Changes in Attitudes toward Mental Illness in Healthcare Professionals and Students
Abstract
1. Introduction
2. Method
2.1. Search Methods
2.2. Study Selection
2.3. Relevant Measures
2.4. Cross-Temporal Meta-Analysis
3. Results
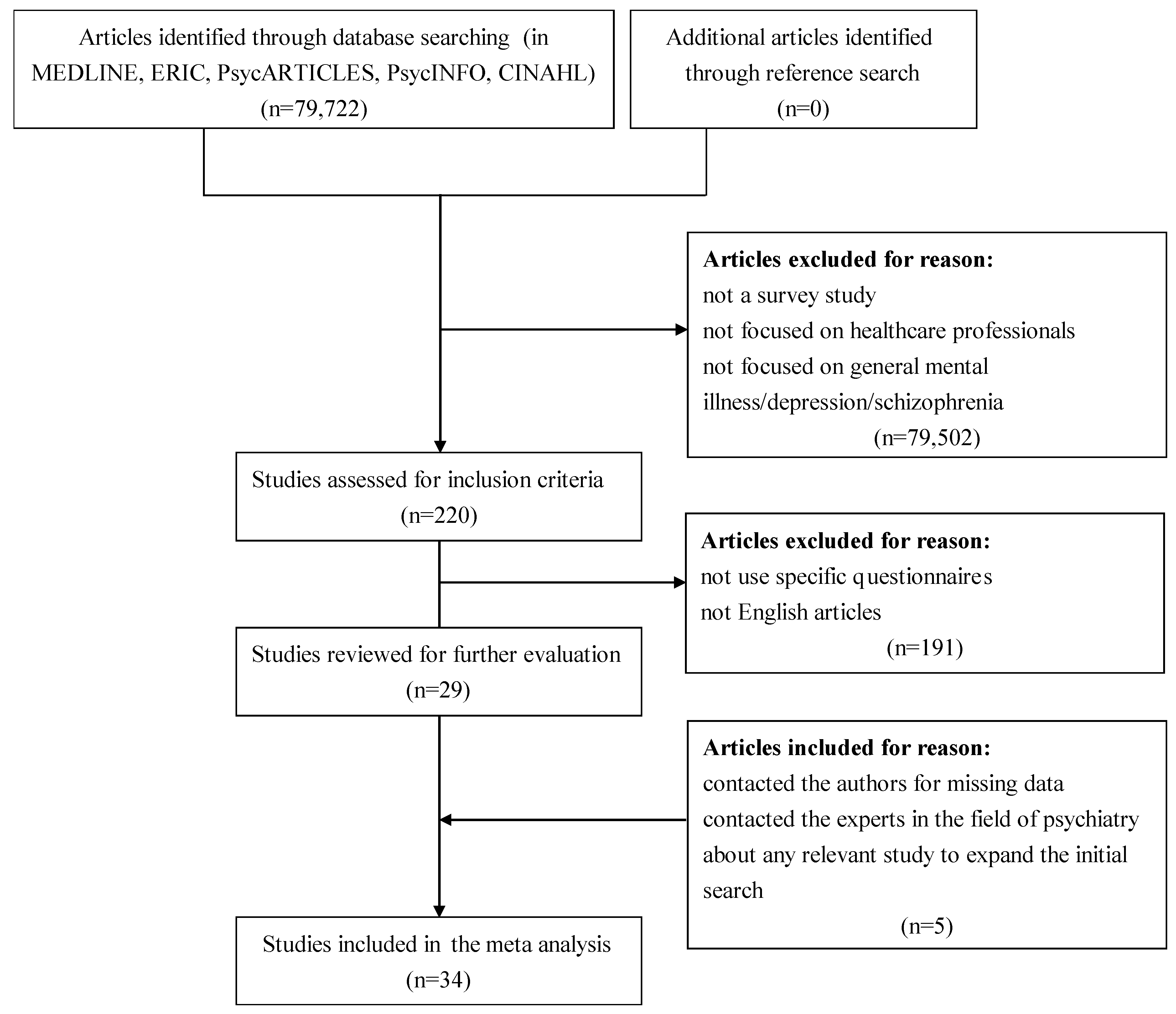
3.1. Data Identification and Extraction
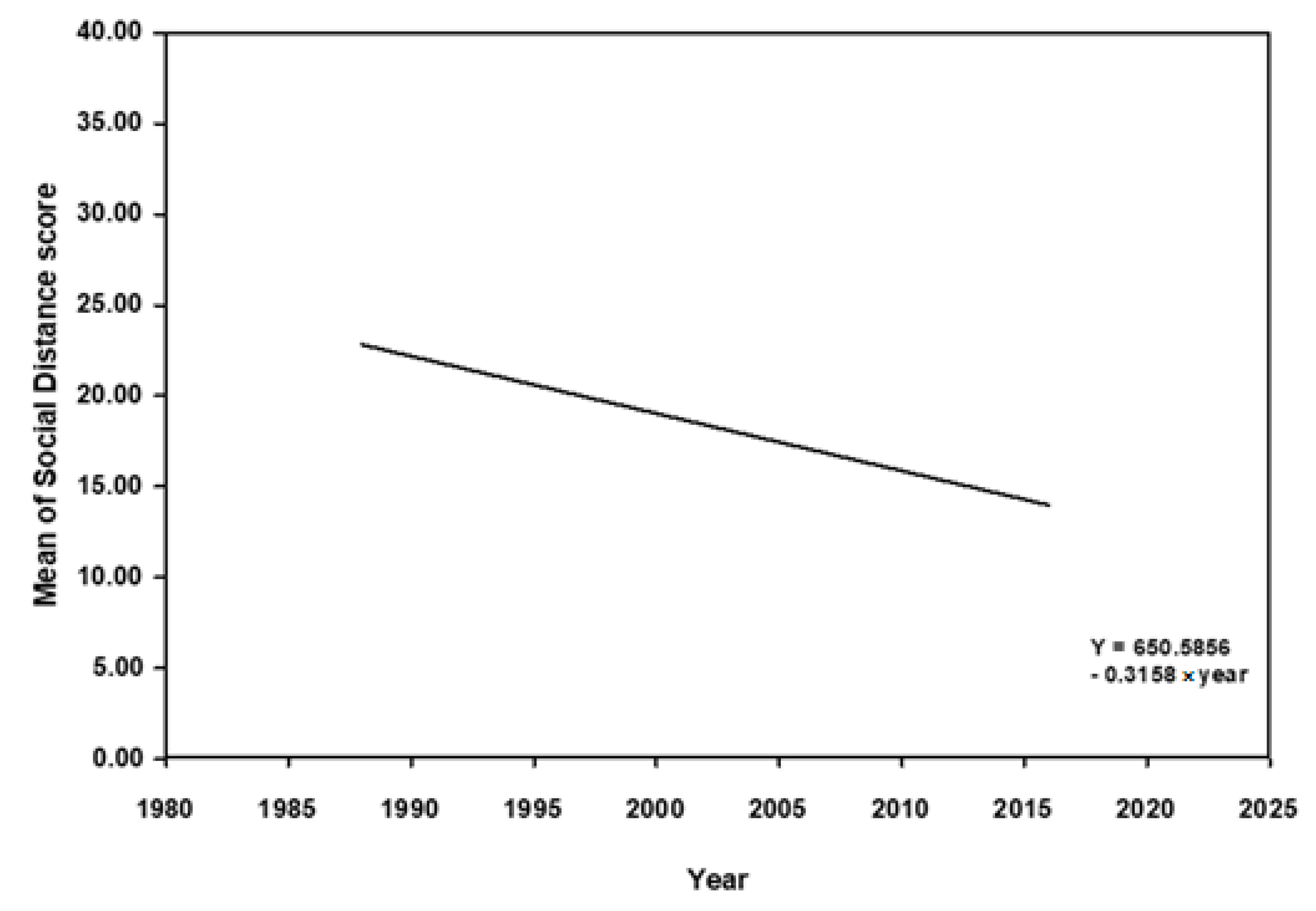
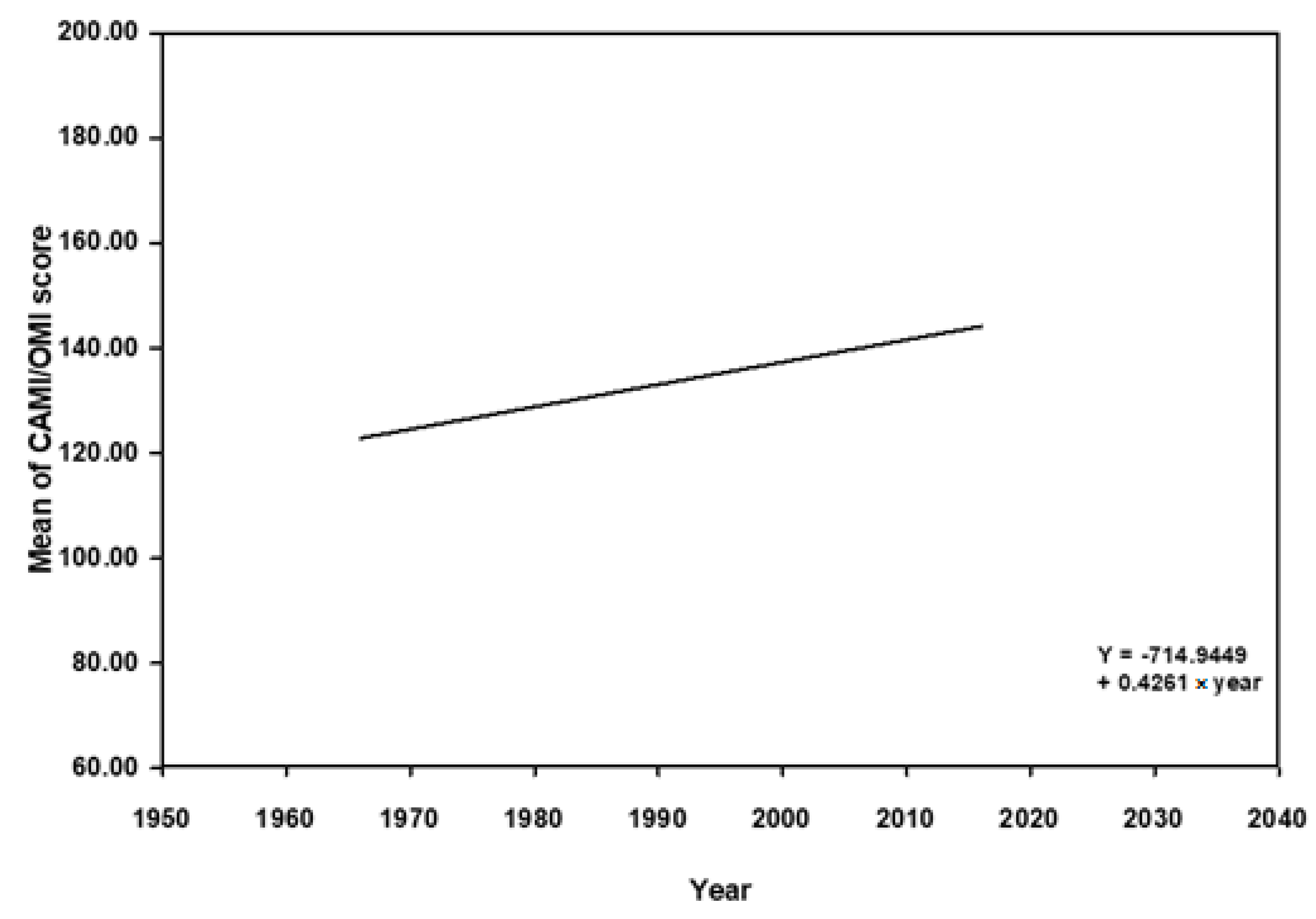
3.2. Correlation between Mean Scores of Social Distances, Attitude, and Years
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Sartorius, N. Fighting schizophrenia and its stigma: A new World Psychiatric Association educational programme. Br. J. Psychiatry 1997, 170, 297. [Google Scholar] [CrossRef] [PubMed]
- Jorm, A.F.; Christensen, H.; Griffiths, K.M. The impact of beyondblue: The national depression initiative on the Australian public’s recognition of depression and beliefs about treatments. Aust. N. Z. J. Psychiatry 2005, 39, 248–254. [Google Scholar] [CrossRef] [PubMed]
- Time to Change. Available online: http://www.time-to-change.org.uk (accessed on 3 March 2019).
