Illness Perceptions, Self-Care Management, and Clinical Outcomes According to Age-Group in Korean Hemodialysis Patients
Abstract
1. Introduction
2. Materials and Methods
2.1. Design and Ethics
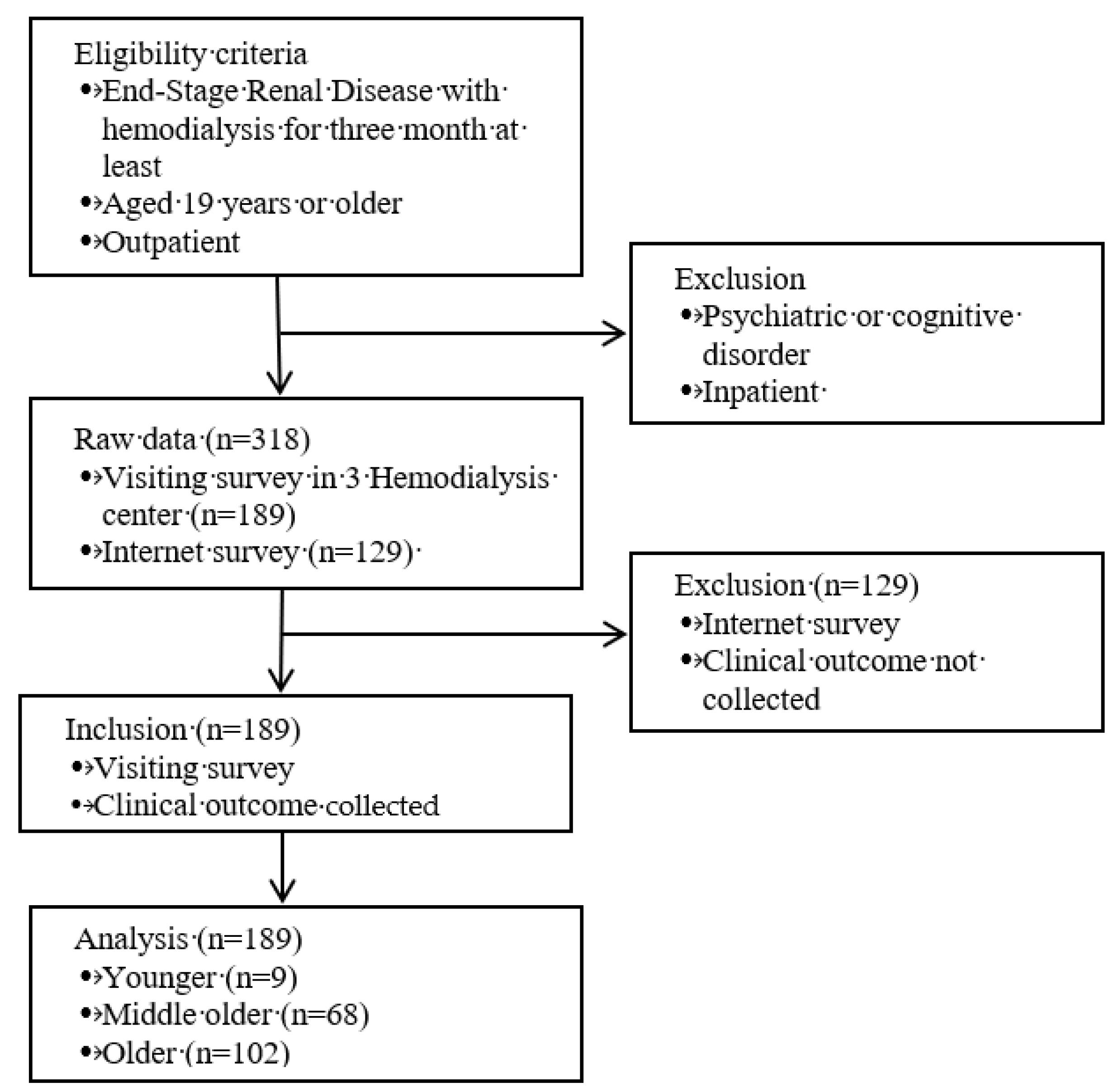
2.2. Participants and Sample Size
2.3. Measures
2.4. Data Analysis
3. Results
3.1. Descriptive Analysis and Difference in Study Variables
3.2. Differences in Study Variables According to Age Group
3.3. Correlations among Illness Perception, Self-Care Management, and Clinical Outcomes according to Age Groups
4. Discussion
5. Limitation
6. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Richard, C.J. Self-care management in adults undergoing hemodialysis. Nephrol. Nurs. J. 2006, 33, 387. [Google Scholar] [PubMed]
- Torre, L.A.; Siegel, R.L.; Ward, E.M.; Jemal, A. Global cancer incidence and mortality rates and trends—An update. Cancer Epidem. Prevent. Biomarkers 2016, 25, 16–27. [Google Scholar] [CrossRef] [PubMed]
- Hecking, M.; Moissl, U.; Genser, B.; Rayner, H.; Dasgupta, I.; Stuard, S.; Stopper, A.; Chazot, C.; Maddux, F.W.; Canaud, B. Greater fluid overload and lower interdialytic weight gain are independently associated with mortality in a large international hemodialysis population. Nephrol. Dial. Transplant. 2018, 33, 1832–1842. [Google Scholar] [CrossRef] [PubMed]
- ESRD Registry Committee, Korean Society of Nephrology. Current Renal Replacement Therapy in Korea. Available online: http://www.ksn.or.kr/rang_board/list.html?code=sinchart (accessed on 19 September 2019).
