Development and Validation of an Evaluation Tool to Measure the Effectiveness of a Smoking Cessation Training among Healthcare Providers in Malaysia: The Providers’ Smoking Cessation Training Evaluation (ProSCiTE)
Abstract
:1. Introduction
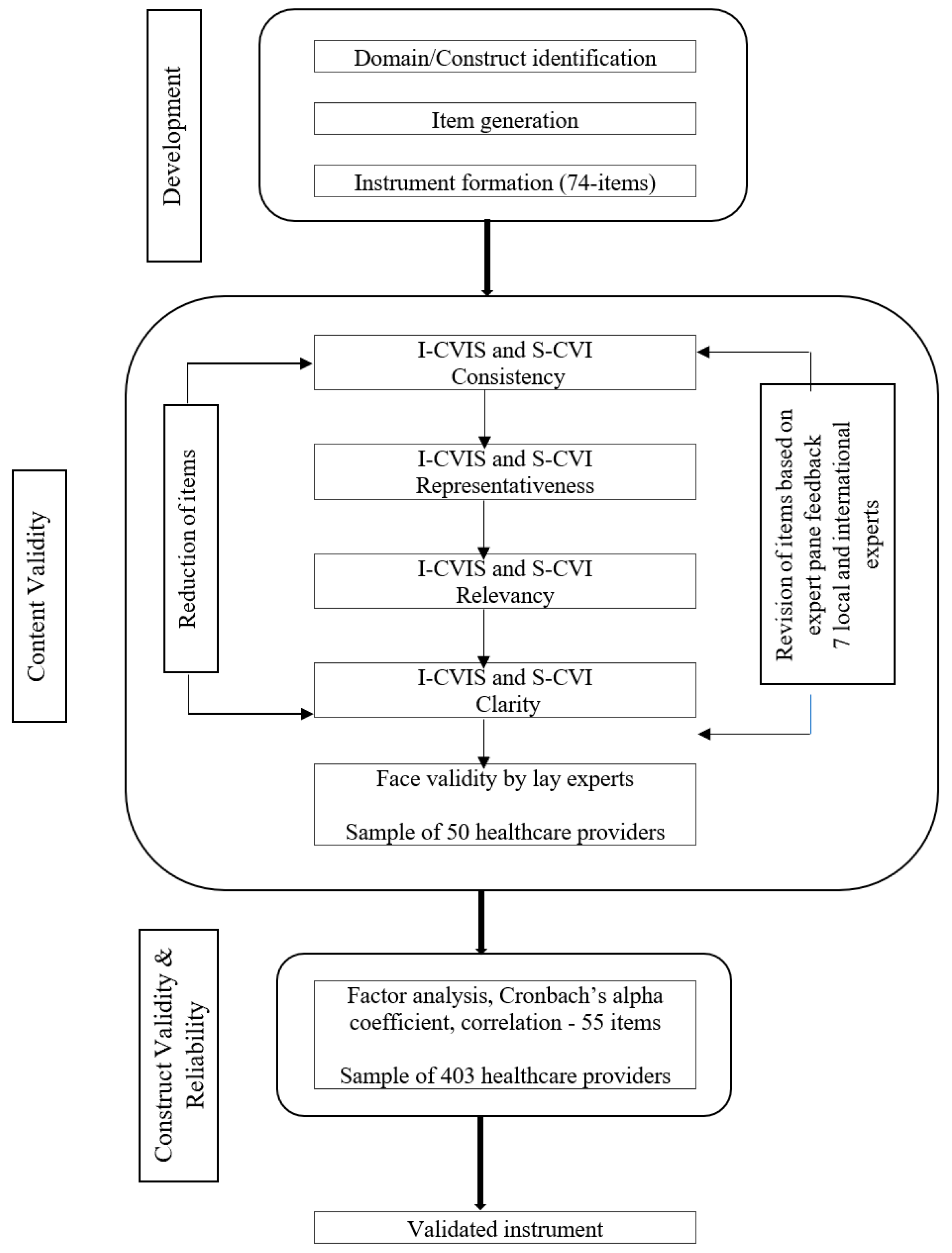
2. Materials and Methods
2.1. ProSCiTE Development
2.2. Content and Face Validity
2.2.1. Participants and Setting
2.2.2. Quantification of Content Validity
2.3. Construct Validity and Reliability
2.3.1. Participants and Setting
2.3.2. Reliability
2.3.3. Determination of Correlation
2.4. Ethical Approval
2.5. Statistical Methods
2.5.1. Descriptive Analysis
2.5.2. Content Validity Analysis
2.5.3. Construct Validity Analysis
2.5.4. Reliability Analysis
2.5.5. Correlation Analysis
3. Results
3.1. Content and Face Validity
3.1.1. Demographics of Expert Reviewers
3.1.2. Content Validity
3.2. Construct Validity and Reliability
3.2.1. Healthcare Providers’ Characteristics
3.2.2. Exploratory Factor Analysis
3.2.3. Item Reliability
3.2.4. Correlation Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Zapka, J.G.; Fletcher, K.E.; Ma, Y.; Pbert, L. Physicians and smoking cessation:development of survey measures. Eval. Health Prof. 1997, 20, 407–427. [Google Scholar] [CrossRef] [PubMed]
- Delucchi, K.L.; Tajima, B.; Guydish, J. Development of the Smoking Knowledge, Attitudes, and Practices (S-KAP) Instrument. J. Drug Issues 2009, 39, 347–364. [Google Scholar] [CrossRef] [PubMed]
- Sereno, A.B.; Soares, E.C.C.; Silva, J.R.L.; Nápoles, A.M.; Bialous, S.A.; Silva, V.L.D.; Novotny, T.E. Feasibility study of a smoking cessation intervention in Directly Observed Therapy Short-Course tuberculosis treatment clinics in Rio de Janeiro, Brazil. Rev. Panam. Salud Pública 2012, 32, 451–456. [Google Scholar] [CrossRef]
- Abdullah, A.S.M.; Rahman, A.M.; Suen, C.W.; Wing, L.S.; Ling, L.W.; Mei, L.Y.; Tat, L.C.; Nin Tai, M.; Wing, T.N.; Yuen, W.T.; et al. Investigation of Hong Kong doctors’ current knowledge, beliefs, attitudes, confidence and practices: Implications for the treatment of tobacco dependency. J. Chin. Med. Assoc. 2006, 69, 461–471. [Google Scholar] [CrossRef]
- Prucha, M.G.; Fisher, S.G.; McIntosh, S.; Grable, J.C.; Holderness, H.; Thevenet-Morrison, K.; De Monegro, Z.Q.; Sanchez, J.J.; Bautista, A.; Díaz, S.; et al. Health Care Worker’s Knowledge, Attitudes and Practices on Tobacco Use in Economically Disadvantaged Dominican Republic Communities. Int. J. Environ. Res. Public Health 2015, 12, 4060–4075. [Google Scholar] [CrossRef]
- Applegate, B.W.; Sheffer, C.E.; Crews, K.M.; Payne, T.J.; Smith, P.O. A survey of tobacco-related knowledge, attitudes and behaviours of primary care providers in Mississippi. J. Eval. Clin. Pract. 2008, 14, 537–544. [Google Scholar] [CrossRef]
- Sheffer, C.E.; Barone, C.; Anders, M.E. Training nurses in the treatment of tobacco use and dependence: Pre- and post-training results. J. Adv. Nurs. 2011, 67, 176–183. [Google Scholar] [CrossRef]
- Sheffer, C.E.; Barone, C.P.; Anders, M.E. Training health care providers in the treatment of tobacco use and dependence: Pre- and post-training results. J. Eval. Clin. Pract. 2009, 15, 607–613. [Google Scholar] [CrossRef]
- MoH, M. Clinical Practice Guideline on Treatment of Tobacco Use Disorder; Ministry of Health Malaysia: Putrajaya, Malaysia, 2016.
