Examining the Factor Structure of the Pittsburgh Sleep Quality Index in a Multi-Ethnic Working Population in Singapore
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Sample
2.2. Measurements
2.3. Statistical Analysis
2.4. Ethics Approval
3. Results
3.1. Characteristics of Study Participants
3.2. Reliability and Correlation Analysis of PSQI Subscales
3.3. Exploratory Factor Analysis
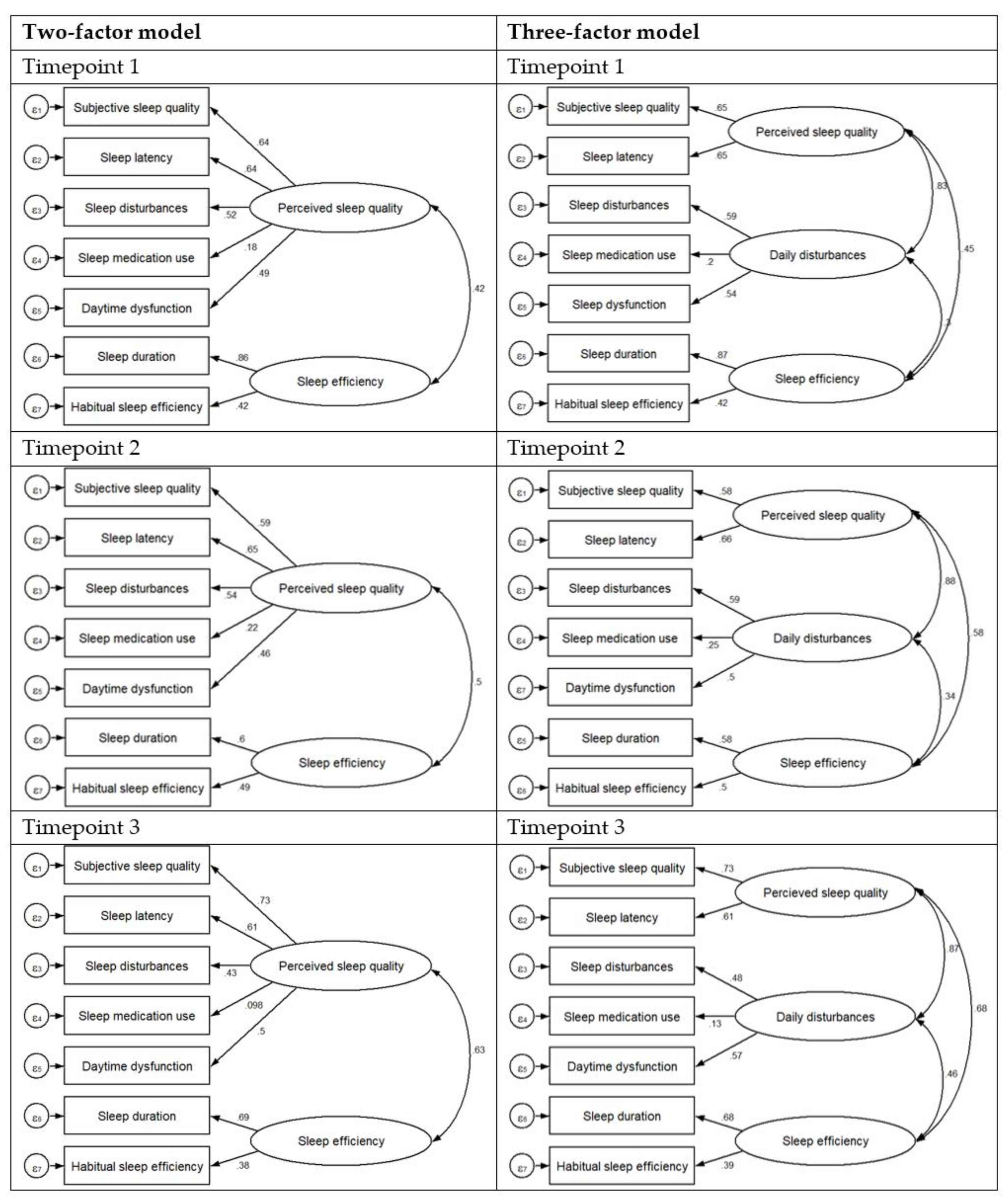
3.4. Confirmatory Factor Analysis
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Medic, G.; Wille, M.; Hemels, M.E.H. Short- and long-term health consequences of sleep disruption. Nat. Sci. Sleep 2017, 9, 151–161. [Google Scholar] [CrossRef] [PubMed]
- Cho, J.R.; Joo, E.Y.; Koo, D.L.; Hong, S.B. Let there be no light: The effect of bedside light on sleep quality and background electroencephalographic rhythms. Sleep Med. 2013, 14, 1422–1425. [Google Scholar] [CrossRef] [PubMed]
- Cho, C.H.; Lee, H.J.; Yoon, H.K.; Kang, S.G.; Bok, K.N.; Jung, K.Y.; Kim, L.; Lee, E.I. Exposure to dim artificial light at night increases REM sleep and awakenings in humans. Chronobiol. Int. 2016, 33, 117–123. [Google Scholar] [CrossRef] [PubMed]
- Falchi, F.; Cinzano, P.; Duriscoe, D.; Kyba, C.C.M.; Elvidge, C.D.; Baugh, K.; Portnov, B.A.; Rybnikova, N.A.; Furgoni, R. The new world atlas of artificial night sky brightness. Sci. Adv. 2016, 2, e1600377. [Google Scholar] [CrossRef] [PubMed]
- Walch, O.J.; Cochran, A.; Forger, D.B. A global quantification of “normal” sleep schedules using smartphone data. Sci. Adv. 2016, 2, e1501705. [Google Scholar] [CrossRef] [PubMed]
- Buysse, D.J. Sleep Health: Can We Define It? Does It Matter? Sleep 2014, 37, 9–17. [Google Scholar] [CrossRef]
- Buysse, D.J.; Reynolds, C.F., 3rd; Monk, T.H.; Berman, S.R.; Kupfer, D.J. The Pittsburgh Sleep Quality Index: A new instrument for psychiatric practice and research. Psychiatry Res. 1989, 28, 193–213. [Google Scholar] [CrossRef]
- Mollayeva, T.; Thurairajah, P.; Burton, K.; Mollayeva, S.; Shapiro, C.M.; Colantonio, A. The Pittsburgh sleep quality index as a screening tool for sleep dysfunction in clinical and non-clinical samples: A systematic review and meta-analysis. Sleep Med. Rev. 2016, 25, 52–73. [Google Scholar] [CrossRef]
- Manzar, M.D.; BaHammam, A.S.; Hameed, U.A.; Spence, D.W.; Pandi-Perumal, S.R.; Moscovitch, A.; Streiner, D.L. Dimensionality of the Pittsburgh Sleep Quality Index: A systematic review. Health Qual. Life Outcomes 2018, 16, 89. [Google Scholar] [CrossRef]
