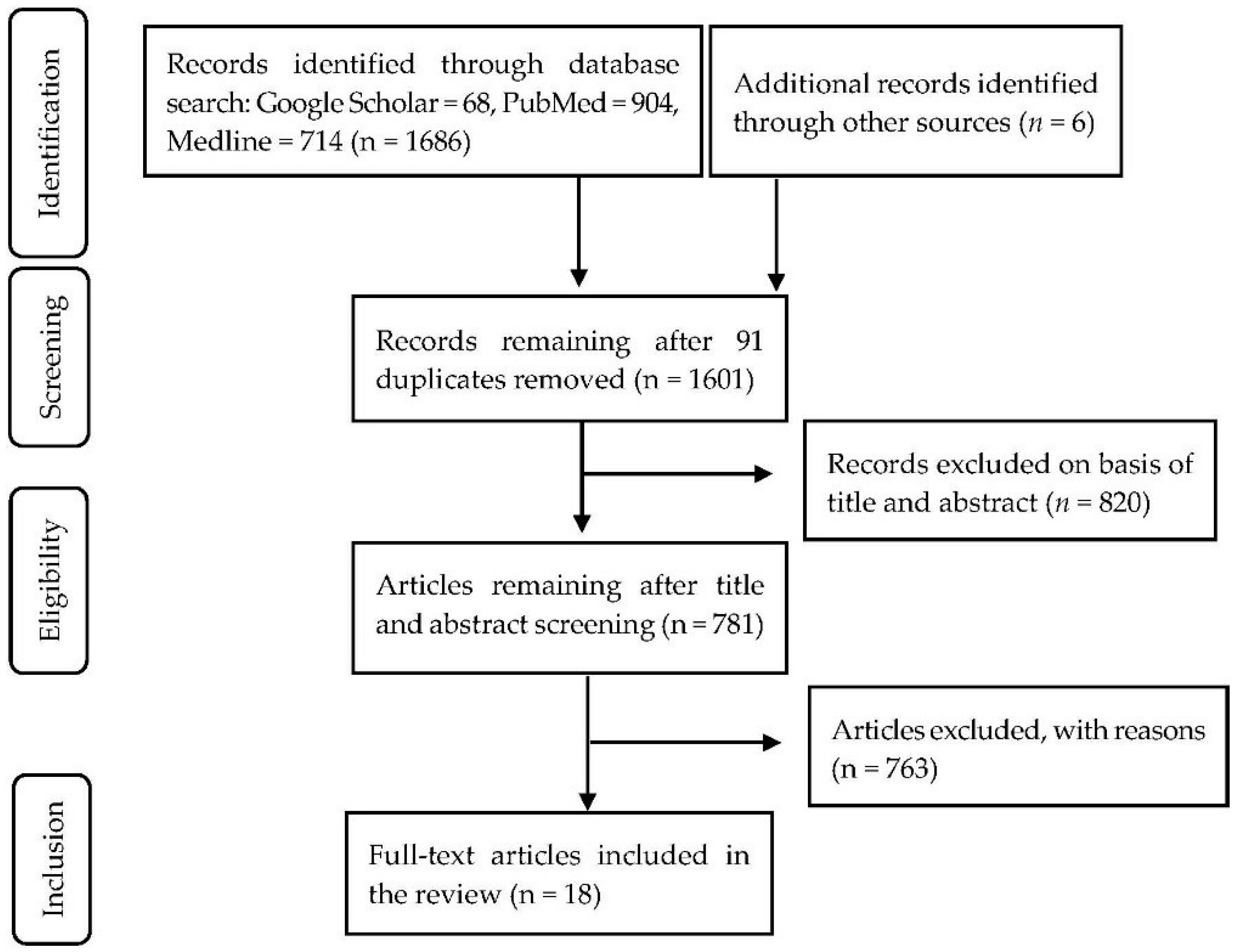
2. Materials and Methods
2.1. Search Strategy and Selection Criteria
2.2. Data Extraction and Synthesis
3. Results
3.1. Overview of Selected Studies
3.2. Healthcare Utilization
3.2.1. Spectrum of CVD Care
3.2.2. Utilization Indicators
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Bor, J.; Herbst, A.J.; Newell, M.L.; Barnighausen, T. Increases in adult life expectancy in rural South Africa: Valuing the scale-up of HIV treatment. Science 2013, 339, 961–965. [Google Scholar] [CrossRef] [PubMed]
- Kadiri, S.; Salako, B.L. Cardiovascular risk factors in middle aged Nigerians. East Afr. Med. J. 1997, 74, 303–306. [Google Scholar] [PubMed]
- Fezeu, L.; Minkoulou, E.; Balkau, B.; Kengne, A.-P.; Awah, P.; Unwin, N.; Alberti, G.K.; Mbanya, J.-C. Association between socioeconomic status and adiposity in urban Cameroon. Int. J. Epidemiol. 2005, 35, 105–111. [Google Scholar] [CrossRef] [PubMed]
- Mayosi, B.M.; Flisher, A.J.; Lalloo, U.G.; Sitas, F.; Tollman, S.M.; Bradshaw, D. The burden of non-communicable diseases in South Africa. Lancet 2009, 374, 934–947. [Google Scholar] [CrossRef]
- World Health Organization. Noncommunicable Diseases. Available online: http://www.who.int/news-room/fact-sheets/detail/noncommunicable-diseases (accessed on 1 June 2018).
