Development and Validation of Positive Smoker Identity Questionnaire (PSmoQi): A New Instrument for Smoking Cessation Correlates
Abstract
1. Introduction
1.1. Theories in Smoking Cessation
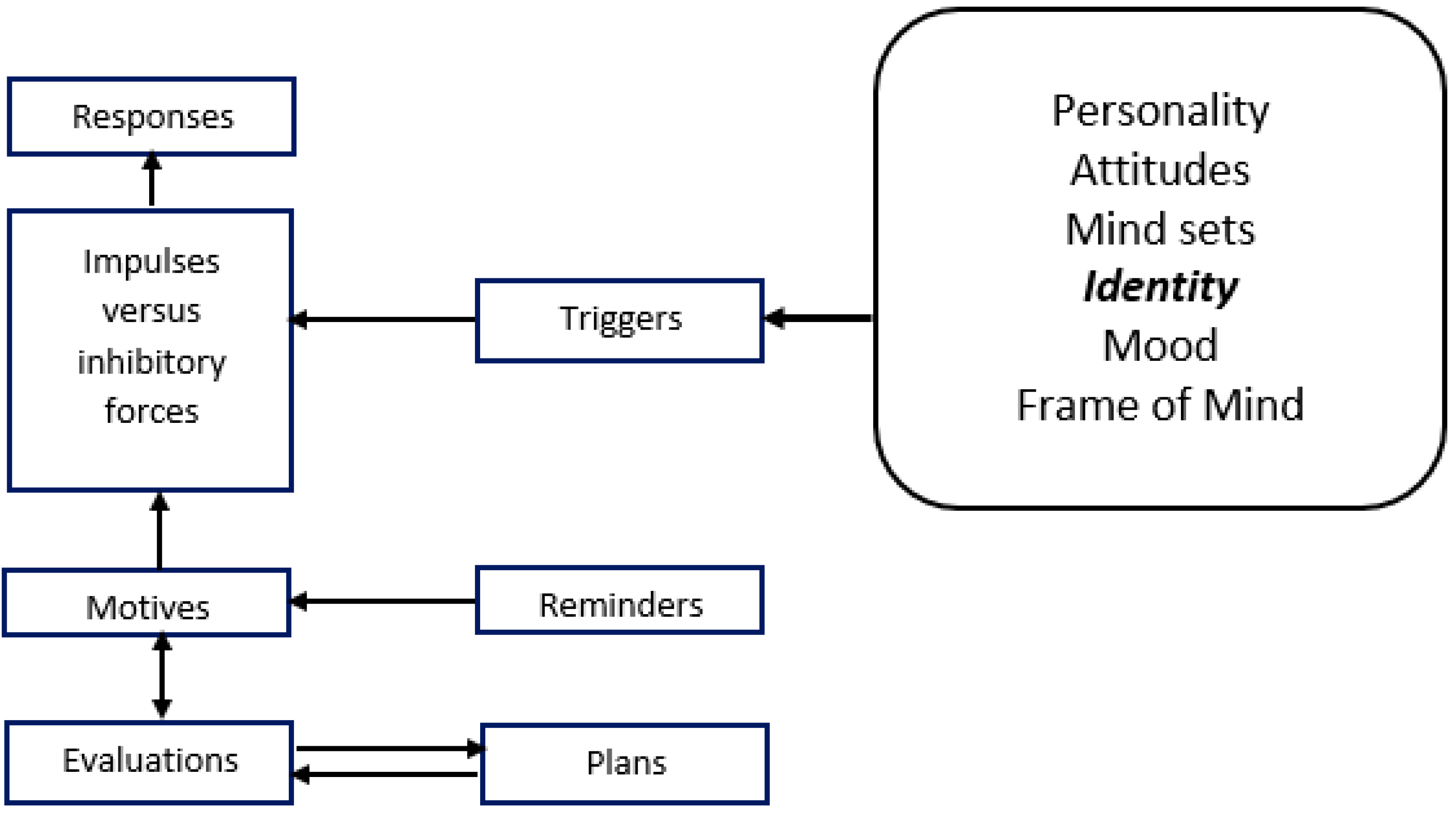
1.2. PRIME Theory
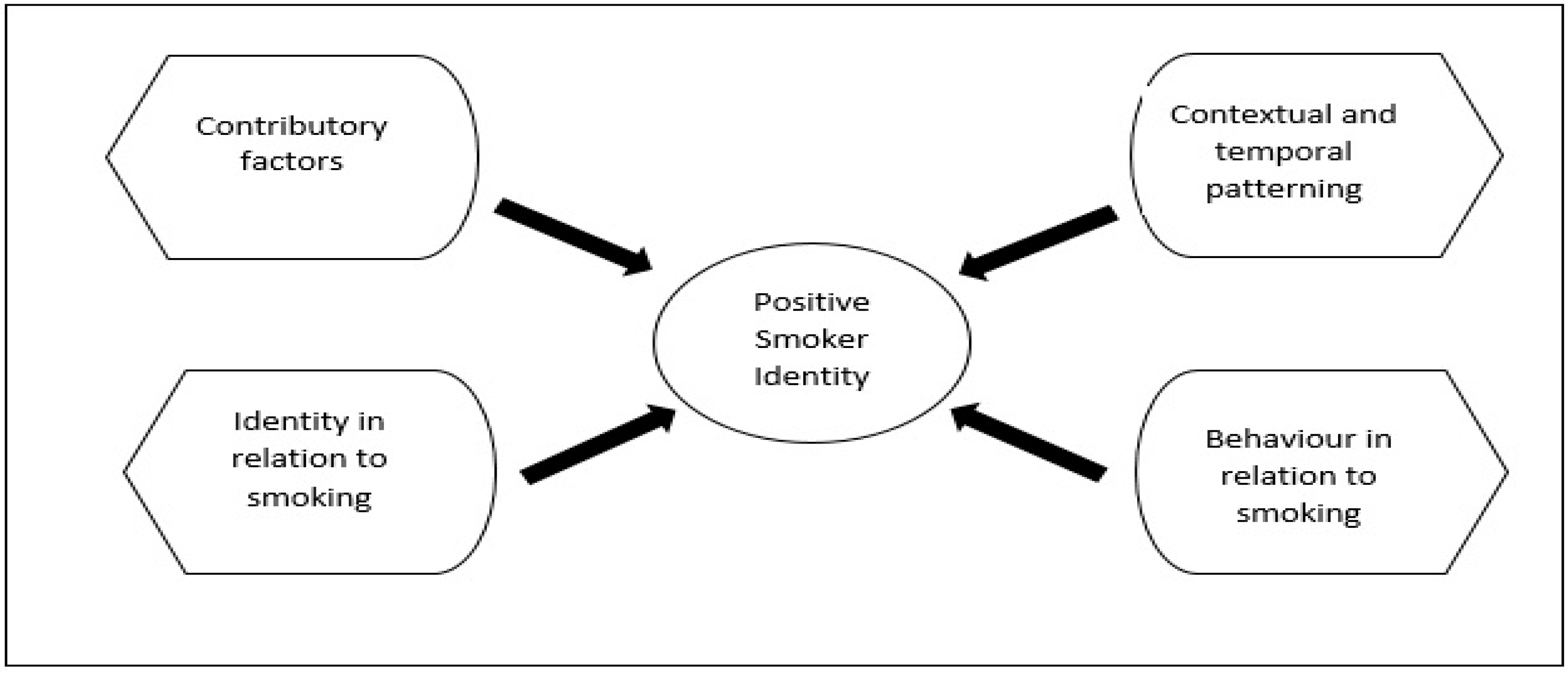
1.3. Smoker Identity Construct
1.4. Research Gap
1.5. Research Goals
1.6. Preliminary Studies and Questionnaire Development
1.7. Face and Content Validation
2. Materials and Methods
2.1. The Participants
2.2. Research Tools
2.3. Data Analysis
2.4. Ethics Approval and Consent to Participate
2.5. Availability of Data and Material
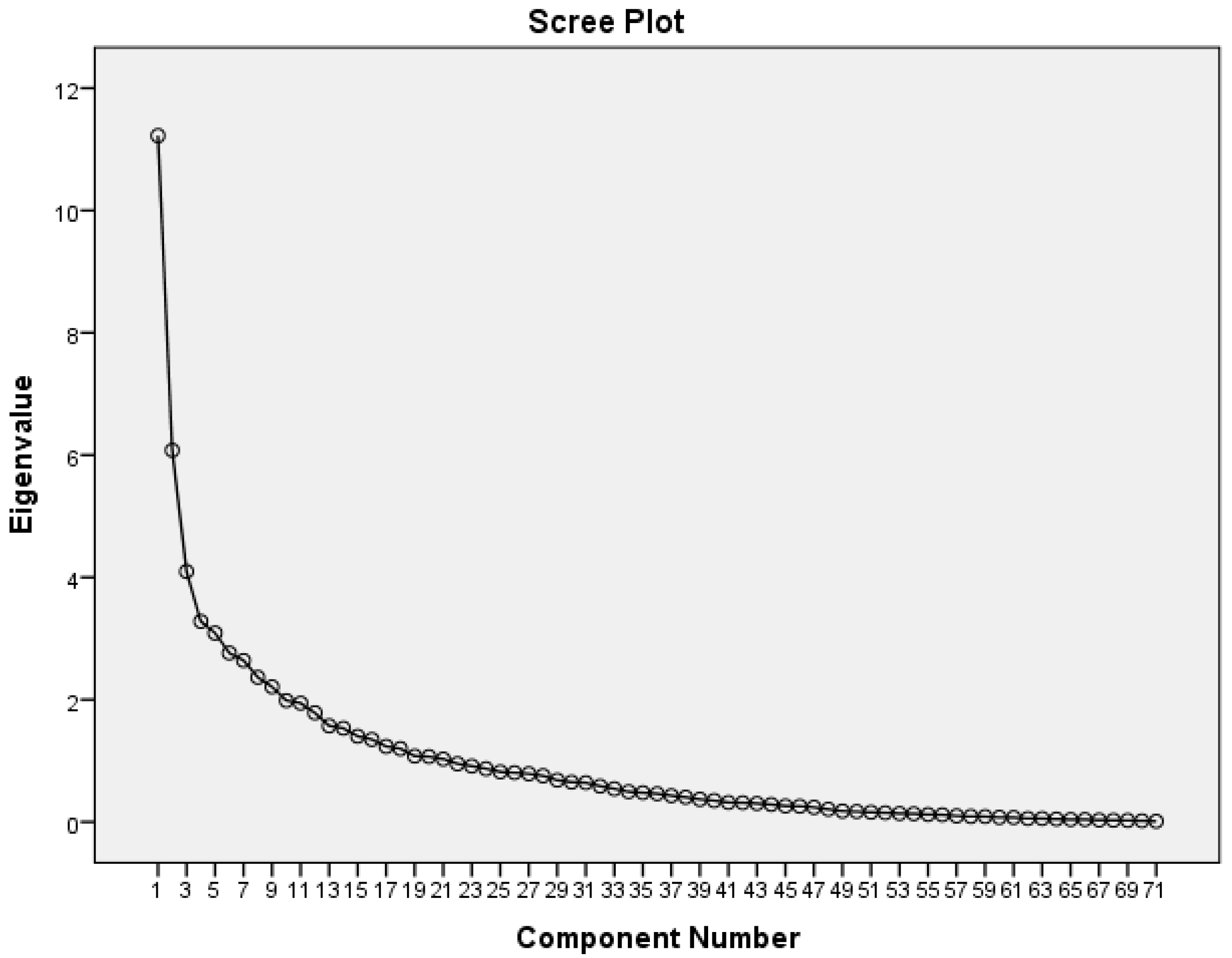
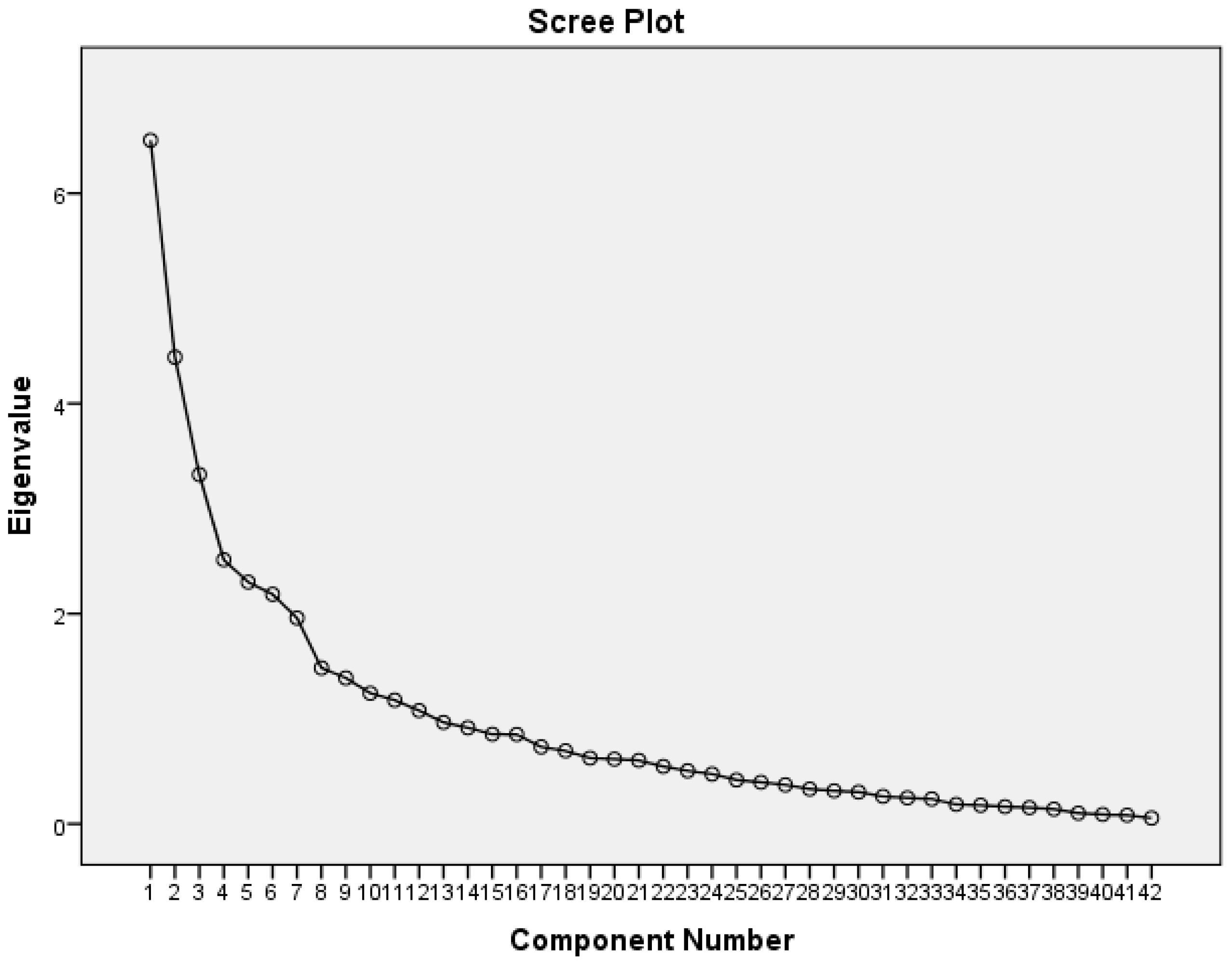
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Riedel, B.W.; Robinson, L.A.; Klesges, R.C.; McLain-Allen, B. What motivates adolescent smokers to make a quit attempt? Drug Alcohol Depend. 2002, 68, 167–174. [Google Scholar] [CrossRef]
- Herzog, T.A.; Abrams, D.B.; Emmons, K.M.; Linnan, L. Predicting increases in readiness to quit smoking: A prospective analysis using the contemplation ladder. Psychol. Health 2000, 15, 369–381. [Google Scholar] [CrossRef]
- Velicer, W.F.; Prochaska, J.O.; Fava, J.L.; Norman, G.J.; Redding, C.A. Smoking cessation and stress management: Applications of the transtheoretical model. Homeostasis 1998, 38, 216–233. [Google Scholar]
- Fava, J.L.; Velicer, W.F.; Prochaska, J.O. Applying the transtheoretical model to a representative sample of smokers. Addict. Behav. 1995, 20, 189–203. [Google Scholar] [CrossRef]
- Bandura, A. Health promotion by social cognitive means. Health Educ. Behav. 2004, 31, 143–164. [Google Scholar] [CrossRef] [PubMed]
- Armitage, C.J.; Conner, M. Social cognition models and health behaviour: A structured review. Psychol. Health 2000, 15, 173–189. [Google Scholar] [CrossRef]
- Greening, L. Adolescents’ Cognitive Appraisals of Cigarette Smoking: An Application of the Protection Motivation Theory1. J. Appl. Soc. Psychol. 1997, 27, 1972–1985. [Google Scholar] [CrossRef]
- Pechmann, C.; Zhao, G.; Goldberg, M.E.; Reibling, E.T. What to convey in antismoking advertisements for adolescents: The use of protection motivation theory to identify effective message themes. J. Mark. 2003, 67, 1–18. [Google Scholar] [CrossRef]
- Sharifi-rad, G.; Hazavei, M.M.; Hasan-zadeh, A.; Danesh-amouz, A. The effect of health education based on health belief model on preventive actions of smoking in grade one, middle school students. Arak Med. Univ. J. 2007, 10, 79–86. [Google Scholar]
- Norman, P.; Conner, M.; Bell, R. The theory of planned behavior and smoking cessation. Health Psychol. 1999, 18, 89–94. [Google Scholar] [CrossRef] [PubMed]
- Higgins, A.; Conner, M. Understanding adolescent smoking: The role of the Theory of Planned Behaviour and implementation intentions. Psychol. Health Med. 2003, 8, 173–186. [Google Scholar] [CrossRef]
- Wen, M.; Van Duker, H.; Olson, L.M. Social contexts of regular smoking in adolescence: Towards a multidimensional ecological model. J. Adolesc. 2009, 32, 671–692. [Google Scholar] [CrossRef] [PubMed]