- Mariman, A.; Vogelaers, D.; Hanoulle, I.; Delesie, L.; Tobback, E.; Pevernagie, D. Validation of the three-factor model of the PSQI in a large sample of chronic fatigue syndrome (CFS) patients. J. Psychosom. Res. 2012, 72, 111–113. [Google Scholar] [CrossRef]
- Nicassio, P.M.; Ormseth, S.R.; Custodio, M.K.; Olmstead, R.; Weisman, M.H.; Irwin, M.R. Confirmatory factor analysis of the Pittsburgh Sleep Quality Index in rheumatoid arthritis patients. Behav. Sleep Med. 2014, 12, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Otte, J.L.; Rand, K.L.; Carpenter, J.S.; Russell, K.M.; Champion, V.L. Factor Analysis of the Pittsburgh Sleep Quality Index in Breast Cancer Survivors. J. Pain Symptom Manag. 2013, 45, 620–627. [Google Scholar] [CrossRef] [PubMed]
- Lequerica, A.; Chiaravalloti, N.; Cantor, J.; Dijkers, M.; Wright, J.; Kolakowsky-Hayner, S.A.; Bushnick, T.; Hammond, F.; Bell, K. The factor structure of the Pittsburgh Sleep Quality Index in persons with traumatic brain injury. A NIDRR TBI model systems module study. NeuroRehabilitation 2014, 35, 485–492. [Google Scholar] [CrossRef] [PubMed]
- Fontes, F.; Goncalves, M.; Maia, S.; Pereira, S.; Severo, M.; Lunet, N. Reliability and validity of the Pittsburgh Sleep Quality Index in breast cancer patients. Support. Care Cancer Off. J. Multinatl. Assoc. Support. Care Cancer 2017, 25, 3059–3066. [Google Scholar] [CrossRef]
- Morris, J.L.; Rohay, J.; Chasens, E.R. Sex Differences in the Psychometric Properties of the Pittsburgh Sleep Quality Index. J. Women’s Health 2017, 27, 278–282. [Google Scholar] [CrossRef]
- Yunus, R.M.; Wazid, S.W.; Hairi, N.N.; Choo, W.Y.; Hairi, F.M.; Sooryanarayana, R.; Ahmad, S.N.; Razak, I.A.; Peramalah, D.; Aziz, S.A.; et al. Association between elder abuse and poor sleep: A cross-sectional study among rural older Malaysians. PLoS ONE 2017, 12, e0180222. [Google Scholar] [CrossRef]
- Hinz, A.; Glaesmer, H.; Brähler, E.; Löffler, M.; Engel, C.; Enzenbach, C.; Hegerl, U.; Sander, C. Sleep quality in the general population: Psychometric properties of the Pittsburgh Sleep Quality Index, derived from a German community sample of 9284 people. Sleep Med. 2017, 30, 57–63. [Google Scholar] [CrossRef]
- Dunleavy, G.; Sathish, T.; Nazeha, N.; Soljak, M.; Visvalingam, N.; Bajpai, R.; Yap, H.S.; Roberts, A.C.; Quoc, T.T.; Tonon, A.C.; et al. Health Effects of Underground Workspaces (HEUW) cohort in Singapore: Study design and baseline characteristics. Epidemiol. Health 2019, 41, e2019025. [Google Scholar] [CrossRef]