- Fiore, M.C.; Jaén, C.R.; Baker, T.B. Treating Tobacco Use and Dependence: 2008 Update; Clinical Practice Guideline; Public Health Service; U.S. Department of Health and Human Services: Rockville, MD, USA, 2008.
- Siu, A.L. Behavioral and pharmacotherapy interventions for tobacco smoking cessation in adults, including pregnant women: U.S. preventive services task force recommendation statement. Ann. Intern. Med. 2015, 163, 622–634. [Google Scholar] [CrossRef]
- Stead, L.F.; Buitrago, D.; Preciado, N.; Sánchez, G.; Lancaster, T.; Hartmann-Boyce, J.; Hartmann-Boyce, J. Physician advice for smoking cessation. Cochrane Database Syst. Rev. 2013, 5, CD000165. [Google Scholar] [CrossRef] [PubMed]
- Lancaster, T.; Stead, L.F. Individual behavioural counselling for smoking cessation. Cochrane Database Syst. Rev. 2017, 3, CD001292. [Google Scholar] [CrossRef] [PubMed]
- Freund, M.; Campbell, E.; Paul, C.; McElduff, P.; Walsh, R.A.; Sakrouge, R.; Wiggers, J.; Knight, J. Smoking Care Provision in Hospitals: A Review of Prevalence. Nicotine Tob. Res. 2008, 10, 757–774. [Google Scholar] [CrossRef] [PubMed]
- Martínez, C.; Fu, M.; Martínez-Sánchez, J.M.; Ballbè, M.; Puig, M.; García, M.; Carabasa, E.; Saltó, E.; Fernández, E. Tobacco control policies in hospitals before and after the implementation of a national smoking ban in Catalonia, Spain. BMC Public Health 2009, 9, 160. [Google Scholar] [CrossRef] [PubMed]
- Bolman, C.; Sino, C.; Hekking, P.; Van Keimpema, A.; Van Meerbeeck, J. Willingness of pulmonologists to guide COPD patients in smoking cessation. Patient Educ. Couns. 2005, 57, 126–133. [Google Scholar] [CrossRef] [PubMed]
- De Ruijter, D.; Smit, E.S.; De Vries, H.; Goossens, L.; Hoving, C. Understanding Dutch practice nurses’ adherence to evidence-based smoking cessation guidelines and their needs for web-based adherence support: Results from semistructured interviews. BMJ Open 2017, 7, e014154. [Google Scholar] [CrossRef] [PubMed]
- Kotz, D.; Willemsen, M.C.; Brown, J.; West, R. Light smokers are less likely to receive advice to quit from their GP than moderate-to-heavy smokers: A comparison of national survey data from the Netherlands and England. Eur. J. Gen. Pract. 2013, 19, 99–105. [Google Scholar] [CrossRef] [Green Version]
- Meijer, E.; Verbiest, M.E.; Chavannes, N.H.; Kaptein, A.A.; Assendelft, W.J.; Scharloo, M.; Crone, M.R. Smokers’ identity and quit advice in general practice: General practitioners need to focus more on female smokers. Patient Educ. Couns. 2018, 101, 730–737. [Google Scholar] [CrossRef]
- Segaar, D.; Willemsen, M.C.; Bolman, C.; De Vries, H. Nurse adherence to a minimal-contact smoking cessation intervention on cardiac wards. Res. Nurs. Health 2007, 30, 429–444. [Google Scholar] [CrossRef]
- Van Rossem, C.; Spigt, M.G.; Kleijsen, J.R.; Hendricx, M.; Van Schayck, C.P.; Kotz, D. Smoking cessation in primary care: Exploration of barriers and solutions in current daily practice from the perspective of smokers and healthcare professionals. Eur. J. Gen. Pract. 2015, 21, 11–17. [Google Scholar] [CrossRef]
- West, R.; Dimarino, M.; Gitchell, J.; McNeill, A. Impact of UK policy initiatives on use of medicines to aid smoking cessation. Tob. Control 2005, 14, 166–171. [Google Scholar] [CrossRef] [Green Version]
- Young, J.M.; Ward, J.E. Implementing guidelines for smoking cessation advice in Australian general practice: Opinions, current practices, readiness to change and perceived barriers. Fam. Pract. 2001, 18, 14–20. [Google Scholar] [CrossRef] [PubMed]
- Hildebrand, J.R.; Sastry, S. “Stop Smoking!” Do We Say It Enough? J. Oncol. Pract. 2013, 9, 230–232. [Google Scholar] [CrossRef] [PubMed]
- Saito, A.; Nishina, M.; Murai, K.; Mizuno, A.; Ueshima, F.; Makiishi, T.; Ichinohe, T. Health professional’s perceptions of and potential barriers to smoking cessation care: A survey study at a dental school hospital in Japan. BMC Res. Notes 2010, 3, 329. [Google Scholar] [CrossRef] [PubMed]
- Tong, E.K.; Strouse, R.; Hall, J.; Kovac, M.; Schroeder, S.A. National survey of U.S. health professionals’ smoking prevalence, cessation practices, and beliefs. Nicotine Tob. Res. 2010, 12, 724–733. [Google Scholar] [CrossRef]
- Omole, O.B.; Ngobale, K.N.; Ayo-Yusuf, O.A. Missed opportunities for tobacco use screening and brief cessation advice in South African primary health care: A cross-sectional study. BMC Fam. Pract. 2010, 11, 94. [Google Scholar] [CrossRef]
- Brotons, C.; Björkelund, C.; Bulc, M.; Ciurana, R.; Godycki-Cwirko, M.; Jurgova, E.; Kloppe, P.; Lionis, C.; Mierzecki, A.; Piñeiro, R.; et al. Prevention and health promotion in clinical practice: The views of general practitioners in Europe. Prev. Med. 2005, 40, 595–601. [Google Scholar] [CrossRef]
- Stead, M.; Angus, K.; Holme, I.; Cohen, D.; Tait, G. Factors influencing European GPs’ engagement in smoking cessation: A multi-country literature review. Br. J. Gen. Pract. 2009, 59, 682–690. [Google Scholar] [CrossRef]
- Berman, B.A.; Yancey, A.K.; Bastani, R.; Grosser, S.C.; Staveren, A.; Williams, R.A.; Lee, D. African-American physicians and smoking cessation counseling. J. Natl. Med. Assoc. 1997, 89, 534–542. [Google Scholar]
- Cornuz, J.; Humair, J.-P.; Seematter, L.; Stoianov, R.; Van Melle, G.; Stalder, H.; Pécoud, A. Efficacy of Resident Training in Smoking CessationA Randomized, Controlled Trial of a Program Based on Application of Behavioral Theory and Practice with Standardized Patients. Ann. Intern. Med. 2002, 136, 429–437. [Google Scholar] [CrossRef]
- Carson, K.V.; Verbiest, M.E.; Crone, M.R.; Brinn, M.P.; Esterman, A.J.; Assendelft, W.J.; Smith, B.J. Training health professionals in smoking cessation. Cochrane Database Syst. Rev. 2012. [Google Scholar] [CrossRef]
- Taha, N.A.; Tee, O.G. Tobacco cessation through community pharmacies: Knowledge, attitudes, practices and perceived barriers among pharmacists in Penang. Health Educ. J. 2015, 74, 681–690. [Google Scholar] [CrossRef]
- Abdulateef, D.S.; Ali, A.J.; Abdulateef, D.S.; Mohesh, M.G. Smoking Knowledge, Attitude, and Practices Among Health Care Professionals from Sulaymaniyah City/Iraq. Tob. Use Insights 2016, 9, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Poon, V.H.K. Model for counseling people in relationships. Can. Fam. Physician 2007, 53, 237–238. [Google Scholar] [PubMed]
- IPH. National Health and Morbidity Survey 2015—Report on Smoking Status among Malaysian Adults; Ministry of Health Malaysia: Putrajaya, Malaysia, 2015.