- Riemsma, R.P.; Pattenden, J.; Bridle, C.; Sowden, A.J.; Mather, L.; Watt, I.S.; Walker, A. Systematic review of the effectiveness of stage based interventions to promote smoking cessation. BMJ 2003, 326, 1175–1177. [Google Scholar] [CrossRef] [PubMed]
- Milne, S.; Sheeran, P.; Orbell, S. Prediction and intervention in health-related behavior: A meta-analytic review of protection motivation theory. J. Appl. Soc. Psychol. 2000, 30, 106–143. [Google Scholar] [CrossRef]
- Carpenter, C.J. A meta-analysis of the effectiveness of health belief model variables in predicting behavior. Health Commun. 2010, 25, 661–669. [Google Scholar] [CrossRef] [PubMed]
- Armitage, C.J.; Conner, M. Efficacy of the theory of planned behaviour: A meta-analytic review. Br. J. Soc. Psychol. 2001, 40, 471–499. [Google Scholar] [CrossRef] [PubMed]
- Sutton, S. Back to the drawing board? A review of applications of the transtheoretical model to substance use. Addiction 2001, 96, 175–186. [Google Scholar] [CrossRef]
- Galvin, K.T. A critical review of the health belief model in relation to cigarette smoking behaviour. J. Clin. Nurs. 1992, 1, 13–18. [Google Scholar] [CrossRef]
- Ajzen, I.; Fishbein, M. Questions raised by a reasoned action approach: Comment on Ogden (2003). Health Psychol. 2004, 23, 431–434. [Google Scholar] [CrossRef]
- Ajzen, I. The theory of planned behaviour: Reactions and reflections. Psychol. Health 2011, 26, 1113–1127. [Google Scholar] [CrossRef]
- West, R. The PRIME Theory of motivation as a possible foundation for addiction treatment. In Drug Addiction Treatment in the 21st Century: Science and Policy Issues; John’s Hopkins University Press: Baltimore, MD, USA, 2007. [Google Scholar]
- Vangeli, E.; West, R. Transition towards a ‘non-smoker’ identity following smoking cessation: An interpretative phenomenological analysis. Br. J. Health Psychol. 2012, 17, 171–184. [Google Scholar] [CrossRef] [PubMed]
- Johnson, J.L.; Lovato, C.Y.; Maggi, S.; Ratner, P.A.; Shoveller, J.; Baillie, L.; Kalaw, C. Smoking and adolescence: Narratives of identity. Res. Nurs. Health 2003, 26, 387–397. [Google Scholar] [CrossRef] [PubMed]
- Brown, A.E.; Carpenter, M.J.; Sutfin, E.L. Occasional smoking in college: Who, what, when and why? Addict. Behav. 2011, 36, 1199–1204. [Google Scholar] [CrossRef] [PubMed]
- Hoek, J.; Maubach, N.; Stevenson, R.; Gendall, P.; Edwards, R. Social smokers’ management of conflicted identities. Tob. Control 2013, 22, 261–265. [Google Scholar] [CrossRef] [PubMed]
- Thompson, L.; Pearce, J.; Barnett, R. Nomadic identities and socio-spatial competence: Making sense of post-smoking selves. Soc. Cult. Geogr. 2009, 10, 565–581. [Google Scholar] [CrossRef]
- Berg, C.J.; Lust, K.A.; Sanem, J.R.; Kirch, M.A.; Rudie, M.; Ehlinger, E.; Ahluwalia, J.S.; An, L.C. Smoker self-identification versus recent smoking among college students. Am. J. Prev. Med. 2009, 36, 333–336. [Google Scholar] [CrossRef] [PubMed]
- Choi, Y.; Choi, S.M.; Rifon, N. “I smoke but I am not a smoker”: Phantom smokers and the discrepancy between self-identity and behavior. J. Am. Coll. Health 2010, 59, 117–125. [Google Scholar] [CrossRef] [PubMed]
