1. Introduction
There is a significant number of tennis players in the world, taking into consideration both the professionals and those who play for leisure. Tennis can be played on a variety of surfaces, such as a hard court (acrylic), clay, grass, and artificial grass. As it is a sport that is played at a high intensity there is a great propensity for injuries. A tennis athlete should have excellent physical preparation, because there is no fixed time to finish the game. Tennis athletes are susceptible to a range of injuries including conditions caused by chronic overuse and acute traumatic injuries [
1]. Disorders of the musculoskeletal system can appear, such as tennis elbow, shoulder injuries, stress fractures, and muscle strains, which cause health problems [
2]. Ferrara and Cohen [
3] wrote that the repetitive impact and abuse of the upper extremities in racquet sports can increase the risk of tissue fatigue and injury, because during the impact between the racket and the ball the muscles are used the most. According to Chadefaux et al. [
4], the racket has an important role in the athlete’s performance, and also in the prevention of pathologies and discomfort. Hennig [
5] did a study to evaluate the influence of the racket on injuries in tennis athletes, and concluded that one of the causes for developing tennis elbow is the number of vibrations transmitted to the arm by the hand, due to the impact between the racket and the ball. Baszczyński et al. [
6] evaluated the spring tension and mass of a tennis racket and determined that higher spring tension causes more vibration, but if a mass was added to the racket the amplitude of vibrations is reduced, because this mass acts as a shock absorber that helps to dissipate kinetic energy. According to many authors, the most common injury observed in tennis athletes occurs in the elbow. Kachanathu et al. [
7] saw that the most acute injuries occurred in the body joints, such as in the elbows, followed by wrists, ankles, shoulders, and knees. They also observed that lateral epicondylitis (tennis elbow) occurs more frequently in recreational rather than in professional tennis athletes. These injuries may also be associated to the chronic repetitive overload. Chung and Lark [
8] say that an incorrect position of the tennis athlete and his or her level of expertise could have a significant influence on the risk of the occurrence of injuries. Normally the elbow joint is stabilized, but the kinetic chain of the tennis service changes this, and promotes variations, for example, in the feet, knees, shoulder, elbow joint, and hand [
9]. Kovacs and Ellenbecker [
10] did a study using an 8-stage model to evaluate the tennis service. For them, this component of tennis is the most complex stroke among competitive athletes. According to Williams and Hebron [
11] there is no substantial difference between service and groundstrokes in relation to shoulder injuries. However, they say that the upper limbs have been found to account for between 20% and 49% of injuries, with the shoulder and elbow being most frequently injured. During the tennis service there are five phases to be considered: wind-up (knee flexion, trunk rotation), early cocking, late cocking (position of maximal abduction-external rotation), acceleration phase (including long axis rotation), and follow through, which can promote, due to the repetition, an increased risk of overloading various structures around the shoulder [
12]. Allen et al. [
13] say that due to the great consistency of the impact conditions, and the advantage that the athlete has in developing a high-speed overhead service, the biomechanical consistency in serving is higher than the other strokes.
Welcome et al. [
14] say that the hand-arm vibration (HAV) exposure is directly associated to the hand-arm vibration syndrome (HAVS), which is a syndrome that affects the blood vessels, joints, muscles, and nerves of the hand, wrist, and arm. These authors have concluded that the vibration transfer depends on the vibration direction and the measurement location. The HAVS may be developed due to a prolonged and intensive exposure to vibration [
15]. According to López-Alonso et al. [
16] the signs of exposure to HAV may be classified as vascular, neurological, or musculoskeletal. Fridén [
17] says that the exposure to HAV can cause a variety of vascular and neuromuscular symptoms, like tingling in the fingers, discomfort or inflammation in the wrist and hand, digital lightening, intolerance to cold, feebleness of the finger flexors or basic muscles, and discoloration and trophic skin lesions of the fingers. One of the most common injuries in tennis athletes, as mentioned before, is tennis elbow, which can be described as a specific pathological disorder originating from the musculature of the lateral epicondyle, generally caused by overload [
18]. An incorrect technique during the service may be the factor that most frequently causes tennis elbow, which can be reduced if the tennis athlete manages to perform the service using both hands alternatively and not only the predominant hand [
19]. Nevertheless, this seems to be difficult due to the technique employed by tennis athletes during the service.
Nowadays, there are a relatively great number of techniques and studies that include motion capture/analysis, vibration analysis, measurement of human performance, etc. [
20,
21,
22,
23], but there are few studies using infrared thermography (IRT). Nevertheless, the use of the IRT technique to evaluate skin temperature in health and sports is constantly growing, which shows the importance of this technique concerning performance in sports [
24,
25,
26,
27,
28,
29,
30]. IRT makes detection of the heat pattern and blood flow possible by the use of a special camera to measure the temperature of the skin and is a safe and a noninvasive technique. The use of IRT in sports is possible due to the fact that the body temperature is one of the principal indicators used to analyze the health status of a human, which can change during and after the practice of sports. IRT is also used to evaluate the thermal body patterns of healthy adults, in order to understand whether significantly higher differences between the contralateral skin temperatures could indicate serious problems, like hyperthermia or hypothermia, or others [
31]. For some authors the results obtained by using the IRT can provide fundamental information for athletes, sports physiotherapists, coaches, and dieticians. IRT is used to evaluate musculoskeletal disorders during the practice of sports, and can help to prevent injuries, by identifying warning signs before the damage occurs, because the temperature of the affected areas, when compared to other similar ones, normally changes in the case of overuse [
32]. del Estal et al. [
33] use the IRT to evaluate the thermal asymmetries in striking combat athletes, like kickboxing and Muay Thai athletes. These authors selected 18 regions of interest (ROIs) and the asymmetries were analyzed by comparing lead and rear sides. According to Uchôa et al. [
34] the variations observed in the skin surface temperature, using IRT analysis, detected after resistance training may be considered an indicator that the muscles could be inflamed. These authors have confirmed that the skin temperature seems to be an important variable to be considered in sports and can help to prevent injuries in the practice of them.
There are a lot of studies concerning the injuries in tennis athletes. However, according to these authors’ knowledge, no studies have been done to evaluate the HAV, simultaneously with the IRT, to identify the probability of injury in tennis athletes during the service, until now. The aim of this study is to evaluate the HAV and changes in body skin temperature in tennis athletes during the service. The authors intend to contribute to help tennis athletes reduce the risk of injury with their results by identifying the signs of injuries before they occur.
2. Materials and Methods
All participants gave written informed consent prior to participation, according to the Helsinki declaration. This research study applied the calculation method outlined in the International Standard [
35,
36]. Six male volunteers, all tennis athletes, with a mean age of 21 years and an experience of over 10 years, which places them in an elite group, participated in this study (
Table 1).
