Heat Health Prevention Measures and Adaptation in Older Populations—A Systematic Review
Abstract
1. Introduction
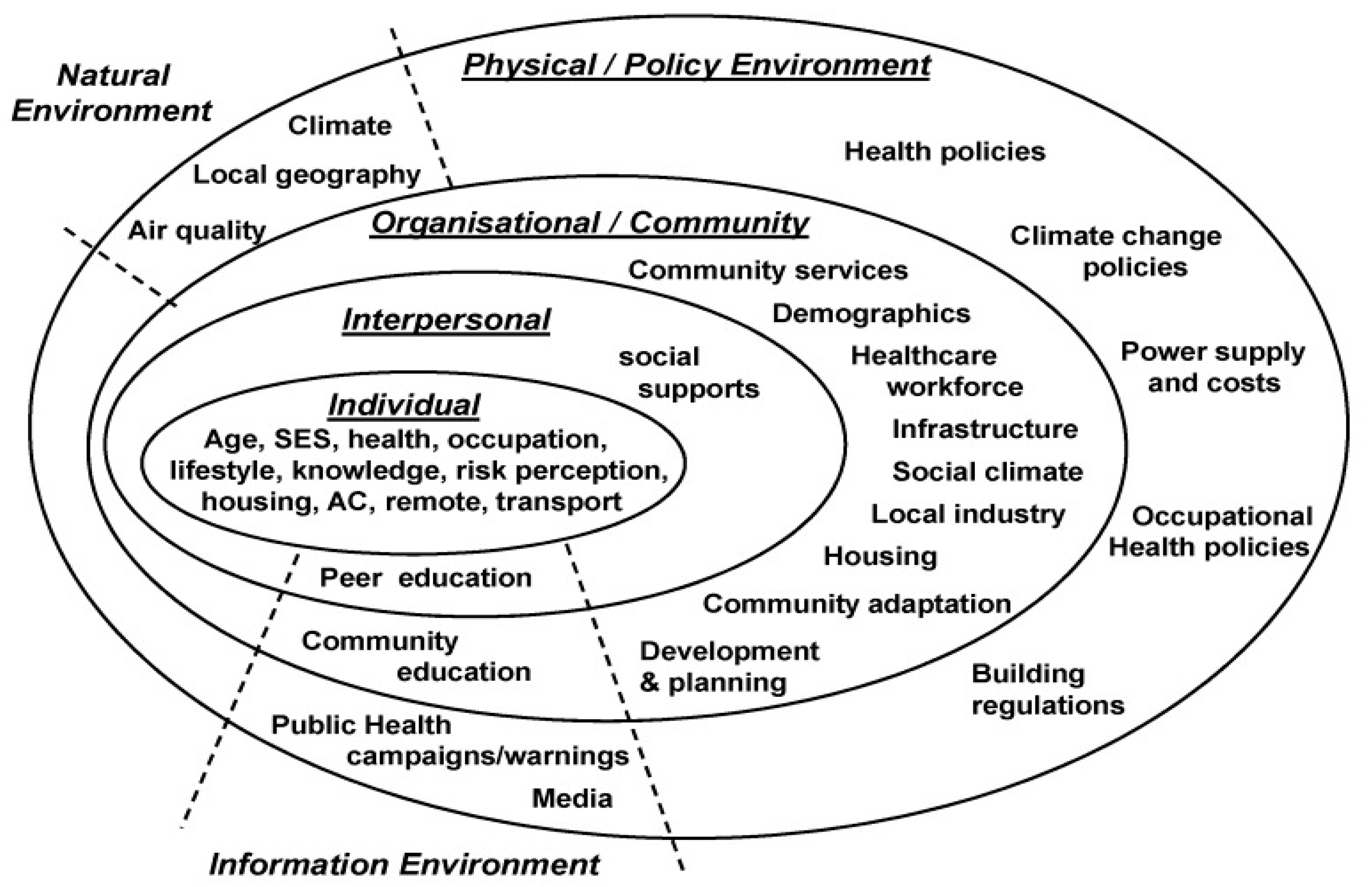
Ottawa Charter for Health Promotion Framework
2. Methods
2.1. Specifications for Systematic Review
2.2. Search Strategy
2.3. Inclusion and Exclusion Criteria
2.4. Quality Assessment
2.5. Data Analysis and Synthesis
3. Results
3.1. Study Characteristics
3.2. Heat Warning Systems and Heat Action Plans
3.3. Risk Factors Awareness, Perception of Vulnerability, and Protective Behaviors
3.4. Effectiveness and Limitations of Heat Action Plans
4. Discussion
4.1. Ottawa Charter Action Areas
4.1.1. Build Healthy Public Policy
4.1.2. Create Supportive Environments
4.1.3. Strengthen Community Actions
4.1.4. Develop Personal Skills
4.1.5. Reorient Health Services
4.1.6. Interrelatedness of Action Areas
4.2. Limitations
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- IPCC. 2018: Summary for Policymakers. In Global Warming of 1.5°C; An IPCC Special Report on the Impacts of Global Warming of 1.5 °C above Pre-Industrial Levels and Related Global Greenhouse Gas Emission Pathways, in the Context of Strengthening the Global Response to the Threat of Climate Change, Sustainable Development, and Efforts to Eradicate Poverty; Masson-Delmotte, V., Zhai, P., Pörtner, H.O., Roberts, D., Skea, J., Shukla, P.R., Pirani, A., Moufouma-Okia, W., Péan, C., Pidcock, R., et al., Eds.; World Meteorological Organization: Geneva, Switzerland, 2018; p. 32. [Google Scholar]
- Semenza, J.C. Climate Change and Human Health. Int. J. Environ. Res. Public Health 2014, 11, 7347–7353. [Google Scholar] [CrossRef] [PubMed]
- Semenza, J.C.; Rubin, C.H.; Falter, K.H.; Selanikio, J.D.; Flanders, W.D.; Howe, H.L.; Wilhelm, J.L. Heat-related deaths during the July 1995 heat wave in Chicago. N. Engl. J. Med. 1996, 335, 84–90. [Google Scholar] [CrossRef]
- Whitman, S.; Good, G.; Donoghue, E.R.; Benbow, N.; Shou, W.; Mou, S. Mortality in Chicago attributed to the July 1995 heat wave. Am. J. Public Health 1997, 87, 1515–1518. [Google Scholar] [CrossRef]
- Fouillet, A.; Rey, G.; Laurent, F.; Pavillon, G.; Bellec, S.; Guihenneuc-Jouyaux, C.; Clavel, J.; Jougla, E.; Hémon, D. Excess mortality related to the August 2003 heat wave in France. Int. Arch. Occup. Environ. Health 2006, 80, 16–24. [Google Scholar] [CrossRef]
- Robine, J.-M.; Cheung, S.L.K.; Le Roy, S.; Van Oyen, H.; Griffiths, C.; Michel, J.-P.; Herrmann, F.R. Death toll exceeded 70,000 in Europe during the summer of 2003. C. R. Biol. 2008, 331, 171–178. [Google Scholar] [CrossRef]
- Shaposhnikov, D.; Revich, B.; Bellander, T.; Bedada, G.B.; Bottai, M.; Kharkova, T.; Kvasha, E.; Lezina, E.; Lind, T.; Semutnikova, E.; et al. Mortality Related to Air Pollution with the Moscow Heat Wave and Wildfire of 2010. Epidemiology 2014, 25, 359–364. [Google Scholar] [CrossRef]
- Perkins-Kirkpatrick, S.E.; White, C.J.; Alexander, L.V.; Argüeso, D.; Boschat, G.; Cowan, T.; Evans, J.P.; Ekström, M.; Oliver, E.C.J.; Phatak, A.; et al. Natural hazards in Australia: Heatwaves. Clim. Chang. 2016, 139, 101–114. [Google Scholar] [CrossRef]
- Oudin Åström, D.; Schifano, P.; Asta, F.; Lallo, A.; Michelozzi, P.; Rocklöv, J.; Forsberg, B. The effect of heat waves on mortality in susceptible groups: A cohort study of a mediterranean and a northern European City. Environ. Health 2015, 14, 30. [Google Scholar] [CrossRef] [PubMed]
- Oudin Åström, D.; Bertil, F.; Joacim, R. Heat wave impact on morbidity and mortality in the elderly population: A review of recent studies. Maturitas 2011, 69, 99–105. [Google Scholar] [CrossRef] [PubMed]
- Leyva, E.W.A.; Beaman, A.; Davidson, P.M. Health Impact of Climate Change in Older People: An Integrative Review and Implications for Nursing: Climate Change, Ageing, and Nursing. J. Nurs. Scholarsh. 2017, 49, 670–678. [Google Scholar] [CrossRef]