- Lim, S.S.; Vos, T.; Flaxman, A.D.; Danaei, G.; Shibuya, K.; Adair-Rohani, H.; AlMazroa, M.A.; Amann, M.; Anderson, H.R.; Andrews, K.G. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: A systematic analysis for the Global Burden of Disease Study 2010. Lancet 2012, 380, 2224–2260. [Google Scholar] [CrossRef]
- Bibbins-Domingo, K.; Chertow, G.M.; Coxson, P.G.; Moran, A.; Lightwood, J.M.; Pletcher, M.J.; Goldman, L. Projected effect of dietary salt reductions on future cardiovascular disease. N. Engl. J. Med. 2010, 362, 590–599. [Google Scholar] [CrossRef] [PubMed]
- Imamura, F.; Micha, R.; Khatibzadeh, S.; Fahimi, S.; Shi, P.; Powles, J.; Mozaffarian, D.; Global Burden of Diseases Nutrition; Chronic Diseases Expert Group. Dietary quality among men and women in 187 countries in 1990 and 2010: A systematic assessment. Lancet Glob. Health 2015, 3, e132–e142. [Google Scholar] [CrossRef]
- Maimela, E.; Alberts, M.; Modjadji, S.E.; Choma, S.S.; Dikotope, S.A.; Ntuli, T.S.; Van Geertruyden, J.P. The Prevalence and Determinants of Chronic Non-Communicable Disease Risk Factors amongst Adults in the Dikgale Health Demographic and Surveillance System (HDSS) Site, Limpopo Province of South Africa. PLoS ONE 2016, 11, e0147926. [Google Scholar] [CrossRef]
- Sliwa, K.; Wilkinson, D.; Hansen, C.; Ntyintyane, L.; Tibazarwa, K.; Becker, A.; Stewart, S. Spectrum of heart disease and risk factors in a black urban population in South Africa (the Heart of Soweto Study): A cohort study. Lancet 2008, 371, 915–922. [Google Scholar] [CrossRef]
- Stewart, S.; Libhaber, E.; Carrington, M.; Damasceno, A.; Abbasi, H.; Hansen, C.; Wilkinson, D.; Sliwa, K. The clinical consequences and challenges of hypertension in urban-dwelling black Africans: Insights from the Heart of Soweto Study. Int. J. Cardiol. 2011, 146, 22–27. [Google Scholar] [CrossRef]
- Adeboye, B.; Bermano, G.; Rolland, C. Obesity and its health impact in Africa: A systematic review. Cardiovasc. J. Afr. 2012, 23, 512–521. [Google Scholar] [CrossRef] [PubMed]
- BeLue, R.; Okoror, T.A.; Iwelunmor, J.; Taylor, K.D.; Degboe, A.N.; Agyemang, C.; Ogedegbe, G. An overview of cardiovascular risk factor burden in sub-Saharan African countries: A socio-cultural perspective. Glob. Health 2009, 5, 10. [Google Scholar] [CrossRef] [PubMed]
- Kruger, R.; Kruger, H.; Macintyre, U. The determinants of overweight and obesity among 10-to 15-year-old schoolchildren in the North West Province, South Africa–the THUSA BANA (Transition and Health during Urbanisation of South Africans; BANA, children) study. J. Public Health Nutr. 2006, 9, 351–358. [Google Scholar] [CrossRef]
- Vorster, H.H. The emergence of cardiovascular disease during urbanisation of Africans. Public Health Nutr. 2002, 5, 239–243. [Google Scholar] [CrossRef] [PubMed]
- Lunyera, J.; Kirenga, B.; Stanifer, J.W.; Kasozi, S.; van der Molen, T.; Katagira, W.; Kamya, M.R.; Kalyesubula, R. Geographic differences in the prevalence of hypertension in Uganda: Results of a national epidemiological study. PLoS ONE 2018, 13, e0201001. [Google Scholar] [CrossRef] [PubMed]
- Bhimma, R.; Naicker, E.; Gounden, V.; Nandlal, L.; Connolly, C.; Hariparshad, S. Prevalence of Primary Hypertension and Risk Factors in Grade XII Learners in KwaZulu-Natal, South Africa. Int. J. Hypertens. 2018, 2018, 3848591. [Google Scholar] [CrossRef] [PubMed]