- Jamal, A.; Phillips, E.; Gentzke, A.S.; Homa, D.M.; Babb, S.D.; King, B.A.; Neff, L.J. Current Cigarette Smoking Among Adults—United States, 2016. MMWR Morb. Mortal. Wkly. Rep. 2018, 67, 53–59. [Google Scholar] [CrossRef]
- Orleans, C.T.; Schoenbach, V.J.; Wagner, E.H.; Quade, D.; Salmon, M.A.; Pearson, D.C.; Kaplan, B.H. Self-help quit smoking interventions: Effects of self-help materials, social support instructions, and telephone counseling. J. Consult. Clin. Psych. 1991, 59, 439–448. [Google Scholar] [CrossRef]
- Ockene, J.K.; Hayes, R.B.; Churchill, L.C.; Crawford, S.L.; Jolicoeur, D.G.; Murray, D.M.; Shoben, A.B.; David, S.P.; Ferguson, K.J.; Huggett, K.N.; et al. Teaching Medical Students to Help Patients Quit Smoking: Outcomes of a 10-School Randomized Controlled Trial. J. Gen. Intern. Med. 2016, 31, 172–181. [Google Scholar] [CrossRef] [PubMed]
- Thomas, T.; Passfield, L.; Coulton, S.; Crone, D. Effectiveness of a tailored training programme in behaviour change counselling for community pharmacists: A pilot study. Patient Educ. Couns. 2016, 99, 132–138. [Google Scholar] [CrossRef]
- Malan, Z.; Mash, B.; Everett-Murphy, K. Evaluation of a training programme for primary care providers to offer brief behaviour change counselling on risk factors for non-communicable diseases in South Africa. Patient Educ. Couns. 2016, 99, 125–131. [Google Scholar] [CrossRef]
- Williams, J.M.; Miskimen, T.; Minsky, S.; Cooperman, N.A.; Miller, M.; Budsock, P.D.; Cruz, J.; Steinberg, M.L. Increasing Tobacco Dependence Treatment Through Continuing Education Training for Behavioral Health Professionals. Psychiatr. Serv. 2015, 66, 21–26. [Google Scholar] [CrossRef] [Green Version]
- Kristina, S.A.; Thavorncharoensap, M.; Pongcharoensuk, P.; Prabandari, Y.S. Impact of Smoking Cessation Training for Community Pharmacists in Indonesia. Asian Pac. J. Cancer Prev. 2015, 16, 3319–3323. [Google Scholar] [CrossRef] [Green Version]
- Brose, L.S.; McEwen, A.; Michie, S.; West, R.; Chew, X.Y.; Lorencatto, F. Treatment manuals, training and successful provision of stop smoking behavioural support. Behav. Res. Ther. 2015, 71, 34–39. [Google Scholar] [CrossRef] [PubMed]
- Simansalam, S.; Brewster, J.M.; Mohamed, M.H.N. Training Malaysian Pharmacy Undergraduates with Knowledge and Skills on Smoking Cessation. Am. J. Pharm. Educ. 2015, 79, 71. [Google Scholar] [CrossRef] [PubMed]
- Hayes, R.B.; Geller, A.; Churchill, L.; Jolicoeur, D.; Murray, D.M.; Shoben, A.; David, S.P.; Adams, M.; Okuyemi, K.; Fauver, R.; et al. Teaching tobacco dependence treatment and counseling skills during medical school: Rationale and design of the Medical Students helping patients Quit tobacco (MSQuit) group randomized controlled trial. Contemp. Clin. Trials 2014, 37, 284–293. [Google Scholar] [CrossRef] [PubMed]
- Raupach, T.; Al-Harbi, G.; McNeill, A.; Bobak, A.; McEwen, A. Smoking cessation education and training in U.K. medical schools: A national survey. Nicotine Tob. Res. 2015, 17, 372–375. [Google Scholar] [CrossRef] [PubMed]
- Dable, R.A.; Wasnik, P.B.; Pawar, B.R.; Bopardikar, S.S.; Nagmode, S.N. Assessment of professional competency and need of smoking cessation counseling for dental students. J. Educ. Eval. Health Prof. 2014, 11, 26. [Google Scholar] [CrossRef] [PubMed]
- Olano-Espinosa, E.; Matilla-Pardo, B.; Minué, C.; Gómez-Gascón, T.; Ayesta, F.J.; Anton, E. Effectiveness of a Health Professional Training Program for Treatment of Tobacco Addiction. Nicotine Tob. Res. 2013, 15, 1682–1689. [Google Scholar] [CrossRef]
- Hagimoto, A.; Nakamura, M.; Masui, S.; Bai, Y.; Oshima, A. Effects of Trained Health Professionals’ Behavioral Counseling Skills on Smoking Cessation Outcomes. Ann. Behav. Med. 2018, 52, 752–761. [Google Scholar] [CrossRef]
- Martínez, C.; Castellano, Y.; Company, A.; Guillen, O.; Margalef, M.; Arrien, M.A.; Sánchez, C.; Cáceres, P.; Barnoya, J.; Fernández, E. Impact of an online training program in hospital workers’ smoking cessation interventions in Bolivia, Guatemala and Paraguay. Gac. Sanit. 2018, 32, 236–243. [Google Scholar] [CrossRef]
- Payne, T.J.; Gaughf, N.W.; Sutton, M.J.; Sheffer, C.E.; Elci, O.U.; Cropsey, K.L.; Taylor, S.; Netters, T.; Whitworth, C.; Deutsch, P.; et al. The impact of brief tobacco treatment training on practice behaviours, self-efficacy and attitudes among healthcare providers. Int. J. Clin. Pract. 2014, 68, 882–889. [Google Scholar] [CrossRef]
- Sheffer, C.E.; Payne, T.; Ostroff, J.S.; Jolicoeur, D.; Steinberg, M.; Czabafy, S.; Foulds, J.; Bars, M.; Wassum, K.; Perry, B. Increasing the Quality and Availability of Evidence-based Treatment for Tobacco Dependence through Unified Certification of Tobacco Treatment Specialists. J. Smok. Cessat. 2016, 11, 229–235. [Google Scholar] [CrossRef]
- Yu, L.; Jiang, S.; Peng, S.; Young, K.J.; Yang, T.; Bottorff, J.L.; Wu, D. Global Health Professions Student Survey (GHPSS) in Tobacco Control in China. Am. J. Health Behav. 2015, 39, 732–741. [Google Scholar] [Green Version]
- Martin, B.A.; Bruskiewitz, R.H.; Chewning, B.A. Effect of a tobacco cessation continuing professional education program on pharmacists’ confidence, skills, and practice-change behaviors. J. Am. Pharm. Assoc. 2010, 50, 9–16. [Google Scholar] [CrossRef] [PubMed]
- Pbert, L.; Jolicoeur, D.; Reed, G.; Gammon, W.L. An Evaluation of Tobacco Treatment Specialist Counseling Performance Using Standardized Patient Interviews. Nicotine Tob. Res. 2007, 9, 119–128. [Google Scholar] [CrossRef] [PubMed]
- Zamanzadeh, V.; Rassouli, M.; Abbaszadeh, A.; Alavi Majd, H.; Nikanfar, A.; Ghahramanian, A. Details of content validity and objectifying it in instrument development. Pract. Today 2015, 1, 163–171. [Google Scholar]
- Zamanzadeh, V.; Ghahramanian, A.; Rassouli, M.; Abbaszadeh, A.; Alavi-Majd, H.; Nikanfar, A.-R. Design and Implementation Content Validity Study: Development of an instrument for measuring Patient-Centered Communication. Int. J. Caring Sci. 2015, 4, 165–178. [Google Scholar] [CrossRef] [PubMed]
- Gichuki, J.W.; Opiyo, R.; Mugyenyi, P.; Namusisi, K. Healthcare Providers’ Level of Involvement in Provision of Smoking Cessation Interventions in Public Health Facilities in Kenya. Public Health Afr. 2015, 6, 523. [Google Scholar] [CrossRef] [PubMed]
- De Vries, H.; Mesters, I.; Van de Steeg, H.; Honing, C. The general public’s information needs and perceptions regarding hereditary cancer: An application of the Integrated Change Model. Patient Educ. Couns. 2005, 56, 154–165. [Google Scholar] [CrossRef]
- Grant, J.S.; Davis, L.L. Selection and use of content experts for instrument development. Res. Nurs. Health 1997, 20, 269–274. [Google Scholar] [CrossRef]
- Hasan, S.I.; Hairi, F.M.; Tajuddin, N.A.A.; Nordin, A.S.A. Empowering healthcare providers through smoking cessation training in Malaysia: A preintervention and postintervention evaluation on the improvement of knowledge, attitude and self-efficacy. Open 2019, 9, e030670. [Google Scholar] [CrossRef]
