Prevalence of Depression and Anxiety in Colorectal Cancer Patients: A Literature Review
Abstract
1. Introduction
2. Material and Methods
2.1. Search Strategy
2.2. Inclusion Criteria
2.3. Data Analysis
3. Results
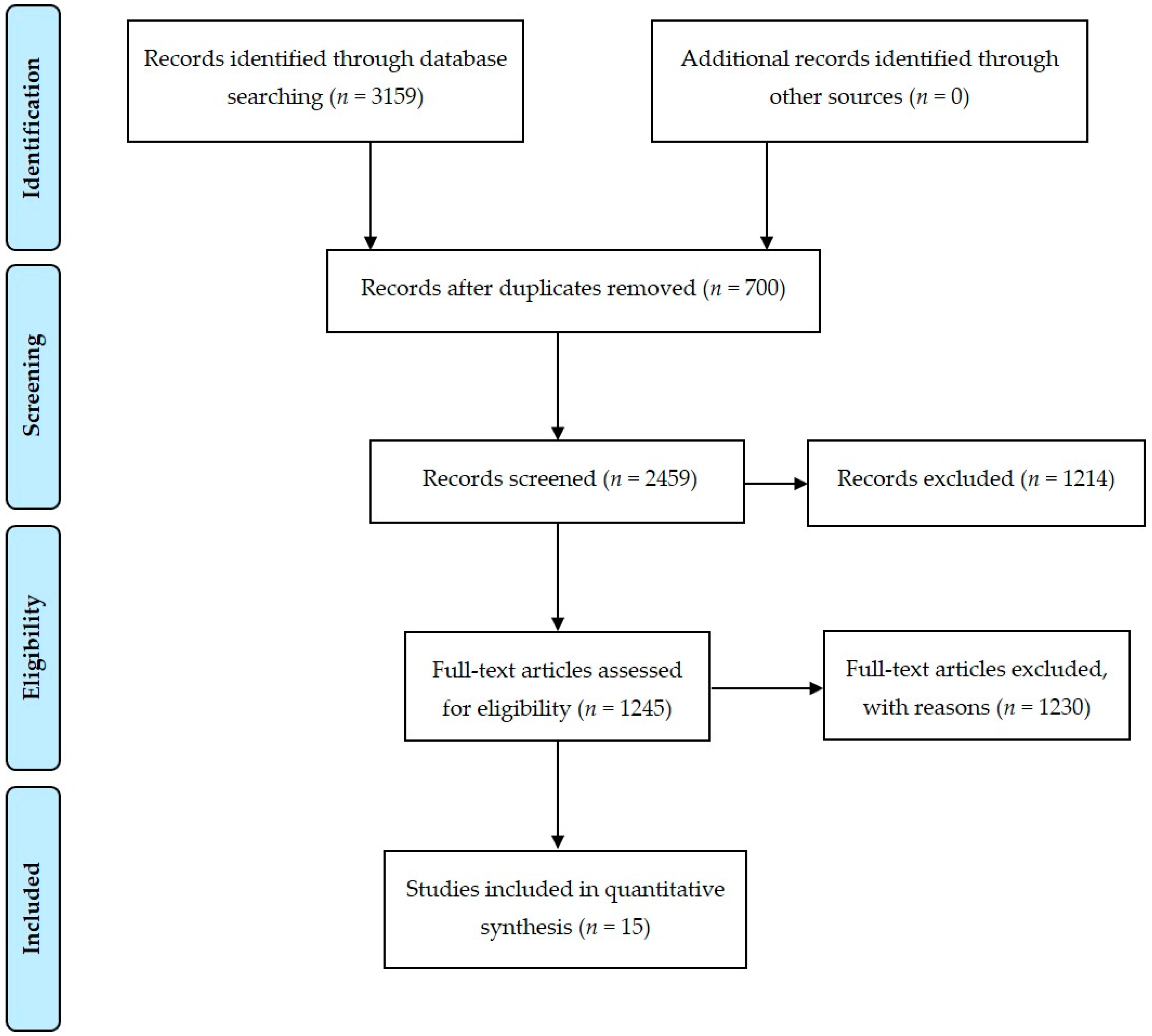
3.1. Study Selection
3.2. Characteristics of Study Participants
3.3. Diagnosis of Depression and Anxiety
3.4. Prevalence of Depression and Anxiety in CRC Patients
3.5. Relationship between Age and the Prevalence of Depression and Anxiety
3.6. Quality Assessment
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Fras, I.; Litin, E.M.; Pearson, J.S. Comparison of psychiatric symptoms in carcinoma of pancreas. Am. J. Psychiatry 1967, 123, 1553–1562. [Google Scholar] [CrossRef]
- Bray, F.; Ferlay, J.; Soerjomataram, I.; Siegel, R.L.; Torre, L.A.; Jemal, A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 2018, 68, 394–424. [Google Scholar] [CrossRef]
- Zhang, A.Y.; Cooper, G.S. Recognition of Depression and Anxiety among Elderly Colorectal Cancer Patients. Nurs. Res. Pract. 2010, 2010, 693961. [Google Scholar] [CrossRef]
- Tavoli, A.; Mohagheghi, M.A.; Montazeri, A.; Roshan, R.; Tavoli, Z.; Omidvari, S. Anxiety and depression in patients with gastrointestinal cancer: Does knowledge of cancer diagnosis matter? BMC Gastroenterol. 2007, 7, 28. [Google Scholar] [CrossRef]
- Medeiros, M.; Oshima, C.T.; Forones, N.M. Depression and Anxiety in Colorectal Cancer Patients. J. Gastrointest. Cancer 2010, 41, 179–184. [Google Scholar] [CrossRef]
- Hong, J.S.; Tian, J. Prevalence of anxiety and depression and their risk factors in Chinese cancer patients. Support Care Cancer 2014, 22, 453–459. [Google Scholar] [CrossRef]
- Abu-Helalah, M.A.; Alshraideh, H.A.; Al-Hanaqta, M.M.; Arqoub, K.H. Quality of Life and Psychological Well-Being of Colorectal Cancer Survivors in Jordan. Asian Pac. J. Cancer Prev. 2014, 15, 7653–7664. [Google Scholar] [CrossRef]
- Nikbakhsh, N.; Moudi, S.; Abbasian, S.; Khafri, S. Prevalence of depression and anxiety among cancer patients. Casp. J. Intern. Med. 2014, 5, 167–170. [Google Scholar]
- Clark, C.J.; Fino, N.F.; Liang, J.H.; Hiller, D.; Bohl, J. Depressive symptoms in older long-term colorectal cancer survivors: A population-based analysis using the SEER-Medicare healthcare outcomes survey. Support Care Cancer 2016, 24, 3907–3914. [Google Scholar] [CrossRef]
- Sun, L.M.; Liang, J.A.; Lin CLSun, S.; Kao, C.H. Risk of mood disorders in patients with colorectal cancer. J. Affect. Disord. 2017, 15, 59–65. [Google Scholar] [CrossRef]