- Levinson, A.H.; Campo, S.; Gascoigne, J.; Jolly, O.; Zakharyan, A.; Tran, Z.V. Smoking, but not smokers: Identity among college students who smoke cigarettes. Nicotine Tob. Res. Off. J. Soc. Res. Nicotine Tob. 2007, 9, 845–852. [Google Scholar] [CrossRef] [PubMed]
- Ridner, S.L.; Walker, K.L.; Hart, J.L.; Myers, J.A. Smoking identities and behavior: Evidence of discrepancies, issues for measurement and intervention. West. J. Nurs. Res. 2010, 32, 434–446. [Google Scholar] [CrossRef]
- Hertel, A.W.; Mermelstein, R.J. Smoker Identity and Smoking Escalation among Adolescents. Health Psychol. Off. J. Div. Health Psychol. Am. Psychol. Assoc. 2012, 31, 467–475. [Google Scholar] [CrossRef]
- Falomir, J.M.; Invernizzi, F. The role of social influence and smoker identity in resistance to smoking cessation. Swiss J. Psychol. 1999, 58, 73–84. [Google Scholar] [CrossRef]
- Freeman, M.A.; Hennessy, E.V.; Marzullo, D.M. Defensive evaluation of antismoking messages among college-age smokers: The role of possible selves. Health Psychol. Off. J. Div. Health Psychol. Am. Psychol. Assoc. 2001, 20, 424–433. [Google Scholar] [CrossRef]
- Van den Putte, B.; Yzer, M.; Willemsen, M.C.; de Bruijn, G.J. The effects of smoking self-identity and quitting self-identity on attempts to quit smoking. Health Psychol. Off. J. Div. Health Psychol. Am. Psychol. Assoc. 2009, 28, 535–544. [Google Scholar] [CrossRef] [PubMed]
- Shadel, W.G.; Mermelstein, R. Individual differences in self-concept among smokers attempting to quit: Validation and predictive utility of measures of the smoker self-concept and abstainer self-concept. Ann. Behav. Med. A Publ. Soc. Behav. Med. 1996, 18, 151–156. [Google Scholar] [CrossRef] [PubMed]
- Tombor, I.; Shahab, L.; Brown, J.; West, R. Positive smoker identity as a barrier to quitting smoking: Findings from a national survey of smokers in England. Drug Alcohol Depend. 2013, 133, 740–745. [Google Scholar] [CrossRef] [PubMed]
- Tombor, I.; Shahab, L.; Herbec, A.; Neale, J.; Michie, S.; West, R. Smoker identity and its potential role in young adults’ smoking behavior: A meta-ethnography. Health Psychol. Off. J. Div. Health Psychol. Am. Psychol. Assoc. 2015, 34, 992–1003. [Google Scholar] [CrossRef]
- Meijer, E.; Vangeli, E.; Gebhardt, W.A.; van Laar, C. Identity processes in smokers who want to quit smoking: A longitudinal interpretative phenomenological analysis. Health 2018. [Google Scholar] [CrossRef]
- Shafie, A.A.; Hassali, M.A.; Rabi, R.; Lee, M.L. Treatment Outcome Assessment of the Pharmacist-Managed Quit Smoking Clinic in Malaysia. J. Smok. Cessat. 2016, 11, 203–210. [Google Scholar] [CrossRef]
- Tombor, I.; Shahab, L.; Brown, J.; Notley, C.; West, R. Does non-smoker identity following quitting predict long-term abstinence? Evidence from a population survey in England. Addict. Behav. 2015, 45, 99–103. [Google Scholar] [CrossRef]
- Amy, L.C.; Michael, S.B.; Diana, W.S. Identifying barriers to entering smoking cessation treatment among socioeconomically disadvantaged smokers. J. Smok. Ceesation 2010, 5, 164–171. [Google Scholar]