- Tabachnick BG, F.S. Using Multivariate Statistics; Pearson Education: Boston, MA, USA, 2013. [Google Scholar]
- Cronbach, L.J. Coefficient alpha and the internal structure of tests. Psychometrika 1951, 16, 297–334. [Google Scholar] [CrossRef] [Green Version]
- Charter, R.A. Sample Size Requirements for Precise Estimates of Reliability, Generalizability, and Validity Coefficients. J. Clin. Exp. Neuropsychol. 1999, 21, 559–566. [Google Scholar] [CrossRef] [PubMed]
- Bai, Y.; Li, J.; Bai, Y.; Ma, W.; Yang, X.; Ma, F. Development and validation of a questionnaire to evaluate the factors influencing training transfer among nursing professionals. BMC Health Serv. Res. 2018, 18, 107. [Google Scholar] [CrossRef] [PubMed]
- De Alwis, M.P.; Martire, R.L.; Äng, B.O.; Garme, K. Development and validation of a web-based questionnaire for surveying the health and working conditions of high-performance marine craft populations. BMJ Open 2016, 6, e011681. [Google Scholar] [CrossRef] [PubMed]
- Halek, M.; Holle, D.; Bartholomeyczik, S. Development and evaluation of the content validity, practicability and feasibility of the Innovative dementia-oriented Assessment system for challenging behaviour in residents with dementia. BMC Health Serv. Res. 2017, 17, 554. [Google Scholar] [CrossRef]
- Lau, X.C.; Wong, Y.L.; Wong, J.E.; Koh, D.; Sedek, R.; Jamil, A.T.; Ng, A.L.O.; Hazizi, A.S.; Ruzita, A.T.; Poh, B.K. Development and Validation of a Physical Activity Educational Module for Overweight and Obese Adolescents: CERGAS Programme. Int. J. Environ. Res. Public Health 2019, 16, 1506. [Google Scholar] [CrossRef] [PubMed]
- Martire, R.L.; De Alwis, M.P.; Äng, B.O.; Garme, K. Construction of a web-based questionnaire for longitudinal investigation of work exposure, musculoskeletal pain and performance impairments in high-performance marine craft populations. BMJ Open 2017, 7, e016006. [Google Scholar] [CrossRef]
- Polit DF, B.C. The content validity index: Are you sure you know what’s being reported? Critique and recommendations. Res. Nurs. Health 2006, 29, 489–497. [Google Scholar] [CrossRef]
- Shirali, G.; Shekari, M.; Angali, K.A. Assessing Reliability and Validity of an Instrument for Measuring Resilience Safety Culture in Sociotechnical Systems. Saf. Health Work 2018, 9, 296–307. [Google Scholar] [CrossRef]
- Cicchetti, D.V.; Sparrow, S.A. Developing criteria for establishing interrater reliability of specific items: Applications to assessment of adaptive behavior. Am. J. Ment. Defic. 1981, 86, 27–137. [Google Scholar]
- Allen, P.; Bennett, K.; Heritage, B. SPSS Statistics Version 22: A Practical Guide, 3rd ed.; Cengage Learning Australia Pty Limited: Sydney, Australia, 2014. [Google Scholar]
- Comrey, A.L.; Lee, H.B. A First Course in Factor Analysis, 2nd ed.; Lawrence Erlbaum Associates, Inc.: Hillsdale, NJ, USA, 1992; 443p. [Google Scholar]
- Floyd, F.J.; Widaman, K.F. Factor analysis in the development and refinement of clinical assessment instruments. Psychol. Assess. 1999, 7, 286–299. [Google Scholar] [CrossRef]
- Kistner, E.O.; Muller, K.E. Exact distributions of intraclass correlation and cronbach’s alpha with gaussian data and general covariance. Psychometrika 2004, 69, 459–474. [Google Scholar] [CrossRef] [PubMed]
- Uma Sekaran, R.B. Research Methods For Business: A Skill Building Approach, 7th ed.; Wiley: Hoboken, NJ, USA, 2016. [Google Scholar]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences; Taylor & Francis: London, UK, 2013. [Google Scholar]
- Gall, M.D.; Walter, J.P.G.; Borg, R. Educational Research: An Introduction, 8th ed.; Pearson: London, UK, 2006. [Google Scholar]
- Cattell, R.B. The three basic factor-analytic research designs—Their interrelations and derivatives. Psychol. Bull. 1952, 49, 499–520. [Google Scholar] [CrossRef] [PubMed]
- Shultz, K.S.; Whitney, D.J.; Zickar, M.J. Measurement Theory in Action: Case Studies and Exercises, 2nd ed.; Routledge/Taylor & Francis Group: New York, NY, USA, 2014; 424p. [Google Scholar]
- Martínez, C.; Castellano, Y.; Andres, A.; Fu, M.; Anton, L.; Ballbè, M.; Fernandez, P.; Cabrera, S.; Riccobene, A.; Gavilan, E.; et al. Factors associated with implementation of the 5A’s smoking cessation model. Tob. Induc. Dis. 2017, 15, 41. [Google Scholar] [CrossRef] [PubMed]
- Choi, S.-H.; Kim, Y.-H. Factors Affecting Korean Registered Nurses’ Intention to Implement Smoking Cessation Intervention. Osong Public Health Res. Perspect. 2016, 7, 63–70. [Google Scholar] [CrossRef]
- Conroy, M.B.; Majchrzak, N.E.; Regan, S.; Silverman, C.B.; Schneider, L.I.; Rigotti, N.A. The Association Between Patient-Reported Receipt of Tobacco Intervention at a Primary Care Visit and Smokers’ Satisfaction with their Health Care. Nicotine Tob. Res. 2005, 7, S29–S34. [Google Scholar] [CrossRef]
- Andrés, A.; Castellano, Y.; Fu, M.; Feliu, A.; Ballbè, M.; Antón, L.; Baena, A.; Fernández, E.; Martínez, C. Exploring individual and contextual factors contributing to tobacco cessation intervention implementation. Addict. Behav. 2019, 88, 163–168. [Google Scholar] [CrossRef]
- World Health Organization (WHO). WHO Tobacco Free Initiative: The Role of Health Professionals in Tobacco Control; World Health Organization (WHO): Geneva, Switzerland, 2005. [Google Scholar]
| Construct | Operational Definition | Items | Responses |
|---|---|---|---|
| Knowledge | Knowledge is information and understanding that you get from experience or education. | 1. Irritability 2. Depression 3. Restlessness 4. Poor concentration 5. Increased appetite 6. Weight gain 7. Lightheadedness 8. Nighttime awakening 9. Constipation 10. Diarrhea 11. Mouth ulcers 12. Urge to smoke | 0 = No 1 = Yes |
| Attitude | Attitude is the tendency, based on trust and experience, to respond to a smoking cessation intervention with specific methods and approaches. | 1. A patient’s chance of quitting smoking increases if the healthcare provider advises him/her to quit. 2. Patients want you to advise them to stop using any tobacco products. Healthcare providers like you should… 3. get specific training on smoking cessation counseling techniques. 4. set a good example for their patients and public by not using any tobacco products. 5. routinely ask patients about tobacco use. 6. routinely ask parents/guardians about tobacco use during pediatric visits. 7. routinely advise patients who use any tobacco products to quit. 8. routinely assist patients using any tobacco products to quit. | 1 = Strongly disagree 2 = Disagree 3 = Neither disagree/agree 4 = Agree 5 = Strongly agree |
