Analyzing Awareness on Risk Factors, Barriers and Prevention of Cervical Cancer among Pairs of Nepali High School Students and Their Mothers
Abstract
1. Introduction
2. Materials and Methods
2.1. Data Collection
2.2. Questionnaire
2.3. Statistical Analyses
2.4. Ethical Considerations
3. Results
3.1. Demographic Information
3.1.1. Students
3.1.2. Mothers
3.2. Knowledge on Risk Factors of Cervical Cancer
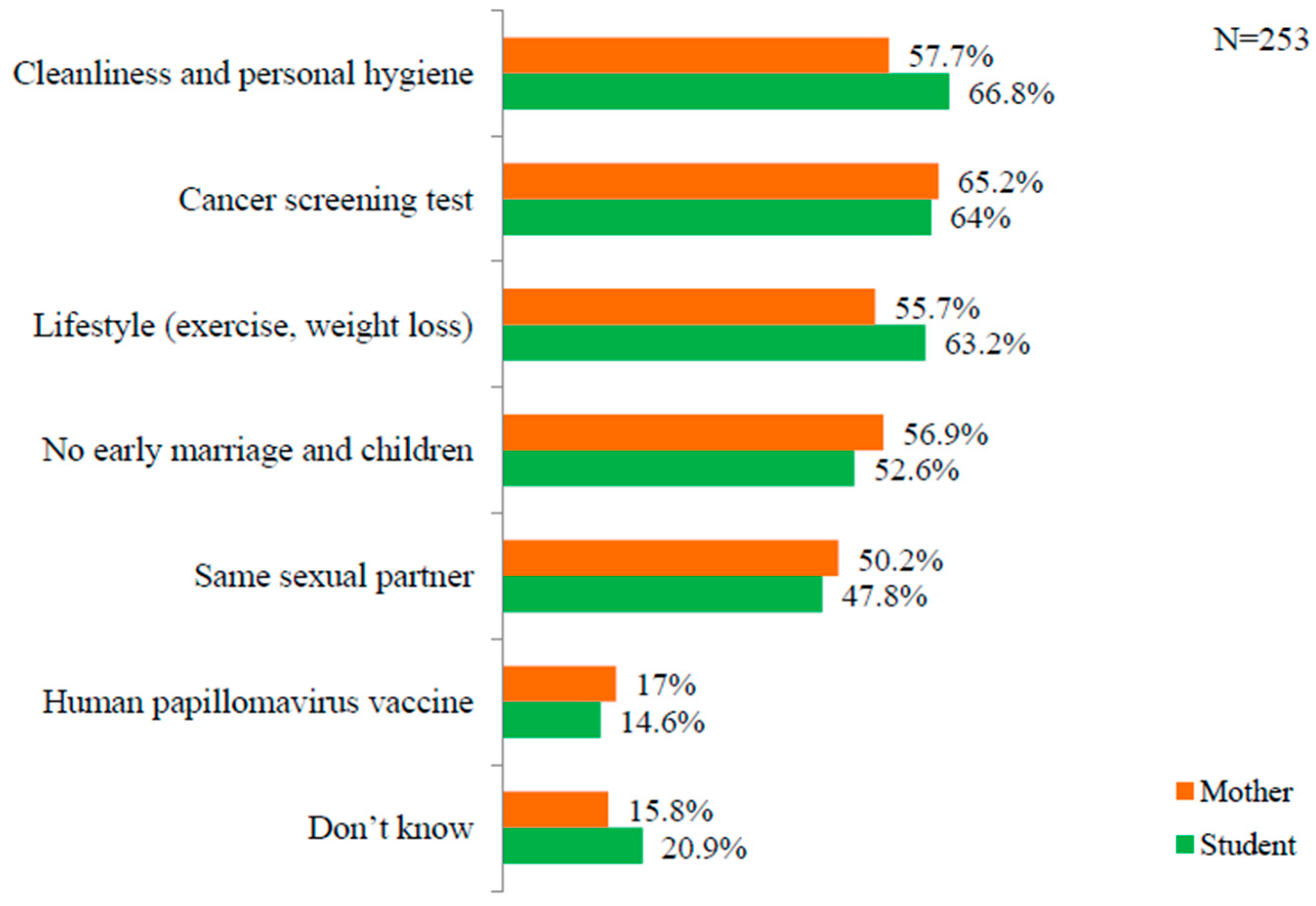
3.3. Knowledge on Prevention of Cervical Cancer
3.4. Total Cervical Cancer Knowledge Score
3.4.1. Students
3.4.2. Mothers
4. Discussion
4.1. Student’s Knowledge and Opinion
4.2. Mothers’ Knowledge and Opinions
4.3. Clinical and Educative Implication
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- WHO. Cervical Cancer, Cancer. 2018. Available online: http://www.who.int/cancer/prevention/diagnosis-screening/cervical-cancer/en/ (accessed on 23 October 2019).
