Addressing Profound Disadvantages to Improve Indigenous Health and Reduce Hospitalisation: A Collaborative Community Program in Remote Northern Territory
Abstract
:1. Introduction
2. Methods
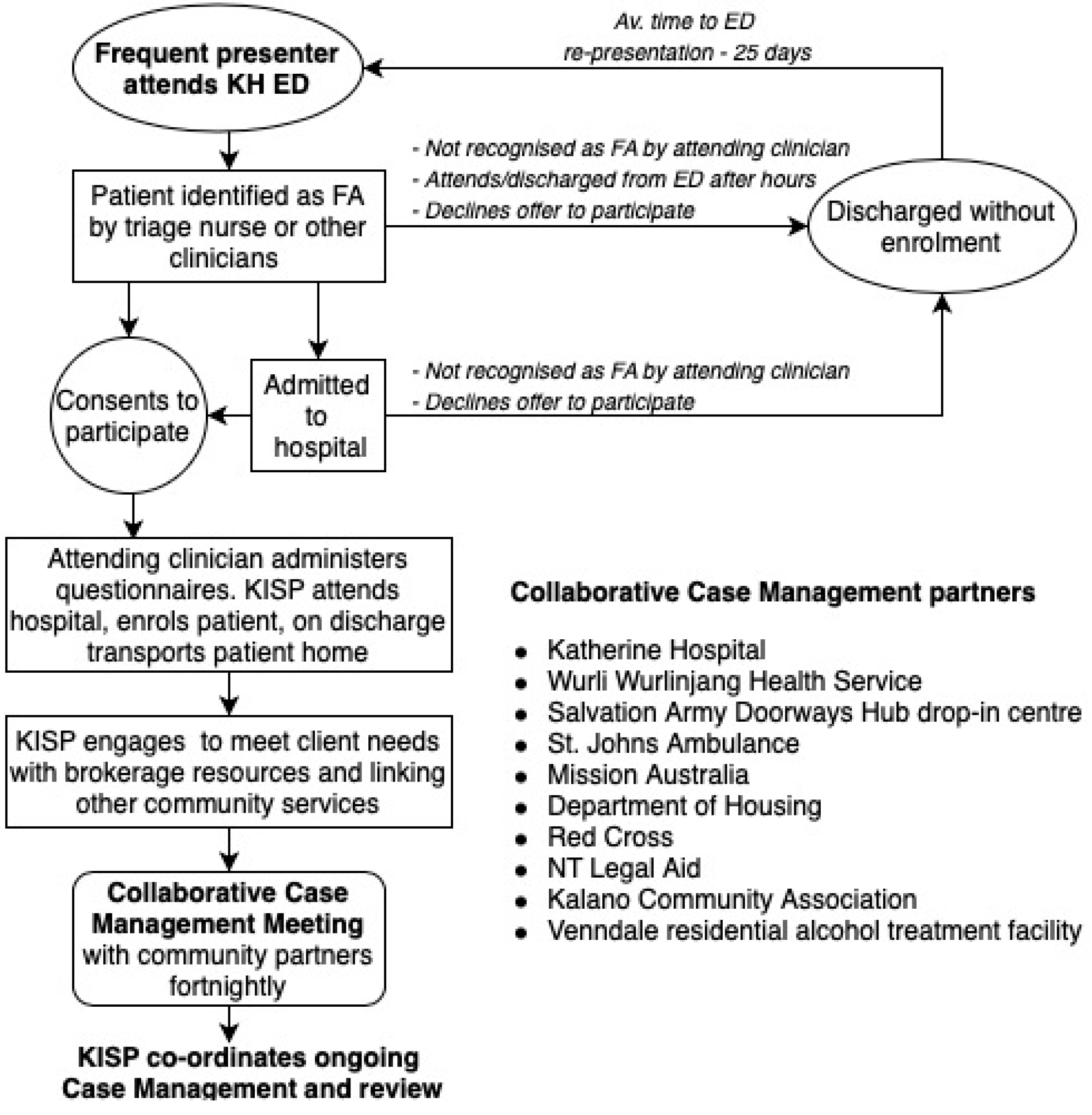
2.1. Intervention
2.2. Study Population and Participant Enrolment
2.3. Study Design
2.4. Data Sources
2.5. Statistical Analysis
2.6. Ethics Approval
3. Results
3.1. Intervention Structure and Governance