- Makowski, A.C.; Mnich, E.E.; Ludwig, J.; Daubmann, A.; Bock, T.; Lambert, M.; Härter, M.; Dirmaier, J.; Tlach, L.; Liebherz, S. Changes in beliefs and attitudes toward people with depression and schizophrenia–results of a public campaign in Germany. Psychiatry Res. 2016, 237, 271–278. [Google Scholar] [CrossRef] [PubMed]
- Henderson, C.; Robinson, E.; Evans-Lacko, S.; Corker, E.; Rebollo-Mesa, I.; Rose, D.; Thornicroft, G. Public knowledge, attitudes, social distance and reported contact regarding people with mental illness 2009–2015. Acta Psychiatr. Scand. 2016, 134, 23–33. [Google Scholar] [CrossRef] [PubMed]
- Hansson, L.; Stjernswärd, S.; Svensson, B. Changes in attitudes, intended behaviour, and mental health literacy in the Swedish population 2009–2014: An evaluation of a national antistigma programme. Acta Psychiatr. Scand. 2016, 134, 71–79. [Google Scholar] [CrossRef] [PubMed]
- Robinson, E.J.; Henderson, C. Public knowledge, attitudes, social distance and reporting contact with people with mental illness 2009–2017. Psychol. Med. 2018. [Google Scholar] [CrossRef]
- Angermeyer, M.C.; Matschinger, H.; Carta, M.G.; Schomerus, G. Changes in the perception of mental illness stigma in Germany over the last two decades. Eur. Psychiatry 2014, 29, 390–395. [Google Scholar] [CrossRef]
- Angermeyer, M.C.; Matschinger, H.; Schomerus, G. Attitudes towards psychiatric treatment and people with mental illness: Changes over two decades. Br. J. Psychiatry 2013, 203, 146–151. [Google Scholar] [CrossRef]
- Schomerus, G.; Schwahn, C.; Holzinger, A.; Corrigan, P.W.; Grabe, H.J.; Carta, M.G.; Angermeyer, M.C. Evolution of public attitudes about mental illness: A systematic review and meta-analysis. Acta Psychiatr. Scand. 2012, 125, 440–452. [Google Scholar] [CrossRef]
- Mirnezami, H.F.; Jacobsson, L.; Edin-Liljegren, A. Changes in attitudes towards mental disorders and psychiatric treatment 1976–2014 in a Swedish population. Nord. J. Psychiatry 2016, 70, 38–44. [Google Scholar] [CrossRef]
- Henderson, C.; Noblett, J.; Parke, H.; Clement, S.; Caffrey, A.; Gale-Grant, O.; Schulze, B.; Druss, B.; Thornicroft, G. Mental health-related stigma in health care and mental health-care settings. Lancet Psychiatry 2014, 1, 467–482. [Google Scholar] [CrossRef]
- Thornicroft, G.; Mehta, N.; Clement, S.; Evans-Lacko, S.; Doherty, M.; Rose, D.; Koschorke, M.; Shidhaye, R.; O’Reilly, C.; Henderson, C. Evidence for effective interventions to reduce mental-health-related stigma and discrimination. Lancet 2016, 387, 1123–1132. [Google Scholar] [CrossRef]
- O’Reilly, C.L.; Bell, J.S.; Chen, T.F. Consumer-led mental health education for pharmacy students. Am. J. Pharm. Educ. 2010, 74, 167. [Google Scholar] [CrossRef] [PubMed]
- Rong, Y.; Glozier, N.; Luscombe, G.M.; Davenport, T.A.; Huang, Y.; Hickie, I.B. Improving knowledge and attitudes towards depression: A controlled trial among Chinese medical students. BMC Psychiatry 2011, 11, 36. [Google Scholar] [CrossRef]
- Knaak, S.; Patten, S.; Ungar, T. Mental illness stigma as a quality-of-care problem. Lancet Psychiatry 2015, 2, 863–864. [Google Scholar] [CrossRef]
- Knaak, S.; Mantler, E.; Szeto, A. Mental illness-related stigma in healthcare: Barriers to access and care and evidence-based solutions. Healthc. Manag. Forum 2017, 30, 111–116. [Google Scholar] [CrossRef]
- Lyons, Z. Attitudes of medical students toward psychiatry and psychiatry as a career: A systematic review. Acad. Psychiatry 2013, 37, 150–157. [Google Scholar] [CrossRef]
- Barkil-Oteo, A. Psychiatry’s identity crisis. Lancet 2012, 379, 2428. [Google Scholar] [CrossRef]
- Katschnig, H. Are psychiatrists an endangered species? Observations on internal and external challenges to the profession. World Psychiatry 2010, 9, 21–28. [Google Scholar] [CrossRef]
- Bishop, T.F.; Seirup, J.K.; Pincus, H.A.; Ross, J.S. Population of US practicing psychiatrists declined, 2003–2013, which may help explain poor access to mental health care. Health Aff. 2016, 35, 1271–1277. [Google Scholar] [CrossRef]
- Abbey, S.C.M.; Tranulis, C.; Moss, P.; Baici, W.; Dabby, L.; Gautam, M.; Paré, M. Stigma and discrimination. Can. J. Psychiatry 2011, 56, 1–9. [Google Scholar] [PubMed]
- Friedrich, B.; Evans-Lacko, S.; London, J.; Rhydderch, D.; Henderson, C.; Thornicroft, G. Anti-stigma training for medical students: The Education Not Discrimination project. Br. J. Psychiatry 2013, 202, s89–s94. [Google Scholar] [CrossRef] [PubMed]