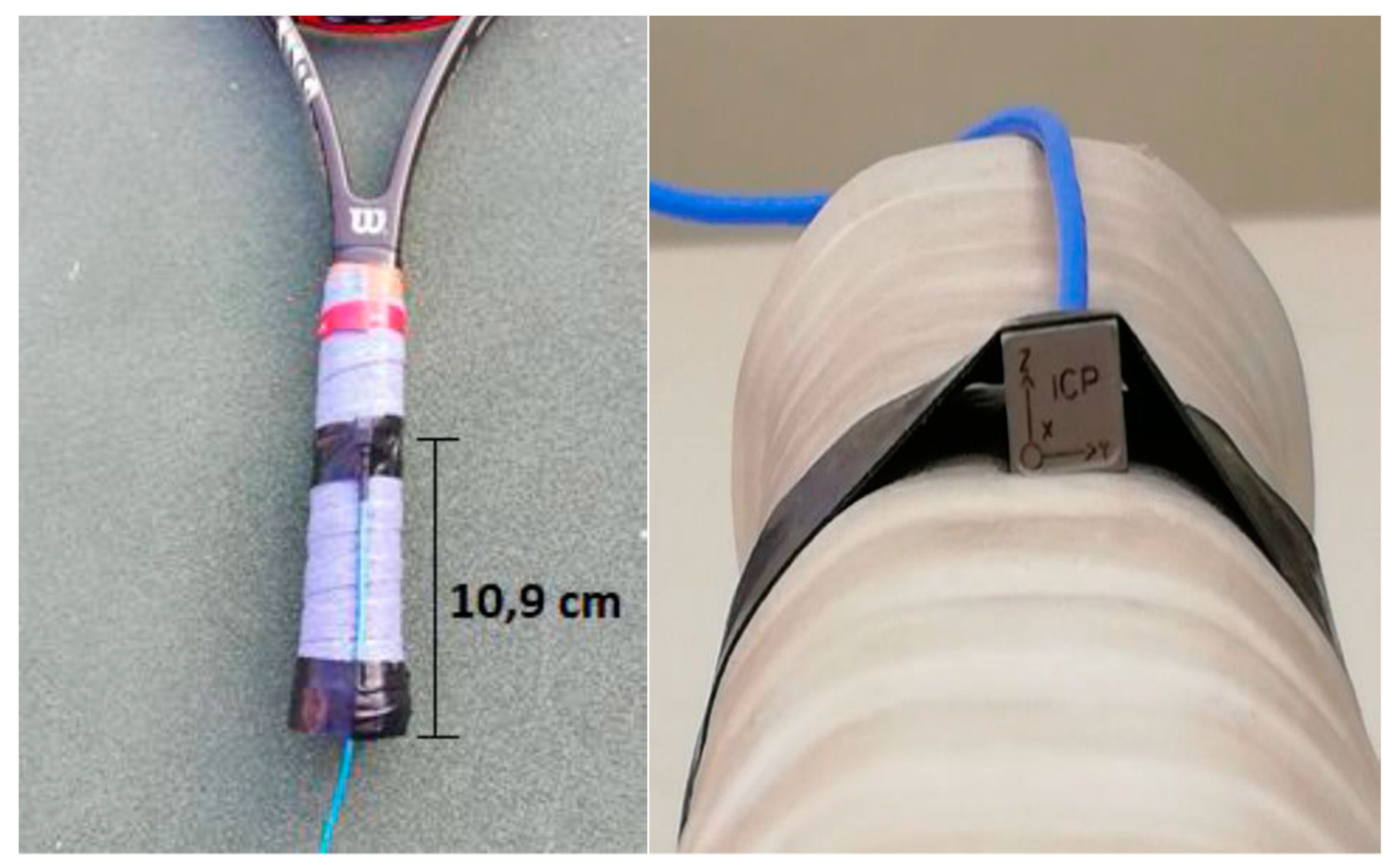
Only one racket, Wilson Pro Staff 97, and one ball type, Wilson US OPEN number 4, were used by all the athletes in all tests. The racket was used under four different conditions, defined by the type of grip used and the use or not of an anti-vibrator as shown in
Figure 1: the over-grip Wilson Pro (with a thickness of 0.6 mm, presents a great traction, which allows a reduction in sliding) and without an anti-vibrator (WGNAV); the over-grip Wilson Pro with an anti-vibrator (WGWAV); the over-grip Tourna (which is considered superfine, with a thickness of 0.45 mm and is normally used when needing to absorb more sweat) and with an anti-vibrator (TGWAV) and an over-grip developed in cork (a combination, made by the authors, combining the Wilson Pro over-grip and 2 mm of cork, with a total thickness of 2.6 mm) with an anti-vibrator (CGWAV). All the volunteers performed at least 10 services under each test condition.
Table 2 presents the randomized order used in this study.