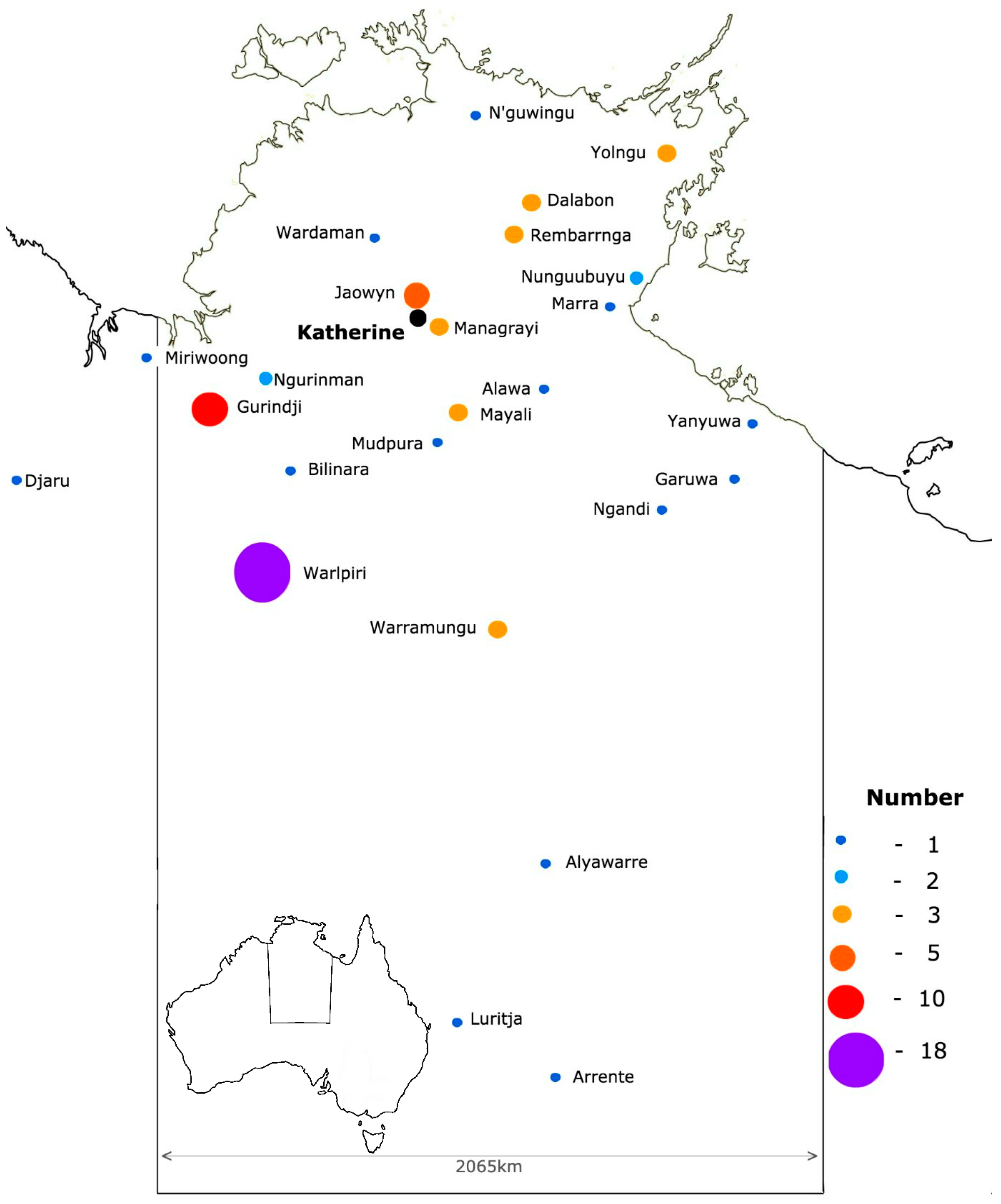
3.2. Participant Demographics
3.3. Health Conditions
3.4. Changes in Service Use
4. Discussion
4.1. Improving Health Service Utilisation
4.2. Social Drivers of Chronic Disease
4.3. Embracing Complexity
4.4. Limitations
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Commonwealth of Australia, Department of Prime Minister and Cabinet. Closing the Gap Report, 2019; Commonwealth of Australia: Canberra, Australia, 2019.