- Atashpeikar, S.; Jalilazar, T.; Heidarzadeh, M. Self-care ability in hemodialysis patients. J. Caring Sci. 2012, 1, 31. [Google Scholar] [PubMed]
- Leventhal, H.; Leventhal, E.A.; Cameron, L. Representations, procedures, and affect in illness self-regulation: A perceptual-cognitive model. Handb. Health Psychol. 2001, 3, 19–47. [Google Scholar]
- Leventhal, H.; Diefenbach, M.; Leventhal, E.A. Illness cognition: Using common sense to understand treatment adherence and affect cognition interactions. Cogn. Ther. Res. 1992, 16, 143–163. [Google Scholar] [CrossRef]
- Cameron, L.D.; Leventhal, H. The Self-Regulation of Health and Illness Behaviour; Psychology Press: New York, NY, USA, 2003. [Google Scholar]
- Chilcot, J. The importance of illness perception in end-stage renal disease: Associations with psychosocial and clinical outcomes. Semin. Dial. 2012, 25, 159–164. [Google Scholar] [CrossRef]
- Griva, K.; Davenport, A.; Harrison, M.; Newman, S. An evaluation of illness, treatment perceptions, and depression in hospital-vs. home-based dialysis modalities. J. Psychosom. Res. 2010, 69, 363–370. [Google Scholar] [CrossRef]
- Chilcot, J.; Wellsted, D.; Farrington, K. Illness representations are associated with fluid nonadherence among hemodialysis patients. J. Psychosom. Res. 2010, 68, 203–212. [Google Scholar] [CrossRef]
- Leventhal, E.A. Aging and the perception of illness. Res. Aging 1984, 6, 119–135. [Google Scholar] [CrossRef]
- Jansen, D.L.; Heijmans, M.J.; Rijken, M.; Spreeuwenberg, P.; Grootendorst, D.C.; Dekker, F.W.; Boeschoten, E.W.; Kaptein, A.A.; Groenewegen, P.P. Illness perceptions and treatment perceptions of patients with chronic kidney disease: Different phases, different perceptions? Br. J. Health Psychol. 2013, 18, 244–262. [Google Scholar] [CrossRef] [PubMed]
- Kim, S. Self-Regulation In Hemodialysis Patients Using Structure Equation Model. Ph.D. Thesis, The Graduate School of Chung-Ang University, Seoul, Korea, 2018. [Google Scholar]
- Nagai, K.; Matsuura, M.; Tsuchida, K.; Kanayama, H.-O.; Doi, T.; Minakuchi, J. Prognostic factors for mortality in middle-aged and older hemodialysis patients: A 5-year observational study. J. Artif. Organs 2018, 21, 94–101. [Google Scholar] [CrossRef] [PubMed]
- Statistical Research Institute. Korean Social Trends 2018. Available online: http://kostat.go.kr/sri/srikor/srikor_pbl/3/index.board (accessed on 19 September 2019).