- MacCallum, R.C.; Widaman, K.F.; Preacher, K.J.; Hong, S. Sample Size in Factor Analysis: The Role of Model Error. Multivar. Behav. Res. 2001, 36, 611–637. [Google Scholar] [CrossRef] [PubMed]
- Heatherton, T.F.; Kozlowski, L.T.; Frecker, R.C.; Fagerstrom, K.O. The Fagerstrom Test for Nicotine Dependence: A revision of the Fagerstrom Tolerance Questionnaire. Br. J. Addict. 1991, 86, 1119–1127. [Google Scholar] [CrossRef] [PubMed]
- HA, A.Y.; Ng, C.G.; Rusdi, A.R. Validation of the Malay version of Fagerstrom test for nicotine dependence (FTND-M) among a group of male staffs in a University Hospital. Malays. J. Psychiatry 2011, 20, 1–7. [Google Scholar]
- Teo, E.W.; Lee, Y.Y.; Khoo, S.; Morris, T. Translation and validation of the Malay version of Shiffman-Jarvik withdrawal scale and cessation self-efficacy questionnaire: A review of psychometric properties. Health Qual. Life Outcomes 2015, 13, 45. [Google Scholar] [CrossRef] [PubMed]
- Kaiser, H.F. An index of factorial simplicity. Psychometrika 1974, 39, 31–36. [Google Scholar] [CrossRef]
- Tabachnick, B.G.; Fidell, L.S. Using Multivariate Statistics, 5th ed.; Allyn & Bacon, Inc.: Boston, MA, USA, 2006. [Google Scholar]
- Sekaran, U.; Bougie, R. Research Methods for Business: A Skill Building Approach, 5th ed.; John Wiley & Sons: Hoboken, NJ, USA, 2009. [Google Scholar]
- Porter, S.R.; Whitcomb, M.E.; Weitzer, W.H. Multiple surveys of students and survey fatigue. New Dir. Inst. Res. 2004, 2004, 63–73. [Google Scholar] [CrossRef]
- Streiner, D.L. Figuring out factors: The use and misuse of factor analysis. Can. J. Psychiatry 1994, 39, 135–140. [Google Scholar] [CrossRef] [PubMed]
- Netemeyer, R.; Bearden, W.; Sharma, S. Scaling Procedures. Issues and Applications; Sage Publications: Thousand Oaks, CA, USA, 2003. [Google Scholar]
- Zhou, X.; Nonnemaker, J.; Sherrill, B.; Gilsenan, A.W.; Coste, F.; West, R. Attempts to quit smoking and relapse: Factors associated with success or failure from the ATTEMPT cohort study. Addict. Behav. 2009, 34, 365–373. [Google Scholar] [CrossRef] [PubMed]
- Vangeli, E.; Stapleton, J.; Smit, E.S.; Borland, R.; West, R. Predictors of attempts to stop smoking and their success in adult general population samples: A systematic review. Addiction 2011, 106, 2110–2121. [Google Scholar] [CrossRef] [PubMed]
- Morrell, H.E.R.; Skarbek, E.A.; Cohen, L.M. The relationship between self-efficacy and nicotine withdrawal severity among adult smokers. Addict. Res. Theory 2011, 19, 494–503. [Google Scholar] [CrossRef]
- Schnoll, R.A.; Martinez, E.; Tatum, K.L.; Glass, M.; Bernath, A.; Ferris, D.; Reynolds, P. Increased self-efficacy to quit and perceived control over withdrawal symptoms predict smoking cessation following nicotine dependence treatment. Addict. Behav. 2011, 36, 144–147. [Google Scholar] [CrossRef] [PubMed]
- Song, A.V.; Ling, P.M. Social Smoking Among Young Adults: Investigation of Intentions and Attempts to Quit. Am. J. Public Health 2011, 101, 1291–1296. [Google Scholar] [CrossRef] [PubMed]
- Kadir Abu Bakar, A.; Aiman Abd Ghani, A.; Bakar Rahman, A.; Zainuddin, A.A.; Nadzri Jai, A.; Chandran, A.; Razali, A.; Baharudin, A.; Rosman, A.; Mahadir Naidu, B.; et al. National Health and Morbidity Survey 2015-VOLUME II: Non-Communicable Diseases, Risk Factors & Other Health Problems; Ministry of Health Malaysia: Putrajaya, Malaysia, 2015. [Google Scholar]