2.1. Hand-Arm Vibration (HAV)
In order to quantify the HAV induced in the athletes, one triaxial accelerometer (ICPR/IEPE Integrated Circuit Piezoelectric) was placed over the grip, at a distance of 10.9 cm from the tip of the over-grip (
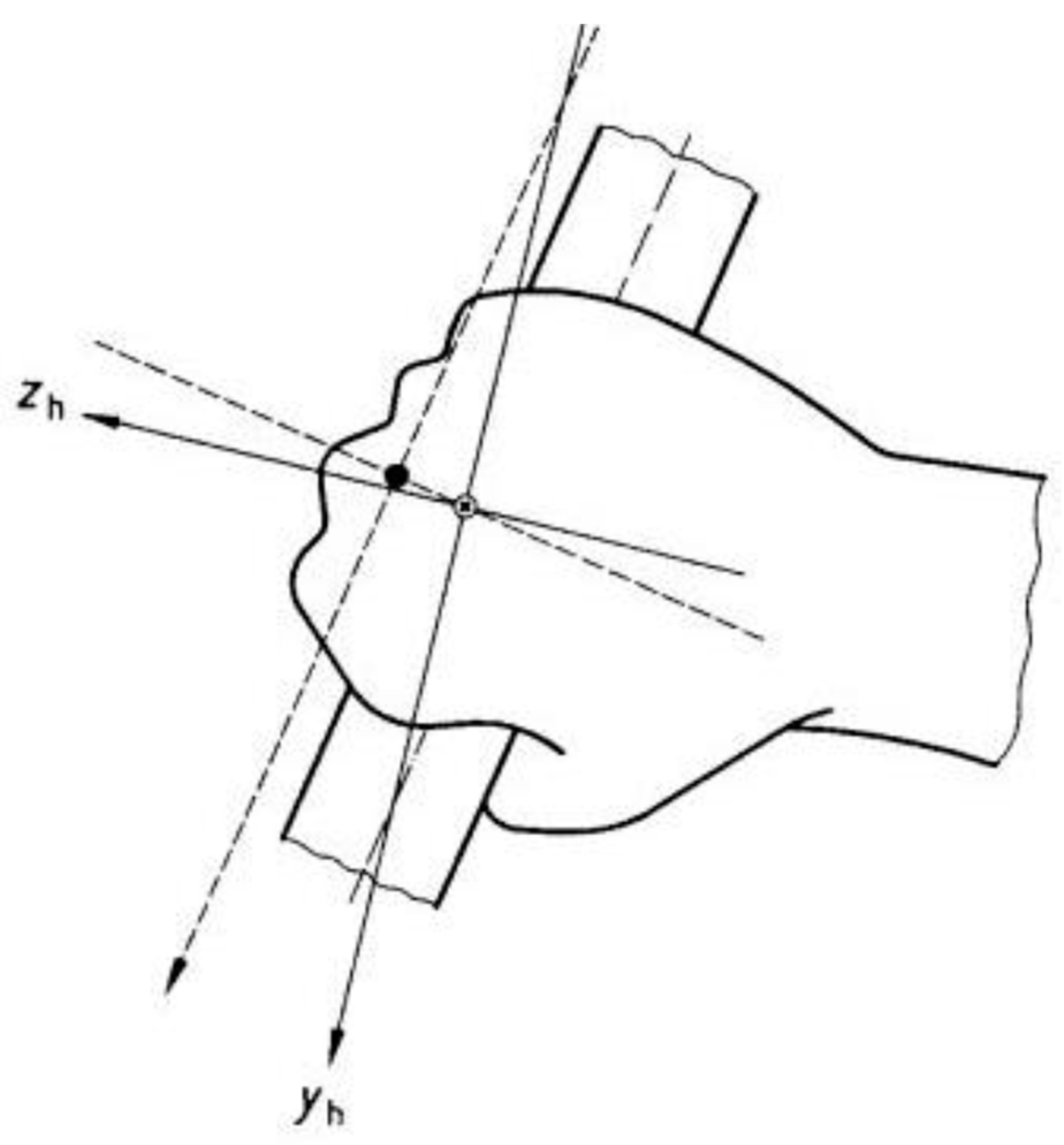
Figure 2). The coordinate system used to acquire HAV data is defined in
Figure 3. The accelerometer channels were aligned with the racket, in such a way that x is the anterior–posterior direction, y is the media–lateral direction, and z is the superior–inferior direction.
The data acquisition system includes an NI 9234 four channel simultaneous sampling IEPE module (National Instruments, Austin, TX, USA) and a wireless NI WLS-9234 chassis connected to a laptop computer equipped with LabVIEW
® software (National Instruments: Austin, TX, USA). The WLS-9234 delivers 102 dB of dynamic range and incorporates software-selectable AC/DC coupling and IEPE signal conditioning for accelerometers and microphones. The four input channels make it possible to digitize simultaneous signals at rates of up to 51.2 kHz per channel and permit built-in antialiasing filters that automatically adjust to the sampling rate. As for the HAV, the frequency range recommended by ISO 5349 is 6.3–1000 Hz and the sampling frequency of the HAV was set at 1000 Hz. The acceleration data was filtered, as specified in the standards, using the SVT Human Vibration tool of LabVIEW (LabView, Manual of NI Sound and Vibration Measurement Suite 6.0, 2007). The filter coefficients were evaluated according to the procedures developed by Rimmel and Mansfield [
37].
In order to quantify the vibration of exposure the authors used the European Directive 2002/44/EC, which defines the following terms for workers related to the HAV:
Hand-arm vibration: when mechanical vibration is transmitted to the hand-arm some risks to the health and safety of the workers appear, like vascular disorders, osteoarticular injuries, and neurological or muscular disorders.
Daily exposure action value (DEA): if the vibration exposure value exceeds 2.5 ms−2 in an 8-h reference period for a vibration dose value, the implementation of a program of technical and/or organizational measures is necessary to reduce the exposure to the mechanical vibration.
Daily exposure limit value (DEL): the vibration exposure value cannot, under any circumstances, exceed the value of 5 ms−2 in an 8-h reference period.
The daily exposure value for an 8-h reference period,
, for the HAV, is defined by:
where the index
i is used to indicate either the
x,
y or
z axes, respectively,
is the weighted root means square acceleration, rms, specified in (ms
−2) in the direction of the three axes,
is the daily duration of exposure to the vibration
, and
is the 8-h reference period (28,800 s).
The rms value of the acceleration over a direction
i is defined as
where
T is the duration of the measurement and
is the weighted acceleration specified in (ms
−2) in the direction of the corresponding three axes. The ISO 5349 standards specify that the total magnitude of the vibration should be determined from the vibration in the
orthogonal coordinates, in the case of HAV, as
It is possible to obtain a relation between the parameter value
and the number of years of exposure,
D:
which enables the vibration exposure limit until there is 10% probability of an individual developing vibration white finger (also denominated Raynaud’s disease).