- Mundfrom, D.J.; Shaw, D.G.; Ke, T.L. Minimum Sample Size Recommendations for Conducting Factor Analyses. Int. J. Test. 2005, 5, 159–168. [Google Scholar] [CrossRef]
- MacCallum, R.C.; Widaman, K.F.; Zhang, S.; Hong, S. Sample size in factor analysis. Psychol. Methods 1999, 4, 84–99. [Google Scholar] [CrossRef]
- Ferguson, E.; Cox, T. Exploratory Factor Analysis: A Users’Guide. Int. J. Sel. Assess. 1993, 1, 84–94. [Google Scholar] [CrossRef]
- Tabachnick, B.G.; Fidell, L.S. Using Multivariate Statistics, 5th ed.; Pearson: Boston, MA, USA, 2006. [Google Scholar]
- Stevens, J.P. Applied Multivariate Statistics for the Social Sciences, 2nd ed.; Erlbaum: Hillsdale, NJ, USA, 1992. [Google Scholar]
- Long, J.S. Confirmatory Factor Analysis; SAGE Publications: Thousand Oaks, CA, USA, 1983. [Google Scholar] [CrossRef]
- Browne, M.W.; Cudeck, R. Alternative Ways of Assessing Model Fit; SAGE: Newbury Park, CA, USA, 1993; pp. 136–162. [Google Scholar]
- Raftery, A.E. Bayesian Model Selection in Structural Equation Models; SAGE: Newbury Park, CA, USA, 1993. [Google Scholar]
- Kline, R. Principles and Practices of Structural Equation Modeling; The Guilford Press: New York, NY, USA, 2005. [Google Scholar]
- Koh, H.W.; Lim, R.B.; Chia, K.S.; Lim, W.Y. The Pittsburgh Sleep Quality Index in a multi-ethnic Asian population contains a three-factor structure. Sleep Breath. = Schlaf Atm. 2015, 19, 1147–1154. [Google Scholar] [CrossRef] [PubMed]
- Comrey, A.L.; Lee, H.B. A first course in factor analysis, 2nd ed.; Lawrence Erlbaum Associates, Inc.: Hillsdale, NJ, USA, 1992; p. xii, 430. [Google Scholar]
- Hair, J.F.; Black, W.C.; Babin, B.J.; Anderson, R.E. Multivariate Data Analysis: A Global Perspective, 7th ed.; Prentice Hall: Upper Saddle River, NJ, USA, 2009. [Google Scholar]
- Chiang, G.S.H.; Sim, B.L.H.; Lee, J.J.M.; Quah, J.H.M. Determinants of poor sleep quality in elderly patients with diabetes mellitus, hyperlipidemia and hypertension in Singapore. Prim. Health Care Res. Dev. 2018, 19, 610–615. [Google Scholar] [CrossRef] [PubMed]
- Shum, A.; Taylor, B.J.; Thayala, J.; Chan, M.F. The effects of sedative music on sleep quality of older community-dwelling adults in Singapore. Complement. Ther. Med. 2014, 22, 49–56. [Google Scholar] [CrossRef]
- Ebrahimi, A.A.; Ghalebandi, M.; Salehi, M.; Alavi, K. A comparative study of the components of sleep quality in medical outpatients. Int. J. Psychiatry Clin. Pract. 2009, 13, 184–187. [Google Scholar] [CrossRef]