- WHO. Cancer Country Profile: Nepal. 2018. Available online: http://www.who.int/cancer/country-profiles/npl_en.pdf (accessed on 23 October 2019).
- Nepal Network for Cancer Treatment & Research (NNCTR). Cervical and Breast Cancer Screening Activities in Nepal. 2010. Available online: https://www.globalgiving.org/pfil/6686/projdoc.pdf (accessed on 10 March 2019).
- Bruni, L.; Albero, G.; Serrano, B.; Mena, M.; Gomez, D.; Munoz, J.; Bosch, F.X.; de Sanjose, S. Papillomavirus and Related Diseases in Nepal; Summary Report; Human ICO/IARC Information Centre on HPV and Cancer (HPV Information Centre): Geneva, Switzerland, 17 June 2019; Available online: https://hpvcentre.net/statistics/reports/NPL.pdf (accessed on 28 October 2019).
- Gyawali, B.; Keeling, J.; Teijlingen, E.; Dhakal, L.; Aro, A.R. Cervical cancer screening in Nepal: Ethical considerations. Med. Bioeth. 2015, 5, 1–6. [Google Scholar] [CrossRef]
- Johnson, D.C.; Bhatta, M.P.; Smith, J.S.; Kempf, M.C.; Boker, T.R.; Vermund, S.H.; Chamot, E.; Aryal, S.; Lhaki, P.; Shrestha, S. Assessment of high-risk human papillomavirus infections using clinician- and self-collected cervical sampling methods in rural women from far western Nepal. PLoS ONE 2014, 9, e101255. [Google Scholar] [CrossRef]
- Joshi, M.; Mishra, S.R. Cervical cancer screening in Nepal. J. Public Health 2013, 12, 18–20. [Google Scholar] [CrossRef]
- WHO. Screening for Cervical Cancer, Cancer. 2019. Available online: https://www.who.int/cancer/ detection/cervical_cancer_screening/en/ (accessed on 23 October 2019).
- Seng, L.M.; Rosman, A.N.; Khan, A.; Haris, N.M.; Mustapha, N.A.S.; Husaini, N.S.M.; Zahari, N.F. Awareness of cervical cancer among women in Malaysia. Int. J. Health Sci. 2018, 12, 42–48. [Google Scholar]
- American Cancer Society. What are the Risk Factors for Cervical Cancer? 2019. Available online: https://www.cancer.org/cancer/cervical-cancer/causes-risks-prevention/risk-factors.html (accessed on 29 October 2019).
- Darj, E.; Chalise, P.; Shakya, S. Barriers and facilitators to cervical cancer screening in Nepal: A qualitative study. Sex. Repro Healthc. 2019, 20, 20–26. [Google Scholar] [CrossRef] [PubMed]
- Yamaguchi, N.; Tsukamoto, Y.; Shimoyama, H.; Nakayama, K.; Misawa, S. Effects of peer education interventions aimed at changing awareness of cervical cancer in nursing students. Niigata J. Health Welf. 2011, 11, 32–42. [Google Scholar]
- UNICEF. Ending child marriage in Nepal. 2018. Available online: https://www.unicef.org/rosa/media/151/file (accessed on 10 December 2018).