| Studies | Population | Smoker Identity Construct | Question(s) Used |
|---|---|---|---|
| Berg et al., (2009) Minnesota, USA [27] | College students | Yes or No | Do you consider yourself a smoker? |
| Choi et al., (2010) Michigan, USA [28] | University students | Yes or No | Do you consider yourself a smoker? |
| Levinson et al., (2007) Denver, USA [29] | College students | Yes or No | Do you consider yourself a smoker? |
| Ridner et al., (2010) Kentucky, USA [30] | College students | Single item response choices. | Which of the following best describes you? (non-smoker, smoker, occasional smoker, and social smoker. |
| Hertel and Mermelstein, (2012) Chicago, USA [31] | High school students | Two continuous Likert-scale items and a categorical scale item. | 1. How much is being a smoker part of who you are? (1 = not at all, to 4 = a lot). 2. How important are cigarettes in your life? (1 = not at all important, to 5 = the most important) 3. Which of the following best describes how you think about yourself? (1 = smoker, 2 = social smoker, occasional smoker, 3 = ex-smoker, 4 = someone who tried smoking, 5 = non-smoker). |
| Falomir and Invernizzi, (1999) Spain [32] | Secondary school students | Three response scale items. (1 = a little, to 7 = a lot) | 1. To what extent do you feel you are a real smoker? 2. To what extent do your friends see you as a real smoker? |
| Shadel and Mermelstein, (1996) Chicago, USA [35] | Clinic-based smoking cessation programme adult clients | Five-item Smoker Self-Concept Scale (1 = strongly disagree, to 7 = strongly agree) | 1. Smoking is part of my self-image. 2. Smoking is part of "who I am." 3. Smoking is a part of my personality. 4. Smoking is a large part of my daily life. 5. Others view smoking as part of my personality |
| Tombor et al., (2013) UK [36] | National adult survey | Yes or No | I like being a smoker |
| Tombor et al., (2015) UK [37] | Adult household survey | Yes or No | I still think of myself as a smoker |
| Meijer et al., (2018) Netherlands [38] | Longitudinal survey | 2 items (1 = strongly agree to 5 = strongly disagree) | Two items for smokers and ex-smokers: “to [continue smoking/start smoking again] would fit with who you are” and “to [continue smoking/start smoking again] would fit with how you want to live” |
| No. | Items |
|---|---|
| 1. | Merokok membuatkan seseorang itu kelihatan lebih sasa (Smoking makes a person looking more sturdy) |
| 2. | Merokok membuatkan seseorang itu kelihatan lebih seksi (Smoking makes a person look sexier) |
| 3. | Merokok membuatkan seseorang itu kelihatan lebih menggoda (Smoking makes a person look more sexually attractive) |
| 4. | Merokok dapat membantu saya membuat apa sahaja yang saya mahu (Smoking can help me do whatever I want) |
| Variable | N (%) |
|---|---|
| Mean Age (SD) | 38 (9.21) |
| Sex | |
| Men | 100 (100) |
| Women | 0 (0) |
| Ethnicity | |
| Malay | 100 (100) |
| Others | 0 (0) |
| Education level | |