2.2. Infrared Thermography (IRT)
The IRT was performed using a thermographic camera T430sc (FLIR
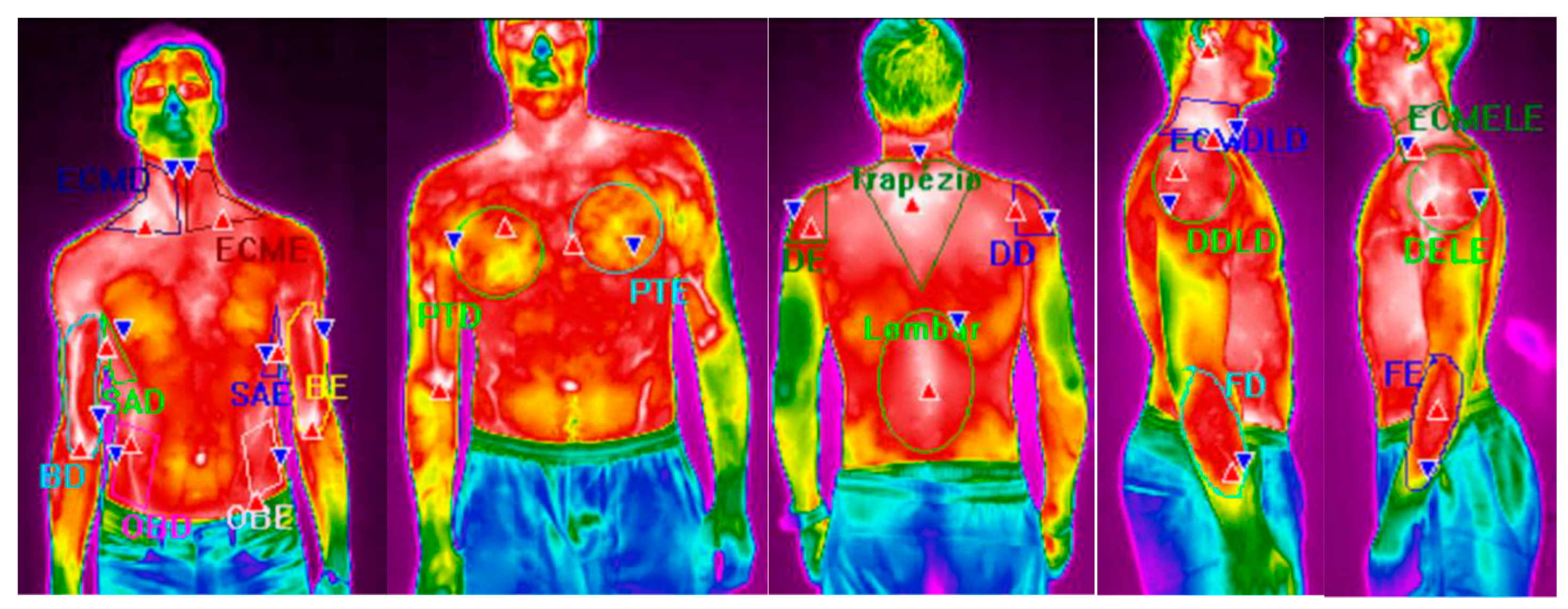
® Systems, Täby, Sweden) 320 × 240 pixels of resolution, spectral range of 7.5–13 μm, image frequency of 60 Hz, accuracy of ±2 °C, and sensitivity <0.030 °C (NETD—Noise Equivalent Temperature Difference). The pictures were taken of the volunteers’ naked trunk. The images were analyzed using the software FLIR ResearchIR Max. Using this software, it was possible to evaluate the maximum, mean, and minimum temperatures over the several ROIs. A total of 20 ROIs (
Figure 4) were analyzed: right biceps (RB), left biceps (LB), right sternocleidomastoid (RS), left sternocleidomastoid (LS), right oblique (RO), left oblique (LO), right pectoral (RP), left pectoral (LP), serratus anterior right (SAR), serratus anterior left (SAL), right deltoid (RD), left deltoid (LD), lumbar (L), trapezius (T), right deltoid lateral perspective (RDR), left deltoid lateral perspective (LDL), right sternocleidomastoid lateral perspective (RSR), left sternocleidomastoid lateral perspective (LSL), right extensor carpi radialis brevis (RECRB), and left extensor carpi radialis brevis (LECRB). Descriptive time intervals of 0.4 s (
Tsk) and the correspondent standard deviation (St.Desv.). Thermal skin variations
were calculated as the difference between the average skin temperature value after the 40 services
and the average skin temperature value at the reference situation, before performing any service,
, according to Equation (5):
All the volunteers were submitted to the same protocol to carry out the tests (
Table 3). The racket used was the Wilson Pro with anti-vibrator. The thermographic camera was placed at a distance of 3 m from each volunteer. Initially, each athlete remained seated in a chair in a comfortable position for a period of 8 min so that the body temperature stabilized. After this several thermographic photographs were taken from four different perspectives: front, rear, right side, and left side. These photographs allowed to obtain the thermal map before the exercise execution, thus corresponding to the athlete’s reference standard. Then the player in the test performed 10 services within 1 min. Next, and during 1 min, the player was again photographed with the camera in the same position. Immediately thereafter, the player repositioned himself to serve another 10 services and was rephotographed again for a period of 1 min and in the same sequence of image acquisition. This procedure was repeated to make a total of 40 services and 20 photos per player. It should be noted that all photos were taken of the bare-chested player in order to be able to assess the skin temperature in the desired areas, due to the fact that the thermal imager can only obtain the skin surface temperatures. A room temperature of 18 °C was measured and kept constant during all the tests. For each volunteer and over-grip considered a total of 40 services and 20 photos were realized, making a total of 960 evaluations and 480 photos.
In order to statistically evaluate the influence of the conditions, a t-test with two samples and unequal variances was applied. If p is less than 0.05 the null hypothesis is rejected, so it is possible to conclude that there is a significant difference between the two samples under analysis.
4. Discussion
This study set out to examine the effect of two different types of over-grip incorporated into the design of a tennis racket frame design and also the presence of one anti-vibrator device. The study was developed not under highly controlled laboratory conditions, but on the tennis court under quasi-realistic playing conditions. Players were allowed to move freely and without constraints on how forcefully they served. Hence, factors like grip position, grip force, or racket velocity and acceleration at ball impact were not fully controlled. Another potential source of variability may arise from removing and then reattaching the accelerometers to the several rackets, although we carefully monitored the accelerometer placement, we cannot guarantee that positions among tests were the same. Despite these limitations, the results provided useful information on the impact and potential benefits of different types of over-grip on the mechanical vibration behavior of rackets when used by tennis players. The infrared thermography was performed using a thermographic camera that offers high scanning speeds, high imaging resolution, and poses no health problems. The first limitation of the IRT technique is the finite depth of penetration, usually confined to 2–3 mm [
39]. Another limitation of this technique is the accuracy of detection of temperature variations on spatial resolution, as well as the reliability varies depending on the analyzed areas [
40]. Nevertheless, this preliminary study, performed on a limited number of subjects, provided the basis upon which a subsequent investigation of skin temperature response compared with the electrical activity of muscles, could attempt to infer an indirect estimation of the physical efficiency and/or the training level of athletes.
From the results present in
Table 4 and
Table 5 it is possible to conclude that the presence of the anti-vibrator reduces the HAV by around 2% to 7% [
41]. The athlete who presents the highest values for the total magnitude of the vibration is athlete 6, who has more experience and is better positioned in terms of ranking. These results can be justified by the fact that the force imposed during the tennis service by this athlete could be greater than that imposed by the remaining athletes. Higher grip forces exerted by tennis players are associated with higher vibration transferred to the player arm [
42]. In fact, athlete 6 is able to produce more power with his legs, due to the movement created by bending his knees, when compared with the others, thus increasing the vibrations induced by the racket. Further, the athlete who presents the lowest value is number 2, the smallest and lightest one, which confirms the last idea. The same tendency is observed in the case of the use of Tourna and Cork in the over-grip. Moreover, it would be expected that, depending on the axis system defined by the position of the accelerometer in the racket, the highest values for effective acceleration would be observed in the direction of ZZ axis. However, in most trials and athletes the highest value occurs in the XX direction, which can be justified by the way each athlete holds the racket, as well as by the movement he makes with his wrist during the service [
42,
43].