- Arbuthnott, K.G.; Hajat, S. The health effects of hotter summers and heat waves in the population of the United Kingdom: A review of the evidence. Environ. Health 2017, 16, 119. [Google Scholar] [CrossRef]
- Kenny, G.P.; Yardley, J.; Brown, C.; Sigal, R.J.; Jay, O. Heat stress in older individuals and patients with common chronic diseases. CMAJ 2010, 182, 1053–1060. [Google Scholar] [CrossRef]
- Cheng, J.; Xu, Z.; Bambrick, H.; Su, H.; Tong, S.; Hu, W. Heatwave and elderly mortality: An evaluation of death burden and health costs considering short-term mortality displacement. Environ. Int. 2018, 115, 334–342. [Google Scholar] [CrossRef] [PubMed]
- Yu, W.; Mengersen, K.; Wang, X.; Ye, X.; Guo, Y.; Pan, X.; Tong, S. Daily average temperature and mortality among the elderly: A meta-analysis and systematic review of epidemiological evidence. Int. J. Biometeorol. 2012, 56, 569–581. [Google Scholar] [CrossRef]
- Jeyakumaran, N.; Gabb, G.; Rowett, D.; Tadros, R. Cardiovascular Disease, Medications and Heat: What Precautionary Advice is Available? Heart Lung Circ. 2016, 25, S317. [Google Scholar] [CrossRef]
- Bunker, A.; Wildenhain, J.; Vandenbergh, A.; Henschke, N.; Rocklöv, J.; Hajat, S.; Sauerborn, R. Effects of Air Temperature on Climate-Sensitive Mortality and Morbidity Outcomes in the Elderly; a Systematic Review and Meta-analysis of Epidemiological Evidence. EBioMedicine 2016, 6, 258–268. [Google Scholar] [CrossRef] [PubMed]
- United Nations, Department of Economic and Social Affairs, Population Division. World Population Ageing 2017—Highlights (ST/ESA/SER.A/397). 2017. Available online: https://www.un.org/en/development/desa/population/publications/pdf/ageing/WPA2017_Highlights.pdf (accessed on 30 August 2019).
- United Nations, Department of Economic and Social Affairs, Population Division. World Population Prospects 2019: Highlights (ST/ESA/SER.A/423). 2019. Available online: https://population.un.org/wpp/Publications/Files/WPP2019_10KeyFindings.pdf (accessed on 30 August 2019).
- Reid, C.E.; O’Neill, M.S.; Gronlund, C.J.; Brines, S.J.; Brown, D.G.; Diez-Roux, A.V.; Schwartz, J. Mapping community determinants of heat vulnerability. Environ. Health Perspect. 2009, 117, 1730–1736. [Google Scholar] [CrossRef]
- Curriero, F.C.; Heiner, K.S.; Samet, J.M.; Zeger, S.L.; Strug, L.; Patz, J.A. Temperature and mortality in 11 cities of the eastern United States. Am. J. Epidemiol. 2002, 155, 80–87. [Google Scholar] [CrossRef]
- Kim, Y.; Joh, S. A vulnerability study of the low-income elderly in the context of high temperature and mortality in Seoul, Korea. Sci. Total Environ. 2006, 371, 82–88. [Google Scholar] [CrossRef]
- Medina-Ramón, M.; Zanobetti, A.; Cavanagh, D.P.; Schwartz, J. Extreme temperatures and mortality: Assessing effect modification by personal characteristics and specific cause of death in a multi-city case-only analysis. Environ. Health Perspect. 2006, 114, 1331–1336. [Google Scholar] [CrossRef]
- O’Neill, M.S.; Zanobetti, A.; Schwartz, J. Disparities by race in heat-related mortality in four US cities: The role of air conditioning prevalence. J. Urban Health 2005, 82, 191–197. [Google Scholar] [CrossRef]
- Yang, J.; Yin, P.; Sun, J.; Wang, B.; Zhou, M.; Li, M.; Tong, S.; Meng, B.; Guo, Y.; Liu, Q. Heatwave and mortality in 31 major Chinese cities: Definition, vulnerability and implications. Sci. Total Environ. 2019, 649, 695–702. [Google Scholar] [CrossRef]
- Marmot, M.P.; Friel, S.P.; Bell, R.P.; Houweling, T.A.J.P.; Taylor, S.P.; Commission on Social Determinants of Health. Closing the gap in a generation: Health equity through action on the social determinants of health. Lancet 2008, 372, 1661–1669. [Google Scholar] [CrossRef]
- World Health Organization. The Ottawa Charter for Health Promotion. Available online: https://www.who.int/healthpromotion/conferences/previous/ottawa/en/index1.html (accessed on 30 August 2019).