| Primary school or lower | 1 (1) |
| Secondary school | 53 (53) |
| Certificate or Diploma Level | 43 (43) |
| Bachelor Degree | 2 (2) |
| Master or higher | 1 (1) |
| Marriage Status | |
| Single | 10 (10) |
| Married | 89 (89) |
| Widower | 1 (1) |
| Income (Ringgit Malaysia;RM) median, (interquartile range) | RM2000 (1500) |
| Variable | N (%) |
|---|---|
| Smoker type | |
| Daily | 77 (77) |
| Occasional | 23 (23) |
| Tobacco products consumed | |
| Conventional cigarette | 95 (95) |
| Vape | 12 (12) |
| Shisha | 4 (4) |
| Pipe | 1 (1) |
| E-cig | 1 (1) |
| Others | 1 (1) |
| Mean age start smoking (SD) | 18 (3.78) |
| Mean age start smoking regularly | 21 (3.53) |
| Frequency of smoking | |
| Daily | 92 (92) |
| Once a week | 6 (6) |
| Once a month | 1 (1) |
| Less frequent than once a month | 1 (1) |
| No. of cigarette per day | |
| 1 or less | 5 (5) |
| 2 to 5 | 26 (26) |
| 6 to 10 | 31 (31) |
| 11 to 20 | 25 (25) |
| More than 20 | 13 (13) |
| Place of smoking | |
| Home | 69 (69) |
| Workplace | 22 (22) |
| Friend’s house | 29 (29) |
| Food café | 61 (61) |
| Public place | 20 (20) |
| Social gathering | 21 (21) |
| Others | 11 (11) |
| Mean Number of cessation trial in the last 1 year (SD) | 1.6 (2.07) |
| Median number of days stop in the last trial (interquartile range) | 3 (7) |
| Methods of smoking cessation trial | |
| Never stop | 30 (30) |
| Willpower | 54 (54) |
| Over-the-counter medications | 5 (5) |
| Advice of friends | 5 (5) |
| Health counselling | 6 (6) |
| Professional NRT | 2 (2) |
| Others | 4 (4) |
| Exposure to smoking cessation campaign | |
| Always | 45 (45) |
| Occasional | 51 (51) |
| Never | 4 (4) |
| Median cost of smoking in Ringgit Malaysia (RM) per month (interquartile range) | RM120 (130) |
| Usage of cheaper than market price cigarette | |
| All of them (100%) | 36 (36) |
| Most of them (70% to 99%) | 20 (20) |
| Occasionally (30% to 69%) | 21 (21) |
| Rarely (1% to 29%) | 8 (8) |
| Never | 15 (15) |
| Component | Factor 1 | Factor 2 | Factor 3 | Factor 4 | Factor 5 | Factor 6 | Factor 7 |
|---|---|---|---|---|---|---|---|
| Factor 1 | 1.00 | −0.06 | 0.14 | 0.16 | 0.07 | −0.14 | −0.02 |
| Factor 2 | −0.06 | 1.00 | 0.09 | −0.01 | 0.10 | 0.15 | 0.06 |
| Factor 3 | 0.14 | 0.09 | 1.00 | 0.04 | 0.06 | −0.09 | 0.01 |
| Factor 4 | 0.16 | −0.01 | 0.04 | 1.00 | −0.02 | −0.09 | −0.09 |
| Factor 5 | 0.07 | 0.10 | 0.06 | −0.02 | 1.00 | 0.04 | 0.00 |
| Factor 6 | −0.14 | 0.15 | −0.09 | −0.09 | 0.04 | 1.00 | 0.03 |
| Factor 7 | −0.02 | 0.06 | 0.01 | −0.09 | 0.00 | 0.03 | 1.00 |
| Item-Total Statistics | |||||
|---|---|---|---|---|---|
| Item | Scale Mean If Item Deleted | Scale Variance If Item Deleted | Corrected Item-Total Correlation | Squared Multiple Correlation | Cronbach’s Alpha If Item Deleted |
| A1a | 46.76 | 166.992 | 0.544 | 0.488 | 0.928 |
| A1b | 46.34 | 162.732 | 0.660 | 0.677 | 0.926 |
| A1c | 46.66 | 162.833 | 0.722 | 0.685 | 0.925 |
| A1d | 46.31 | 161.105 | 0.716 | 0.639 | 0.925 |
| A1f | 45.71 | 162.895 | 0.586 | 0.583 | 0.928 |
| A1g | 46.45 | 162.088 | 0.744 | 0.684 | 0.925 |
| A1i | 45.98 | 161.495 | 0.617 | 0.657 | 0.927 |
| A1j | 46.08 | 158.781 | 0.736 | 0.719 | 0.924 |