| Self-efficacy | Self-efficacy is one’s belief in one’s ability to succeed in specific situations or accomplish a task in a smoking cessation intervention. Self-efficacy in this study refers to the confidence to provide a smoking cessation intervention using the 5 As brief intervention for smoking cessation. | 1. I know appropriate questions to ask my patients. 2. I am able to motivate my patients who are interested in quitting smoking. 3. I am able to assist patients to quit even if the patient thinks that it is difficult to give up. 4. I have the pharmacological therapy skills to assist patients to quit smoking. 5. I have the behavioral therapy skills to assist patients to quit smoking. 6. I can advise patients to consider smoking cessation. 7. I can provide counseling when time is limited. 8. I can counsel patients who are not interested in quitting. 9. I know how to prescribe medication (nicotine replacement therapy/bupropion) to treat tobacco dependency. 10. I can assess a patient’s different stages of readiness to quit smoking. 11. I can assess a patient’s level of nicotine dependency using the Fagerstrom test. 12. I can use a smokerlyzer to determine a patient’s carbon monoxide level. 13. I can assist recent quitters to learn how to cope with situations or triggers that might lead them to relapse to using tobacco. | 1 = Certainly not 2 = Probably not 3 = Neutral 4 = Probably 5 = Certainly |
| Behavior | Behavior is the way in which healthcare providers act in response to any particular situation or stimulus regarding smoking cessation interventions. Behavior in this study refers to the delivery of the 5 As brief intervention for smoking cessation. | In your current practice, how often do you… 1. ask patients whether they smoke? 2. ask patients the number of cigarettes smoked per day? 3. advise patients who smoke to quit smoking? 4. advise female patients to quit smoking if they are pregnant or planning to become pregnant? 5. advise patients to quit smoking if you think their illness is related to smoking? 6. assess patients’ readiness to quit smoking according to the stages of change below? a. precontemplation b. contemplation c. preparation d. action e. maintenance 7. assess reasons for quitting/continuing to quit smoking? 8. assist those who are not interested in quitting smoking to think about quitting? 9. assist those who are interested in quitting smoking to develop a plan to quit? 10. assist in setting quitting dates? 11. arrange referrals for appropriate smoking cessation services? 12. provide counseling for patients who want to quit smoking? 13. provide educational materials related to smoking cessation? 14. document tobacco-relevant discussions and plans in medical records? 15. use the Fagerstrom test to assess a patient’s level of addiction? 16. use a smokerlyzer to determine a patient’s carbon monoxide level? 17. prescribe or recommend the purchase of nicotine replacement therapy products for patients attempting to quit? 18. prescribe bupropion to those ready to quit smoking? (if applicable) 19. prescribe a combination of bupropion and nicotine replacement products to those ready to quit smoking? (if applicable) 20. prescribe second-line medications (e.g., clonidine, nortriptyline, bupropion) to patients ready to quit smoking? (if applicable) 21. provide treatment maintenance and follow-up services to those who have quit smoking? 22. arrange a follow-up visit or phone call to discuss quitting smoking? | 1 = Never 2 = Rarely 3 = Sometimes 4 = Often 5 = Always |
| Barrier | Barrier is a law, rule, or problem that makes something difficult or impossible or that might limit or prevent the capacity to offer a smoking cessation intervention for patients using the 5 As brief intervention for smoking cessation. | 1. Patients not interested in quitting smoking. 2. Patients not ready to change. 3. Patients do not comply with the given pharmacological therapy. 4. Patients do not comply with the given behavioral therapy. 5. Lack of impact of pharmacological therapy on patients. 6. Lack of impact of behavioral therapy on patients. 7. Lack of knowledge on smoking cessation. 8. Lack of time. 9. Other health problems require priority treatment. 10. Lack of reimbursement to healthcare providers. 11. Lack of community resources to which to refer patients. 12. Inadequate smoking cessation pharmaceutical drugs. 13. Lack of patient education materials. 14. Lack of smoking cessation training. 15. Complexity of smoking cessation guidelines. | 1 = Not a barrier 2 = Somewhat a barrier 3 = Moderate barrier 4 = Extreme barrier |
| Variable | Category | Frequency (n = 7) | Percentage (%) |
|---|---|---|---|
| Gender | Male | 4 | 57.14 |
| Female | 3 | 42.86 | |
| Region | Local | 3 | 42.86 |
| International | 4 | 57.14 | |
| Experience in tobacco control field | >10 years | 7 | 100.00 |
| Constructs | Items | Consistency | Representativeness | Relevancy | Clarity | Results | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| I-CVI * | k | I-CVI * | k | I-CVI * | k | I-CVI * | k | |||
| Knowledge | 1. Irritability | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | VALIDATED |
| 2. Depression | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | VALIDATED | |
| 3. Restlessness | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | VALIDATED | |
| 4. Poor concentration | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | VALIDATED | |
| 5. Increased appetite | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | VALIDATED | |
| 6. Weight gain | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | VALIDATED | |
| 7. Lightheadedness | 0.86 | 0.85 | 0.86 | 0.85 | 0.86 | 0.85 | 0.86 | 0.85 | VALIDATED | |
| 8. Nighttime awakening | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | VALIDATED | |
| 9. Constipation | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | VALIDATED | |
| 10. Diarrhea | 1 | 1 | 1 | t | 1 | 1 | 1 | 1 | VALIDATED | |
| 11. Mouth ulcers | 1 | 1 | 1 | 1 | 1 | 1 | 0.86 | 0.85 | VALIDATED | |
| Item 12 | 0.86 | 0.85 | 0.86 | 0.85 | 0.86 | 0.85 | 0.86 | 0.85 | VALIDATED | |
| S-CVI | 0.98 | 0.98 | 0.98 | 0.97 | ||||||
| Attitude | 1. A patient’s chance of quitting smoking increases if the healthcare provider advises him/her to quit. | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | VALIDATED |
| 2. Patients want you to advise them to stop using any tobacco products. | 0.86 | 0.85 | 0.86 | 0.85 | 0.86 | 0.85 | 0.86 | 0.85 | VALIDATED | |
| Healthcare providers like you should… | ||||||||||
| 3. get specific training on smoking cessation counseling techniques. | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | VALIDATED | |
| 4. set a good example for their patients and public by not using any tobacco products. | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | VALIDATED | |
| 5. routinely ask patients about tobacco use. | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | VALIDATED | |
| 6. routinely ask parents/guardians about tobacco use during pediatric visits. | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | VALIDATED | |
| 7. routinely advise patients who use any tobacco products to quit. | 1 | 1 | 1 | 1 | 1 | 1 | 0.86 | 0.85 | VALIDATED | |
| 8. routinely assist patients using any tobacco products to quit. | 1 | 1 | 1 | 1 | 1 | 1 | 0.86 | 0.85 | VALIDATED | |
| S-CVI | 0.98 | 0.98 | 0.98 | 0.95 | ||||||
| Self-efficacy | 1. I know appropriate questions to ask my patients. | 1 | 1 | 0.57 | 0.41 | 1 | 1 | 1 | 1 | VALIDATED |