- Fry, D.; Zask, A. Applying the Ottawa Charter to inform health promotion programme design. Health Promot. Int. 2017, 32, 901–912. [Google Scholar] [CrossRef] [PubMed]
- Britto, M.T.; Fuller, S.C.; Kaplan, H.C.; Kotagal, U.; Lannon, C.; Margolis, P.A.; Muething, S.E.; Schoettker, P.J.; Seid, M. Using a network organisational architecture to support the development of Learning Healthcare Systems. BMJ Qual. Saf. 2018, 27, 937–946. [Google Scholar] [CrossRef] [PubMed]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; Prisma Group. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. J. Clin. Epidemiol. 2009, 62, 1006–1012. [Google Scholar] [CrossRef]
- Fink, R.; Erzen, I.; Medved, S. Symptomatic Response of the Elderly with Cardiovascular Disease during a Heat Wave in Slovenia. Cent. Eur. J. Public Health 2017, 25, 293–298. [Google Scholar] [CrossRef]
- Loughnan, M.E.; Carroll, M.; Tapper, N. Learning from our older people: Pilot study findings on responding to heat. Australas. J. Ageing 2014, 33, 271–277. [Google Scholar] [CrossRef]
- Hansen, A.; Bi, P.; Nitschke, M.; Pisaniello, D.; Newbury, J.; Kitson, A. Older persons and heat-susceptibility: The role of health promotion in a changing climate. Health Promot. J. Austr. 2011, 22, S17–S20. [Google Scholar] [CrossRef]
- Hendry, M.; Williams, N.H.; Wilkinson, C. A survey of local health promotion initiatives for older people in Wales. BMC Public Health 2008, 8, 217. [Google Scholar] [CrossRef]
- Nitschke, M.; Tucker, G.R.; Hansen, A.L.; Williams, S.; Zhang, Y.; Bi, P. Impact of two recent extreme heat episodes on morbidity and mortality in Adelaide, South Australia: A case-series analysis. Environ. Health 2011, 10, 42. [Google Scholar] [CrossRef] [PubMed]
- Schifano, P.; Cappai, G.; De Sario, M.; Michelozzi, P.; Marino, C.; Bargagli, A.M.; Perucci, C.A. Susceptibility to heat wave-related mortality: A follow-up study of a cohort of elderly in Rome. Environ. Health 2009, 8, 50. [Google Scholar] [CrossRef]
- Zhang, Y.; Nitschke, M.; Krackowizer, A.; Dear, K.; Pisaniello, D.; Weinstein, P.; Tucker, G.; Shakib, S.; Bi, P. Risk factors of direct heat-related hospital admissions during the 2009 heatwave in Adelaide, Australia: A matched case-control study. BMJ Open 2016, 6, e010666. [Google Scholar] [CrossRef]
- Haque, M.A.; Budi, A.; Azam Malik, A.; Suzanne Yamamoto, S.; Louis, V.R.; Sauerborn, R. Health coping strategies of the people vulnerable to climate change in a resource-poor rural setting in Bangladesh. BMC Public Health 2013, 13, 565. [Google Scholar] [CrossRef]
- Khare, S.; Hajat, S.; Kovats, S.; Lefevre, C.E.; de Bruin, W.B.; Dessai, S.; Bone, A. Heat protection behaviour in the UK: Results of an online survey after the 2013 heatwave. BMC Public Health 2015, 15, 878. [Google Scholar] [CrossRef]
- Kreslake, J.M.; Price, K.M.; Sarfaty, M. Developing effective communication materials on the health effects of climate change for vulnerable groups: A mixed methods study. BMC Public Health 2016, 16, 946. [Google Scholar] [CrossRef]
- Price, K.; Perron, S.; King, N. Implementation of the Montreal Heat Response Plan during the 2010 Heat Wave. Can. J. Public Health 2013, 104, E96–E100. [Google Scholar] [CrossRef] [PubMed]
- Price, K.; Benmarhnia, T.; Gaudet, J.; Kaiser, D.; Sadoine, M.L.; Perron, S.; Smargiassi, A. The Montreal heat response plan: Evaluation of its implementation towards healthcare professionals and vulnerable populations. Can. J. Public Health 2018, 109, 108–116. [Google Scholar] [CrossRef]
- Hansen, A.; Bi, P.; Nitschke, M.; Pisaniello, D.; Newbury, J.; Kitson, A. Perceptions of Heat-Susceptibility in Older Persons: Barriers to Adaptation. Int. J. Environ. Res. Public Health 2011, 8, 4714–4728. [Google Scholar] [CrossRef] [PubMed]
- Hansen, A.; Peng, B.; Pisaniello, D.; Nitschke, M.; Tucker, G.; Newbury, J.; Kitson, A.; Dal Grande, E.; Avery, J.; Ying, Z.; et al. Heat-health behaviours of older people in two Australian states. Australas. J. Ageing 2015, 34, E19–E25. [Google Scholar] [CrossRef]
- Ibrahim, J.E.; McInnes, J.A.; Andrianopoulos, N.; Evans, S. Minimising harm from heatwaves: A survey of awareness, knowledge, and practices of health professionals and care providers in Victoria, Australia. Int. J. Public Health 2012, 57, 297–304. [Google Scholar] [CrossRef]
- McInnes, J.A.; Ibrahim, J.E. Minimising harm to older Victorians from heatwaves: A qualitative study of the role of community-based health profession and carer organisations. Australas. J. Ageing 2010, 29, 104–110. [Google Scholar] [CrossRef]