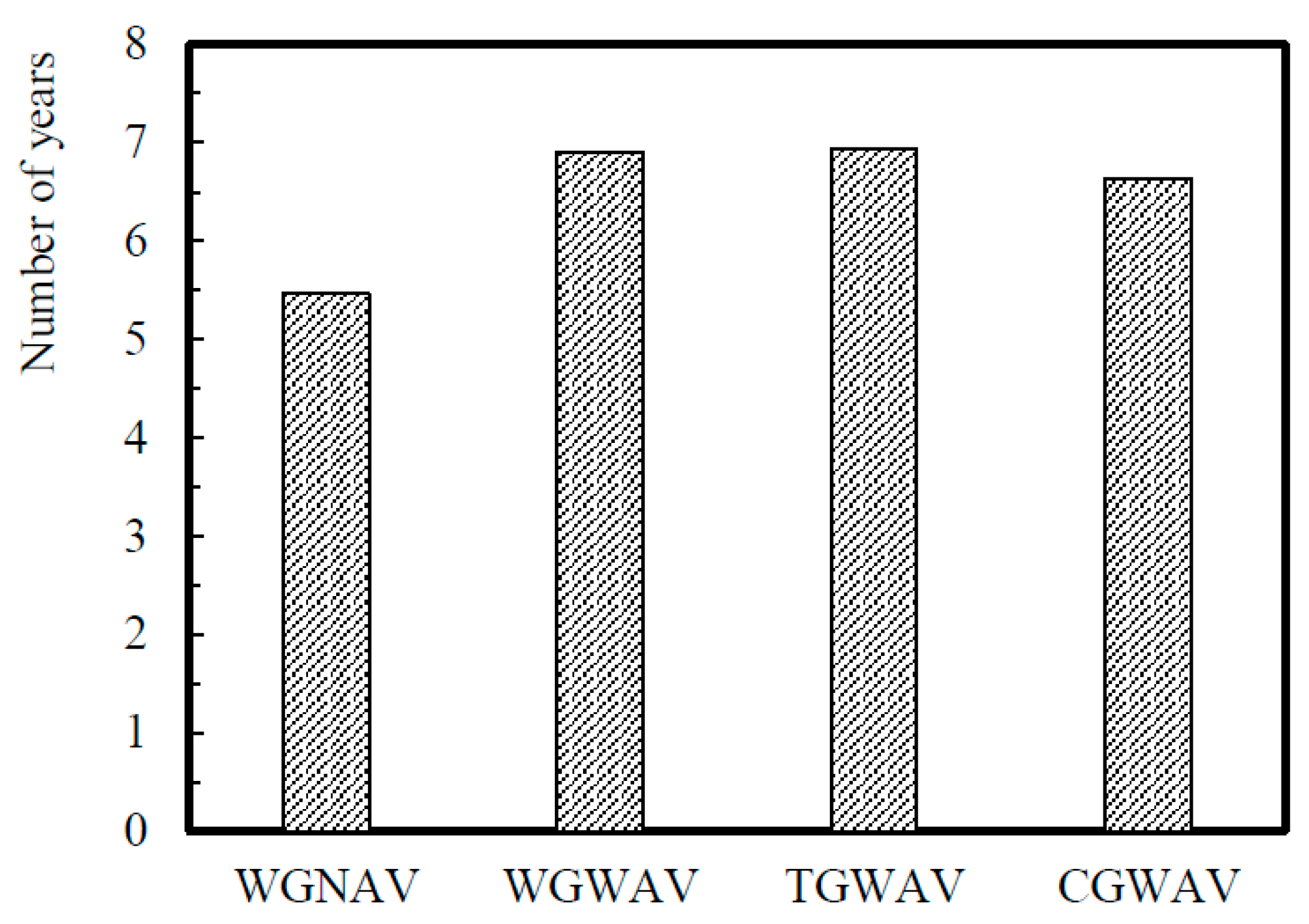
From
Table 4,
Table 5,
Table 6 and
Table 7 it is also possible to conclude that the highest values of HAV are evaluated in the case of the standard Wilson Pro racket (WGNAV) and the lowest for Wilson Pro racket with the anti-vibrator device (WGWAV). Moreover, comparing the variation of HAV values among athletes for each over-grip type, i.e., for each one of the WGNAV and WGWAV conditions, it is possible to see that highest difference appears between athletes 2 and 6, and is about 40% on both over-grip types. The cork over-grip should, theoretically, reduce vibrations due to the material characteristics of cork. However, the HAV values increase by around 6%, which can be explained by the difficulty the athletes had in holding the racket firmly, owing to the greater thickness of this over-grip, which means that the athlete must use greater force to service, which increases the vibrations induced. The Tourna grip, when compared with the standard Wilson Pro, does not present significant differences. According to Marchetti et al. [
44] the access point of vibration is the palm of the hand, so the way the athlete handles the racket has a significant influence on the HAV. The average values for the weighted acceleration specified (a
hv), considering the results of the six athletes and obtained in the four situations evaluated are 42.99 ± 8.4, 41.42 ± 8.2, 41.21 ± 8.5, and 43.01 ± 8.4 m/s
2, for WGNAV, WGWAV, TGWAV, and CGWAV, respectively. The higher values for the standard deviation are justified by the differences observed between the athletes.
Statistical analysis of the results presented through
Table 4,
Table 5,
Table 6 and
Table 7 have shown that the presence of the anti-vibrator and Tourna or Cork over-grips can affect athletes differently: for athlete 1, the presence of cork, when compared to Wilson Pro racket with anti-vibrator, affects the values of RMS in the X and Y directions, with
p values of 0.043 and 0.0296, respectively; for athlete 2, the RMS Y values of the pair Wilson pro racket with and without anti-vibrator show statistically significant differences, with
p equal to 0.017. The presence of cork on the grip has also statistical significance differences in all the values of RMS, when compared to WGWAV; in the case of athletes 3 and 4 no statistically significance differences are obtained (
p > 0.05); for the athletes 5 and 6, the TGWAV changes the HAV values significantly, when compared to the WGWAV, for all the RMS values, with
p values well below 0.05.