- Mols, F.; Schoormans, D.; de Hingh, I.; Oerlemans, S.; Husson, O. Symptoms of Anxiety and Depression Among Colorectal Cancer Survivors from the Population-Based, Longitudinal PROFILES Registry: Prevalence, Predictors, and Impact on Quality of Life. Cancer 2018, 124, 2621–2628. [Google Scholar] [CrossRef]
- Walker, J.; Hansen, C.H.; Martin, P.; Symeonides, S.; Ramessur, R.; Murray, G.; Sharpe, M. Prevalence, associations, and adequacy of treatment of major depression in patients with cancer: A cross-sectional analysis of routinely collected clinical data. Lancet Psychiatry 2014, 1, 343–350. [Google Scholar] [CrossRef]
- Massie, M.L. Prevalence of depression in patients with cancer. J. Natl. Cancer Inst. Monogr. 2004, 32, 57–71. [Google Scholar] [CrossRef]
- Walker, J.; Holm Hansen, C.; Martin, P.; Sawhney, A.; Thekkumpurath, P.; Beale, C.; Symeonides, S.; Wall, L.; Murray, G.; Sharpe, M. Prevalence of depression in adults with cancer: A systematic review. Ann. Oncol. 2013, 24, 895–900. [Google Scholar] [CrossRef]
- Tsunoda, A.; Nakao, K.; Hiratsuka, K.; Yasuda, N.; Shibusawa, M.; Kusano, M. Anxiety, depression and quality of life in colorectal cancer patients. Int. J. Clin. Oncol. 2005, 10, 411–417. [Google Scholar] [CrossRef]
- Matsushita, T.; Matsushima, E.; Maruyama, M. Anxiety and depression of patients with digestive cancer. Psychiatry Clin. Neurosci. 2005, 59, 576–583. [Google Scholar] [CrossRef]
- Lynch, B.M.; Steginga, S.K.; Hawkes, A.L.; Pakenham, K.I.; Dunn, J. Describing and Predicting Psychological Distress after Colorectal Cancer. Cancer 2008, 112, 1363–1370. [Google Scholar] [CrossRef]
- Akyol, M.; Ulger, E.; Alacacioglu, A.; Kucukzeybek, Y.; Yildiz, Y.; Bayoglu, V.; Gumus, Z.; Yildiz, I.; Salman, T.; Varol, U.; et al. Sexual satisfaction, anxiety, depression and quality of life among Turkish colorectal cancer patients (Izmir Oncology Group (IZOG) study). Jpn. J. Clin. Oncol. 2015, 45, 657–664. [Google Scholar] [CrossRef]
- Satin, J.R.; Linden, W.; Phillips, M.J. Depression as a predictor of disease progression and mortality in cancer patients: A meta-analysis. Cancer 2009, 115, 5349–5361. [Google Scholar] [CrossRef]
- Sehlo, M.G.; Al Ahwal, M.S. Depression in patients with colorectal cancer. Saudi Med. J. 2013, 34, 341–347. [Google Scholar]
- Aminisani, N.; Nikbakht, H.; Asghari Jafarabadi, M.; Shamshirgaran, S.M. Depression, anxiety, and health related quality of life among colorectal cancer survivors. J. Gastrointest. Oncol. 2017, 8, 81–88. [Google Scholar] [CrossRef]