- Stuart, H.; Chen, S.P.; Christie, R.; Dobson, K.; Kirsh, B.; Knaak, S.; Koller, M.; Krupa, T.; Lauria-Horner, B.; Luong, D. Opening minds in Canada: Background and rationale. Can. J. Psychiatry 2014, 59, 8–12. [Google Scholar] [CrossRef] [PubMed]
- Crismon, M.L.; Jermain, D.M.; Torian, S.J. Attitudes of pharmacy students toward mental illness. Am. J. Hosp. Pharm. 1990, 47, 1369–1373. [Google Scholar] [CrossRef]
- Volmer, D.; Mäesalu, M.; Bell, J.S. Pharmacy students’ attitudes toward and professional interactions with people with mental disorders. Int. J. Soc. Psychiatry 2008, 54, 402–413. [Google Scholar] [CrossRef]
- Tay, S.; Alcock, K.; Scior, K. Mental health problems among clinical psychologists: Stigma and its impact on disclosure and help-seeking. J. Clin. Psychol. 2018, 74, 1545–1555. [Google Scholar] [CrossRef]
- Mak, W.W.S.; Cheung, F.M.C.; Wong, S.Y.S.; Tang, W.K.; Lau, J.T.F.; Woo, J.; Lee, D.T.F. Stigma towards people with psychiatric disorders. Hong Kong Med. J. 2015, 21 (Suppl. 2), 9–12. [Google Scholar]
- Chiba, R.; Umeda, M.; Goto, K.; Miyamoto, Y.; Yamaguchi, S.; Kawakami, N. Psychometric properties of the Japanese version of the Recovery Attitudes Questionnaire (RAQ) among mental health providers: A questionnaire survey. BMC Psychiatry 2016, 16, 1–9. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. Ann. Intern. Med. 2009, 151, 264–269. [Google Scholar] [CrossRef]
- PROSPERO. International Prospective Register of Systematic Reviews. Available online: http://www.crd.york.ac.uk/prospero (accessed on September 20 2019).
- Link, B.G.; Cullen, F.T.; Frank, J.; Wozniak, J.F. The social rejection of former mental patients: Understanding why labels matter. Am. J. Sociol. 1987, 92, 1461–1500. [Google Scholar] [CrossRef]
- Evans-Lacko, S.; Rose, D.; Little, K.; Flach, C.; Rhydderch, D.; Henderson, C.; Thornicroft, G. Development and psychometric properties of the reported and intended behaviour scale (RIBS): A stigma-related behaviour measure. Epidemiol. Psychiatr. Sci. 2011, 20, 263–271. [Google Scholar] [CrossRef] [PubMed]
- Cohen, J.; Struening, E.L. Opinions about mental illness in the personnel of two large mental hospitals. J. Abnorm. Soc. Psychol. 1962, 64, 349. [Google Scholar] [CrossRef] [PubMed]
- Taylor, S.M.; Dear, M.J. Scaling community attitudes toward the mentally ill. Schizophr. Bull. 1981, 7, 225–240. [Google Scholar] [CrossRef] [PubMed]
- Gabbidon, J.; Clement, S.; van Nieuwenhuizen, A.; Kassam, A.; Brohan, E.; Norman, I.; Thornicroft, G. Mental Illness: Clinicians’ Attitudes (MICA) Scale—Psychometric properties of a version for healthcare students and professionals. Psychiatry Res. 2013, 206, 81–87. [Google Scholar] [CrossRef]
- Modgill, G.; Patten, S.B.; Knaak, S.; Kassam, A.; Szeto, A.C.H. Opening minds stigma scale for health care providers (OMS-HC): Examination of psychometric properties and responsiveness. BMC Psychiatry 2014, 14, 120. [Google Scholar] [CrossRef]
- Angermeyer, M.C.; Daubmann, A.; Wegscheider, K.; Mnich, E.; Schomerus, G.; vd Knesebeck, O. The relationship between biogenetic attributions and desire for social distance from persons with schizophrenia and major depression revisited. Epidemiol. Psychiatr. Sci. 2015, 24, 335–341. [Google Scholar] [CrossRef]
- Kermode, M.; Bowen, K.; Arole, S.; Pathare, S.; Jorm, A.F. Attitudes to people with mental disorders: A mental health literacy survey in a rural area of Maharashtra, India. Soc. Psychiatry Psychiatr. Epidemiol. 2009, 44, 1087–1096. [Google Scholar] [CrossRef]
- Reavley, N.J.; Jorm, A.F. Recognition of mental disorders and beliefs about treatment and outcome: Findings from an Australian national survey of mental health literacy and stigma. Aust. N. Z. J. Psychiatry 2011, 45, 947–956. [Google Scholar] [CrossRef]
- Schomerus, G.; Matschinger, H.; Angermeyer, M.C. Causal beliefs of the public and social acceptance of persons with mental illness: A comparative analysis of schizophrenia, depression and alcohol dependence. Psychol. Med. 2014, 44, 303–314. [Google Scholar] [CrossRef]
- Brohan, E.; Slade, M.; Clement, S.; Thornicroft, G. Experiences of mental illness stigma, prejudice and discrimination: A review of measures. BMC Health Serv. Res. 2010, 10, 80. [Google Scholar] [CrossRef]
- Charles, J.L.K.; Bentley, K.J. Measuring mental health provider-based stigma: Development and initial psychometric testing of a self-assessment instrument. Community Ment. Health J. 2018, 54, 33–48. [Google Scholar] [CrossRef] [PubMed]