| A2 | 46.08 | 162.377 | 0.721 | 0.667 | 0.925 |
| A3 | 46.01 | 163.485 | 0.622 | 0.589 | 0.927 |
| A4 | 46.15 | 165.199 | 0.598 | 0.520 | 0.927 |
| A5 | 46.19 | 163.489 | 0.642 | 0.568 | 0.926 |
| A6 | 46.29 | 161.925 | 0.684 | 0.575 | 0.926 |
| A7 | 46.33 | 164.749 | 0.572 | 0.512 | 0.928 |
| A10 | 45.32 | 169.371 | 0.459 | 0.390 | 0.930 |
| A11 | 46.38 | 165.733 | 0.564 | 0.486 | 0.928 |
| A12 | 46.47 | 168.231 | 0.501 | 0.624 | 0.929 |
| A13 | 46.49 | 169.222 | 0.418 | 0.615 | 0.931 |
| A14 | 46.58 | 163.438 | 0.685 | 0.636 | 0.926 |
| Item-Total Statistics | |||||
|---|---|---|---|---|---|
| Item | Scale Mean If Item Deleted | Scale Variance If Item Deleted | Corrected Item-Total Correlation | Squared Multiple Correlation | Cronbach’s Alpha If Item Deleted |
| A8 | 38.79 | 51.602 | 0.602 | 0.688 | 0.806 |
| A9 | 38.72 | 51.072 | 0.587 | 0.720 | 0.806 |
| B3 | 38.38 | 51.309 | 0.538 | 0.464 | 0.811 |
| B5 | 38.93 | 50.894 | 0.519 | 0.304 | 0.813 |
| B6 | 38.52 | 52.111 | 0.577 | 0.373 | 0.808 |
| B7 | 39.07 | 54.187 | 0.467 | 0.357 | 0.817 |
| B9 | 39.02 | 53.535 | 0.454 | 0.583 | 0.819 |
| B10 | 38.93 | 53.116 | 0.499 | 0.610 | 0.815 |
| B12 | 38.64 | 53.041 | 0.508 | 0.414 | 0.814 |
| B14 | 38.86 | 54.970 | 0.395 | 0.335 | 0.823 |
| B18 | 39.04 | 54.685 | 0.360 | 0.300 | 0.827 |
| Component | Factor 1 | Factor 2 | Factor 3 | Factor 4 | Factor 5 | Factor 6 | Factor 7 |
|---|---|---|---|---|---|---|---|
| Factor 1 | 1.000 | −0.087 | 0.072 | 0.056 | 0.032 | 0.037 | −0.188 |
| Factor 2 | −0.087 | 1.000 | 0.089 | 0.017 | −0.011 | 0.168 | 0.132 |
| Factor 3 | 0.072 | 0.089 | 1.000 | −0.041 | −0.027 | 0.090 | −0.122 |
| Factor 4 | 0.056 | 0.017 | −0.041 | 1.000 | 0.000 | 0.002 | −0.049 |
| Factor 5 | 0.032 | −0.011 | −0.027 | 0.000 | 1.000 | −0.018 | −0.031 |
| Factor 6 | 0.037 | 0.168 | 0.090 | 0.002 | −0.018 | 1.000 | −0.017 |
| Factor 7 | −0.188 | 0.132 | −0.122 | −0.049 | −0.031 | −0.017 | 1.000 |
| Rotated Component Matrix a | Item-Total Correlation b | |||||||
|---|---|---|---|---|---|---|---|---|
| Item | Factors and Loading | |||||||
| Contributory Factors | Contextual and Temporal Patterning | Identity Related to Smoking | Factor 4 | Factor 5 | Factor 6 | Behaviour in Relation to Smoking | ||
| A1b | 0.737 | 0.689 | ||||||
| A1c | 0.792 | 0.760 | ||||||
| A1d | 0.775 | 0.690 | ||||||
| A1g | 0.823 | 0.753 | ||||||
| A1j | 0.789 | 0.701 | ||||||
| A2 | 0.707 | 0.652 | ||||||
| A6 | 0.721 | 0.655 | ||||||
| A14 | 0.697 | 0.658 | ||||||
| A8 | 0.797 | 0.660 | ||||||
| A9 | 0.790 | 0.661 | ||||||
| B3 | 0.655 | 0.528 | ||||||
| B5 | 0.645 | 0.509 | ||||||
| B6 | 0.664 | 0.563 | ||||||
| B7 | 0.484 | 0.414 | ||||||
| B10 | 0.458 | 0.402 | ||||||
| B12 | 0.610 | 0.476 | ||||||
| B8 | - | |||||||
| B17 | 0.632 | 0.246 | ||||||
| B22 | 0.741 | 0.155 | ||||||
| B23 | 0.692 | 0.343 | ||||||
| C10 | −0.507 | −0.275 | ||||||
| D13 | −0.534 | 0.444 | −0.228 | |||||
| B1 | - | |||||||
| B4 | 0.610 | 0.453 | ||||||
| B13 | 0.505 | 0.356 | ||||||
| C1 | 0.648 | 0.541 | ||||||
| C6 | 0.411 | 0.408 | ||||||
| D7 | - | |||||||
| D8 | 0.653 | 0.417 | ||||||
| D9 | 0.705 | 0.541 | ||||||