| 2. I am able to motivate my patients who are interested in quitting smoking. | 1 | 1 | 0.71 | 0.66 | 1 | 1 | 1 | 1 | VALIDATED | |
| 3. I am able to assist patients to quit even if the patient thinks that it is difficult to give up. | 1 | 1 | 0.71 | 0.66 | 1 | 1 | 0.86 | 0.85 | VALIDATED | |
| 4. I have the pharmacological therapy skills to assist patients to quit smoking. | 1 | 1 | 0.57 | 0.41 | 1 | 1 | 1 | 1 | VALIDATED | |
| 5. I have the behavioral therapy skills to assist patients to quit smoking. | 1 | 1 | 0.71 | 0.66 | 1 | 1 | 1 | 1 | VALIDATED | |
| 6. I can advise patients to consider smoking cessation. | 0.86 | 0.85 | 0.57 | 0.41 | 0.71 | 0.66 | 1 | 1 | VALIDATED | |
| 7. I can provide counseling when time is limited. | 1 | 1 | 1 | 1 | 1 | 1 | 0.86 | 0.85 | VALIDATED | |
| 8. I can counsel patients who are not interested in quitting. | 1 | 1 | 1 | 1 | 0.86 | 0.85 | 1 | 1 | VALIDATED | |
| 9. I know how to prescribe medication (nicotine replacement therapy/bupropion) to treat tobacco dependency. | 0.86 | 0.85 | 1 | 1 | 1 | 1 | 1 | 1 | VALIDATED | |
| 10. I can assess a patient’s different stages of readiness to quit smoking. | 1 | 1 | 1 | 1 | 0.86 | 0.85 | 1 | 1 | VALIDATED | |
| 11. I can assess a patient’s level of nicotine dependency using the Fagerstrom test. | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | VALIDATED | |
| 12. I can use a smokerlyzer to determine a patient’s carbon monoxide level. | 1 | 1 | 0.86 | 0.85 | 1 | 1 | 1 | 1 | VALIDATED | |
| 13. I can assist recent quitters to learn how to cope with situations or triggers that might lead them to relapse in using tobacco. | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | VALIDATED | |
| S-CVI | 0.98 | 0.82 | 0.86 | 0.98 | ||||||
| Behavior | In your current practice, how often do you…. | |||||||||
| 1. ask patients whether they smoke? | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | VALIDATED | |
| 2. ask patients the number of cigarettes smoked per day? | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | VALIDATED | |
| 3. advise patients who smoke to quit smoking? | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | VALIDATED | |
| 4. advise female patients to quit smoking if they are pregnant or planning to become pregnant? | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | VALIDATED | |
| 5. advise patients to quit smoking if you think their illness is related to smoking? | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | VALIDATED | |
| 6. assess a patient’s readiness to quit smoking according to the stages of change below? | CORRECTED | |||||||||
| a. precontemplation | 0.71 | 0.66 | 0.71 | 0.66 | 0.57 | 0.41 | 0.71 | 0.66 | EXCLUDED | |
| b. contemplation | 0.71 | 0.66 | 0.71 | 0.66 | 0.57 | 0.41 | 0.71 | 0.66 | EXCLUDED | |
| c. preparation | 0.57 | 0.41 | 0.57 | 0.41 | 0.43 | 0.21 | 0.57 | 0.41 | EXCLUDED | |
| d. action | 0.57 | 0.41 | 0.57 | 0.41 | 0.43 | 0.21 | 0.57 | 0.41 | EXCLUDED | |
| e. maintenance | 0.57 | 0.41 | 0.57 | 0.41 | 0.43 | 0.21 | 0.57 | 0.41 | EXCLUDED | |
| 7. assess reasons for quitting/continuing to quit smoking? | 0.71 | 0.66 | 0.86 | 0.85 | 0.86 | 0.85 | 0.86 | 0.85 | VALIDATED | |
| 8. assist those who are not interested in quitting smoking to think about quitting? | 1 | 1 | 1 | 1 | 1 | 1 | 0.86 | 0.85 | VALIDATED | |
| 9. assist those who are interested in quitting smoking to develop a plan to quit? | 1 | 1 | 1 | 1 | 1 | 1 | 0.86 | 0.85 | VALIDATED | |
| 10. assist in setting quitting dates? | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | VALIDATED | |
| 11. arrange referrals for appropriate smoking cessation services? | 1 | 1 | 0.86 | 0.85 | 1 | 1 | 1 | 1 | VALIDATED | |
| 12. provide counseling for patients who want to quit smoking? | 0.86 | 0.85 | 0.86 | 0.85 | 1 | 1 | 0.86 | 0.85 | VALIDATED | |
| 13. provide educational materials related to smoking cessation? | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | VALIDATED | |
| 14. document tobacco-relevant discussions and plans in medical records? | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | VALIDATED | |
| 15. use the Fagerstrom test to assess a patient’s level of addiction? | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | VALIDATED | |
| 16. use a smokerlyzer to determine a patient’s carbon monoxide level? | 0.86 | 0.85 | 1 | 1 | 1 | 1 | 1 | 1 | VALIDATED | |
| 17. prescribe or recommend the purchase of nicotine replacement therapy products for patients attempting to quit? | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | VALIDATED | |
| 18. prescribe bupropion to those ready to quit smoking? (if applicable) | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | EXCLUDED | |
| 19. prescribe a combination of bupropion and nicotine replacement products to those ready to quit smoking? (if applicable) | 0.86 | 0.85 | 0.86 | 0.85 | 0.86 | 0.85 | 0.86 | 0.85 | EXCLUDED | |
| 20. prescribe second-line medications (e.g., clonidine, nortriptyline, bupropion) to patients ready to quit smoking? (if applicable) | 0.86 | 0.85 | 0.86 | 0.85 | 0.86 | 0.85 | 0.86 | 0.85 | EXCLUDED | |
| 21. provide treatment maintenance and follow-up services to those who have quit smoking? | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | VALIDATED | |
| 22. arrange a follow up visit or phone call to discuss quitting smoking? | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | VALIDATED | |
| S-CVI | 0.90 | 0.90 | 0.89 | 0.90 | ||||||
| Barriers | 1. Patients not interested in quitting smoking. | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | VALIDATED |
| 2. Patients not ready to change. | 1 | 1 | 1 | 1 | 0.86 | 0.85 | 1 | 1 | VALIDATED | |
| 3. Patients do not comply with the given pharmacological therapy. | 1 | 1 | 1 | 1 | 0.86 | 0.85 | 1 | 1 | VALIDATED | |
| 4. Patients do not comply with the given behavioral therapy. | 1 | 1 | 1 | 1 | 0.86 | 0.85 | 1 | 1 | VALIDATED | |
| 5. Lack of impact of pharmacological therapy on patients. | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | VALIDATED | |
| 6. Lack of impact of behavioral therapy on patients. | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | VALIDATED | |
| 7. Lack of knowledge on smoking cessation. | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | VALIDATED | |
| 8. Lack of time. | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | VALIDATED | |
| 9. Other health problems require priority treatment. | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | VALIDATED | |
| 10. Lack of reimbursement to healthcare providers. | 0.86 | 0.85 | 0.86 | 0.85 | 0.86 | 0.85 | 1 | 1 | VALIDATED | |
| 11. Lack of community resources to which to refer patients. | 1 | 1 | 0.86 | 0.85 | 0.86 | 0.85 | 1 | 1 | VALIDATED | |
| 12. Inadequate smoking cessation pharmaceutical drugs. | 1 | 1 | 0.86 | 0.85 | 0.86 | 0.85 | 1 | 1 | VALIDATED | |
| 13. Lack of patient education materials. | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | VALIDATED | |
