Health Inequality Among the Elderly in Rural China and Influencing Factors: Evidence from the Chinese Longitudinal Healthy Longevity Survey
Abstract
1. Introduction
2. Materials and Methods
2.1. Data
2.2. Methods
2.2.1. Health Measures
2.2.2. Measurement of Health Inequality
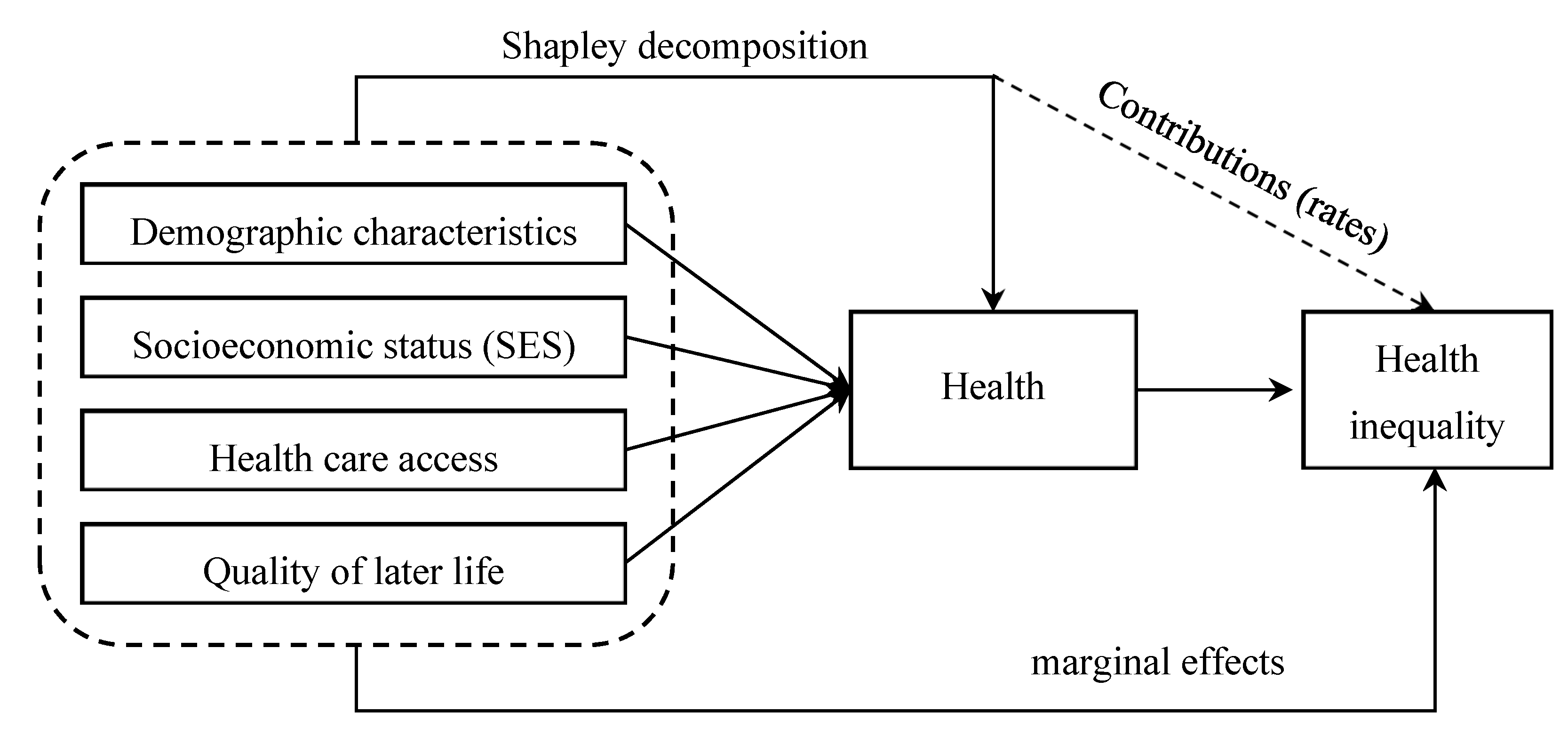
2.2.3. Decomposition Methods of Factors Influencing Health Inequality
2.3. Variables
2.3.1. Interpreted Variables
2.3.2. Explanatory Variables
3. Results
3.1. Health Characteristics of the Elderly in Rural China
3.2. Health Inequality Among the Elderly in Rural China
3.3. Decomposition of the Factors Affecting Health Inequality Among the Rural Elderly in China
3.3.1. Demographic Characteristics and Health Inequality Among the Rural Elderly
3.3.2. Socioeconomic Status (SES) and Health Inequality Among the Rural Elderly
3.3.3. Health Care Access and Health Inequality Among the Rural Elderly
3.3.4. Quality of Later Life and Health Inequality Among the Rural Elderly
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Organization, W.H. World report on ageing and health. Indian J. Med. Res. 2017, 1, 150–151. [Google Scholar]
- Wang, H.; Yu, Y. Increasing Health Inequality in China: An Empirical Study with Ordinal Data. J. Econ. Inequal. 2016, 1, 41–61. [Google Scholar] [CrossRef]
- Yang, W.; Kanavos, P. The less healthy urban population: Income-related health inequality in China. BMC Public Health 2012, 1, 804–819. [Google Scholar] [CrossRef] [PubMed]
- Poel, E.V.D.; Owen, O.D.; Doorslaer, E.V. Urbanization and the spread of diseases of affluence in China. Econ. Hum. Biol. 2009, 2, 200–216. [Google Scholar] [CrossRef] [PubMed]
- Zimmer, Z.; Wen, M.; Kaneda, T. A multi-level analysis of urban/rural and socioeconomic differences in functional health status transition among older Chinese. Soc. Sci. Med. 2010, 3, 559–567. [Google Scholar] [CrossRef]
- Zhong, Y.; Wang, J.; Nicholas, S. Gender, childhood and adult socioeconomic inequalities in functional disability among Chinese older adults. Int. J. Equity Health 2017, 16, 165–176. [Google Scholar] [CrossRef]
- Chen, L.; Wu, Y.; Coyte, P.C. Income-related children’s health inequality and health achievement in China. Int. J. Equity Health 2014, 13, 102–113. [Google Scholar] [CrossRef]
- Fang, P.Q.; Dong, S.P.; Xiao, J.J. Regional inequality in health and its determinants: Evidence from China. Health Policy 2010, 1, 14–25. [Google Scholar] [CrossRef]
- Pickett, K.E.; Wilkinson, R.G. Income inequality and health: A causal review. Soc. Sci. Med. 2015, 128, 316–326. [Google Scholar] [CrossRef]
- Bakkeli, N.Z. Income inequality and health in China: A panel data analysis. Soc. Sci. Med. 2016, 157, 39–47. [Google Scholar] [CrossRef]