| C5 | -0.571 | −0.430 | ||||||
| D3 | 0.697 | −0.005 | ||||||
| D12 | 0.699 | 0.053 | ||||||
| C2 | 0.522 | 0.372 | ||||||
| C3 | 0.688 | 0.508 | ||||||
| C4 | 0.713 | 0.485 | ||||||
| C13 | 0.602 | 0.292 | ||||||
| B11 | −0.580 | −0.042 | ||||||
| B20 | −0.477 | 0.053 | ||||||
| D5 | 0.535 | 0.241 | ||||||
| D10 | 0.692 | 0.006 | ||||||
| D11 | 0.547 | 0.280 | ||||||
| Factors | Coefficient of Reliability (Cronbach’s Alpha) |
|---|---|
| Contributory factors | 0.90 |
| Contextual and temporal patterning | 0.81 |
| Identity related to smoking | 0.72 |
| Behaviour in relation to smoking | 0.65 |
| Factor 4 | 0.05 |
| Factor 5 | −0.45 |
| Factor 6 | 0.22 |
| Scales | Total PSmoQi Scores | Factor 1 | Factor 2 | Factor 3 | Factor 7 | Sector E | FTND | CSEQ | SSCS | No. of Quit Attempt |
|---|---|---|---|---|---|---|---|---|---|---|
| Total PSmoQi Scores | 1 | |||||||||
| Factor 1 | 0.683 ** | 1 | ||||||||
| Factor 2 | −0.642 ** | −0.055 | 1 | |||||||
| Factor 3 | −0.393 ** | 0.037 | 0.114 | 1 | ||||||
| Factor 7 | 0.268 ** | 0.127 | 0.149 | −0.193 | 1 | |||||
| Sector E | −0.119 | −0.132 | −0.106 | 0.238 * | −0.127 | 1 | ||||
| FTND | 0.169 | 0.077 | −0.051 | −0.239 * | 0.078 | −0.160 | 1 | |||
| CSEQ | −0.188 | −0.276 ** | −0.001 | 0.076 | 0.044 | 0.248 * | −0.327 ** | 1 | ||
| SSCS | 0.516 ** | 0.545 ** | −0.257 ** | −0.009 | 0.057 | −0.258 ** | 0.242 * | −0.375 ** | 1 | |
| No. of quit attempt | −0.040 | −0.070 | −0.078 | 0.131 | −0.013 | 0.235 * | −0.085 | 0.147 | −0.158 | 1 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ahmad, M.H.; Ibrahim, M.I.; Ab Rahman, A.; Musa, K.I.; Mohd Zin, F.; Mohd Zain, R.; Hasan, R.; Hassan, N.; Ahmad, I.; Idris, N.S. Development and Validation of Positive Smoker Identity Questionnaire (PSmoQi): A New Instrument for Smoking Cessation Correlates. Int. J. Environ. Res. Public Health 2019, 16, 351. https://doi.org/10.3390/ijerph16030351
Ahmad MH, Ibrahim MI, Ab Rahman A, Musa KI, Mohd Zin F, Mohd Zain R, Hasan R, Hassan N, Ahmad I, Idris NS. Development and Validation of Positive Smoker Identity Questionnaire (PSmoQi): A New Instrument for Smoking Cessation Correlates. International Journal of Environmental Research and Public Health. 2019; 16(3):351. https://doi.org/10.3390/ijerph16030351
Chicago/Turabian StyleAhmad, Mohd Hanief, Mohd Ismail Ibrahim, Azriani Ab Rahman, Kamarul Imran Musa, Faridah Mohd Zin, Rehanah Mohd Zain, Ruhaya Hasan, Noraryana Hassan, Imran Ahmad, and Nur Suhaila Idris. 2019. "Development and Validation of Positive Smoker Identity Questionnaire (PSmoQi): A New Instrument for Smoking Cessation Correlates" International Journal of Environmental Research and Public Health 16, no. 3: 351. https://doi.org/10.3390/ijerph16030351
APA StyleAhmad, M. H., Ibrahim, M. I., Ab Rahman, A., Musa, K. I., Mohd Zin, F., Mohd Zain, R., Hasan, R., Hassan, N., Ahmad, I., & Idris, N. S. (2019). Development and Validation of Positive Smoker Identity Questionnaire (PSmoQi): A New Instrument for Smoking Cessation Correlates. International Journal of Environmental Research and Public Health, 16(3), 351. https://doi.org/10.3390/ijerph16030351