- Australian Institute of Health and Welfare. Rural and Remote Health; AIHW: Canberra, Australia, 2017.
- Zhao, Y.; You, J.; Wright, J.; Guthridge, S.L.; Lee, A.H. Health inequity in the Northern Territory. Int. J. Equity Health 2013, 12, 79. [Google Scholar]
- RMIT and Australian Broadcasting Corporation. 2015. Available online: https://www.abc.net.au/interactives/homeless/ (accessed on 18 February 2019).
- Quilty, S.; Shannon, G.; Yao, A.; Sargent, W.; McVeigh, M. Factors contributing to frequent attendance to the Emergency Department of a remote Northern Territory hospital. Med. J. Aust. 2016, 204, 111.e1–111.e7. [Google Scholar] [CrossRef] [PubMed]
- Costa, N.; Sullivan, M.; Walker, R. Emergency department presentations of Victorian Aboriginal and Torres Straight Islander people. Health Inf. Manag. J. 2008, 37, 15–24. [Google Scholar]
- Moore, G.; Gerdtz, M.; Manias, E. Homelessness, health status and emergency department use: An integrated review of the literature. Australas. Emerg. Nurs. J. 2007, 10, 178–185. [Google Scholar] [CrossRef]
- Moss, J.E.; Houghton, L.M.; Flower, C.; Moss, D.L.; Nielsen, D.A.; Taylor, D.M. A multidisciplinary care co-ordination team improves emergency department discharge planning. Med. J. Aust. 2009, 177, 435–439. [Google Scholar]
- Vinton, D.T.; Capp, R.; Rooks, S.P.; Abbott, J.T.; Ginde, A.A. Frequent users of US emergency departments: Characteristics and opportunities for intervention. Emerg. Med. J. 2014, 31, 526–532. [Google Scholar] [CrossRef] [PubMed]
- Sadowski, L.S.; Kee, R.A.; VanderWeele, T.J.; Buchanan, D. Effects of housing and case management program on emergency department visits and hospitalization of adults: A randomized trial. JAMA 2009, 301, 1771–1778. [Google Scholar] [CrossRef] [PubMed]
- Althaus, F.; Paroz, S.; Hugli, O. Effectiveness of interventions targeting frequent users of emergency departments: A systematic review. Ann. Emerg. Med. 2011, 58, 41–52. [Google Scholar] [CrossRef] [PubMed]
- Hudon, C.; Chouinard, M.C.; Lambert, M.; Diadiou, F.; Bouliane, D. Key factors of case management interventions for frequent users of healthcare services: A thematic analysis review. BMJ Open 2017, 7, e017762. [Google Scholar] [CrossRef] [PubMed]
- Shumway, M.; Boccellari, A.; O’Brien, K.; Okin, R.L. Cost effectiveness of clinical case management for Ed frequent attenders: Results of a randomized trial. Am. J. Emerg. Med. 2008, 26, 155–164. [Google Scholar] [CrossRef] [PubMed]
- Tadros, A.S. Effects of an emergency medical services-based resource access program on frequent users of health services. Prehosp. Emerg. Care 2012, 16, 541–547. [Google Scholar] [CrossRef] [PubMed]
- Hennessy, K.J.; Page, C.M.; McInnes, K.L.; Walsh, K.J.; Pittock, A.B.; Bathols, J.M.; Suppiah, R. Climate Change in the Northern Territory. Consultancy Report for the Northern Territory Department of Infrastructure, Planning and Environment; Climate Impact Group, CSIRO Atmospheric Research, School of Earth Sciences, Melbourne University: Melbourne, Australia, 2004. [Google Scholar]
- Available online: http://www.federalfinancialrelations.gov.au/content/npa/community_services/national-partnership/NT_remote_aboriginal_investment_Community_Safety.pdf (accessed on 1 October 2019).