- Lusic, K.L.; Valic, M.; Pecotic, R.; Pavlinac, D.I.; Dogas, Z. Good and poor sleepers among OSA patients: Sleep quality and overnight polysomnography findings. Neurol. Sci. Off. J. Ital. Neurol. Soc. Ital. Soc. Clin. Neurophysiol. 2017, 38, 1299–1306. [Google Scholar] [CrossRef]
- Selvi, Y.; Boysan, M.; Kandeger, A.; Uygur, O.F.; Sayin, A.A.; Akbaba, N.; Koc, B. Heterogeneity of sleep quality in relation to circadian preferences and depressive symptomatology among major depressive patients. J. Affect. Disord. 2018, 235, 242–249. [Google Scholar] [CrossRef]
- Becker, N.B.; de Neves Jesus, S. Adaptation of a 3-factor model for the Pittsburgh Sleep Quality Index in Portuguese older adults. Psychiatry Res. 2017, 251, 298–303. [Google Scholar] [CrossRef]
- Magee, C.A.; Caputi, P.; Iverson, D.C.; Huang, X.-F. An investigation of the dimensionality of the Pittsburgh Sleep Quality Index in Australian adults. Sleep Biol. Rhythms 2008, 6, 222–227. [Google Scholar] [CrossRef]
- Passos, M.H.P.; Silva, H.A.; Pitangui, A.C.R.; Oliveira, V.M.A.; Lima, A.S.; Araújo, R.C. Reliability and validity of the Brazilian version of the Pittsburgh Sleep Quality Index in adolescents. J. Pediatr. 2017, 93, 200–206. [Google Scholar] [CrossRef]
- Nunnally, J.C. Psychometric Theory; McGraw-Hill Higher: New York, NY, USA, 1994. [Google Scholar]
- Rener-Sitar, K.; John, M.T.; Bandyopadhyay, D.; Howell, M.J.; Schiffman, E.L. Exploration of dimensionality and psychometric properties of the Pittsburgh Sleep Quality Index in cases with temporomandibular disorders. Health Qual. Life Outcomes 2014, 12, 10. [Google Scholar] [CrossRef] [PubMed]
- Backhaus, J.; Junghanns, K.; Broocks, A.; Riemann, D.; Hohagen, F. Test-retest reliability and validity of the Pittsburgh Sleep Quality Index in primary insomnia. J. Psychosom. Res. 2002, 53, 737–740. [Google Scholar] [CrossRef]
- Gelaye, B.; Lohsoonthorn, V.; Lertmeharit, S.; Pensuksan, W.C.; Sanchez, S.E.; Lemma, S.; Berhane, Y.; Zhu, X.; Vélez, J.C.; Barbosa, C.; et al. Construct Validity and Factor Structure of the Pittsburgh Sleep Quality Index and Epworth Sleepiness Scale in a Multi-National Study of African, South East Asian and South American College Students. PLoS ONE 2015, 9, e116383. [Google Scholar] [CrossRef]
- Pilz, L.K.; Keller, L.K.; Lenssen, D.; Roenneberg, T. Time to rethink sleep quality: PSQI scores reflect sleep quality on workdays. Sleep 2018, 41. [Google Scholar] [CrossRef] [PubMed]