- Corrigan, P.W.; Watson, A.C. Understanding the impact of stigma on people with mental illness. World Psychiatry 2002, 1, 16. [Google Scholar] [PubMed]
- Moxham, L.; Taylor, E.; Patterson, C.; Perlman, D.; Brighton, R.; Sumskis, S.; Keough, E.; Heffernan, T. Can a clinical placement influence stigma? An analysis of measures of social distance. Nurse Educ. Today 2016, 44, 170–174. [Google Scholar] [CrossRef] [PubMed]
- Twenge, J.M. Changes in masculine and feminine traits over time: A meta-analysis. Sex Roles 1997, 36, 305–325. [Google Scholar] [CrossRef]
- Twenge, J.M. Attitudes toward women, 1970–1995: A meta-analysis. Psychol. Women Q. 1997, 21, 35–51. [Google Scholar] [CrossRef]
- Twenge, J.M. The age of anxiety? The birth cohort change in anxiety and neuroticism, 1952–1993. J. Personal. Soc. Psychol. 2000, 79, 1007. [Google Scholar] [CrossRef]
- Twenge, J.M. Birth cohort changes in extraversion: A cross-temporal meta-analysis, 1966–1993. Personal. Individ. Differ. 2001, 30, 735–748. [Google Scholar] [CrossRef]
- Twenge, J.M. Changes in women’s assertiveness in response to status and roles: A cross-temporal meta-analysis, 1931–1993. J. Personal. Soc. Psychol. 2001, 81, 133. [Google Scholar] [CrossRef]
- Oliver, M.B.; Hyde, J.S. Gender differences in sexuality: A meta-analysis. Psychol. Bull. 1993, 114, 29. [Google Scholar] [CrossRef]
- Wells, B.E.; Twenge, J.M. Changes in young people’s sexual behavior and attitudes, 1943–1999: A cross-temporal meta-analysis. Rev. Gen. Psychol. 2005, 9, 249–261. [Google Scholar] [CrossRef]
- Hedges, L.V.; Becker, B.J. Statistical methods in the meta-analysis of research on gender differences. In The Psychology of Gender: Progress through Meta-Analysis; The Johns Hopkins University Press: Baltimore, MD, USA, 1986. [Google Scholar]
- Borenstein, M.; Hedges, L.; Higgins, J.; Rothstein, H. Comprehensive Meta-Analysis Version 3.3. 070; Biostat: Englewood, NJ, USA, 2014; Volume 104. [Google Scholar]
- Bell, J.S.; Johns, R.; Chen, T.F. Pharmacy students’ and graduates’ attitudes towards people with schizophrenia and severe depression. Am. J. Pharm. Educ. 2006, 70, 77. [Google Scholar] [CrossRef] [PubMed]
- Bell, J.S.; Aaltonen, S.E.; Airaksinen, M.S.; Volmer, D.; Gharat, M.S.; Muceniece, R.; Vitola, A.; Foulon, V.; Desplenter, F.A.; Chen, T.F. Determinants of mental health stigma among pharmacy students in Australia, Belgium, Estonia, Finland, India and Latvia. Int. J. Soc. Psychiatry 2010, 56, 3–14. [Google Scholar] [CrossRef] [PubMed]
- Hanzawa, S.; Nosaki, A.; Yatabe, K.; Nagai, Y.; Tanaka, G.; Nakane, H.; Nakane, Y. Study of understanding the internalized stigma of schizophrenia in psychiatric nurses in Japan. Psychiatry Clin. Neurosci. 2012, 66, 113–120. [Google Scholar] [CrossRef] [PubMed]
- Loch, A.A.; Hengartner, M.P.; Guarniero, F.B.; Lawson, F.L.; Wang, Y.P.; Gattaz, W.F.; Rössler, W. The more information, the more negative stigma towards schizophrenia: Brazilian general population and psychiatrists compared. Psychiatry Res. 2013, 205, 185–191. [Google Scholar] [CrossRef]
- Mittal, D.; Corrigan, P.; Sherman, M.D.; Chekuri, L.; Han, X.; Reaves, C.; Mukherjee, S.; Morris, S.; Sullivan, G. Healthcare providers’ attitudes toward persons with schizophrenia. Psychiatr. Rehabil. J. 2014, 37, 297. [Google Scholar] [CrossRef]
- Reavley, N.J.; Mackinnon, A.J.; Morgan, A.J.; Jorm, A.F. Stigmatising attitudes towards people with mental disorders: A comparison of Australian health professionals with the general community. Aust. N. Z. J. Psychiatry 2014, 48, 433–441. [Google Scholar] [CrossRef]
- Amarasuriya, S.D.; Jorm, A.F.; Reavley, N.J.; Mackinnon, A.J. Stigmatising attitudes of undergraduates towards their peers with depression: A cross-sectional study in Sri Lanka. BMC Psychiatry 2015, 15, 129. [Google Scholar] [CrossRef]
- Dabby, L.; Tranulis, C.; Kirmayer, L.J. Explicit and implicit attitudes of Canadian psychiatrists toward people with mental illness. Can. J. Psychiatry 2015, 60, 451–459. [Google Scholar] [CrossRef]
- O’reilly, C.L.; Bell, J.S.; Kelly, P.J.; Chen, T.F. Exploring the relationship between mental health stigma, knowledge and provision of pharmacy services for consumers with schizophrenia. Res. Soc. Adm. Pharm. 2015, 11, e101–e109. [Google Scholar] [CrossRef]