- Faul, F.; Erdfelder, E.; Buchner, A.; Lang, A.-G. Statistical power analyses using G* Power 3.1: Tests for correlation and regression analyses. Behav. Res. Methods 2009, 41, 1149–1160. [Google Scholar] [CrossRef] [PubMed]
- Broadbent, E.; Petrie, K.J.; Main, J.; Weinman, J. The brief illness perception questionnaire. J. Psychosom. Res. 2006, 60, 631–637. [Google Scholar] [CrossRef] [PubMed]
- Hibbard, J.H.; Mahoney, E.R.; Stockard, J.; Tusler, M. Development and testing of a short form of the patient activation measure. Health Serv. Res. 2005, 40, 1918–1930. [Google Scholar] [CrossRef] [PubMed]
- Daugirdas, J.T.; Depner, T.A.; Inrig, J.; Mehrotra, R.; Rocco, M.V.; Suri, R.S.; Weiner, D.E.; Greer, N.; Ishani, A.; MacDonald, R. KDOQI clinical practice guideline for hemodialysis adequacy: 2015 update. Am. J. Kidney Dis. 2015, 66, 884–930. [Google Scholar] [CrossRef]
- Pani, A.; Floris, M.; Rosner, M.H.; Ronco, C. Hyperkalemia in hemodialysis patients. Semin. Dial. 2014, 27, 571–576. [Google Scholar] [CrossRef]
- Uhlig, K.; Berns, J.S.; Kestenbaum, B.; Kumar, R.; Leonard, M.B.; Martin, K.J.; Sprague, S.M.; Goldfarb, S. KDOQI US commentary on the 2009 KDIGO clinical practice guideline for the diagnosis, evaluation, and treatment of CKD–mineral and bone disorder (CKD-MBD). Am. J. Kidney Dis. 2010, 55, 773–799. [Google Scholar] [CrossRef]
- Ahrari, S.; Moshki, M.; Bahrami, M. The relationship between social support and adherence of dietary and fluids restrictions among hemodialysis patients in Iran. J. Caring Sci. 2014, 3, 11. [Google Scholar]
- Cupisti, A.; Ferretti, V.; D’Alessandro, C.; Petrone, I.; Di Giorgio, A.; Meola, M.; Panichi, V.; Conti, P.; Lippi, A.; Caprioli, R. Nutritional knowledge in hemodialysis patients and nurses: Focus on phosphorus. J. Ren. Nutr. 2012, 22, 541–546. [Google Scholar] [CrossRef]
- Kim, Y.; Evangelista, L.S. Relationship between illness perceptions, treatment adherence, and clinical outcomes in patients on maintenance hemodialysis. Nephrol. Nurs. J. J. Am. Nephrol. Nurses Assoc. 2010, 37, 271. [Google Scholar]
- Li, H.; Jiang, Y.-F.; Lin, C.-C. Factors associated with self-management by people undergoing hemodialysis: A descriptive study. Int. J. Nurs. Stud. 2014, 51, 208–216. [Google Scholar] [CrossRef] [PubMed]
- Naalweh, K.S.; Barakat, M.A.; Sweileh, M.W.; Al-Jabi, S.W.; Sweileh, W.M.; Sa’ed, H.Z. Treatment adherence and perception in patients on maintenance hemodialysis: A cross–sectional study from Palestine. BMC Nephrol. 2017, 18, 178. [Google Scholar] [CrossRef] [PubMed]
- Nah, R.; Robertson, N.; Niyi-Odumosu, F.A.; Clarke, A.L.; Bishop, N.C.; Smith, A.C. Relationships between illness representations, physical activity and depression in chronic kidney disease. J. Ren. Care 2019. [Google Scholar] [CrossRef]
- Natashia, D.; Yen, M.; Chen, H.M.; Fetzer, S.J. Self-Management Behaviors in Relation to Psychological Factors and Interdialytic Weight Gain Among Patients Undergoing Hemodialysis in Indonesia. J. Nurs. Scholarsh. 2019. [Google Scholar] [CrossRef]
- Sugisawa, H.; Shinoda, T.; Shimizu, Y.; Kumagai, T.; Sugisaki, H. Psychosocial Mediators between Socioeconomic Status and Dietary Restrictions among Patients Receiving Hemodialysis in Japan. Int. J. Nephrol. 2019, 2019. [Google Scholar] [CrossRef]