| Variables | Timepoint 1 n = 464 | Timepoint 2 n = 424 | Timepoint 3 n = 329 |
|---|---|---|---|
| Age (years), (mean ± SD) | 39.0 ± 11.4 | 39.2 ± 11.3 | 40.7 ± 11.1 |
| Age (years), (n, %) | |||
| 21–30 | 153 (33.0) | 136 (32.1) | 84 (25.5) |
| 31–40 | 121 (26.1) | 117 (27.6) | 98 (29.8) |
| >40 | 190 (41.0) | 171 (40.3) | 147 (44.7) |
| Gender, (n, %) | |||
| Male | 369 (79.5) | 334 (78.8) | 256 (77.8) |
| Female | 95 (20.5) | 90 (21.2) | 73 (22.2) |
| Ethnicity, (n, %) | |||
| Chinese | 296 (63.8) | 271 (63.9) | 216 (65.7) |
| Malays | 99 (21.3) | 89 (21.0) | 60 (18.2) |
| Indians | 48 (10.3) | 44 (10.4) | 39 (11.9) |
| Others a | 21 (4.5) | 20 (4.7) | 14 (4.26) |
| Marital status, (n, %) | |||
| Singleb | 184 (39.7) | 168 (39.6) | 116 (35.3) |
| Married | 280 (60.3) | 256 (60.4) | 213 (64.7) |
| Education, (n, %) | |||
| Primary, secondary and higher secondary | 116 (25.0) | 103 (24.3) | 86 (26.1) |
| Pre-college | 183 (39.4) | 172 (40.6) | 123 (37.4) |
| College and above | 165 (35.6) | 149 (35.1) | 120 (36.5) |
| Monthly income, (n, %) | |||
| <S$4000 | 331 (71.3) | 305 (71.9) | 227 (69.0) |
| ≥S$4000 | 133 (28.7) | 119 (28.1) | 102 (31.0) |
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | ||
|---|---|---|---|---|---|---|---|---|---|
| Timepoint 1 | 1. Subjective sleep quality | 1 | |||||||
| 2. Sleep latency | 0.42 ** | 1 | |||||||
| 3. Sleep duration | 0.29 ** | 0.22 ** | 1 | ||||||
| 4. Habitual sleep efficiency | 0.09 * | 0.15 ** | 0.36 ** | 1 | |||||
| 5. Sleep disturbances | 0.27 ** | 0.36 ** | 0.10 * | 0.10 * | 1 | ||||
| 6. Sleep medication use | 0.09 * | 0.07 | 0.08 | 0.06 | 0.08 | 1 | |||
| 7. Daytime dysfunction | 0.32 ** | 0.25 ** | 0.20 ** | 0.04 | 0.31 ** | 0.14 ** | 1 | ||
| 8. Global PSQI | 0.60 ** | 0.65 ** | 0.67 ** | 0.57 ** | 0.49 ** | 0.27 ** | 0.53 ** | 1 | |
| Mean | 1.04 | 0.94 | 1.03 | 0.61 | 1.10 | 0.07 | 0.69 | 5.48 | |
| Standard deviation | 0.55 | 0.85 | 0.93 | 0.98 | 0.51 | 0.37 | 0.66 | 2.76 | |
| Median | 1 | 1 | 1 | 0 | 1 | 0 | 1 | 5 | |
| IQR | 1–1 | 0–1 | 0–2 | 0–1 | 1–1 | 0–0 | 0–1 | 4–7 | |
| Timepoint 2 | 1. Subjective sleep quality | 1 | |||||||
| 2. Sleep latency | 0.39 ** | 1 | |||||||
| 3. Sleep duration | 0.21 ** | 0.21 ** | 1 | ||||||
| 4. Habitual sleep efficiency | 0.12 * | 0.23 ** | 0.29 ** | 1 | |||||
| 5. Sleep disturbances | 0.26 ** | 0.40 ** | 0.09 | 0.15 ** | 1 | ||||
| 6. Sleep medication use | 0.14 ** | 0.09 * | 0.01 | −0.01 | 0.13 ** | 1 | |||
| 7. Daytime dysfunction | 0.34 ** | 0.21 ** | 0.16 ** | 0.02 | 0.28 ** | 0.22 ** | 1 | ||