- Kyle, R.G.; Nicoll, A.; Forbat, L.; Hubbard, G. Adolescents’ awareness of cancer risk factors and associations with health-related behaviors. Health Educ. Res. 2013, 28, 816–827. [Google Scholar] [CrossRef] [PubMed]
- Central Bureau of Statistics, Government of Nepal. National Population and Housing Census (National Report). 2011. Available online: https://unstats.un.org/unsd/demographic-social/census/documents/Nepal/Nepal-Census-2011-Vol1.pdf (accessed on 29 October 2019).
- Rashid, S.; Labani, S.; Das, B.C. Knowledge, awareness and attitude on HPV, HPV vaccine and cervical cancer among college students in India. PLoS ONE 2016, 11, e0166713. [Google Scholar] [CrossRef] [PubMed]
- Takata, T.E.; Ueda, Y.; Morimoto, A.; Yoshino, K.; Kimura, T.; Nishikawa, N.; Sekine, M.; Horikoshi, Y.; Takagi, T.; Enomoto, T. Survey of Japanese mothers of daughters eligible for human papillomavirus vaccination on attitudes about media and reports of adverse events and the suspension of governmental recommendation for vaccination. J. Obstet. Gynaecol. Res. 2015, 41, 1965–1971. [Google Scholar] [CrossRef]
- Sawada, M.; Ueda, Y.; Yagi, A.; Morimoto, A.; Nakae, R.; Kakubari, R.; Abe, H.; Takata, T.E.; Iwamiya, T.; Matsuzaki, S.; et al. HPV vaccination in Japan: Results of a 3 year follow up survey of obstetricians and gynecologists regarding their opinions toward the vaccine. Int. J. Clin. Oncol. 2018, 23, 121–125. [Google Scholar] [CrossRef]
- Chang, S.C.H.; Woo, J.S.T.; Gorzalka, B.B.; Brotto, L.A. A questionnaire study of cervical cancer screening beliefs and practices of chinese and caucasian mother- daughter pairs living in Canada. J. Obstet. Gynaecol. Can. 2010, 32, 254–262. [Google Scholar] [CrossRef]
- Turner, L.W.; Hunt, S.B.; Dibrezzo, R.O.; Jones, C. Design and implementation of an osteoporosis prevention program using the health belief model. Am. J. Health Stud. 2004, 19, 15. [Google Scholar]
- Janz, N.K.; Becker, M.H. The Health Belief Model: A decade later. Health Educ. Q. 1984, 11, 1–17. [Google Scholar] [CrossRef] [PubMed]
- Jaglarz, K.; Tomaszewski, K.A.; Kamzol, W.; Puskulluoglu, M.; Krzemieniecki, K. Creating and field testing the questionnaire for the assessment of knowledge about cervical cancer and its prevention among schoolgirls and female students. J. Gynaecol Oncol. 2014, 25, 81–89. [Google Scholar] [CrossRef] [PubMed]
- Mulatu, K.; Motma, A.; Seid, M.; Tadesse, M. Assessment of knowledge, attitude and practice on cervical cancer screening among female students of Mizan Tepi University. Cancer Biol. Ther. Oncol. 2017, 1, 1–6. [Google Scholar]
- Adhikari, R.; Tamang, J. Premarital sexual behavior among male college students of Kathmandu, Nepal. BMC Public Health 2009, 9, 241. [Google Scholar] [CrossRef]
- Sugisaki, K.; Ueda, S.; Monobe, H.; Suketomo, H.Y.; Eto, T.; Waanabe, M.; Mori, R. Cancer understanding among Japanese students based on a national wide survey. Environ. Health Prev. Med. 2014, 19, 395. [Google Scholar] [CrossRef][Green Version]
- Singh, Y.; Vaidya, P. Human Papilloma virus vaccination in Nepal. Asian Pac. J. Cancer Prev. 2010, 11, 615–617. [Google Scholar]
- Mouallif, M.; Bowyer, H.; Festali, S.; Albert, A.; Filali, Y.; Guenin, S.; Delvenne, P.; Waller, J.; Ennaji, M. Primary cervical cancer prevention in Morocco: HPV vaccine awareness and acceptability among parents. Procedia Vaccinol. 2014, 8, 68–76. [Google Scholar] [CrossRef][Green Version]
- Ministry of Finance, Government of Nepal. Budget Speech of Fiscal Year 2019/2020. Available online: https://mof.gov.np/uploads/document/file/budget_speech_website_20190619052055.pdf (accessed on 10 August 2019).