- Nitschke, M.; Hansen, A.; Bi, P.; Pisaniello, D.; Newbury, J.; Kitson, A.; Tucker, G.; Avery, J.; Dal Grande, E. Risk Factors, Health Effects and Behaviour in Older People during Extreme Heat: A Survey in South Australia. Int. J. Environ. Res. Public Health 2013, 10, 6721–6733. [Google Scholar] [CrossRef]
- Nitschke, M.; Tucker, G.; Hansen, A.; Williams, S.; Zhang, Y.; Bi, P. Evaluation of a heat warning system in Adelaide, South Australia, using case-series analysis. BMJ Open 2016, 6, e012125. [Google Scholar] [CrossRef]
- Nitschke, M.; Krackowizer, A.; Hansen, A.L.; Bi, P.; Tucker, G.R. Heat health messages: A randomized controlled trial of a preventative messages tool in the older population of South Australia. Int. J. Environ. Res. Public Health 2017, 14, 992. [Google Scholar] [CrossRef] [PubMed]
- Liotta, G.; Inzerilli, M.C.; Palombi, L.; Madaro, O.; Orlando, S.; Scarcella, P.; Betti, D.; Marazzi, M.C. Social Interventions to Prevent Heat-Related Mortality in the Older Adult in Rome, Italy: A Quasi-Experimental Study. Int. J. Environ. Res. Public Health 2018, 15, 715. [Google Scholar] [CrossRef] [PubMed]
- Michelozzi, P.; de’Donato, F.K.; Bargagli, A.M.; D’Ippoliti, D.; De Sario, M.; Marino, C.; Schifano, P.; Cappai, G.; Leone, M.; Kirchmayer, U.; et al. Surveillance of summer mortality and preparedness to reduce the health impact of heat waves in Italy. Int. J. Environ. Res. Public Health 2010, 7, 2256–2273. [Google Scholar] [CrossRef]
- Schifano, P.; Leone, M.; De Sario, M.; de’Donato, F.; Bargagli, A.M.; D’Ippoliti, D.; Marino, C.; Michelozzi, P. Changes in the effects of heat on mortality among the elderly from 1998–2010: Results from a multicenter time series study in Italy. Environ. Health 2012, 11, 58. [Google Scholar] [CrossRef]
- Benmarhnia, T.; Bailey, Z.; Kaiser, D.; Auger, N.; King, N.; Kaufman, J.S. A Difference-in-Differences Approach to Assess the Effect of a Heat Action Plan on Heat-Related Mortality, and Differences in Effectiveness According to Sex, Age, and Socioeconomic Status (Montreal, Quebec). Environ. Health Perspect. 2016, 124, 1694–1699. [Google Scholar] [CrossRef] [PubMed]
- Sheridan, S.C. A survey of public perception and response to heat warnings across four North American cities: An evaluation of municipal effectiveness. Int. J. Biometeorol. 2007, 52, 3–15. [Google Scholar] [CrossRef]
- White-Newsome, J.L.; Sanchez, B.N.; Parker, E.A.; Dvonch, J.T.; Zhang, Z.Z.; O’Neill, M.S. Assessing heat-adaptive behaviors among older, urban-dwelling adults. Maturitas 2011, 70, 85–91. [Google Scholar] [CrossRef]
- Abrahamson, V.; Raine, R. Health and social care responses to the Department of Health Heatwave Plan. J. Public Health 2009, 31, 478–489. [Google Scholar] [CrossRef] [PubMed]
- Abrahamson, V.; Wolf, J.; Lorenzoni, I.; Fenn, B.; Kovats, S.; Wilkinson, P.; Adger, W.N.; Raine, R. Perceptions of heatwave risks to health: Interview-based study of older people in London and Norwich, UK. J. Public Health 2009, 31, 119–126. [Google Scholar] [CrossRef]
- Wolf, J.; Adger, W.N.; Lorenzoni, I.; Abrahamson, V.; Raine, R. Social capital, individual responses to heat waves and climate change adaptation: An empirical study of two UK cities. Glob. Environ. Chang. 2010, 20, 44–52. [Google Scholar] [CrossRef]
- Herrmann, A.; Sauerborn, R. General Practitioners’ Perceptions of Heat Health Impacts on the Elderly in the Face of Climate Change—A Qualitative Study in Baden-Wurttemberg, Germany. Int. J. Environ. Res. Public Health 2018, 15, 843. [Google Scholar] [CrossRef]
- Takahashi, N.; Nakao, R.; Ueda, K.; Ono, M.; Kondo, M.; Honda, Y.; Hashizume, M. Community trial on heat related-illness prevention behaviors and knowledge for the elderly. Int. J. Environ. Res. Public Health 2015, 12, 3188–3214. [Google Scholar] [CrossRef]
- German Federal Ministry for the Environment, Nature Conservation, Building and Nuclear Safety. Recommendations for Action Heat Action Plans to Protect Human Health. Available online: https://www.bmu.de/fileadmin/Daten_BMU/Download_PDF/Klimaschutz/hap_handlungsempfehlungen_en_bf.pdf (accessed on 30 August 2019).
- Heatwave Plan for Victoria. Available online: http://docs2.health.vic.gov.au/docs/doc/45C7A59BDE5B1E95CA257A360015AAB5/%24FILE/Heatwave%20plan%20for%20Victoria.pdf (accessed on 30 August 2019).