| 8. Global PSQI | 0.58 ** | 0.67 ** | 0.60 ** | 0.60 ** | 0.54 ** | 0.29 ** | 0.53 ** | 1 | |
| Mean | 0.98 | 0.90 | 0.95 | 0.70 | 1.09 | 0.09 | 0.72 | 5.41 | |
| Standard deviation | 0.52 | 0.82 | 0.91 | 1.03 | 0.55 | 0.42 | 0.70 | 2.79 | |
| Median | 1 | 1 | 1 | 0 | 1 | 0 | 1 | 5 | |
| IQR | 1–1 | 0–1 | 0–2 | 0–1 | 1–1 | 0–0 | 0–1 | 3–7 | |
| Timepoint 3 | 1. Subjective sleep quality | 1 | |||||||
| 2. Sleep latency | 0.45 ** | 1 | |||||||
| 3. Sleep duration | 0.32 ** | 0.29 ** | 1 | ||||||
| 4. Habitual sleep efficiency | 0.19 ** | 0.18 ** | 0.26 ** | 1 | |||||
| 5. Sleep disturbances | 0.27 ** | 0.31 ** | 0.17 ** | 0.08 | 1 | ||||
| 6. Sleep medication use | 0.01 | 0.13 * | −0.01 | 0.01 | 0.11 * | 1 | |||
| 7. Daytime dysfunction | 0.41 ** | 0.24 ** | 0.19 ** | 0.06 | 0.26 ** | 0.09 | 1 | ||
| 8. Global PSQI | 0.67 ** | 0.70 ** | 0.65 ** | 0.50 ** | 0.52 ** | 0.24 ** | 0.55 ** | 1 | |
| Mean | 1.01 | 0.86 | 0.97 | 0.42 | 1.08 | 0.09 | 0.64 | 5.08 | |
| Standard deviation | 0.58 | 0.87 | 0.94 | 0.80 | 0.55 | 0.42 | 0.67 | 2.77 | |
| Median | 1 | 1 | 1 | 0 | 1 | 0 | 1 | 5 | |
| IQR | 1–1 | 0–1 | 0–2 | 0–1 | 1–1 | 0–0 | 0–1 | 3–7 |
| PSQI Subscales | Perceived Sleep Quality | Sleep Efficiency |
|---|---|---|
| Timepoint 1 | ||
| Subjective sleep quality | 0.67 b | 0.23 f |
| Sleep latency | 0.69 b | 0.19 f |
| Sleep duration | 0.20 f | 0.79 a |
| Habitual sleep efficiency | −0.02 f | 0.84 a |
| Sleep disturbances | 0.71 a | −0.02 f |
| Sleep medication use | 0.29 f | 0.04 f |
| Daytime dysfunction | 0.67 b | 0.03 f |
| Percentage of total variance, % | 32.1 | 16.7 |
| Timepoint 2 | ||
| Subjective sleep quality | 0.64 b | 0.26 f |
| Sleep latency | 0.55 c | 0.45 d |
| Sleep duration | 0.14 f | 0.68 b |
| Habitual sleep efficiency | 0.01 f | 0.77 a |
| Sleep disturbances | 0.61 c | 0.22 f |
| Sleep medication use | 0.56 c | −0.32 e |
| Daytime dysfunction | 0.71 a | −0.04 f |
| Percentage of total variance, % | 31.6 | 17.2 |
| Timepoint 3 | ||
| Subjective sleep quality | 0.66 b | 0.37 e |
| Sleep latency | 0.68 b | 0.23 f |
| Sleep duration | 0.36 e | 0.63 b |
| Habitual sleep efficiency | 0.12 f | 0.68 b |
| Sleep disturbances | 0.66 b | −0.07f |
| Sleep medication use | 0.42 e | 0.52 d |
| Daytime dysfunction | 0.66 a | 0.02 f |
| Percentage of total variance, % | 32.8 | 15.7 |
| Timepoint | Model | Chi-Square (p-Value) | GFI | AGFI | CFI | TLI | RMSEA | SRMR | CAIC | BIC |
|---|---|---|---|---|---|---|---|---|---|---|