- Rutherford, M.E.; Mulholland, K.; Hill, P.C. How access to health care relates to under-five mortality in sub-Saharan Africa: Systematic review. Trop. Med. Int. Health 2010, 15, 508–519. [Google Scholar] [CrossRef] [PubMed]
- Zere, E.; Oluwole, D.; Kirigia, J.M.; Mwikisa, C.N.; Mbeeli, T. Inequities in skilled attendance at birth in Namibia: A decomposition analysis. BMC Pregnancy Childbirth 2011, 11, 34. [Google Scholar] [CrossRef]
- Bonfrer, I.; Van de Poel, E.; Grimm, M.; Van Doorslaer, E. Does the distribution of healthcare utilization match needs in Africa? Health Policy Plan. 2013, 29, 921–937. [Google Scholar] [CrossRef]
- United Nations. About the Sustainable Development Goals. Available online: https://www.un.org/sustainabledevelopment/health/ (accessed on 1 June 2018).
- Kearney, P.M.; Whelton, M.; Reynolds, K.; Muntner, P.; Whelton, P.K.; He, J. Global burden of hypertension: Analysis of worldwide data. Lancet 2005, 365, 217–223. [Google Scholar] [CrossRef]
- Somotun, O.A.-A.; Osungbade, K.O.; Akinyemi, O.O.; Obembe, T.A.; Adeniji, F.I. What factors influence the average length of stay among stroke patients in a Nigerian tertiary hospital? Pan Afr. Med. J. 2017, 26, 228. [Google Scholar] [CrossRef] [PubMed]
- Desalu, O.O.; Wahab, K.W.; Fawale, B.; Olarenwaju, T.O.; Busari, O.A.; Adekoya, A.O.; Afolayan, J.O. A review of stroke admissions at a tertiary hospital in rural Southwestern Nigeria. Ann. Afr. Med. 2011, 10. [Google Scholar] [CrossRef] [PubMed]
- Sarfo, F.S.; Acheampong, J.W.; Appiah, L.T.; Oparebea, E.; Akpalu, A.; Bedu-Addo, G. The profile of risk factors and in-patient outcomes of stroke in Kumasi, Ghana. Ghana Med. J. 2014, 48, 127–134. [Google Scholar] [CrossRef] [PubMed]
- Huffman, M.D.; Rao, K.D.; Pichon-Riviere, A.; Zhao, D.; Harikrishnan, S.; Ramaiya, K.; Ajay, V.S.; Goenka, S.; Calcagno, J.I.; Caporale, J.E.; et al. A cross-sectional study of the microeconomic impact of cardiovascular disease hospitalization in four low- and middle-income countries. PLoS ONE 2011, 6, e20821. [Google Scholar] [CrossRef] [PubMed]
- Mash, B.; Fairall, L.; Adejayan, O.; Ikpefan, O.; Kumari, J.; Mathee, S.; Okun, R.; Yogolelo, W. A morbidity survey of South African primary care. PLoS ONE 2012, 7, e32358. [Google Scholar] [CrossRef]
- Appiah, L.T.; Sarfo, F.S.; Agyemang, C.; Tweneboah, H.O.; Appiah, N.; Bedu-Addo, G.; Opare-Sem, O. Current trends in admissions and outcomes of cardiac diseases in Ghana. Clin. Cardiol. 2017, 40, 783–788. [Google Scholar] [CrossRef]
- Rhoda, A.; Cunningham, N.; Azaria, S.; Urimubenshi, G. Provision of inpatient rehabilitation and challenges experienced with participation post discharge: Quantitative and qualitative inquiry of African stroke patients. BMC Health Serv. Res. 2015, 15, 423. [Google Scholar] [CrossRef] [PubMed]
- Owolabi, L.F.; Ibrahim, A. Stroke in young adults: A prospective study from northwestern Nigeria. ISRN Neurol. 2012, 2012, 468706. [Google Scholar] [CrossRef] [PubMed]
- Gidey, A.; Weldeyes, E. Trends in cardiovascular disease over time: A 30-year retrospective analysis of medical-ICU admissions in Addis Ababa, Ethiopia. Ethiop. Med. J. 2015, 53, 133–139. [Google Scholar]
- Goudge, J.; Gilson, L.; Russell, S.; Gumede, T.; Mills, A. Affordability, availability and acceptability barriers to health care for the chronically ill: Longitudinal case studies from South Africa. BMC Health Serv. Res. 2009, 9, 75. [Google Scholar] [CrossRef]