- Takayama, S.; Fukuno, K.; Ideuchi, H.; Kobayashi, R.; Itoh, T.; Miyakoshi, T.; Sato, H.; Takeda, K.; Kobayashi, M.; Saitoh, H. The Effects of Gender and Age on Serum Calcium and Phosphorus Levels in Hemodialysis Patients. Jpn. J. Nephrol. Pharmacother. 2015, 4, 3–11. [Google Scholar]
- Tohme, F.; Mor, M.K.; Pena-Polanco, J.; Green, J.A.; Fine, M.J.; Palevsky, P.M.; Weisbord, S.D. Predictors and outcomes of non-adherence in patients receiving maintenance hemodialysis. Int. Urol. Nephrol. 2017, 49, 1471–1479. [Google Scholar] [CrossRef]
- Tasmoc, A.; Hogas, S.; Covic, A. A longitudinal study on illness perceptions in hemodialysis patients: Changes over time. Arch. Med. Sci. AMS 2013, 9, 831. [Google Scholar] [CrossRef]
- Leventhal, H.; Meyer, D.; Nerenz, D. The Common Sense Representation of Illness Danger; Pergamon: Oxford, UK, 1980; Volume 2, pp. 7–30. [Google Scholar]
- Nowicka-Sauer, K.; Banaszkiewicz, D.; Staśkiewicz, I.; Kopczyński, P.; Hajduk, A.; Czuszyńska, Z.; Ejdys, M.; Szostakiewicz, M.; Sablińska, A.; Kałużna, A. Illness perception in Polish patients with chronic diseases: Psychometric properties of the Brief Illness Perception Questionnaire. J. Health Psychol. 2016, 21, 1739–1749. [Google Scholar] [CrossRef]
- Hatthakit, U. Lived experiences of patients on hemodialysis: A meta-synthesis. Nephrol. Nurs. J. 2012, 39, 295–304. [Google Scholar]
- Chiaranai, C. The lived experience of patients receiving hemodialysis treatment for end-stage renal disease: A qualitative study. J. Nurs. Res. 2016, 24, 101–108. [Google Scholar] [CrossRef] [PubMed]
- Tu, H.-Y.; Shao, J.-H.; Wu, F.-J.; Chen, S.-H.; Chuang, Y.-H. Stressors and coping strategies of 20–45-year-old hemodialysis patients. Collegian 2014, 21, 185–192. [Google Scholar] [CrossRef] [PubMed]
- Vork, D.L.; Schneekloth, T.D.; Bartley, A.C.; Vaughan, L.E.; Lapid, M.I.; Jowsey-Gregoire, S.G.; El-Zoghby, Z.M.; Herrmann, S.M.; Tran, C.L.; Albright, R.C. Younger Adults Initiating Hemodialysis: Antidepressant Use for Depression Associated With Higher Health Care Utilization. Mayo Clin. Proc. 2018, 93, 321–332. [Google Scholar] [CrossRef]
- Laudański, K.; Nowak, Z.; Niemczyk, S. Age-related differences in the quality of life in end-stage renal disease in patients enrolled in hemodialysis or continuous peritoneal dialysis. Med. Sci. Monit. Int. Med. J. Exp. Clin. Res. 2013, 19, 378. [Google Scholar] [CrossRef]
- Karamanidou, C.; Weinman, J.; Horne, R. A qualitative study of treatment burden among haemodialysis recipients. J. Health Psychol. 2014, 19, 556–569. [Google Scholar] [CrossRef]
- Hornik, B.; Duława, J. Frailty, Quality of Life, Anxiety, and Other Factors Affecting Adherence to Physical Activity Recommendations by Hemodialysis Patients. Int. J. Environ. Res. Public Health 2019, 16, 1827. [Google Scholar] [CrossRef]
- Perl, J.; Karaboyas, A.; Morgenstern, H.; Sen, A.; Rayner, H.C.; Vanholder, R.C.; Combe, C.; Hasegawa, T.; Finkelstein, F.O.; Lopes, A.A. Association between changes in quality of life and mortality in hemodialysis patients: Results from the DOPPS. Nephrol. Dial. Transplant. 2016, 32, 521–527. [Google Scholar] [CrossRef]