- Batty, G.D.; Russ, T.C.; Stamatakis, E.; Kivimäki, M. Psychological distress in relation to site specific cancer mortality: Pooling of unpublished data from 16 prospective cohort studies. BMJ 2017, 356, j108. [Google Scholar] [CrossRef]
- Samawi, H.H.; Shaheen, A.A.; Tang, P.A.; Heng, D.Y.C.; Cheung, W.Y.; Vickers, M.M. Risk and predictors of suicide in colorectal cancer patients: A Surveillance, Epidemiology, and End Results analysis. Curr. Oncol. 2017, 24, 513–517. [Google Scholar] [CrossRef]
- Chida, Y.; Hamer, M.; Wardle, J.; Steptoe, A. Do stress-related psychosocial factors contribute to cancer incidence and survival? Nat. Clin. Pract. Oncol. 2008, 5, 466–475. [Google Scholar] [CrossRef]
| Included Studies | Participants | N | Female (%) | CRC Patients | Mean Age (Years) | Methods | Investigators | In/Out Patients | Prevalence of Depression (%) |
|---|---|---|---|---|---|---|---|---|---|
| Fras et al., 1967, USA [1] | Gastrointestinal cancer | 110 | Not cited | 64 | N/A | MMPI | Research assistants | Inpatients | 13 |
| Tsunoda et al., 2005, Japan [15] | Colorectal cancer | 128 | 42.0 | 128 | 69 ± 10.5 | HADS | Research assistants | Outpatients | 36.7 |
| Matsushita et al., 2005, Japan [16] | Digestive cancer | 85 | 37.6 | 38 | 68.0 ± 10.3 | HADS | Research assistants | Inpatients | 28 |
| Lynch et al., 2008, Australia [17] | Colorectal cancer | 1822 | 40.0 | 1822 | Only age stratification | BSI-18 | Research assistants | Outpatients | 7.5 (6 months) 7.1 (12 months) |
| Tavoli et al., 2007, Iran [4] | Gastrointestinal cancer | 142 | 44.4 | 54 | 54.1 ± 14.8 | HADS | Psychologist | Inpatients | 57 |
| Zhang et al., 2010, USA [3] | Colorectal cancer | 56,182 | 53.4 | 56,182 | Only age stratification | ICD-9 | Psychiatrist | Outpatients | 1.6 |
| Medeiros et al., 2010, Brazil [5] | Colorectal cancer | 37 | 56.8 | 37 | 59 ± 11.5 (chemotherapy group) 65 ± 10.7 (control) | BDI | Research assistants | Inpatients | 19.4 |
| Hong et al., 2014, China [6] | Mixed | 1217 | 40.3 | 103 | 51.2 ± 13.1 | HADS | Research assistants | Inpatients | 54.4 |
| Abu-Helalah et al., 2014, Jordan [7] | Colorectal cancer | 241 | 47.7 | 241 | 56.7 ± 13.6 | HADS | Research assistants | Outpatients | 18 |
| Walker et al., 2014, UK [12] | Mixed | 21,151 | 71.0 | 3355 | 64.4 ± 11.9 | HADS/SCID-I | Psychiatrist | Inpatients/Outpatients | 7 |
| Nikbakhsh et al., 2014, Iran [8] | Mixed | 150 | 52.0 | 24 | 59.0 ± 14.3 | HADS | Research assistants | Inpatients/Outpatients | 16.9 |