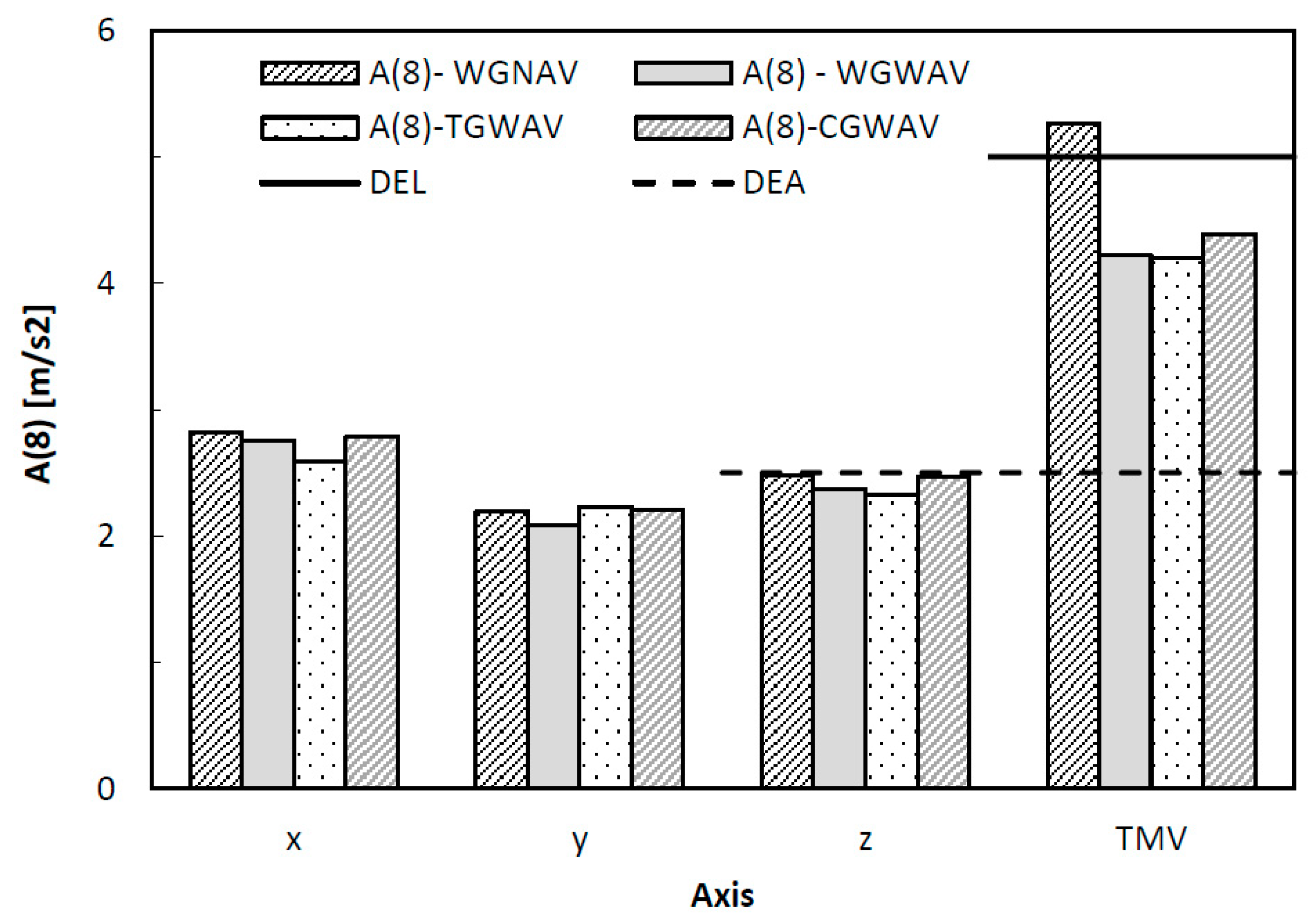
The values of the daily exposure action and the daily exposure limit, presented in
Figure 7, were obtained considering a daily duration of 300 s. It is possible to observe that the HAV values obtained during the service are much bigger when compared with those evaluated by the authors in other studies [
45,
46], which means that the risk of the tennis athletes developing various disorders, like the carpal tunnel syndrome, tingling numbness in the fingers (blood vessels and nerves affected), fingers changing color (blood vessels affected), and loss of manual dexterity (nerves and muscles affected), is higher [
47,
48]. Moreover, the results of
Figure 7 indicate that during the service the tennis athlete may be exposed to health and safety risks, which could be minimized by taking some precautions, for example, using a correct tennis serve technique and an appropriate racket with an adjustable grip. A similar idea was also reported by Ferrara and Cohen [
3]. Therefore, according to these results, the risk is very high when tennis athletes play the serve.
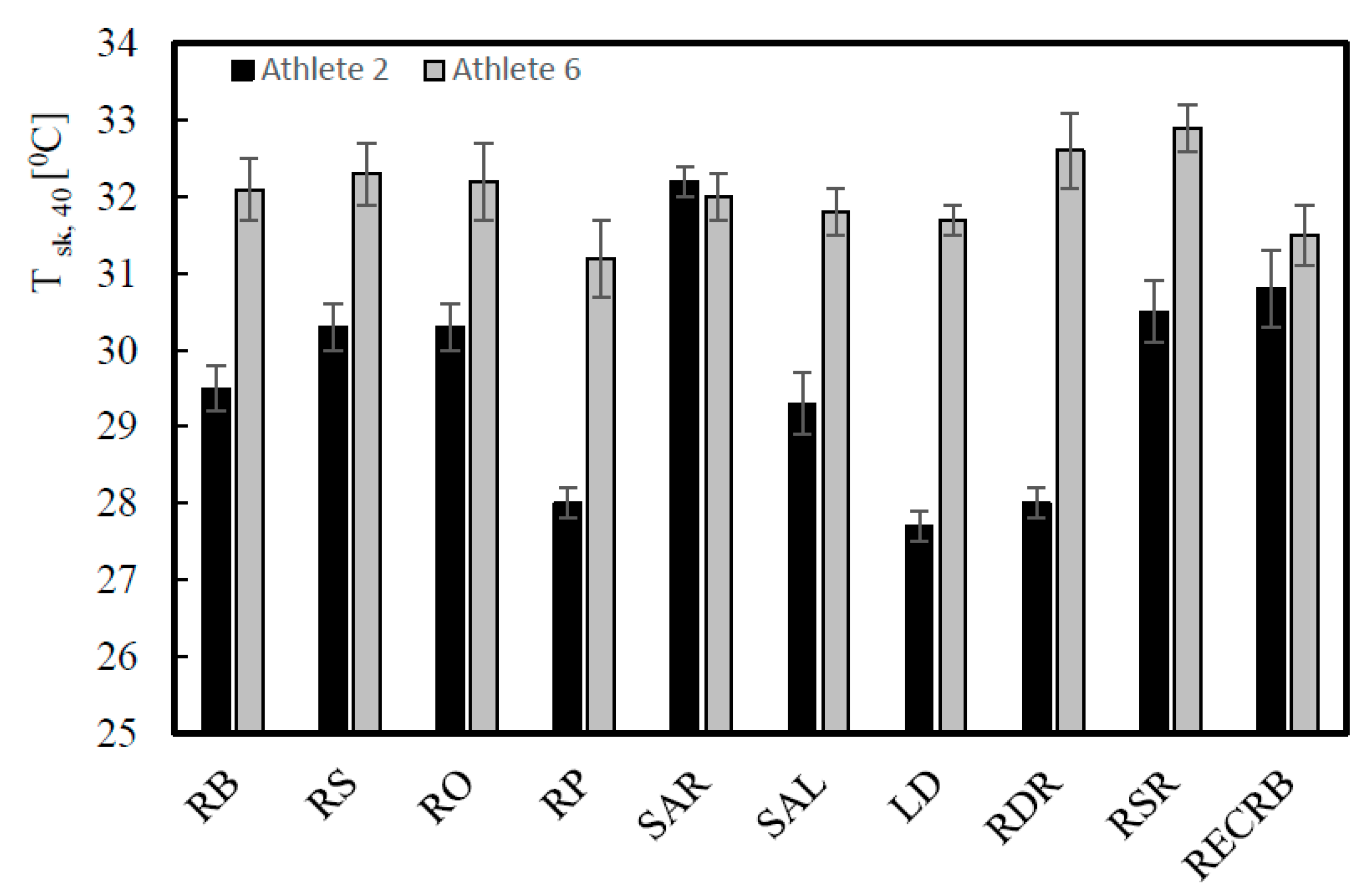
The infrared thermography technology can be used to identify the regions that are more solicited during physical activity and exercise and is one of the most often used indicators of health status in humans [
49]. From the results presented in
Table 8, it may be seen that for almost all the athletes and for all the muscles under analysis, there is a decrease in the skin temperature, which agrees with previous works [