- Smith, J.D.; Mittal, D.; Chekuri, L.; Han, X.; Sullivan, G. A comparison of provider attitudes toward serious mental illness across different health care disciplines. Stigma Health 2017, 2, 327. [Google Scholar] [CrossRef]
- Pranckeviciene, A.; Zardeckaite-Matulaitiene, K.; Marksaityte, R.; Endriulaitiene, A.; Tillman, D.R.; Hof, D.D. Social distance in Lithuanian psychology and social work students and professionals. Soc. Psychiatry Psychiatr. Epidemiol. 2018, 53, 849–857. [Google Scholar] [CrossRef]
- Tillman, D.R.; Hof, D.D.; Pranckeviciene, A.; Endriulaitienė, A.; Markšaitytė, R.; Žardeckaitė-Matulaitienė, K. Social distance from mental illness among counseling, social work, and psychology students and helping professionals. J. Soc. Action Couns. Psychol. 2018, 10, 24–37. [Google Scholar]
- Perlman, D.; Moxham, L.; Patterson, C.; Cregan, A. Stigmatization behavior of pre-registration nurses: Do the self-determined psychological needs influence this? Issues Ment. Health Nurs. 2019, 40, 342–346. [Google Scholar] [CrossRef]
- LeMay, M.L. Counselor candidates’ attitudes and opinions about mental illness. Couns. Educ. Superv. 1968, 8, 51–54. [Google Scholar] [CrossRef]
- Levine, D. A cross-national study of attitudes toward mental illness. J. Abnorm. Psychol. 1972, 80, 111. [Google Scholar] [CrossRef]
- Kirkby, R.J.; James, A. Attitudes of medical practitioners to mental illness. Aust. N. Z. J. Psychiatry 1979, 13, 165–168. [Google Scholar] [CrossRef]
- Murray, M.G.; Steffen, J.J. Attitudes of case managers toward people with serious mental illness. Community Ment. Health J. 1999, 35, 505–514. [Google Scholar] [CrossRef]
- Smith, A.L. An Investigation of Attitudes towards Adults with Mental Illness among Mental Health Professionals In-Training, Non Mental Health Professionals In-Training, Mental Health Professionals, and Non Mental Health Professionals; The University of North Carolina at Greensboro: Greensboro, NC, USA, 2008. [Google Scholar]
- Arvaniti, A.; Samakouri, M.; Kalamara, E.; Bochtsou, V.; Bikos, C.; Livaditis, M. Health service staff’s attitudes towards patients with mental illness. Soc. Psychiatry Psychiatr. Epidemiol. 2009, 44, 658–665. [Google Scholar] [CrossRef]
- Smith, A.L.; Cashwell, C.S. Stigma and mental illness: Investigating attitudes of mental health and non-mental-health professionals and trainees. J. Humanist. Couns. Educ. Dev. 2010, 49, 189–202. [Google Scholar] [CrossRef]
- Chambers, M.; Guise, V.; Välimäki, M.; Botelho, M.A.R.; Scott, A.; Staniuliene, V.; Zanotti, R. Nurses’ attitudes to mental illness: A comparison of a sample of nurses from five European countries. Int. J. Nurs. Stud. 2010, 47, 350–362. [Google Scholar] [CrossRef]
- Guise, V.; Chambers, M.; Välimäki, M.; Makkonen, P. A mixed-mode approach to data collection: Combining web and paper questionnaires to examine nurses’ attitudes to mental illness. J. Adv. Nurs. 2010, 66, 1623–1632. [Google Scholar] [CrossRef] [PubMed]
- O’Connor, K.; Brennan, D.; O’loughlin, K.; Wilson, L.; Pillay, D.; Clarke, M.; Casey, P.; Malone, K.; Lane, A. Attitudes towards patients with mental illness in Irish medical students. Ir. J. Med Sci. 2013, 182, 679–685. [Google Scholar] [CrossRef] [PubMed]
- Kopera, M.; Suszek, H.; Bonar, E.; Myszka, M.; Gmaj, B.; Ilgen, M.; Wojnar, M. Evaluating explicit and implicit stigma of mental illness in mental health professionals and medical students. Community Ment. Health J. 2015, 51, 628–634. [Google Scholar] [CrossRef] [PubMed]
- Winkler, P.; Mladá, K.; Janoušková, M.; Weissová, A.; Tušková, E.; Csémy, L.; Evans-Lacko, S. Attitudes towards the people with mental illness: Comparison between Czech medical doctors and general population. Soc. Psychiatry Psychiatr. Epidemiol. 2016, 51, 1265–1273. [Google Scholar] [CrossRef]
- Janoušková, M.; Weissová, A.; Formánek, T.; Pasz, J.; Bankovská Motlová, L. Mental illness stigma among medical students and teachers. Int. J. Soc. Psychiatry 2017, 63, 744–751. [Google Scholar] [CrossRef]
- Mosaku, K.S.; Wallymahmed, A.H. Attitudes of primary care health workers towards mental health patients: A cross-sectional study in Osun state, Nigeria. Community Ment. Health J. 2017, 53, 176–182. [Google Scholar] [CrossRef]
- Siqueira, S.R.G.; Abelha, L.; Lovisi, G.M.; Sarução, K.R.; Yang, L. Attitudes towards the mentally ill: A study with health workers at a university hospital in Rio de Janeiro. Psychiatr. Q. 2017, 88, 25–38. [Google Scholar] [CrossRef]