| 14. Lack of smoking cessation training. | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | VALIDATED | |
| 15. Complexity of smoking cessation guidelines. | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | VALIDATED | |
| S-CVI | 0.99 | 0.97 | 0.94 | 1.0 | ||||||
| Variables | Category | Frequency (n) | Percentage (%) |
|---|---|---|---|
| Age | <33 years old | 238 | 59.1 |
| ≥33 years old | 165 | 40.9 | |
| Gender | Male | 151 | 37.5 |
| Female | 252 | 62.5 | |
| Ethnicity | Malay | 270 | 67.0 |
| Chinese | 93 | 23.1 | |
| Indian | 30 | 7.4 | |
| Others | 10 | 2.5 | |
| Religion | Islam | 278 | 69.2 |
| Buddhist | 66 | 16.4 | |
| Christian | 30 | 7.5 | |
| Hindu | 19 | 4.7 | |
| Others | 9 | 2.2 | |
| Education level | Diploma | 124 | 30.8 |
| Bachelor | 194 | 48.1 | |
| Master | 73 | 18.1 | |
| PhD | 2 | 0.5 | |
| Others | 10 | 2.5 | |
| Profession | Nurse | 72 | 17.9 |
| Medical assistant | 62 | 15.4 | |
| Doctor | 112 | 27.8 | |
| Dentist | 6 | 1.5 | |
| Pharmacist | 142 | 35.2 | |
| HEO | 4 | 1.0 | |
| Others | 5 | 1.2 | |
| Smoking status a | Current smoker | 14 | 3.5 |
| Former smoker | 28 | 7.0 | |
| Nonsmoker | 358 | 89.5 | |
| Working experience | <9 years | 247 | 61.3 |
| ≥9 years | 156 | 38.7 | |
| Smoking cessation training | Yes | 175 | 43.4 |
| No | 228 | 56.6 | |
| Interest in upgrading smoking cessation skills b | Not very interested | 17 | 4.30 |
| Not interested | 15 | 3.80 | |
| Somewhat interested | 161 | 40.6 | |
| Extremely interested | 204 | 51.4 |
| Construct | Items | Factor Loadings |
|---|---|---|
| Attitude | 7. Healthcare providers like you should routinely advise patients who use any tobacco products to quit. | 0.82 |
| 8. Healthcare providers like you should routinely assist patients using any tobacco products to quit. | 0.81 | |
| 3. Healthcare providers like you should get specific training on smoking cessation counseling techniques. | 0.81 | |
| 4. Healthcare providers like you should set a good example for their patients and the public by not using any tobacco products. | 0.80 | |
| 5. Healthcare providers like you should routinely ask patients about tobacco use. | 0.77 | |
| 6. Healthcare providers like you should routinely ask parents/guardians about tobacco use during pediatric visits. | 0.73 | |
| 1. A patient’s chance of quitting smoking increases if the healthcare provider advises him/her to quit. | 0.48 | |
| 2. Patients want you to advise them to stop using any tobacco products. | 0.40 | |
| Self-efficacy | 13. I can assist recent quitters to learn how to cope with situations or triggers that might lead them to relapse to using tobacco. | 0.82 |
| 10. I can assess a patient’s different stages of readiness to quit smoking. | 0.77 | |
| 5. I have the behavioral therapy skills to assist patients in quitting smoking. | 0.77 | |
| 4. I have the pharmacological therapy skills to assist patients in quitting smoking. | 0.76 | |
| 3. I am able to assist patients to quit even if the patient thinks that it is difficult to give up. | 0.75 | |
| 9. I know how to prescribe medication (nicotine replacement therapy/bupropion) to treat tobacco dependency. | 0.74 | |
| 11. I can assess a patient’s level of nicotine dependency using the Fagerstrom test. | 0.73 | |
| 8. I can counsel patients who are not interested in quitting. | 0.73 | |
| 7. I can provide counseling when time is limited. | 0.71 | |
| 1. I know appropriate questions to ask my patients. | 0.68 | |
| 2. I am able to motivate my patients who are interested in quitting smoking. | 0.67 | |
| 12. I can use a smokerlyzer to determine a patient’s carbon monoxide level. | 0.65 | |
| 6. I can advise patients to consider smoking cessation. | 0.57 | |
| Behavior | In your current practice, how often do you… | |
| 10. assist in setting quit dates? | 0.77 | |
| 7. assess reasons for quitting/continuing to quit smoking? | 0.76 | |
| 9. assist those who are interested in quitting smoking to develop a plan to quit? | 0.74 | |
| 6. assess patients’ readiness to quit smoking? | 0.74 | |
| 11. arrange referrals for appropriate smoking cessation services? | 0.74 | |
| 2. ask patients the number of cigarettes smoked per day? | 0.73 | |
| 14. document tobacco-relevant discussions and plans in medical records? | 0.73 | |
| 3. advise patients who smoke to quit smoking? | 0.72 | |
| 12. provide counseling for patients who want to quit smoking? | 0.71 | |
| 15. use the Fagerstrom test to assess a patient’s level of addiction? | 0.70 | |
| 22. arrange a follow up visit or phone call to discuss quitting smoking? | 0.68 | |
| 13 provide educational materials related to smoking cessation? | 0.67 | |
| 8. assist those who are not interested in quitting smoking to think about quitting? | 0.66 | |
| 1. ask patients whether they smoke? | 0.66 | |
| 21. provide treatment maintenance and follow-up services to those who have quit smoking? | 0.65 | |
| 16. use smokerlyzer to determine patient’s Carbon Monoxide level? | 0.65 | |
| 5. advise patients to quit smoking if you think their illness is related to smoking? | 0.64 | |
| 4. advise female patients to quit smoking if they are pregnant or planning to become pregnant? | 0.58 | |
| 17. prescribe or recommend the purchase of nicotine replacement therapy products for patients attempting to quit? | 0.55 | |
| Barrier | 6. Lack of impact of behavioral therapy on patients. | 0.72 |
| 5. Lack of impact of pharmacological therapy on patients. | 0.72 | |
| 7. Lack of knowledge on smoking cessation. | 0.71 | |
| 14. Lack of smoking cessation training. | 0.70 | |
| 11. Lack of community resources to which to refer patients. | 0.68 | |
| 4. Patients do not comply with the given behavioral therapy. | 0.67 | |
| 13. Lack of patient/client education materials. | 0.67 | |
| 15. Complexity of smoking cessation guidelines. | 0.66 | |
| 3. Patients do not comply with the given pharmacological therapy. | 0.65 | |
| 9. Other health problems require priority treatment. | 0.65 | |
| 12. Inadequate smoking cessation pharmaceutical drugs. | 0.62 | |
| 8. Lack of time. | 0.58 | |
| 10. Lack of reimbursement to healthcare providers. | 0.57 | |
| 2. Patients not ready to change. | 0.55 | |
| 1. Patients not interested in quitting smoking. | 0.50 |
| Construct | Items | N | Min. | Max. | Mean | SD | α |
|---|---|---|---|---|---|---|---|
| Attitude | 1.A patient’s chance of quitting smoking increases if the healthcare provider advises him/her to quit. | 403 | 1 | 5 | 3.93 | 0.82 | 0.89 |
| 2. Patients want you to advise them to stop using any tobacco products. | 403 | 1 | 5 | 3.70 | 0.86 | ||
| Healthcare providers like you should… | 403 | 1 | 5 | 4.51 | 0.68 | ||
| 3. get specific training on smoking cessation counseling techniques. | 403 | 1 | 5 | 4.54 | 0.66 | ||
| 4. set a good example for their patients and public by not using any tobacco products. | 403 | 1 | 5 | 4.26 | 0.74 | ||
| 5. routinely ask patients about tobacco use. | 403 | 1 | 5 | 4.20 | 0.76 | ||
| 6. routinely ask parents/guardians about tobacco use during pediatric visits. | 403 | 1 | 5 | 4.32 | 0.70 | ||