- Damasceno, A.; Gomes, J.; Azevedo, A.; Carrilho, C.; Lobo, V.; Lopes, H.; Madede, T.; Pravinrai, P.; Silva-Matos, C.; Jalla, S.; et al. An epidemiological study of stroke hospitalizations in Maputo, Mozambique: A high burden of disease in a resource-poor country. Stroke 2010, 41, 2463–2469. [Google Scholar] [CrossRef] [PubMed]
- Olaleye, O.A.; Lawal, Z.I. Utilization of physiotherapy in the continuum of stroke care at a tertiary hospital in Ibadan, Nigeria. Afr. Health Sci. 2017, 17, 79–87. [Google Scholar] [CrossRef] [PubMed]
- Kaseke, F.; Stewart, A.; Gwanzura, L.; Hakim, J.; Chikwasha, V. Clinical characteristics and outcomes of patients with stroke admitted to three tertiary hospitals in Zimbabwe: A retrospective one-year study. Malawi Med. J. 2017, 29, 177–182. [Google Scholar] [CrossRef] [PubMed]
- Ansa, V.; Otu, A.; Oku, A.; Njideoffor, U.; Nworah, C.; Odigwe, C. Patient outcomes following after-hours and weekend admissions for cardiovascular disease in a tertiary hospital in Calabar, Nigeria. Cardiovasc. J. Afr. 2016, 27, 328–332. [Google Scholar] [CrossRef] [PubMed]
- Nkusi, A.E.; Muneza, S.; Nshuti, S.; Hakizimana, D.; Munyemana, P.; Nkeshimana, M.; Rudakemwa, E.; Amendezo, E. Stroke Burden in Rwanda: A Multicenter Study of Stroke Management and Outcome. World Neurosurg. 2017, 106, 462–469. [Google Scholar] [CrossRef] [PubMed]
- de Villiers, L.; Badri, M.; Ferreira, M.; Bryer, A. Stroke outcomes in a socio-economically disadvantaged urban community. S. Afr. Med. J. 2011, 101, 345–348. [Google Scholar] [CrossRef]
- Sarfo, F.S.; Akassi, J.; Awuah, D.; Adamu, S.; Nkyi, C.; Owolabi, M.; Ovbiagele, B. Trends in stroke admission and mortality rates from 1983 to 2013 in central Ghana. J. Neurol. Sci. 2015, 357, 240–245. [Google Scholar] [CrossRef] [PubMed]
- Walker, R.W.; Viney, R.; Green, L.; Mawanswila, M.; Maro, V.P.; Gjertsen, C.; Godfrey, H.; Smailes, R.; Gray, W.K. Trends in stroke admissions to a Tanzanian hospital over four decades: A retrospective audit. Trop. Med. Int. Health 2015, 20, 1290–1296. [Google Scholar] [CrossRef] [PubMed]
- Naghavi, M.; Forouzanfar, M.H. Burden of non-communicable diseases in sub-Saharan Africa in 1990 and 2010: Global Burden of Diseases, Injuries, and Risk Factors Study 2010. Lancet 2013, 381, S95. [Google Scholar] [CrossRef]
- Owolabi, M.O.; Mensah, G.A.; Kimmel, P.L.; Adu, D.; Ramsay, M.; Waddy, S.P.; Ovbiagele, B.; Rabada-Diehl, C.; Rasooly, R.; Akarolo-Anthony, S.N.; et al. Understanding the rise in cardiovascular diseases in Africa: Harmonising H3Africa genomic epidemiological teams and tools. Cardiovasc. J. Afr. 2014, 25, 134–136. [Google Scholar] [CrossRef] [PubMed]
- Boateng, D.; Wekesah, F.; Browne, J.L.; Agyemang, C.; Agyei-Baffour, P.; Aikins, A.D.; Smit, H.A.; Grobbee, D.E.; Klipstein-Grobusch, K. Knowledge and awareness of and perception towards cardiovascular disease risk in sub-Saharan Africa: A systematic review. PLoS ONE 2017, 12, e0189264. [Google Scholar] [CrossRef] [PubMed]
- Ataklte, F.; Erqou, S.; Kaptoge, S.; Taye, B.; Echouffo-Tcheugui, J.B.; Kengne, A.P. Burden of undiagnosed hypertension in sub-saharan Africa: A systematic review and meta-analysis. Hypertension 2015, 65, 291–298. [Google Scholar] [CrossRef] [PubMed]