| Akyol et al., 2015, Turkey [18] | Colorectal cancer | 105 | 31.0 | 105 | 52.9 ± 9.0 | HADS | Research assistants | Outpatients | 44 |
| Clark et al., 2016, USA [9] | Resected colorectal cancer | 1785 | 50.8 | 1785 | 78.0 ± 7.0 | VR-12 | Research assistants | Inpatients/Outpatients | 15.6 |
| Sun et al., 2017, Taiwan [10] | Colorectal cancer | 135,288 | 39.0 | 27,242 | 64.2 ± 13.5 | ICD-9 | Psychiatrist | Inpatients/Outpatients | 6.6 |
| Mols et al., 2018, UK [11] | Colorectal cancer | 2625 | 44.9 | 2625 | 69.4 ± 9.5 | HADS | Research assistants | Outpatients | 19 |
| Included Studies | Participants | N | Female (%) | CRC Patients | Mean Age | Methods | Investigators | In/Out-Patients | Prevalence of Anxiety (%) |
|---|---|---|---|---|---|---|---|---|---|
| Fras et al., 1967, USA [1] | Gastrointestinal cancer | 110 | Not cited | 64 | N/A | MMPI | Research assistants | Inpatients | 13 |
| Tsunoda et al., 2005, Japan [15] | Colorectal cancer | 128 | 42.0 | 128 | 69 ± 10.5 | HADS | Research assistants | Outpatients | 7.8 |
| Lynch et al., 2008, Australia [17] | Colorectal cancer | 1822 | 40.0 | 1822 | Only age stratification | BSI-18 | Research assistants | Outpatients | 7.4 (6 months) 6.7 (12 months) |
| Tavoli et al., 2007, Iran [4] | Gastrointestinal cancer | 142 | 44.4 | 54 | 54.1 ± 14.8 | HADS | Psychologist | Inpatients | 47.2 |
| Zhang et al., 2010, USA [3] | Colorectal cancer | 56,182 | 53.4 | 56,182 | Only age stratification | ICD-9 | Psychiatrist | Outpatients | 1.0 |
| Hong et al., 2014, China [6] | Mixed | 1217 | 40.26 | 103 | 51.2 ± 13.1 | HADS | Research assistants | Inpatients | 2.9 |
| Abu-Helalah et al., 2014, Jordan [7] | Colorectal cancer | 241 | 47.7 | 241 | 56.7 ± 13.6 | HADS | Research assistants | Outpatients | 23 |
| Nikbakhsh et al., 2014, Iran [8] | Mixed | 150 | 52.0 | 24 | 59.0 ± 14.3 | HADS | Research assistants | Inpatients/Outpatients | 15.4 |
| Akyol et al., 2015, Turkey [18] | Colorectal cancer | 105 | 31.0 | 105 | 52.9 ± 9.0 | HADS | Research assistants | Outpatients | 29 |
| Sun et al., 2017, Taiwan [10] | Colorectal cancer | 135,288 | 39.0 | 27,242 | 64.2 ± 13.5 | ICD-9 | Psychiatrist | Inpatients/Outpatients | 32.5 |
| Mols et al., 2018, UK [11] | Colorectal cancer | 2625 | 44.9 | 2625 | 69.4 ± 9.5 | HADS | Research assistants | Outpatients | 20.9 |
| Included Studies | Item 1 | Item 2 | Item 3 | Item 4 | Item 5 | Item 6 | Item 7 | Item 8 | Item 9 | Score |