| Author (Year of Publication) | Country of Origin | Sample | Age | Association with Age and Variables | Operational Definition | Assessment Based On… |
|---|---|---|---|---|---|---|
| Ahrari et. al. (2014) [23] | Iran | 237 | 46.1 ± 15.4 | ↑ | Frequency and degree of adherence | Diet, fluid, |
| Atashpeikar et al. (2012) [5] | Iran | 115 | 50.2 ± 15.4 | ↑ | Self-care | Vascular access, diet, general care |
| Cupisti et. al. (2012) [24] | Italy | 119 | 62 ± 13 | ↑ | Phosphorus control | Serum phosphorus, phosphorus knowledge |
| Kim and Evangelista (2010) [25] | USA | 151 | 51.9 ± 15.6 | ↑ | Adherence | HD attendance, medication, |
| Li et. al. (2014) [26] | China | 216 | 53.16 ± 12.86 | ↓ | Self-management | Problem solving |
| Naalweh et. al. (2017) [27] | Palestine | 220 | 56.82 ± 14.51 | ↑ | Adherence | Medication, fluid restriction, diet recommendation, behavior |
| Nah et al. (2019) [28] | UK | 70 | 60.1 ± 15.9 | ↓ | Physical activity | Vigorous-moderate-intensity activity; walking and sitting |
| Natashia et. al. (2019) [29] | Indonesia | 145 | 54.7 ± 12.2 | ↑ | Self-management | Self-care |
| Sugisawa et. al. (2019) [30] | Japan | 6644 | 66.5 | ↑ | Dietary Restrictions | self-efficacy for dietary restrictions, dietary restrictions |
| Takayama et. al. (2015) [31] | Japan | 331 | 63.2 | ↑ | Control of calcium and phosphorus | Serum phosphorus and calcium, Prescription of phosphorus binder |
| Tohme et. al. (2017) [32] | USA | 286 | 64 (IQR: 56–73) | ↑ | Adherence | Missed dialysis, abbreviated dialysis |
| Characteristics | Categories | Younger (n = 19) | Middle Older (n = 68) | Older (n = 102) | Fisher’s Exact Test | p |
|---|---|---|---|---|---|---|
| Age, Median (range) | Year | 45.0 (34–49) | 58.0 (50–64) | 73.0 (65–91) | ||
| Gender, n (%) | Male | 10 (52.6) | 42 (61.8) | 57 (55.9) | 0.835 | 0.694 |
| Female | 9 (47.4) | 26 (38.2) | 45 (44.1) | |||
| Education, n (%) | Under elementary | 3 (15.8) | 7 (10.3) | 23 (22.5) | 6.963 | 0.319 |
| Middle school | 3 (15.8) | 21 (30.9) | 23 (22.5) | |||
| High School | 10 (52.6) | 29 (42.6) | 36 (35.4) | |||
| College or higher | 3 (15.8) | 11 (16.2) | 20 (19.6) | |||
| Income, Monthly (1000 KRW), n (%) | <1000 | 10 (52.6) | 29 (42.6) | 54 (52.9) | 5.023 | 0.281 |
| 1000–2000 | 7 (36.9) | 18 (26.5) | 28 (27.5) | |||
| >2000 | 2 (10.5) | 21 (30.9) | 20 (19.6) | |||
| Medical Cost, Monthly (1000 KRW), n (%) | <100 | 8 (42.1) | 21 (30.9) | 15 (14.7) | 10.219 | 0.028 |
| 100–500 | 10 (52.6) | 43 (63.2) | 80 (78.4) | |||
| >500 | 1 (5.3) | 4 (5.9) | 7 (6.9) | |||
| Hemodialysis Period (year), n (%) | <5 | 12 (63.2) | 36 (52.9) | 66 (64.7) | 5.237 | 0.255 |
| 5–10 | 7 (36.8) | 22 (32.4) | 25 (24.5) | |||
| >10 | 0 (0) | 10 (14.7) | 21 (10.8) | |||
| Hypertension, n (%) | Yes | 9 (47.4) | 22 (32.4) | 37 (36.3) | 1.500 | 0.460 |
| No | 10 (52.6) | 46 (67.6) | 65 (63.7) | |||
| Diabetes Meletus, n (%) | Yes | 13 (68.4) | 39 (57.4) | 46 (45.1) | 4.708 | 0.094 |
| No | 6 (31.6) | 29 (42.6) | 56 (54.9) | |||
| Kidney Transplantation History, n (%) | Yes | 0 (0) | 4 (5.9) | 0 (0) | 5.824 | 0.027 |
| No | 19 (100.0) | 64 (94.1) | 102 (100.0) |
| Variables | Younger a | Middle Older b | Older c | H | p | Post Hoc |
|---|---|---|---|---|---|---|