- Bradley, K.A.; DeBenedetti, A.F.; Volk, R.J.; Williams, E.C.; Frank, D.; Kivlahn, D.R. AUDIT-C as a brief screen tool for alcohol misuse in primary care. Alcohol. Clin. Exp. Res. 2007, 31, 1208–1217. [Google Scholar] [CrossRef] [PubMed]
- Heatherton, T.F.; Kozlowski, L.T.; Frecker, R.C.; Fagerstrom, K. The fagerstrom test for nicotine dependence: A revision of the fagerstrom tolerance test. Brit. J. Addict. 1991, 86, 1119–1127. [Google Scholar] [CrossRef] [PubMed]
- Australian Bureau of Statistics, 2049.0—Census of Population and Housing: Estimating Homelessness, Appendix 1: Definition of Homelessness; Australian Bureau of Statistics: Canberra, Australia, 2018.
- Australian Institute of Health and Welfare. Australia’s Health 2016; Australia’s Health Series No. 15. Cat. No. AUS 199; AIHW: Canberra, Australia, 2016.
- Larewnce, J.G.; Carapetis, J.R.; Griffiths, K.; Edwards, K.; Condon, J. Acute rheumatic fever and rheumatic heart disease: Incidence and progression in the Northern Territory of Australia, 1197–2010. Circulation 2013, 128, 429–501. [Google Scholar]
- Shahid, S.; Taylor, E.V.; Cheetham, S.; Woods, J.A.; Aoun, S.M.; Thompson, S.C. Key features of palliative care service delivery to Indigenous peoples in Australia, New Zealand, Canada and the United States: A comprehensive review. Palliat. Care 2018, 17, 72–92. [Google Scholar] [CrossRef] [PubMed]
- Phillips, G.A.; Brophy, D.S.; Weiland, T.J.; Chenhall, A.J.; Dent, A.W. The effect of multidisciplinary case management on selected outcomes for frequent attenders in an emergency department. Med. J. Aust. 2006, 186, 602–606. [Google Scholar] [CrossRef]
| KISP Collaborative Case Management Group |
|---|
| Katherine Hospital |
| Wurli-Wurlinjang Health Service |
| Kalano Community Association |
| St. John’s Ambulance |
| Mission Australia |
| Red Cross |
| Salvation Army Doorways Hub homeless drop-in centre |
| NT Department of Housing |
| Northern Territory Legal Aid |
| Venndale Residential Alcohol Treatment Facility |
| Sommerville Community Services |
| Catholic Care |
| Demographics | |
| Age | 51yrs (range 23–86) |
| Sex (n = 109) | 54% female |
| Indigenous | 91% |
| Drug and alcohol use | % of participants |
| Alcohol AUDIT-C score (n = 96) | 5.6 (mean) |
| 0 | 28% |
| 1 to 2 | 4% |
| 3 to 4 | 4% |
| Greater than 4 | 64% |
| Smoker (n = 93) | 63% |
| Other drugs (n = 83) | 19% |
| Cannabis | 17% |
| Amphetamines | 1% |
| Volatile substance (petrol fumes, other inhalant) | 1% |
| Benzodiazepine | 1% |
| Medical or social vulnerability | % of participants |
| Medical/social vulnerability contributing to presentation (n = 75) | |
| Medical | 20% |
| Social | 17% |
| Both Medical and social | 63% |
| Social issues | % of participants |
| Food insecurity (n = 83) | 60% |
| No access to transport (n = 80) | 80% |
| Domestic violence (n = 69) | 13% |
| Accommodation (n = 90) | |
| Meets ABS definition of homelessness | 64% |
| Consider themselves homeless | 51% |
| Living rough (no access to a dwelling) | 26% |