- Spencer, G.; Corbin, J.H.; Miedema, E. Sustainable development goals for health promotion: A critical frame analysis. Health Promot. Int. 2019, 34, 847–858. [Google Scholar] [CrossRef]
- Labonté, R. Health promotion in an age of normative equity and rampant inequality. Int. J. Health Policy 2016, 5, 675–682. [Google Scholar] [CrossRef] [PubMed]
- Martinez, G.S.; Imai, C.; Masumo, K. Local heat stroke prevention plans in Japan: Characteristics and elements for public health adaptation to climate change. Int. J. Environ. Res. Public Health 2011, 8, 4563–4581. [Google Scholar] [CrossRef]
- Toloo, G.; FitzGerald, G.; Aitken, P.; Verrall, K.; Tong, S. Evaluating the effectiveness of heat warning systems: Systematic review of epidemiological evidence. Int. J. Public Health 2013, 58, 667–681. [Google Scholar] [CrossRef]
- Van Loenhout, J.A.; Roiguez-Llanes, J.M.; Guha-Sapir, D. Stakeholders’ Perception on National Heatwave Plans and Their Local Implementation in Belgium and The Netherlands. Int. J. Environ. Res. Public Health 2016, 13, 1120. [Google Scholar] [CrossRef] [PubMed]
- Marmot, M.; Bell, R. Fair society, healthy lives. Public Health 2012, 126, S4–S10. [Google Scholar] [CrossRef]
- Bassil, K.L.; Cole, D.C. Effectiveness of public health interventions in reducing morbidity and mortality during heat episodes: A structured review. Int. J. Environ. Res. Public Health 2010, 7, 991–1001. [Google Scholar] [CrossRef]
- Bennetts, H.; Pullen, S.; Zillante, G. Design strategies for houses subject to heatwaves. Open House Int. 2012, 37, 29–38. [Google Scholar]
- Hatvani-Kovacs, G.; Boland, J. Retrofitting Precincts for Heatwave Resilience: Challenges and Barriers in Australian Context. Challenges 2015, 6, 3–25. [Google Scholar] [CrossRef]
- Keramitsoglou, I.; Sismanidis, P.; Analitis, A.; Butler, T.; Founda, D.; Giannakopoulos, C.; Giannatou, E.; Karali, A.; Katsouyanni, K.; Kendrovski, V.; et al. Urban thermal risk reduction: Developing and implementing spatially explicit services for resilient cities. Sustain. Cities Soc. 2017, 34, 56–68. [Google Scholar] [CrossRef]
- United Nations, Department of Economic and Social Affairs, Population Division. World Urbanization Prospects 2018: Highlights (ST/ESA/SER.A/421). 2019. Available online: https://population.un.org/wup/Publications/Files/WUP2018-Highlights.pdf (accessed on 1 September 2019).
- Greenfield, E.A. Healthy Aging and Age-Friendly Community Initiatives. Public Policy Aging Rep. 2015, 25, 43–46. [Google Scholar] [CrossRef]
- Coll-Planas, L.; Valle Gómez, G.; Bonilla, P.; Masat, T.; Puig, T.; Monteserin, R. Promoting social capital to alleviate loneliness and improve health among older people in Spain. Health Soc. Care Community 2017, 25, 145–157. [Google Scholar] [CrossRef]
- Harada, K.; Masumoto, K.; Katagiri, K.; Fukuzawa, A.; Chogahara, M.; Kondo, N.; Okada, S. Community intervention to increase neighborhood social network among Japanese older adults. Geriatr. Gerontol. Int. 2018, 18, 462–469. [Google Scholar] [CrossRef]
- Baker, D.W.; Wolf, M.S.; Feinglass, J.; Thompson, J.A.; Gazmararian, J.A.; Huang, J. Health Literacy and Mortality Among Elderly Persons. Arch. Intern. Med. 2007, 167, 1503–1509. [Google Scholar] [CrossRef]
- Geboers, B.; de Winter, A.F.; Spoorenberg, S.L.W.; Wynia, K.; Reijneveld, S.A. The association between health literacy and self-management abilities in adults aged 75 and older, and its moderators. Qual. Life Res. 2016, 25, 2869–2877. [Google Scholar] [CrossRef] [PubMed]
- Serper, M.; Patzer, R.E.; Curtis, L.M.; Smith, S.G.; O’Conor, R.; Baker, D.W.; Wolf, M.S. Health Literacy, Cognitive Ability, and Functional Health Status among Older Adults. Health Serv. Res. 2014, 49, 1249–1267. [Google Scholar] [CrossRef] [PubMed]
- Johansson, H.; Stenlund, H.; Lundström, L.; Weinehall, L. Reorientation to more health promotion in health services—A study of barriers and possibilities from the perspective of health professionals. J. Multidiscip. Health 2010, 3, 213–224. [Google Scholar] [CrossRef] [PubMed]
- Yeatman, H.R.; Nove, T. Reorienting health services with capacity building: A case study of the Core Skills in Health Promotion Project. Health Promot. Int. 2002, 17, 341–350. [Google Scholar] [CrossRef][Green Version]
- Baig, M.M.; GholamHosseini, H.; Moqeem, A.A.; Mirza, F.; Lindén, M. A Systematic Review of Wearable Patient Monitoring Systems—Current Challenges and Opportunities for Clinical Adoption. J. Med. Syst. 2017, 41, 115. [Google Scholar] [CrossRef]
- Majumder, S.; Mondal, T.; Deen, M.J. Wearable sensors for remote health monitoring. Sensors 2017, 17, 130. [Google Scholar] [CrossRef]
- Munos, B.; Baker, P.C.; Bot, B.M.; Crouthamel, M.; de Vries, G.; Ferguson, I.; Hixson, J.D.; Malek, L.A.; Mastrototaro, J.J.; Misra, V.; et al. Mobile health: The power of wearables, sensors, and apps to transform clinical trials: Mobile technology and clinical trials. Ann. N. Y. Acad. Sci. 2016, 1375, 3–18. [Google Scholar] [CrossRef]
- Wagner, F.; Basran, J.; Dal Bello-Haas, V. A review of monitoring technology for use with older adults. J. Geriatr. Phys. Ther. 2012, 35, 28–34. [Google Scholar] [CrossRef]
- Pol, M.; van Nes, F.; van Hartingsveldt, M.; Buurman, B.; de Rooij, S.; Kröse, B. Older People’s Perspectives Regarding the Use of Sensor Monitoring in Their Home. Gerontologist 2016, 56, 485–493. [Google Scholar] [CrossRef]
- Claes, V.; Devriendt, E.; Tournoy, J.; Milisen, K. Attitudes and perceptions of adults of 60 years and older towards in-home monitoring of the activities of daily living with contactless sensors: An explorative study. Int. J. Nurs. Stud. 2015, 52, 134–148. [Google Scholar] [CrossRef]
- Williams, S.; Bi, P.; Newbury, J.; Robinson, G.; Pisaniello, D.; Saniotis, A.; Hansen, A. Extreme heat and health: Perspectives from health service providers in rural and remote communities in South Australia. Int. J. Environ. Res. Public Health 2013, 10, 5565–5583. [Google Scholar] [CrossRef] [PubMed]
- Bittner, M.-I.; Stößel, U. Perceptions of heatwave risks to health: Results of an qualitative interview study with older people and their carers in Freiburg, Germany. Psycho-Soc. Med. 2012, 9, Doc05. [Google Scholar]
- Wondmagegn, B.Y.; Xiang, J.; Williams, S.; Pisaniello, D.; Bi, P. What do we know about the healthcare costs of extreme heat exposure? A comprehensive literature review. Sci. Total Environ. 2019, 657, 608–618. [Google Scholar] [CrossRef] [PubMed]