| Timepoint 1 | 1-factor model a | 83.97 (<0.001) | 0.79 | 0.68 | 0.81 | 0.72 | 0.10 | 0.06 | 109.63 | 6335.88 |
| 2-factor model b | 36.61 (<0.001) | 0.91 | 0.85 | 0.94 | 0.90 | 0.06 | 0.03 | 62.28 | 6294.66 | |
| 3-factor model c | 28.46 (0.003) | 0.93 | 0.86 | 0.95 | 0.91 | 0.06 | 0.03 | 54.12 | 6298.79 | |
| Timepoint 2 | 1-factor model a | 67.22 (<0.001) | 0.80 | 0.69 | 0.83 | 0.75 | 0.10 | 0.06 | 92.61 | 5969.28 |
| 2-factor model b | 44.33 (<0.001) | 0.87 | 0.79 | 0.90 | 0.84 | 0.08 | 0.04 | 69.72 | 5952.44 | |
| 3-factor model c | 37.37 (<0.001) | 0.89 | 0.79 | 0.92 | 0.84 | 0.08 | 0.04 | 62.77 | 5957.59 | |
| Timepoint 3 | 1-factor model a | 31.23 (0.005) | 0.89 | 0.83 | 0.93 | 0.90 | 0.06 | 0.04 | 55.85 | 4553.3 |
| 2-factor model b | 21.31 (0.067) | 0.92 | 0.88 | 0.97 | 0.95 | 0.04 | 0.03 | 45.93 | 4549.17 | |
| 3-factor model c | 17.27 (0.100) | 0.94 | 0.88 | 0.98 | 0.95 | 0.04 | 0.03 | 41.89 | 4556.73 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dunleavy, G.; Bajpai, R.; Comiran Tonon, A.; Chua, A.P.; Cheung, K.L.; Soh, C.-K.; Christopoulos, G.; de Vries, H.; Car, J. Examining the Factor Structure of the Pittsburgh Sleep Quality Index in a Multi-Ethnic Working Population in Singapore. Int. J. Environ. Res. Public Health 2019, 16, 4590. https://doi.org/10.3390/ijerph16234590
Dunleavy G, Bajpai R, Comiran Tonon A, Chua AP, Cheung KL, Soh C-K, Christopoulos G, de Vries H, Car J. Examining the Factor Structure of the Pittsburgh Sleep Quality Index in a Multi-Ethnic Working Population in Singapore. International Journal of Environmental Research and Public Health. 2019; 16(23):4590. https://doi.org/10.3390/ijerph16234590
Chicago/Turabian StyleDunleavy, Gerard, Ram Bajpai, André Comiran Tonon, Ai Ping Chua, Kei Long Cheung, Chee-Kiong Soh, Georgios Christopoulos, Hein de Vries, and Josip Car. 2019. "Examining the Factor Structure of the Pittsburgh Sleep Quality Index in a Multi-Ethnic Working Population in Singapore" International Journal of Environmental Research and Public Health 16, no. 23: 4590. https://doi.org/10.3390/ijerph16234590
APA StyleDunleavy, G., Bajpai, R., Comiran Tonon, A., Chua, A. P., Cheung, K. L., Soh, C.-K., Christopoulos, G., de Vries, H., & Car, J. (2019). Examining the Factor Structure of the Pittsburgh Sleep Quality Index in a Multi-Ethnic Working Population in Singapore. International Journal of Environmental Research and Public Health, 16(23), 4590. https://doi.org/10.3390/ijerph16234590