25,
49,
50], and can be explained by the cutaneous vasoconstrictor response to exercise. In fact, the results of
Table 8 show that for some athletes the differences are higher than 0.5 °C and it may require attention. Moreover, from the results of the contralateral skin temperature for the different regions of interest presented in
Table 9, is possible to see that major variances occur in the RECRB/LECRB contralateral ROIs, followed by the RB/LB contralateral regions, with values that are higher than 0.4 °C in four athletes. These observations may justify the frequent appearance of the injury known as tennis elbow. In fact, Hildebrandt et al. [
51] says that a difference of more than 1 °C between contralateral ROIs can indicate a pathophysiological process and Marins et al. [
32] concludes that a difference higher than 1.6 °C for the contralateral ROIs can be considered “High Severity”, in the level of attention, and a difference less than 0.5 °C no special attention is required. Regarding the
p values presented in
Table 9, it can be concluded that
p is smaller than 0.05 for the comparison between RECRB/LECRB, for all the athletes, and for three athletes in the case of RB/LB. Therefore, this means that there is a statistically significant difference between the two contralateral ROIs under analysis, especially the extensor carpi radialis brevis, which confirms the possible appearance of the tennis elbow injury.
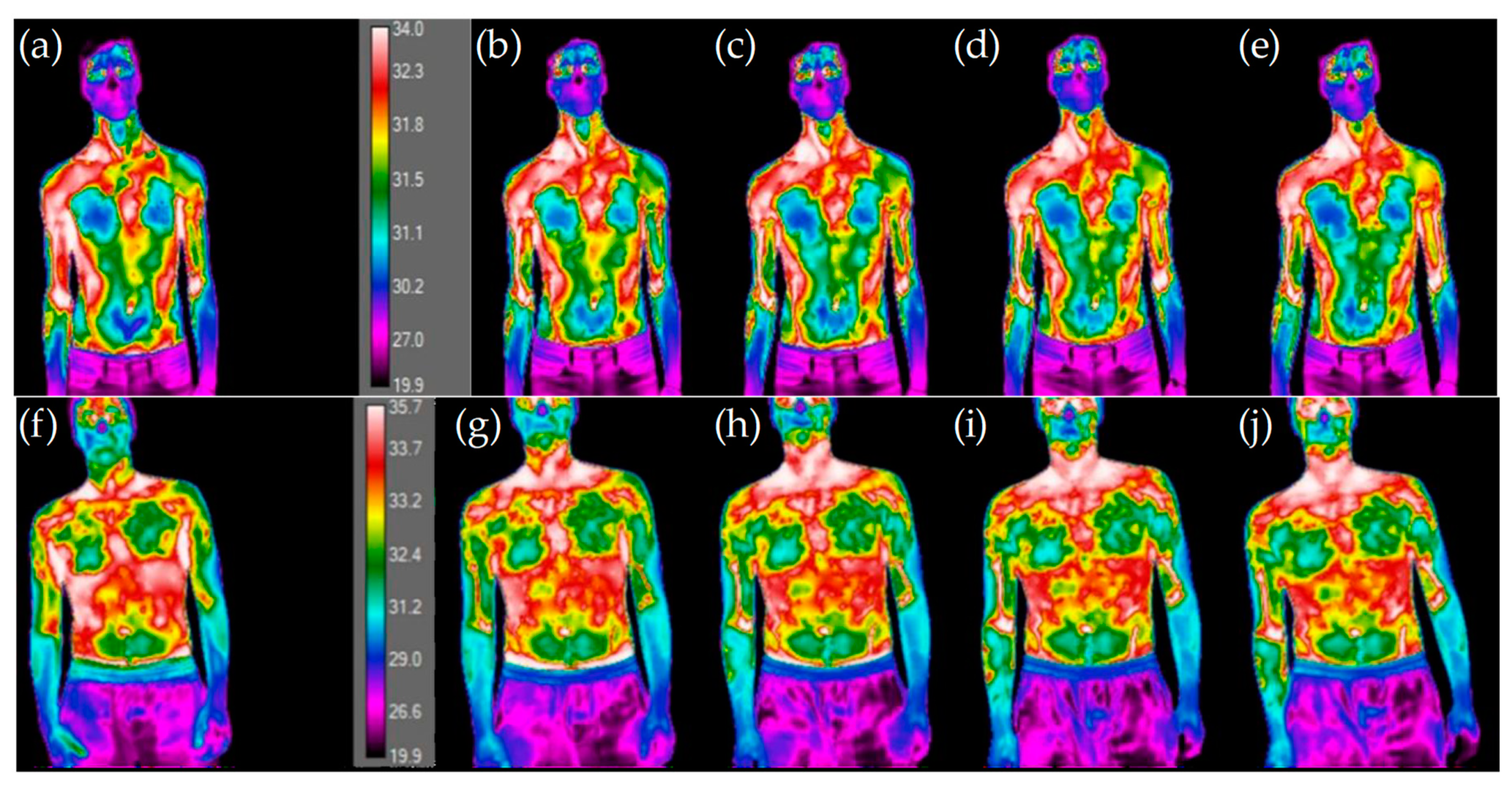
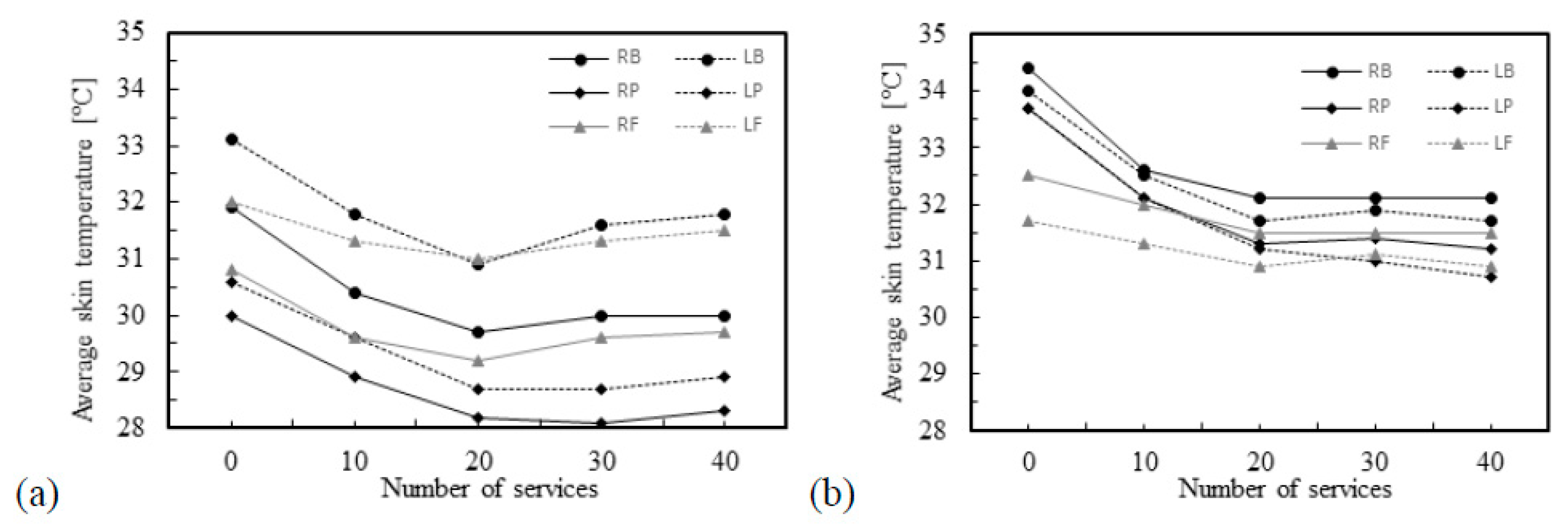
In