- Moher, D.; Pham; Klassen, T.P.; Schulz, K.F.; Berlin, J.A.; Jadad, A.R.; Liberati, A. What contributions do languages other than English make on the results of meta-analyses? J. Clin. Epidemiol. 2000, 53, 964–972. [Google Scholar] [CrossRef]
- Morrison, A.; Polisena, J.; Husereau, D.; Moulton, K.; Clark, M.; Fiander, M.; Mierzwinski-Urban, M.; Clifford, T.; Hutton, B.; Rabb, D. The effect of english-language restriction on systematic review-based meta-analyses: A systematic review of empirical studies. Int. J. Technol. Assess. Health Care 2012, 28, 138–144. [Google Scholar] [CrossRef]
- Adams, J.; Hillier-Brown, F.C.; Moore, H.J.; Lake, A.A.; Araujo-Soares, V.; White, M.; Summerbell, C. Searching and synthesising ‘grey literature’ and ‘grey information’ in public health: Critical reflections on three case studies. Syst. Rev. 2016, 5, 164. [Google Scholar] [CrossRef]
- Mahood, Q.; Eerd, D.V.; Irvin, E. Searching for grey literature for systematic reviews: Challenges and benefits. Res. Synth. Methods 2014, 5, 221–234. [Google Scholar] [CrossRef]
- Ahmad, I.; Marwat, M.; Khan, H. Comparative analysis of study designs in health research. Gomal J. Med. Sci. 2014, 11, 242–244. [Google Scholar]
- Jehan, F.; Kazi, A.M. Basic study designs in health research. J. Pak. Med. Assoc. 2012, 62, 408–411. [Google Scholar]
- Herold, N.; Alexander, L.; Green, D.; Donat, M. Greater increases in temperature extremes in low versus high income countries. Environ. Res. Lett. 2017, 12, 34007. [Google Scholar] [CrossRef]
- Ahmadalipour, A.; Moradkhani, H.; Kumar, M. Mortality risk from heat stress expected to hit poorest nations the hardest. Clim. Chang. 2019, 152, 569–579. [Google Scholar] [CrossRef]
- Campbell, S.; Remenyi, T.A.; White, C.J.; Johnston, F.H. Heatwave and health impact research: A global review. Health Place 2018, 53, 210–218. [Google Scholar] [CrossRef] [PubMed]

| Parameters | Details |
|---|---|
| Population | Older people 65 years and over |
| Intervention | Heat prevention, adaptation or mitigation measures |
| Comparison | No prevention measures |
| Outcomes | Any observable/measurable effects of heat related mortality or morbidity |
| Author and Year | Country | Objectives | Subjects | Study Design | Intervention or Factors | Outcomes | Recommendations |
|---|---|---|---|---|---|---|---|
| Hansen et al. 2011 [43] | Australia | Investigate heat-susceptibility in older people and perceived adaptation barriers during heatwaves in Adelaide | n = 35 four groups of health providers, managers and policy makers | Telephone interviews and focus groups | Questioning respondents knowledge of risks to older people and barriers to adaptive behaviours | Respondents identified physiological (poor health, chronic conditions, functional disabilities), socioeconomic issues (costs associated with running air-conditioners), psychological issues (anxieties, cognitive dysfunction), and barriers/enablers to adaptive strategies | Clear instructions on operation of air-conditioners Energy rebates for older people Specific strategies for specific medical conditions |
| Hansen et al. 2015 [44] | Investigate prevention behaviours (PB) of independently living residents in South Australia and Victoria | n = 1000 ≥65 | Cross-sectional Telephone survey | Demographics, social contacts, self-evaluated health status, coping strategies, medications, air conditioning, and heat warnings | Most demonstrated PB; More heat warnings recall and AC in South Australia vs. Victoria; Female sex, chronic illness sufferers reported increased morbidity | Review current policies Disseminate heat warnings via media and SMS | |
| Ibrahim et al. 2012 [45] | Investigate healthcare providers current practices to care for older people living independently in Victoria | n = 327 Six groups | Cross-sectional electronic survey | 32 questions - demographic, professional characteristics, heatwave impacts, heat health knowledge, current practices to treat heat-related illness | Most aware of danger to older people; Gaps in knowledge: thermo-regulation, electric fans use and most critical time to offer help; Few emergency plans in place; Reactive and opportunistic in practices | Emergency response plans needed Improvement required in knowledge Call for a more proactive approach | |
| McInnes et al. 2010 [46] | Investigate roles of community organisations and health providers in reducing harm to older people living independently in Victoria | n = 12 Four groups | Cross-sectional study, face-to-face and telephone survey | Semi-structured interviews exploring their roles in an heatwave emergency and issues such as coordination, identification of high-risk persons and training/education | No formal heat action plans (HAPs); At-risk individuals identified prior to summer; Good communication networks available, potentially able to provide appropriate care but lacking coordination and training; Mainly reactive and opportunistic activities | Need formalised heat action plans More proactive strategies and practices More resources and training needed Develop ’buddy’ system of volunteers | |
| Nitschke et al. 2013 [47] | Investigate resilience, prevention behaviours, risk factors and health outcomes of independently living residents in South Australia | n = 499 ≥65 | Cross-sectional computer assisted telephone survey | Survey explored demographics, housing, social connectedness, self-reported health status and vulnerability, heat health knowledge and resilience | Majority are resilient; Variety of prevention behaviours reported; High medication usage for chronic diseases, female sex, mobility aids, chronic diseases, mental health increased risk and poorer outcomes; Less social contact for those <75 | Targeted intervention required to address medication use, co-morbidities, knowledge improvement and social isolation Policy development required | |
| Nitschke et al. 2016 [48] | Investigate effectiveness of heatwave warning system in Adelaide | Residents of all ages | Comparing morbidity–mortality data ecological design | Incidence rate ratios (IRRs) of daily ambulance call-outs, emergency presentations and mortality data from 2009 and 2014 heatwaves | Significant reduction in morbidity especially emergency presentations in 75+ group; No reduction in mortality rate | In-depth assessment of services provided during heatwave including reach and behaviour change More studies into mortality risks factors | |