- Chen, Z.; Yen, S.T.; Eastwood, D.B. Changing Health Inequality in China: The Role of Relative Income. In Investing in Human Capital for Economic Development in China; World Scientific Publishing: Singapore, 2010; pp. 261–275. [Google Scholar]
- Liu, J.F.; Chi, I.; Chen, G.; Song, X.; Zheng, X. Prevalence and correlates of functional disability in Chinese older adults. Geriatr. Gerontol. Int. 2009, 3, 253–261. [Google Scholar] [CrossRef] [PubMed]
- Hougaard, J.L.; Østerdal, L.P.; Yu, Y. The Chinese healthcare system. Appl. Health Econ. Health Policy 2011, 9, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Cai, J.L.; Coyte, P.C.; Zhao, H.Z. Decomposing the causes of socioeconomic-related health inequality among urban and rural populations in China: A new decomposition approach. Int. J. Equity Health 2017, 1, 128–142. [Google Scholar] [CrossRef] [PubMed]
- Kaplan, R.M.; Anderson, J.P. A general health policy model: Update and applications. Health Serv. Res. 1988, 2, 203–235. [Google Scholar]
- Wagstaff, A. Correcting the concentration index: A comment. J. Health Econ. 2009, 2, 516–520. [Google Scholar] [CrossRef]
- Erreygers, G.; Kessels, R. Regression-Based Decompositions of Rank-Dependent Indicators of Socioeconomic Inequality of Health. Res. Econ. Inequal. 2013, 21, 227–259. [Google Scholar]
- Shorrocks, A.F. Decomposition procedures for distributional analysis: A unified framework based on the Shapley value. J. Econ. Inequal. 2013, 1, 99–126. [Google Scholar] [CrossRef]
- Heckley, G.; Gerdtham, U.G.; Kjellsson, G. A general method for decomposing the causes of socioeconomic inequality in health. J. Health Econ. 2016, 48, 89–106. [Google Scholar] [CrossRef]
- Hampel, F.R. The Influence Curve and its Role in Robust Estimation. Publ. Am. Stat. Assoc. 1974, 69, 383–393. [Google Scholar] [CrossRef]
- Firpo, S.; Lemieux, F.T. Unconditional Quantile Regressions. Econometrica 2009, 3, 953–973. [Google Scholar]
- Monti, A.C. The study of the gini concentration ratio by means of the influence function. Statistica 1991, 51, 561–577. [Google Scholar]
- Pishkar, M.Z.; Jahantigh, M.; Arbabisarjou, A. Health Promotion Behaviors and Chronic Diseases of Aging in the Elderly People of Iranshahr. Glob. J. Health Sci. 2015, 3, 139–145. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Prus, S. Age, SES, and Health: A Population Level Analysis of Health Inequalities over the Life Course. Soc. Econ. Dimens. Aging Popul. Res. Pap. 2007, 2, 275–296. [Google Scholar]
- Fonta, L.C. Assessing Health Inequality among the Elderly in Ghana. Univ. Ghana 2015, 7, 1–78. [Google Scholar]
- Halliday, T. Health Inequality over the Life-Cycle. B.E. J. Econ. Anal. Policy 2011, 3, 1–34. [Google Scholar] [CrossRef]