- Temu, T.M.; Kirui, N.; Wanjalla, C.; Ndungu, A.M.; Kamano, J.H.; Inui, T.S.; Bloomfield, G.S. Cardiovascular health knowledge and preventive practices in people living with HIV in Kenya. BMC Infect. Dis. 2015, 15, 421. [Google Scholar] [CrossRef] [PubMed]
- Aminde, L.N.; Takah, N.; Ngwasiri, C.; Noubiap, J.J.; Tindong, M.; Dzudie, A.; Veerman, J.L. Population awareness of cardiovascular disease and its risk factors in Buea, Cameroon. BMC Public Health 2017, 17, 545. [Google Scholar] [CrossRef] [PubMed]
- Jones, R. Is length of stay a reliable efficiency measure. Br. J. Healthc. Manag. 2015, 21, 344–345. [Google Scholar] [CrossRef]
- Loewenson, R. Structural adjustment and health policy in Africa. Int. J. Health Serv. 1993, 23, 717–730. [Google Scholar] [CrossRef] [PubMed]
- Whitehead, M.; Dahlgren, G.; Evans, T. Equity and health sector reforms: Can low-income countries escape the medical poverty trap? Lancet 2001, 358, 833–836. [Google Scholar] [CrossRef]
- Mbewu, A. The burden of cardiovascular disease in sub-Saharan Africa: Burden of cardiovascular disease. SA Heart J. 2009, 6, 4–10. [Google Scholar]
- Murray, C.J.; Frenk, J. A framework for assessing the performance of health systems. Bull. World Health Organ. 2000, 78, 717–731. [Google Scholar] [PubMed]
- Kleindorfer, D.; Panagos, P.; Pancioli, A.; Khoury, J.; Kissela, B.; Woo, D.; Schneider, A.; Alwell, K.; Jauch, E.; Miller, R.; et al. Incidence and short-term prognosis of transient ischemic attack in a population-based study. Stroke 2005, 36, 720–723. [Google Scholar] [CrossRef] [PubMed]
- Coull, A.J.; Lovett, J.K.; Rothwell, P.M.; Oxford Vascular, S. Population based study of early risk of stroke after transient ischaemic attack or minor stroke: Implications for public education and organisation of services. BMJ 2004, 328, 326. [Google Scholar] [CrossRef] [PubMed]
- Summers, D.; Leonard, A.; Wentworth, D.; Saver, J.L.; Simpson, J.; Spilker, J.A.; Hock, N.; Miller, E.; Mitchell, P.H.; American Heart Association Council on Cardiovascular, N.; et al. Comprehensive overview of nursing and interdisciplinary care of the acute ischemic stroke patient: A scientific statement from the American Heart Association. Stroke 2009, 40, 2911–2944. [Google Scholar] [CrossRef] [PubMed]
| Reference | Country | Objective(s) | Study Focus | Study Design and Sample Size | Summary of Findings on Access to Care and Determinants |
|---|---|---|---|---|---|
| [23] | Nigeria | To understand length of stay (LOS) and determinants of stroke | Stroke inpatient care | Retrospective quantitative study (143 patients) |
|
| [24] | Nigeria | Reviewing clinical patterns | Stroke inpatient care | Retrospective quantitative study (101 patients) |
|
| [25] | Ghana | To describe risk factors, clinical types, and stroke inpatient mortality | Stroke inpatient care | Observational, prospective quantitative study (265 patients) |
|
| [26] | Tanzania | Estimating individual and household economic impact of cardiovascular disease | Cardiovascular disease (CVD) inpatient care | Retrospective, quantitative study (498 patients) |
|
| [27] | South Africa | Determining range and prevalence of reasons for attending outpatient care | All outpatient enquiries | Prospective cross-sectional survey, quantitative study (18,856 consultations) |
|
| [28] | Ghana | Assessing CVD admissions and outcomes | Overall CVD inpatient care | Retrospective (11 years) quantitative (4226 patients) |