| 7. routinely advise patients who use any tobacco products to quit. | 403 | 1 | 5 | 4.33 | 0.71 | ||
| Total | 403 | 8 | 40 | 33.79 | 4.43 | ||
| Self-efficacy | 1. I know appropriate questions to ask my patients. | 403 | 1 | 5 | 3.72 | 0.90 | 0.94 |
| 2. I am able to motivate my patients who are interested in quitting smoking. | 403 | 1 | 5 | 3.75 | 0.86 | ||
| 3. I am able to assist patients to quit even if the patient thinks that it is difficult to give up. | 403 | 1 | 5 | 3.58 | 0.85 | ||
| 4. I have the pharmacological therapy skills to assist patients in quitting smoking. | 403 | 1 | 5 | 3.38 | 1.09 | ||
| 5. I have the behavioral therapy skills to assist patients in quitting smoking. | 403 | 1 | 5 | 3.23 | 1.03 | ||
| 6. I can advise patients to consider smoking cessation. | 403 | 1 | 5 | 3.98 | 0.75 | ||
| 7. I can provide counseling when time is limited. | 403 | 1 | 5 | 3.32 | 1.00 | ||
| 8. I can counsel patients who are not interested in quitting. | 403 | 1 | 5 | 3.21 | 0.98 | ||
| 9. I know how to prescribe medication (nicotine replacement therapy/bupropion) to treat tobacco dependency. | 403 | 1 | 5 | 3.07 | 1.21 | ||
| 10. I can assess a patient’s different stages of readiness to quit smoking. | 403 | 1 | 5 | 3.34 | 1.07 | ||
| 11. I can assess a patient’s level of nicotine dependency using the Fagerstrom test. | 403 | 1 | 5 | 3.28 | 1.27 | ||
| 12. I can use a smokerlyzer to determine a patient’s carbon monoxide level. | 403 | 1 | 5 | 2.96 | 1.37 | ||
| 13. I can assist recent quitters to learn how to cope with situations or triggers that might lead them to relapse to using tobacco. | 403 | 1 | 5 | 3.28 | 1.13 | ||
| Total | 403 | 13 | 65 | 44.09 | 10.41 | ||
| Behavior | In your current practice, how often do you…. | ||||||
| 1. ask patients whether they smoke? | 403 | 1 | 5 | 3.64 | 0.98 | 0.96 | |
| 2. ask patients the number of cigarettes smoked per day? | 403 | 1 | 5 | 3.46 | 1.04 | ||
| 3. advise patients who smoke to quit smoking? | 403 | 1 | 5 | 3.80 | 0.99 | ||
| 4. advise female patients to quit smoking if they are pregnant or planning to become pregnant? | 403 | 1 | 5 | 3.75 | 1.35 | ||
| 5. advise patients to quit smoking if you think their illness is related to smoking? | 403 | 1 | 5 | 4.17 | 0.92 | ||
| 6. assess a patient’s readiness to quit smoking? | 403 | 1 | 5 | 3.55 | 1.11 | ||
| 7. assess reasons for quitting/continuing to quit smoking? | 403 | 1 | 5 | 3.53 | 1.06 | ||
| 8. assist those who are not interested in quitting smoking to think about quitting? | 403 | 1 | 5 | 3.55 | 1.04 | ||
| 9. assist those who are interested in quitting smoking to develop a plan to quit? | 403 | 1 | 5 | 3.57 | 1.11 | ||
| 10. assist in setting quit dates? | 403 | 1 | 5 | 3.16 | 1.29 | ||
| 11. arrange referrals for appropriate smoking cessation services? | 403 | 1 | 5 | 3.16 | 1.25 | ||
| 12. provide counseling for patients who want to quit smoking? | 403 | 1 | 5 | 3.43 | 1.25 | ||
| 13. provide educational materials related to smoking cessation? | 403 | 1 | 5 | 3.20 | 1.24 | ||
| 14. document tobacco-relevant discussions and plans in medical records? | 403 | 1 | 5 | 2.94 | 1.35 | ||
| 15. use the Fagerstrom test to assess a patient’s level of addiction? | 403 | 1 | 5 | 2.86 | 1.52 | ||
| 16. use a smokerlyzer to determine a patient’s carbon monoxide level? | 403 | 1 | 5 | 2.45 | 1.52 | ||
| 17. prescribe or recommend the purchase of nicotine replacement therapy products for patients attempting to quit? | 403 | 1 | 5 | 2.90 | 1.42 | ||
| 21. provide treatment maintenance and follow-up services to those who have quit smoking? | 403 | 1 | 5 | 2.76 | 1.47 | ||
| 22. arrange a follow-up visit or phone call to discuss quitting smoking? | 403 | 1 | 5 | 2.67 | 1.44 | ||
| Total | 403 | 19 | 95 | 62.55 | 17.37 | ||
| Barrier | 1. Patients not interested in quitting smoking. | 403 | 1 | 4 | 3.30 | 0.78 | 0.90 |
| 2. Patients not ready to change. | 403 | 1 | 4 | 3.30 | 0.77 | ||
| 3. Patients do not comply with the given pharmacological therapy. | 403 | 1 | 4 | 3.00 | 0.80 | ||
| 4. Patients do not comply with the given behavioral therapy. | 403 | 1 | 4 | 2.99 | 0.76 | ||
| 5. Lack of impact of pharmacological therapy on patients. | 403 | 1 | 4 | 2.84 | 0.78 | ||
| 6. Lack of impact of behavioral therapy on patients. | 403 | 1 | 4 | 2.89 | 0.73 | ||
| 7. Lack of knowledge on smoking cessation. | 403 | 1 | 4 | 2.76 | 0.87 | ||
| 8. Lack of time. | 403 | 1 | 4 | 2.83 | 0.87 | ||
| 9. Other health problems require priority treatment. | 403 | 1 | 4 | 2.63 | 0.85 | ||
| 10. Lack of reimbursement to healthcare providers. | 403 | 1 | 4 | 2.44 | 0.90 | ||
| 11. Lack of community resources to which to refer patients. | 403 | 1 | 4 | 2.66 | 0.88 | ||
| 12. Inadequate smoking cessation pharmaceutical drugs. | 403 | 1 | 4 | 2.68 | 0.92 | ||
| 13. Lack of patient education materials. | 403 | 1 | 4 | 2.59 | 0.85 | ||
| 14. Lack of smoking cessation training. | 403 | 1 | 4 | 2.86 | 0.83 | ||
| 15. Complexity of smoking cessation guidelines. | 403 | 1 | 4 | 2.56 | 0.82 | ||
| Total | 403 | 15 | 60 | 42.33 | 8.00 |
| Constructs | Attitude | Self-Efficacy | Behavior | Barriers |
|---|---|---|---|---|
| Attitude | 1 | |||
| Self-efficacy | 0.27** | 1 | ||
| Behavior | 0.34** | 0.61** | 1 | |
| Barriers | 0.09 | −0.04 | 0.08 | 1 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hasan, S.I.; Mohd Hairi, F.; Amer Nordin, A.S.; Danaee, M. Development and Validation of an Evaluation Tool to Measure the Effectiveness of a Smoking Cessation Training among Healthcare Providers in Malaysia: The Providers’ Smoking Cessation Training Evaluation (ProSCiTE). Int. J. Environ. Res. Public Health 2019, 16, 4297. https://doi.org/10.3390/ijerph16214297
Hasan SI, Mohd Hairi F, Amer Nordin AS, Danaee M. Development and Validation of an Evaluation Tool to Measure the Effectiveness of a Smoking Cessation Training among Healthcare Providers in Malaysia: The Providers’ Smoking Cessation Training Evaluation (ProSCiTE). International Journal of Environmental Research and Public Health. 2019; 16(21):4297. https://doi.org/10.3390/ijerph16214297
Chicago/Turabian StyleHasan, Siti Idayu, Farizah Mohd Hairi, Amer Siddiq Amer Nordin, and Mahmoud Danaee. 2019. "Development and Validation of an Evaluation Tool to Measure the Effectiveness of a Smoking Cessation Training among Healthcare Providers in Malaysia: The Providers’ Smoking Cessation Training Evaluation (ProSCiTE)" International Journal of Environmental Research and Public Health 16, no. 21: 4297. https://doi.org/10.3390/ijerph16214297
APA StyleHasan, S. I., Mohd Hairi, F., Amer Nordin, A. S., & Danaee, M. (2019). Development and Validation of an Evaluation Tool to Measure the Effectiveness of a Smoking Cessation Training among Healthcare Providers in Malaysia: The Providers’ Smoking Cessation Training Evaluation (ProSCiTE). International Journal of Environmental Research and Public Health, 16(21), 4297. https://doi.org/10.3390/ijerph16214297