- Witten, T.M. Life Course Analysis—The Courage to Search for Something More. J. Hum. Behav. Soc. Environ. 2003, 2, 189–224. [Google Scholar] [CrossRef]
- Wagstaff, A.; Watanabe, N. What difference does the choice of SES make in health inequality measurement? Health Econ. 2003, 10, 885–890. [Google Scholar] [CrossRef]
- Wagstaff, A.; Van Doorslaer, E. Income inequality and health: What does the literature tell us? Sick Inequal. 2016, 1, 543–567. [Google Scholar] [CrossRef]
- Tian, X.C.; Ying, W.; Xiao, Y.L.; Yu, X.R.; Lei, H. Inter-provincial inequality of public health services in China: The perspective of local officials’ behavior. Int. J. Equity Health 2018, 1, 108–123. [Google Scholar]
- Phaswana, M.N.; Peltzer, K.; Chirinda, W. Self-rated health and associated factors among older South Africans: Evidence from the study on global ageing and adult health. Glob. Health Action 2013, 6, 19880–19890. [Google Scholar] [CrossRef]
- Zhang, Z.H.; Luo, Y.X.; Robinson, D. Reducing Food Poverty and Vulnerability among the Rural Elderly with Chronic Diseases: The Role of the New Rural Pension Scheme in China. Int. J. Environ. Res. Public Health 2018, 6, 1253. [Google Scholar] [CrossRef] [PubMed]

| Year | Sample of Survey Year | Continuous Survey Sample | Survey Year Rural Sample | Rural Sample for Continuous Survey |
|---|---|---|---|---|
| 2002 | 16,064 | — | 8670 | — |
| 2005 | 15,638 | 8175 (2002–2005) | 8658 | 4337 |
| 2008 | 16,954 | 4191 (2002–2008) | 10,293 | 1897 |
| 2011 | 9765 | 2513 (2002–2011) | 5145 | 737 |
| 2014 | 7192 | 1681 (2002–2014) | 3980 | 332 |
| Content | Weight | Questionnaire No. | |
|---|---|---|---|
| Mobility Scale (MOB) | |||
| 4 | Did not drive a car, health related; did not ride in a car as usual for age (younger than 15 yr), health related, and/or did not use public transportation, health related; or had or would have used more help than usual for age to use public transportation, health related. | −0.062 | E4, E14 |
| Physical Activity Scale (PAC) | |||
| 3 | In wheelchair, moved or controlled movement of wheelchair without help from someone else; or had trouble or did not try to lift, stoop, bend over, or use stairs or inclines, health related; and/or limped, used a cane, crutches, or walker, health related; and/or had any other physical limitation in walking, or did not try to walk as far or as fast as others the same age are able, health related. | −0.060 | G9, G11, E11–E13 |
| Social Activity Scale (SAC) | |||
| 4 | Limited in other (e.g., recreational) role activity, health related. | −0.061 | E6–E8 |
| 3 | Limited in major (primary) role activity, health related. | −0.061 | E2–E3 |
| 2 | Performed no major role activity, health related, but did perform self-care activities. | −0.061 | E3 |