Figure 9, it may be observed that with the increase in the number of services the skin temperatures become more uniform and distinguishable. There is a clear distinction between the first thermographic photograph (reference situation) and the later ones (after performing services), the latter are very similar, suggesting a uniform distribution of temperature. For athlete number 3 an increase in the skin temperature values may be seen, while for athlete number 5 a decrease in the skin temperature is detected. In fact,
Figure 10 shows that athlete 3 is the unique athlete who presents an increase in the skin temperature values with the number of services. Nevertheless, the skin temperature values evaluated at the reference condition are in accordance with reported by Webb [
52], despite being lower than the traditional 36 °C, when the room temperature is about 15–18 °C. The differences observed in the reference skin temperature between several athletes can be explained by the anthropometric data. In fact, factors relating to individual and personal characteristics can influence the skin temperature, for example, the body mass index [
32,
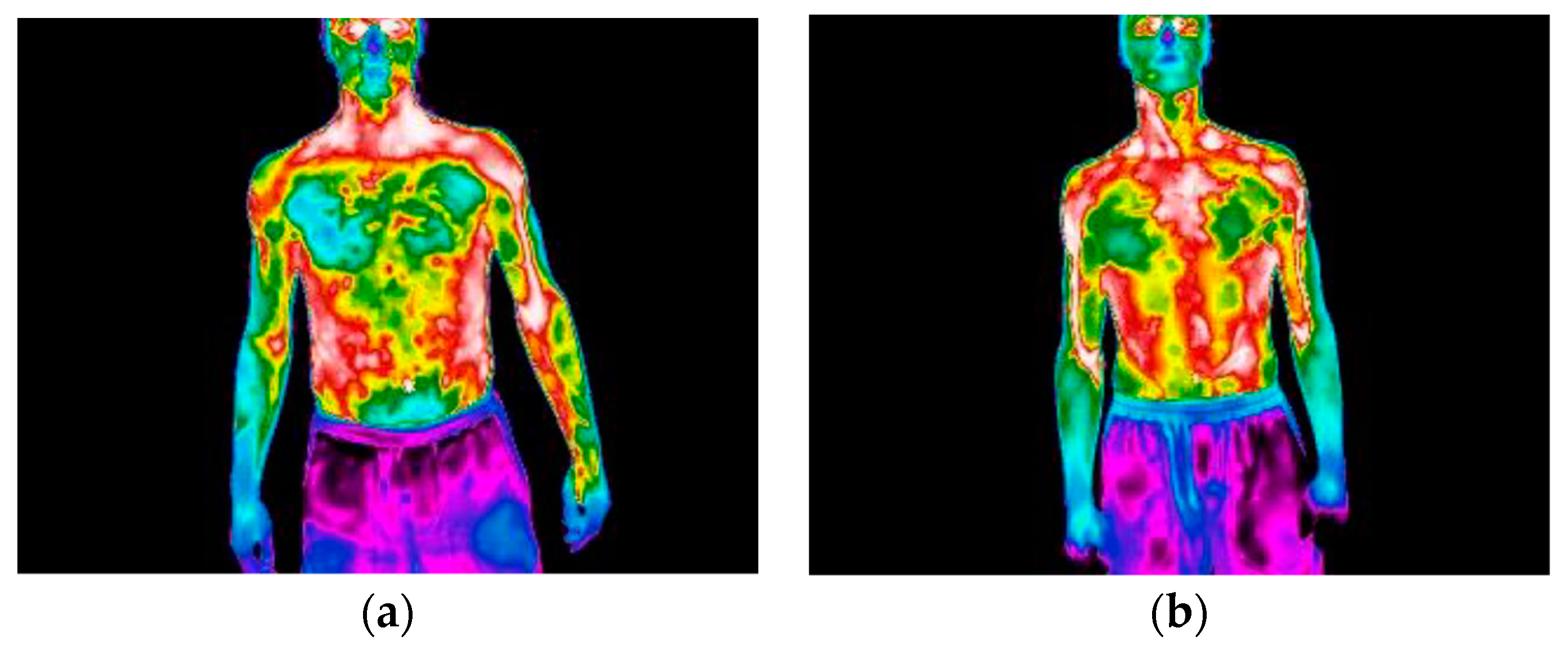
53], and athlete number 3 has the lowest body mass index, which may help to justify the results for this athlete. The infrared thermal images presented in
Figure 11 allows to confirm that independently of the preferred hand used by the athlete to hold rackets, i.e., right-handed or left-handed, the highest arm skin temperature values are detected near the elbow of the arm that holds the racket.