- Cremonini, V.; Pagnucci, N.; Giacometti, F.; Rubbi, I. Health care professionals attitudes towards mental illness: Observational study performed at a public health facility in northern Italy. Arch. Psychiatr. Nurs. 2018, 32, 24–30. [Google Scholar] [CrossRef]
- WHO. Mental Health Action Plan 2013–2020; WHO: Geneva, Switzerland, 2014. [Google Scholar]
- Mino, Y.; Yasuda, N.; Tsuda, T.; Shimodera, S. Effects of a one-hour educational program on medical students’ attitudes to mental illness. Psychiatry Clin. Neurosci. 2001, 55, 501–507. [Google Scholar] [CrossRef]
- Kakuma, R.; Kleintjes, S.; Lund, C.; Drew, N.; Green, A.; Flisher, A.J. Mental Health Stigma: What is being done to raise awareness and reduce stigma in South Africa? Afr. J. Psychiatry 2010, 13, 116–124. [Google Scholar] [CrossRef]
- Bayar, M.R.; Poyraz, B.Ç.; Aksoy-Poyraz, C.; Arikan, M.K. Reducing mental illness stigma in mental health professionals using a web-based approach. Isr. J. Psychiatry Relat. Sci. 2009, 46, 226–230. [Google Scholar] [PubMed]
- ÜÇOk, A.; Soyguer, H.; Atakli, C.; Kuşcu, K.; Sartorius, N.; Duman, Z.C.; Polat, A.; Erkoç, Ş. The impact of antistigma education on the attitudes of general practitioners regarding schizophrenia. Psychiatry Clin. Neurosci. 2006, 60, 439–443. [Google Scholar] [CrossRef] [PubMed]
- Altindag, A.; Yanik, M.; Ucok, A.; Alptekin, K.; Ozkan, M. Effects of an antistigma program on medical students’ attitudes towards people with schizophrenia. Psychiatry Clin. Neurosci. 2006, 60, 283–288. [Google Scholar] [CrossRef] [PubMed]
- Happell, B.; Byrne, L.; McAllister, M.; Lampshire, D.; Roper, C.; Gaskin, C.J.; Martin, G.; Wynaden, D.; McKenna, B.; Lakeman, R. Consumer involvement in the tertiary-level education of mental health professionals: A systematic review. Int. J. Ment. Health Nurs. 2014, 23, 3–16. [Google Scholar] [CrossRef] [PubMed]
- Cooper, C.; Carver, N. Problem based learning in mental health nursing: The students’ experience. Int. J. Ment. Health Nurs. 2012, 21, 175–183. [Google Scholar] [CrossRef] [PubMed]
| Study Author, Publication Date | Country | Year of Data Collection | Group | N | Total Score, μ (SD) |
|---|---|---|---|---|---|
| Crismon, 1990 [25] | United States | 1988 | Pharmacists | 165 | 15.87 (4.08) |
| Bell et al., 2006 [55] | Australia | 2004 | Third-year pharmacy students | 216 | 18.75 (5.04) |
| Pharmacy graduates | 232 | 18.52 (5.00) | |||
| Volmer et al., 2008 [26] | Estonia | 2006 | Pharmacy students | 157 | 20.36 (3.88) |
| Bell et al., 2010 [56] | Australia, Belgium, India, Finland, Estonia, Latvia | 2006 | Pharmacy students in India | 106 | 18.75 (3.57) |
| Pharmacy students in Australia | 241 | 19.65 (3.97) | |||
| Pharmacy students in Finland | 130 | 18.05 (3.12) | |||
| Pharmacy students in Estonia and Latvia | 70 | 20.90 (4.04) | |||
| Pharmacy students in Belgium | 102 | 19.61 (2.92) | |||
| Hanzawa et al., 2012 [57] | Japan | 2009 | Psychiatric nurses | 215 | 19.76 (4.30) |
| Loch et al., 2013 [58] | Brazil | 2009 | Psychiatrists | 1414 | 14.00 (3.58) |
| Mittal et al., 2014 [59] | United States | 2011 | Mental health providers | 205 | 14.87 (6.01) |
| Primary care providers | 146 | 16.23 (6.89) | |||
| Reavley et al., 2014 [60] | Australia | 2012 | General Practitioners | 518 | 14.14 (5.18) |
| Psychiatrists | 506 | 14.14 (5.67) | |||
| Psychologists | 498 | 12.25 (4.48) | |||
| Amarasuriya et al., 2015 [61] | Sri Lanka | 2013 | Medical students | 605 | 13.03 (4.02) |
| Dabby et al., 2015 [62] | Canada | 2012 | Psychiatrists | 68 | 10.47 (3.36) |
| Mak et al., 2015 [28] | Hong Kong | 2011 | Nursing professionals a | 209 | 16.31 (5.06) |
| Social work professionals a | 150 | 13.23 (4.29) | |||
| Medical professionals a | 149 | 16.87 (5.13) | |||
| Nursing students a | 203 | 12.81 (4.99) | |||
| Social work students a | 207 | 13.86 (5.04) | |||
| Medical students a | 60 | 13.30 (4.88) | |||
| Nursing professionals b | 186 | 18.55 (4.77) | |||
| Social work professionals b | 154 | 15.61 (4.34) | |||
| Medical professionals b | 201 | 19.74 (4.96) | |||
| Nursing students b | 203 | 16.17 (4.99) | |||
| Social work students b | 185 | 17.99 (5.71) | |||
| Medical students b | 52 | 16.73 (5.55) | |||
| O’Reilly et al., 2015 [63] | Australia | 2009 | Pharmacists | 186 | 17.81 (3.79) |
| Chiba et al., 2016 [29] | Japan | 2012 | Psychiatrists, nurses, clinical psychologists, pharmacists, occupational therapists, social workers | 307 | 15.22 (4.75) |
| Smith et al., 2017 [64] | United States | 2012 | Primary care nurses | 91 | 15.83 (4.67) |