| Illness Perception | 5.40 ± 1.83 | 6.63 ± 1.58 | 6.41 ± 1.36 | 8.764 | 0.013 | a < b |
| Timeline | 6.79 ± 3.19 | 8.04 ± 2.16 | 7.56 ± 2.57 | 2.020 | 0.364 | |
| Treatment Control | 5.89 ± 2.45 | 7.18 ± 2.27 | 7.03 ± 2.50 | 4.027 | 0.134 | |
| Consequence | 5.74 ± 2.75 | 6.78 ± 2.47 | 6.70 ± 2.52 | 2.777 | 0.249 | |
| Concern | 5.37 ± 2.79 | 6.57 ± 2.68 | 6.28 ± 2.67 | 3.064 | 0.216 | |
| Understanding | 5.05 ± 2.01 | 6.43 ± 2.35 | 5.87 ± 2.56 | 5.851 | 0.054 | |
| Identity | 5.00 ± 2.00 | 6.29 ± 2.54 | 5.91 ± 2.45 | 5.173 | 0.075 | |
| Emotion | 4.95 ± 2.01 | 5.54 ± 2.75 | 5.71 ± 2.23 | 2.197 | 0.333 | |
| Personal Control | 4.42 ± 1.74 | 6.21 ± 2.28 | 6.25 ± 2.27 | 11.852 | 0.003 | a < b < c |
| Self-Care Management (transformed to 100) | 55.81 ± 13.53 | 57.84 ± 11.46 | 61.33 ± 14.71 | 4.419 | 0.110 | |
| Believes Active Role Important | 2.97 ± 0.59 | 3.1 ± 0.58 | 3.29 ± 0.57 | 8.007 | 0.018 | |
| Confidence and Knowledge to Take Action | 2.86 ± 0.43 | 2.92 ± 0.39 | 2.99 ± 0.55 | 1.686 | 0.430 | |
| Taking Action | 2.76 ± 0.57 | 2.85 ± 0.5 | 2.96 ± 0.59 | 2.558 | 0.278 | |
| Staying the Course under Stress | 2.53 ± 0.56 | 2.71 ± 0.57 | 2.91 ± 0.66 | 9.124 | 0.010 | a < c |
| Clinical Outcomes | ||||||
| Phosphorus (mg/dl) | 5.96 ± 1.89 | 5.32 ± 1.32 | 4.67 ± 1.48 | 15.957 | 0.000 | a > b > c |
| Potassium (Eq/L) | 5.12 ± 1.43 | 4.78 ± 0.84 | 4.51 ± 0.77 | 7.075 | 0.029 | |
| Hemoglobin (g/dl) | 10.74 ± 3.16 | 10.45 ± 0.99 | 10.81 ± 1.42 | 1.663 | 0.435 | |
| Albumin (g/dl) | 4.02 ± 0.57 | 3.94 ± 0.39 | 3.86 ± 0.52 | 4.578 | 0.101 |
| Variable | Univariate Correlation | Adjusted for Age Group | ||
|---|---|---|---|---|
| Age Groups | Illness Perception | Age Groups | Illness Perception | |
| Self-Care Management | 0.148(.043) | 0.282(0.000) | - | 0.268(0.000) |
| Phosphorus (mg/dl) | −0.284(.000) | −0.257(0.000) | - | −0.233(0.001) |
| Potassium (Eq/L) | −0.223(.002) | 0.208(0.004) | - | 0.244(0.001) |
| Hemoglobin (g/dl) | 0.063(.393) | 0.147(0.045) | - | 0.140(0.056) |
| Albumin (g/dl) | −0.107(.146) | 0.011(0.884) | - | 0.024(0.741) |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, S.; Kim, E.; Ryu, E. Illness Perceptions, Self-Care Management, and Clinical Outcomes According to Age-Group in Korean Hemodialysis Patients. Int. J. Environ. Res. Public Health 2019, 16, 4459. https://doi.org/10.3390/ijerph16224459
Kim S, Kim E, Ryu E. Illness Perceptions, Self-Care Management, and Clinical Outcomes According to Age-Group in Korean Hemodialysis Patients. International Journal of Environmental Research and Public Health. 2019; 16(22):4459. https://doi.org/10.3390/ijerph16224459
Chicago/Turabian StyleKim, Sisook, Eunhye Kim, and Eunjung Ryu. 2019. "Illness Perceptions, Self-Care Management, and Clinical Outcomes According to Age-Group in Korean Hemodialysis Patients" International Journal of Environmental Research and Public Health 16, no. 22: 4459. https://doi.org/10.3390/ijerph16224459
APA StyleKim, S., Kim, E., & Ryu, E. (2019). Illness Perceptions, Self-Care Management, and Clinical Outcomes According to Age-Group in Korean Hemodialysis Patients. International Journal of Environmental Research and Public Health, 16(22), 4459. https://doi.org/10.3390/ijerph16224459