|---|---|---|---|---|---|---|---|---|---|---|
| Fras et al., (1967) [1] | Unclear | No | Yes | No | Yes | Yes | Unclear | Yes | Yes | 5/9 |
| Tsunoda et al., (2005) [15] | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | 9/9 |
| Matsushita et al., (2005) [16] | Unclear | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | 8/9 |
| Lynch et al., (Australia) [17] | Yes | Yes | Yes | Unclear | Yes | Yes | Yes | Yes | Yes | 8/9 |
| Tavoli et al., (2007) [4] | Unclear | Unclear | Yes | Yes | Yes | Yes | Yes | Yes | Yes | 7/9 |
| Zhang et al., (2010) [3] | Yes | Yes | Yes | Unclear | Yes | Yes | Yes | Yes | Yes | 8/9 |
| Medeiros et al., (2010) [5] | Yes | Yes | No | Yes | Yes | Yes | Yes | Yes | Yes | 8/9 |
| Hong et al., (2014) [6] | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | 9/9 |
| Abu-Helalah et al., (2014) [7] | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | 9/9 |
| Walker et al., (2014) [12] | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | 9/9 |
| Nikbakhsh et al., (2014) [8] | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | 9/9 |
| Akyol et al., (2015) [18] | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | 9/9 |
| Clark et al., (2016) [9] | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | 9/9 |
| Sun et al., (2017) [10] | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | 9/9 |
| Mols et al., (2018) [11] | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | 9/9 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Peng, Y.-N.; Huang, M.-L.; Kao, C.-H. Prevalence of Depression and Anxiety in Colorectal Cancer Patients: A Literature Review. Int. J. Environ. Res. Public Health 2019, 16, 411. https://doi.org/10.3390/ijerph16030411
Peng Y-N, Huang M-L, Kao C-H. Prevalence of Depression and Anxiety in Colorectal Cancer Patients: A Literature Review. International Journal of Environmental Research and Public Health. 2019; 16(3):411. https://doi.org/10.3390/ijerph16030411
Chicago/Turabian StylePeng, Yu-Ning, Mei-Li Huang, and Chia-Hung Kao. 2019. "Prevalence of Depression and Anxiety in Colorectal Cancer Patients: A Literature Review" International Journal of Environmental Research and Public Health 16, no. 3: 411. https://doi.org/10.3390/ijerph16030411
APA StylePeng, Y.-N., Huang, M.-L., & Kao, C.-H. (2019). Prevalence of Depression and Anxiety in Colorectal Cancer Patients: A Literature Review. International Journal of Environmental Research and Public Health, 16(3), 411. https://doi.org/10.3390/ijerph16030411