- Hardcastle, S.J.; Hancox, J.; Hattar, A.; Maxwell- Smith, C.; Ntoumani, C.T.; Hagger, M.S. Motivating the unmotivated: How can health behavior be changed in those unwilling to change? Front. Psychol. 2015, 6, 835. [Google Scholar] [CrossRef]
- Pitts, M.K.; Dyson, S.J.; Rosenthal, D.A.; Garland, S.M. Knowledge and awareness of human papillomavirus: Attitudes towards HPV vaccination among a representative sample of women in Victoria, Australia. Sex. Health 2007, 4, 177–180. [Google Scholar] [CrossRef]
- Rosser, J.; Zakaras, J.M.; Hamisi, S.; Huchko, M.J. Men’s knowledge and attitudes about cervical cancer screening in Kenya. BMC Women’s Health 2014, 14, 138. [Google Scholar] [CrossRef]
- Liu, T.; Li, S.; Ratcliffe, J.; Chen, G. Assessing knowledge and attitudes towards cervical cancer screening among rural women in eastern china. Int. J. Environ. Res. Public Health 2017, 14, 967. [Google Scholar] [CrossRef]
- Pandey, R.A.; Karmacharya, E. Cervical cancer screening behavior and associated factors among women of Ugrachandi Nala, Kavre, Nepal. Eur. J. Med. Res. 2017, 22, 32. [Google Scholar] [CrossRef]
- Poudel, K.; Sumi, N. Health behavior regarding Cardiovascular Diseases among Nepali adults. J. Community Health 2017, 42, 1240–1246. [Google Scholar] [CrossRef]
- Shrestha, S.; Saha, R.; Tripathi, N. Knowledge, attitude and practice regarding cervical cancer screening amongst women visiting tertiary center in Kathmandu, Nepal. Nep. J. Med. Sci. 2013, 2, 2. [Google Scholar] [CrossRef]
- Ranjit, A.; Gupta, S.; Shrestha, R.; Kushner, A.L.; Nwomeh, B.C.; Groen, R.S. Awareness and prevalence of cervical cancer screening among women in Nepal. Int. J. Gynecol. Obstet. 2016, 134, 37–40. [Google Scholar] [CrossRef]
- WHO. Prevention of Cervical Cancer through Screening Visual Inspection with Acetic Acid (VIA) and Treatment with Cryotherapy. 2012. Available online: http://www.who.int/reproductivehealth/publications/cancers/9789241503860/en/ (accessed on 3 January 2019).
- WHO. Comprehensive Cervical Cancer Prevention and Control: A Healthier Future for Girls and women. 2013. Available online: https://apps.who.int/iris/bitstream/handle/10665/78128/9789241505147_eng.pdf;jsessionid=79B630E91CD70A0714AB076D4CEB7DB6?sequence=3 (accessed on 29 October 2019).