| Lives in a house | 64% |
| Lives in supported accommodation | 2% |
| Lives in a temporary shelter | 4% |
| Lives between multiple dwellings/locations | 36% |
| Those living in a house (n = 64) | |
| Average number of people per room | 2.3 (range 1–6.6) |
| Number with >2.5 people per bedroom | 42% |
| Medical Comorbidities (n = 103, Mean 2.8 per Participant, Range 0–10) | % of Participants |
|---|---|
| Drug and alcohol addiction | 54% |
| Cardiovascular disease | 33% |
| Metabolic disease | 30% |
| Renal disease | 23% |
| (on dialysis) | 10% |
| Neurological disease | 18% |
| Respiratory disease | 18% |
| Infectious disease | 16% |
| Liver/Gastrointestinal tract disease | 15% |
| Mental health | 15% |
| Physical disability | 10% |
| (Rheumatic Heart) | 8% |
| Hearing/vision impairment | 8% |
| Malignancy | 4% |
| Palliative care needs | 4% |
| Autoimmune disease | 2% |
| Pregnancy | 0% |
| Non-compliance contributing to index presentation (n = 72) | 51% |
| Before and after Event | IRR | 95% CI | Average of Episodes per Month | |
|---|---|---|---|---|
| Pre-Enrolment | Post-Enrolment | |||
| ED presentations | 0.77 | 0.69–0.85 | 1.14 | 0.88 |
| Hospital admissions | 0.93 | 0.77–1.10 | 0.35 | 0.35 |
| Primary care contact episodes | 1.90 | 1.78–2.03 | 1.80 | 3.80 |
| Careflight retrievals | 0.67 | 0.35–1.20 | 0.05 | 0.03 |
| Ambulance episodes | 1.21 | 1.07–1.38 | 0.62 | 0.72 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Quilty, S.; Wood, L.; Scrimgeour, S.; Shannon, G.; Sherman, E.; Lake, B.; Budd, R.; Lawton, P.; Moloney, M. Addressing Profound Disadvantages to Improve Indigenous Health and Reduce Hospitalisation: A Collaborative Community Program in Remote Northern Territory. Int. J. Environ. Res. Public Health 2019, 16, 4306. https://doi.org/10.3390/ijerph16224306
Quilty S, Wood L, Scrimgeour S, Shannon G, Sherman E, Lake B, Budd R, Lawton P, Moloney M. Addressing Profound Disadvantages to Improve Indigenous Health and Reduce Hospitalisation: A Collaborative Community Program in Remote Northern Territory. International Journal of Environmental Research and Public Health. 2019; 16(22):4306. https://doi.org/10.3390/ijerph16224306
Chicago/Turabian StyleQuilty, Simon, Lisa Wood, Sophie Scrimgeour, Geordan Shannon, Elisha Sherman, Bruce Lake, Richard Budd, Paul Lawton, and Mary Moloney. 2019. "Addressing Profound Disadvantages to Improve Indigenous Health and Reduce Hospitalisation: A Collaborative Community Program in Remote Northern Territory" International Journal of Environmental Research and Public Health 16, no. 22: 4306. https://doi.org/10.3390/ijerph16224306
APA StyleQuilty, S., Wood, L., Scrimgeour, S., Shannon, G., Sherman, E., Lake, B., Budd, R., Lawton, P., & Moloney, M. (2019). Addressing Profound Disadvantages to Improve Indigenous Health and Reduce Hospitalisation: A Collaborative Community Program in Remote Northern Territory. International Journal of Environmental Research and Public Health, 16(22), 4306. https://doi.org/10.3390/ijerph16224306