| Nitschke et al. 2017 [49] | Investigate effectiveness of targeted information in preventing adverse health outcomes during heatwave | n = 637 ≥65 | RCT | Intervention group provided with specific instructions on heat protective measures; Control group advised to follow media and seek own medical assistance as needed | Higher use of AC, wet cloth on face/body and significant heat stress reduction in intervention group; Control group also demonstrated protective behaviours through media | Results generalizable to other older people population in SA Further studies on built environment thermal comfort, social services, GPs active involvement | |
| Liotta et al. 2018 [50] | Italy | Assess effectiveness of long live the elderly (LLE) program in reducing heat-related mortality from social isolation of independently living residents | n = 12207 ≥75 | Quasi- experimental retrospective cohort study | Intervention group given social support and all health needs via both formal institutions and volunteers; No extra support for control group; Mean property tax evaluation determined SES | Mortality rate reduced 13% under LLE with 25 deaths averted; LLE indirectly reduced impact of low SES and mortality | Routine assessments of older people and provision of case-specific social services could improve health outcomes during heatwaves |
| Michelozzi et al. 2010 [51] | Analyse current practices and methodologies of the Italian national heat prevention program | 93% residents ≥65 across 34 cities | Examine dose– response relationship between mortality and maximum apparent temperature (MAT) | Assessing strengths and limitations of different methods to monitor daily summer mortality in 2008, 2003 and reference period 1995–2002, using Rome and Milan as examples | Mortality (MAT) differed across cities; City-specific warning systems, coordinated central information network, constant modulation of preventative measures major strengths; Specific prevention programs ensured timely mitigation measures; Reduction in mortality rate attributable to prevention strategies | Implement local registries to identify vulnerable individuals - ensures uniform identification At-risk individuals require specific home-care plans Further assessment of heat mitigation plans required | |
| Schifano et al. 2012 [52] | Investigating effectiveness of heatwave prevention plans post-2003 | Residents ≥65 across 16 cities | Multi-centre time series (1998–2002) vs. (2006–2010) random effect multi-variate meta-analysis | Comparing 16 city-specific daily mortality rates pre and post heat prevention measures, by studying relationships between mortality and maximum apparent temperature | Observable reduction in effects of high temperature on mortality rates attributable to mitigation plans | More attention needed at beginning of summer when populations yet to adapt to heat and prevention activities not yet fully functional, and end of summer when the effect of heat is stronger | |
| Benmarhnia et al. 2016 [53] | America/Canada | Investigating causal effects heat action plans (HAP) and association with different subgroups | Male vs. Female; ≥65 vs. <65; Education first vs. third tertile | Quasi-experimental retrospective - difference-in-differences approach | Comparing daily mortality rates (2000–2003) and post-HAP introduction (2004–2007) | A reduction in 2.52 deaths per day overall with 2.44 deaths per day less for older people ≥ 65; A 2.48 deaths per day less for low SES group; No differences between genders | Specifically targeting vulnerable population may reduce inequalities between populations More frequent home visits and daily phone calls to more at-risk individuals |
| Sheridan 2007 [54] | Investigate efficacy - four heat warning systems in Dayton, Philadelphia Phoenix, Arizona, Toronto | n = 908 ≥65 | Cross-sectional telephone survey | Perception of own vulnerability, knowledge of prevention behaviour and course of action during heatwaves | Most aware of heat warnings but few understood what to do; Only ~ half changed behaviour; Main source of warnings from television and radio | Broadcast specific/easy to understand heat health advisories Address warnings ’blocking out’/confusion Explain safe use of electric fans | |
| White-Newsome et al. 2011 [55] | Investigate behaviours and adaptability to increased indoor temperatures and environment in Detroit | n = 29 Aged >65 | Cross-sectional survey of volunteered residents | Data collection via hourly activity logs of eight heat-adaptive behaviours | Indoor temperature significantly influenced behaviour; More adaptive behaviours in high-rises and highly impervious areas; Changing clothes, taking additional showers and going outside rarely used | Public health interventions outreach to this vulnerable group to encourage full range of prevention behaviours | |
| Abrahamson et al. 2009 [56] | UK | Explore frontline healthcare professionals’ risks awareness and support for older people at risk of heatwaves adverse effects and perceived barriers to effective implementation of HAP | n = 109 covering three different socio-economic areas | Semi-structured interviews and focus groups | Awareness of details of HAP; opinions of self and organizations’ ability to identify and prioritize high-risk individuals; barriers and facilitators to effective implementation of HAP | Poor awareness of HAP from health professionals; Summer workloads not prioritised with older people in mind citing complexities and classification of vulnerability and infrequency of heatwaves as barriers | Multidisciplinary approach to interventions recommended Further evaluation of existing practices |
| Abrahamson et al. 2009 [57] | Investigate knowledge, perceptions of heat health risks, and protective behaviours of older people living independently | n = 73 Aged 72–94 | Semi-structured interviews | Face-to-face interviews with subjects recommended by GPs | Few respondents considered themselves old or vulnerable or at risk of heat related illness, despite being aware of comorbidities; Most respondents disliked ’nanny state’ approach of intervention | Imbed warnings into favourite TV programs Clear/easy to understand instructions Focus on most ’at-risk’ individuals by health professionals Warn community rather than targeting individuals | |