- Thapa, N.; Maharjan, M.; Petrini, M.A.; Shah, R.; Shah, S.; Maharjan, N.; Shrestha, N.; Cai, H. Knowledge, attitude, practice and barriers of cervical cancer screening among women living in mid- western rural, Nepal. J. Gynecol. Oncol. 2018, 29, 4. [Google Scholar] [CrossRef]
- Navarro, A.M.; Raman, R.; McNicholas, L.J.; Loza, O. Diffusion of cancer education information through a Latino Community Health Advisor Program. Prev. Med. 2007, 45, 135–138. [Google Scholar] [CrossRef][Green Version]
- Poudel, K.; Sumi, N. Knowledge about risk factors for cancer among adults in Nepal. KnE Life Sci. 2018, 4, 126–136. [Google Scholar] [CrossRef]
- Ncube, B.; Bey, A.; Knight, J.; Bessler, P.; Jolly, P.E. Factors associated with the uptake of cervical cancer screening among women in Portland, Jamaica. N. Am. J. Med. Sci. 2015, 7, 104–113. [Google Scholar] [CrossRef]
- Mishra, S.R.; Khanal, P.; Karki, D.K.; Kallestrup, P.; Enemark, U. National health insurance policy in Nepal: Challenges for implementation. Glob. Health Action 2015, 8, 28763. [Google Scholar] [CrossRef]
- Tapera, R.; Manyala, E.; Erick, P.; Maswabi, T.M.; Tumoyagae, T.; Mbongwe, B.; Letsholo, B. Knowledge and Attitudes towards Cervical cancer screening amongst University of Botswana female students. Asian Pac. J. Cancer Prev. 2017, 18, 2445–2450. [Google Scholar] [CrossRef]
- McLeroy, K.R.; Bibeau, D.; Steckler, A.; Glanz, K. An ecological perspective on health promotion programs. Health Educ. Q. 1988, 15, 351–377. [Google Scholar] [CrossRef]

| Variables | Category (N) | Mean ± Standard Deviation | p-Value |
|---|---|---|---|
| Sex | Male (125) | 10.4 ± 5.2 | 0.01 |
| Female (128) | 11.9 ± 3.9 | ||
| Education Level | Grade 9 (137) | 10.5 ± 4.7 | 0.02 |
| Grade 10 (116) | 11.8 ± 4.3 | ||
| Area of Residence | Rural (79) | 10.4 ± 5.0 | 0.10 |
| Urban (174) | 11.4 ± 4.5 | ||
| Healthy Diet Consumption Per Week | Not much (30) | 8.9 ± 5.5 | 0.00 |
| Sometimes (76) | 11.0 ± 4.9 | ||
| 3 to 4 times (106) | 11.9 ± 3.8 | ||
| Every day (41) | 11.9 ± 4.9 | ||
| Family History of Illness | No (197) | 11.1 ± 4.6 | 0.88 |
| Yes (56) | 11.2 ± 4.8 | ||
| Cancer Talk with Others | No (187) | 10.6 ± 4.9 | 0.00 |
| Yes (66) | 12.6 ± 3.4 | ||
| Mother’s Age during Marriage | Before 20 years (164) | 10.9 ± 4.6 | 0.31 |
| After 20 years (89) | 11.6 ± 4.6 | ||
| Mother’s Cancer Screening Practice | No (215) | 10.7 ± 5.2 | 0.56 |
| Yes (38) | 11.4 ± 4.6 |
| Variables | B | β | p-Value |
|---|---|---|---|
| Sex a | 1.45 | 0.16 | 0.01 |
| Cancer Talk with Others b | 2.01 | 0.19 | 0.00 |
| Education Level c | 1.49 | 0.19 | 0.01 |
| Healthy Diet Consumption d | 0.65 | 0.13 | 0.04 |
| Variables | Category (N) | Mean ± SD | p-Value |
|---|---|---|---|
| Age | Less than 49 years (225) | 10.2 ± 4.9 | 0.43 |
| Above 49 years (28) | 11.0 ± 3.8 | ||
| Education Level | Illiterate (104) | 9.9 ± 5.5 | 0.00 |
| Up to grade 8 (39) | 8.9 ± 4.4 | ||
| Up to grade 12 (86) | 11.5 ± 3.7 | ||
| University and above (24) | 13.2 ± 3.1 | ||
| Number of Children | Less than 3 (177) | 10.5 ± 4.7 | 0.51 |
| More than 3 (76) | 10.0 ± 4.9 | ||
| Area of Residence | Rural (79) | 9.0 ± 5.2 | 0.00 |
| Urban (174) | 10.9 ± 4.5 | ||
| Smoking Habit | No (226) | 10.3 ± 4.8 | 0.96 |