| Primary care physicians | 55 | 16.88 (4.05) | |||
| Mental health nurses | 67 | 15.01 (4.81) | |||
| Psychiatrists | 62 | 15.92 (5.07) | |||
| Psychologists | 76 | 13.89 (3.91) | |||
| Pranckeviciene et al., 2018 [65] | Lithuanian | 2015 | Students (social work) | 296 | 18.14 (3.76) |
| Students (psychology) | 419 | 17.18 (3.64) | |||
| Social workers | 111 | 17.43 (4.00) | |||
| Psychologists | 122 | 16.61 (3.37) | |||
| Tay et al., 2018 [27] | United Kingdom | 2015 | Psychologists | 678 | 12.18 (3.71) |
| Tillman et al., 2018 [66] | United States | 2016 | Students (social work) | 104 | 11.90 (3.77) |
| Students (counseling) | 87 | 11.04 (3.20) | |||
| Students (psychology) | 111 | 11.90 (3.94) | |||
| Social workers | 23 | 10.01 (3.59) | |||
| Counselors | 34 | 11.02 (3.24) | |||
| Psychologists | 38 | 12.13 (3.16) | |||
| Perlman et al., 2019 [67] | Australia | 2016 | Nurses | 168 | 15.82 (3.76) |
| Study Author, Publication Date | Scale | Country | Year of Data Collection | Group | N | Total Score, μ (SD) |
|---|---|---|---|---|---|---|
| LeMay et al., 1968 [68] | OMI | United States | 1966 | Counselor candidates (male) | 31 | 134.50 (14.66) |
| Counselor candidates (female) | 50 | 134.29 (13.13) | ||||
| Levine et al., 1972 [69] | OMI | Great Britain, Czechoslovakia, Germany | 1968 | Physicians (British) | 181 | 127.23 (19.52) |
| Physicians (Czechoslovakian) | 103 | 110.75 (18.52) | ||||
| Nurses (West German) | 80 | 120.69 (22.52) | ||||
| Nurses (British) | 188 | 128.30 (20.18) | ||||
| Nurses (Czechoslovakian) | 116 | 105.35 (19.31) | ||||
| Kirkby et al., 1979 [70] | OMI | Australia | 1977 | Medical practitioners | 37 | 129.18 (20.25) |
| Murray et al., 1999 [71] | OMI | United States | 1997 | Supportive case managers | 24 | 147.48 (16.56) |
| Intense case managers | 23 | 135.87 (17.30) | ||||
| Smith et al., 2008 [72] | CAMI | United States | 2006 | Health professionals and medical students | 168 | 113.87 (20.83) |
| Arvaniti et al., 2009 [73] | OMI | Greece | 2006 | Health professionals and medical students | 580 | 147.38 (25.85) |
| Smith et al., 2010 [74] | CAMI | United States | 2008 | Mental health students | 58 | 143.10 (15.59) |
| Mental health professionals | 58 | 141.40 (17.19) | ||||
| Chambers et al., 2010 [75] | CAMI | Finland, Lithuania, Ireland, Italy, Portugal | 2007 | Nurses | 810 | 134.00 (20.74) |
| Guise et al., 2010 [76] | CAMI | United Kingdom | 2009 | Nurses | 81 | 135.50 (17.07) |
| O’ Connor et al., 2013 [77] | CAMI | Ireland | 2010 | Medical students (third year) | 140 | 159.20 (14.60) |
| Medical students (final year) | 145 | 158.50 (16.50) | ||||
| Kopera et al., 2015 [78] | OMI | Poland | 2011 | Psychiatrists, psychotherapists Medical students | 57 | 147.80 (13.96) |
| Winkler et al., 2016 [79] | CAMI | Czech Republic | 2014 | Medical doctors | 1200 | 142.22 (16.30) |
| Janouskova et al., 2017 [80] | CAMI | Czech Republic | 2016 | Medical students | 457 | 163.56 (18.68) |
| Mosaku et al., 2017 [81] | CAMI | Nigeria | 2013 | Health workers | 112 | 115.60 (19.96) |
| Siqueira et al., 2017 [82] | CAMI | Brazil | 2014 | Health professionals | 246 | 113.20 (14.80) |
| Cremonini et al., 2018 [83] | CAMI | Italy | 2016 | Health care professionals | 120 | 160.77 (15.60) |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lien, Y.-Y.; Lin, H.-S.; Tsai, C.-H.; Lien, Y.-J.; Wu, T.-T. Changes in Attitudes toward Mental Illness in Healthcare Professionals and Students. Int. J. Environ. Res. Public Health 2019, 16, 4655. https://doi.org/10.3390/ijerph16234655
Lien Y-Y, Lin H-S, Tsai C-H, Lien Y-J, Wu T-T. Changes in Attitudes toward Mental Illness in Healthcare Professionals and Students. International Journal of Environmental Research and Public Health. 2019; 16(23):4655. https://doi.org/10.3390/ijerph16234655
Chicago/Turabian StyleLien, Yin-Yi, Hui-Shin Lin, Chi-Hsuan Tsai, Yin-Ju Lien, and Ting-Ting Wu. 2019. "Changes in Attitudes toward Mental Illness in Healthcare Professionals and Students" International Journal of Environmental Research and Public Health 16, no. 23: 4655. https://doi.org/10.3390/ijerph16234655
APA StyleLien, Y.-Y., Lin, H.-S., Tsai, C.-H., Lien, Y.-J., & Wu, T.-T. (2019). Changes in Attitudes toward Mental Illness in Healthcare Professionals and Students. International Journal of Environmental Research and Public Health, 16(23), 4655. https://doi.org/10.3390/ijerph16234655