| Wolf et al. 2010 [58] | Investigate older people self-reported vulnerability and subsequent influence on adaptive behaviour | n = 105 Aged 72–94 in Norwich and London | Semi-structured interviews and open-ended questions. Respondents (A) and nominated people (B) to whom they turned to for assistance also interviewed | Perceptions and knowledge of heat risks explored including daily routine, socialisation habits, physical activity, actual/hypothetical behavioural changes in response to heatwaves, barriers to do so, medical conditions and medications, and type of housing. | Most (A) did not think they were vulnerable nor perceive heatwaves as a threat to themselves; They did not understand the increased risks associated with certain medical conditions and medications; Reported behaviours more towards coping rather than mitigation; (B) respondents displayed inconsistent and limited knowledge of heat risks; Also (B) did not want to impinge on (A) independence; Potentially exacerbate (A) vulnerability | Further research into the role of bonding social capital and climate change adaptation Definite need to address barriers in mitigating behaviours Call for government initiatives to finance local social development such as community groups in providing support thus empowering the older people Re-evaluation of adaptation strategies and policy effectiveness | |
| Herrman et al. 2018 [59] | Germany | Investigate GPs perceptions on susceptibility and nursing care of older people during heatwaves in Baden-Württemberg | n = 24 over four districts | Face-to-face semi-structured interviews, Qualitative software analysed | Exploring knowledge of heatwaves, perceptions of older people morbidity and mortality risks factors and impact levels of future climate change to their well-being | Inconsistent knowledge of heatwaves amongst GPs; Variable levels of concern for older people heat–health based on varied perceptions of risks; Demonstrable uncertainties on impact of climate change on health | More training for GPs on climate change and heatwaves impacts on older people’s health Increase social support and nursing care for older people in extreme weather and heatwaves |
| Takahashi et al. 2015 [60] | Japan | Investigate improvement in prevention behaviours and heat health knowledge of older people in Nagasaki | n = 1524 aged 65–84 selected via stratified random sampling | Randomised controlled community trial | Three groups: 1. Heat health warnings + pamphlets 2. Heat health warnings + water bottles + pamphlets 3. Control group | Group 1 took more breaks, reduced activities, wore hats and sun block; Group 2 improved protective behaviours significantly - increased water intake and body cooling; All—poor knowledge of fans usage | Both individual and community based approaches are required for optimal improvement in heat health knowledge and prevention behaviours |
| Author/Year | Build Healthy Public Policy | Create Supportive Environment | Strengthen Community Action | Develop Personal Skills | Reorient Health Services |
|---|---|---|---|---|---|
| Hansen et al. 2011 [43] | N/A | N/A | N/A | N/A | Surveyed healthcare providers and legislators perceptions and knowledge |
| Hansen et al. 2015 [44] | N/A | N/A | N/A | Surveyed heat health behaviours | N/A |
| Ibrahim et al. 2012 [45] | N/A | N/A | N/A | N/A | Investigated health providers knowledge and practices |
| McInnes et al. 2010 [46] | N/A | N/A | N/A | N/A | Investigated community healthcare providers roles |
| Nitschke et al. 2013 [47] | N/A | N/A | N/A | Surveyed risk factors and Protective behaviours | N/A |
| Nitschke et al. 2016 [48] | Evaluation of HWS | N/A | N/A | N/A | N/A |
| Nitschke et al. 2017 [49] | Regional policy in place | N/A | N/A | Surveyed protective behaviours | N/A |
| Liotta et al. 2018 [50] | National and regional policies in place | Coordinated care network | Carers and volunteers involved | Individuals consent sought | Centralised database |
| Michelozzi et al. 2010 [51] | Evaluated national and regional policies | N/A | N/A | N/A | N/A |
| Schifano et al. 2012 [52] | Evaluated efficacy of HAPs | N/A | N/A | N/A | N/A |
| Benmarhnia et al. 2016 [53] | Evaluated effectiveness of HAP | N/A | N/A | N/A | N/A |
| Sheridan 2007 [54] | Reviewed HWS effectiveness | N/A | N/A | Surveyed individual responses | N/A |
| White-Newsome et al. 2011 [55] | N/A | Assess effects of indoor temperature | N/A | Surveyed protective behaviours | N/A |
| Abrahamson et al. 2009 [57] | N/A | N/A | N/A | N/A | Surveyed health professionals knowledge and perceptions |
| Abrahamson et al. 2009 [56] | N/A | N/A | N/A | Surveyed awareness and behaviours | N/A |
| Wolf et al. 2010 [58] | N/A | N/A | N/A | Surveyed perceptions of vulnerability and behaviours | N/A |
| Herrman et al. 2018 [59] | N/A | N/A | N/A | N/A | Investigated GPs knowledge and practices |
| Takahashi et al. 2015 [60] | Regional policy in place | Coordinated local network | Welfare commissioners involved | Surveyed prevention behaviours | Overseen by Institute of tropical medicine |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vu, A.; Rutherford, S.; Phung, D. Heat Health Prevention Measures and Adaptation in Older Populations—A Systematic Review. Int. J. Environ. Res. Public Health 2019, 16, 4370. https://doi.org/10.3390/ijerph16224370
Vu A, Rutherford S, Phung D. Heat Health Prevention Measures and Adaptation in Older Populations—A Systematic Review. International Journal of Environmental Research and Public Health. 2019; 16(22):4370. https://doi.org/10.3390/ijerph16224370
Chicago/Turabian StyleVu, An, Shannon Rutherford, and Dung Phung. 2019. "Heat Health Prevention Measures and Adaptation in Older Populations—A Systematic Review" International Journal of Environmental Research and Public Health 16, no. 22: 4370. https://doi.org/10.3390/ijerph16224370
APA StyleVu, A., Rutherford, S., & Phung, D. (2019). Heat Health Prevention Measures and Adaptation in Older Populations—A Systematic Review. International Journal of Environmental Research and Public Health, 16(22), 4370. https://doi.org/10.3390/ijerph16224370