| Yes (27) | 10.3 ± 4.9 | ||
| Drinking Habit | No (194) | 10.3 ± 5.0 | 0.89 |
| Yes (59) | 10.4 ± 3.9 | ||
| Family History of Illness | No (178) | 10.4 ± 4.6 | 0.84 |
| Yes (51) | 10.5 ± 5.1 | ||
| Exercise Habit Per Week | No (200) | 9.8 ± 4.9 | 0.00 |
| Sometimes (18) | 11.6 ± 3.5 | ||
| 3 to 4 times (9) | 11.9 ± 3.4 | ||
| Every day (26) | 13.2 ± 3.3 | ||
| Healthy Diet Consumption | No (24) | 8.9 ± 4.1 | 0.08 |
| Yes (229) | 10.5 ± 4.8 | ||
| Cancer Screening Habit | No (215) | 9.9 ± 4.9 | 0.01 |
| Yes (38) | 12.8 ± 3.0 | ||
| Talk on Cancer | No (152) | 9.8 ± 5.0 | 0.02 |
| Yes (101) | 11.2 ± 4.2 | ||
| Age during Marriage | Before 20 years (164) | 9.8 ± 5.0 | 0.01 |
| After 20 years (89) | 11.4 ± 4.2 | ||
| Sex of Children | Male (125) | 9.3 ± 4.2 | 0.05 |
| Female (128) | 10.9 ± 4.5 |
| Variables | B | β | p-Value |
|---|---|---|---|
| Area of Residence a | 1.29 | 0.13 | 0.04 |
| Exercise Habit b | 0.80 | 0.16 | 0.01 |
| Talk on Cancer c | 0.33 | 0.03 | 0.58 |
| Age during Marriage d | 0.70 | 0.07 | 0.26 |
| Sex of Children e | 1.07 | 0.11 | 0.06 |
| Cancer Screening Habit f | 2.23 | 0.17 | 0.01 |
| Education Level g | 0.66 | 0.15 | 0.03 |
| SN | Barriers | Category (N) | Mean ± SD | p-Value |
|---|---|---|---|---|
| 1 | I have low risk of cervical cancer. | No (67) | 12.1 ± 4.1 | 0.00 |
| Yes (186) | 9.7 ± 4.8 | |||
| 2 | I will get stressed after finding the result of cancer screening. | No (242) | 12.7 ± 4.5 | 0.08 |
| Yes (11) | 10.2 ± 4.7 | |||
| 3 | Screening is not necessary since there is no certainty of cancer. | No (238) | 11.1 ± 4.9 | 0.54 |
| Yes (15) | 10.3 ± 4.7 | |||
| 4 | Screening test is expensive. | No (247) | 11.7 ± 4.0 | 0.28 |
| Yes (6) | 10.3 ± 4.7 | |||
| 5 | I don’t know where to go for screening. | No (214) | 10.5 ± 4.7 | 0.09 |
| Yes (39) | 9.1 ± 5.1 | |||
| 6 | I don’t have time to go for screening. | No (240) | 10.5 ± 4.8 | 0.04 |
| Yes (13) | 7.7 ± 5.3 | |||
| 7 | I don’t have much information about screening. | No (122) | 11.6 ± 4.2 | 0.00 |
| Yes (131) | 9.2 ± 4.9 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Poudel, K.; Sumi, N. Analyzing Awareness on Risk Factors, Barriers and Prevention of Cervical Cancer among Pairs of Nepali High School Students and Their Mothers. Int. J. Environ. Res. Public Health 2019, 16, 4382. https://doi.org/10.3390/ijerph16224382
Poudel K, Sumi N. Analyzing Awareness on Risk Factors, Barriers and Prevention of Cervical Cancer among Pairs of Nepali High School Students and Their Mothers. International Journal of Environmental Research and Public Health. 2019; 16(22):4382. https://doi.org/10.3390/ijerph16224382
Chicago/Turabian StylePoudel, Kritika, and Naomi Sumi. 2019. "Analyzing Awareness on Risk Factors, Barriers and Prevention of Cervical Cancer among Pairs of Nepali High School Students and Their Mothers" International Journal of Environmental Research and Public Health 16, no. 22: 4382. https://doi.org/10.3390/ijerph16224382
APA StylePoudel, K., & Sumi, N. (2019). Analyzing Awareness on Risk Factors, Barriers and Prevention of Cervical Cancer among Pairs of Nepali High School Students and Their Mothers. International Journal of Environmental Research and Public Health, 16(22), 4382. https://doi.org/10.3390/ijerph16224382