|
| [29] | South Africa, Rwanda and Tanzania | To assess post-stroke rehabilitation inpatient care services | Stroke inpatient care, rehabilitation | Retrospective, mixed methods surveys (South Africa = 168, Rwanda = 139, Tanzania = 145) |
|
| [30] | Nigeria | To review patterns, types, and case fatality of stroke in young adults | Stroke inpatient care | Prospective quantitative study (71 patients) |
|
| [31] | Ethiopia | To describe trends of medical intensive care unit admission over 30 years in Ethiopia | CVD inpatient care | Retrospective quantitative study (500 patients) |
|
| [32] | South Africa | Describing household experiences in accessing care for chronic illness in rural South Africa | Chronic care utilization | Household survey and qualitative longitudinal study(280 households) |
|
| [33] | Mozambique | To assess incidence, characteristics, and short-term consequences of stroke hospitalization in Maputo | Stroke inpatient care | Prospective quantitative study (651 patients) |
|
| [34] | Nigeria | To investigate referral patterns and utilization of physiotherapy for stroke care at a hospital in Nigeria | Stroke inpatient physiotherapy | Four-year retrospective quantitative study (783 patients) |
|
| [35] | Zimbabwe | Description of clinical characteristics and outcomes of stroke patients in tertiary hospitals in Zimbabwe | Stroke inpatient care | Retrospective quantitative study (450 patients) |
|
| [36] | Nieria | Determining differences in CVD mortality admissions between weekend and after-hours | CVD inpatient care | Three-year retrospective, quantitative study (339 patients) |
|
| [37] | Rwanda | Determining the burden of stroke in Rwanda | Stroke inpatient care | Prospective observational quantitative study (96 patients) |
|
| [38] | South Africa | To determine survival, disability, and functional stroke outcomes following discharge from hospital | Stroke inpatient care | Retrospective observational quantitative study (196 patients) |
|
| [39] | Ghana | To assess stroke admission and mortality rates | Stroke inpatient care | Retrospective quantitative study (12 233 admissions) |
|
| [40] | Tanzania | To assess stroke admissions to a tertiary referral hospital | Stroke inpatient care | Retrospective and quantitative (305 stroke admissions) |
|
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chikafu, H.; Chimbari, M.J. Cardiovascular Disease Healthcare Utilization in Sub-Saharan Africa: A Scoping Review. Int. J. Environ. Res. Public Health 2019, 16, 419. https://doi.org/10.3390/ijerph16030419
Chikafu H, Chimbari MJ. Cardiovascular Disease Healthcare Utilization in Sub-Saharan Africa: A Scoping Review. International Journal of Environmental Research and Public Health. 2019; 16(3):419. https://doi.org/10.3390/ijerph16030419
Chicago/Turabian StyleChikafu, Herbert, and Moses J. Chimbari. 2019. "Cardiovascular Disease Healthcare Utilization in Sub-Saharan Africa: A Scoping Review" International Journal of Environmental Research and Public Health 16, no. 3: 419. https://doi.org/10.3390/ijerph16030419
APA StyleChikafu, H., & Chimbari, M. J. (2019). Cardiovascular Disease Healthcare Utilization in Sub-Saharan Africa: A Scoping Review. International Journal of Environmental Research and Public Health, 16(3), 419. https://doi.org/10.3390/ijerph16030419