| 1 | Performed no major role activity, health related, and did not perform, or had more help than usual in performance of one or more self-care activities, health related. | −0.106 | E1–E3, E6, E9–E10 |
| Symptom/Problem Complexes (CPX) | |||
| 5 | Trouble learning, remembering, or thinking clearly. | −0.340 | C54–C55, G15O1 |
| 6 | Any combination of one or more hands, feet, arms, or legs either missing, deformed (crooked), paralyzed (unable to move), or broken—includes wearing artificial limbs or braces. | −0.333 | C55 |
| 8 | Pain, burning, bleeding, itching, or other difficulty with rectum, bowel movements, or urination (passing water). | −0.292 | E5, G15B1, G15S1 |
| 12 | Spells of feeling upset, being depressed, or of crying. | −0.257 | B23–B24, B26 |
| 18 | Pain in ear, tooth, jaw, throat, lips, tongue; several missing or crooked permanent teeth—includes wearing bridges or false teeth; stuffy, runny nose; or any trouble hearing-includes wearing a hearing aid. | −0.170 | C55, G22, H1 |
| Variables | Description | Mean ± SD or n (%) |
|---|---|---|
| Health Status | QWB Score | 0.6276 ± 0.1500 |
| Demographic characteristics | ||
| Gender | Male | 7923 (40.96) |
| Female | 11,418 (59.04) | |
| Age groups | Age group1 (65–74) | 2149 (11.11) |
| Age group2 (75–84) | 3255 (16.83) | |
| Age group3 (85–94) | 6980 (36.09) | |
| Age group4 (95+) a | 6957 (35.97) | |
| Marital status | Married | 4728 (24.45) |
| Divorced, separated, widowed, or single | 14,613 (75.55) | |
| Socioeconomic status (SES) | ||
| Income inequality | Gini coefficient of province | 0.3677 ± 0.0749 |
| Education | Years of education | 1.3810 ± 2.6982 |
| Region | Eastern China a | 8001 (41.37) |
| Central China | 6313 (32.64) | |
| Western China | 5027 (25.99) | |
| Health care access | ||
| Timely medical treatment | Yes | 17,037 (88.09) |
| No | 2304 (11.91) | |
| Medical facilities | Number of medical institution beds per 1000 people | 1.0190 ± 0.4847 |
| Medical expenses | Total medical expenses last year (yuan) | 1,343.0770 ± 4,827.2570 |
| Main medical payment channel | Medical insurance | 3294 (17.03) |
| Other | 16,047 (82.97) | |
| Quality of later life | ||
| Living arrangements | Living in nursing homes | 346 (1.79) |
| Not living in nursing homes | 18,995 (98.21) | |
| Pension | Yes | 996 (5.15) |
| No | 18,345 (94.85) | |
| Physical exercise | Yes | 3513 (18.16) |
| No | 15,828 (81.84) | |
| 2002 | 2005 | 2008 | 2011 | 2014 | |
|---|---|---|---|---|---|
| 65–74 years old | 0.7730 | 0.7772 | 0.7832 | 0.7810 | 0.7770 |
| 75–84 years old | 0.7128 | 0.7157 | 0.7197 | 0.7233 | 0.7276 |
| 85–94 years old | 0.6357 | 0.6478 | 0.6396 | 0.6433 | 0.6600 |
| Above 95 years old | 0.5639 | 0.5747 | 0.5627 | 0.5725 | 0.5868 |
| 2002 | 2005 | 2008 | 2011 | 2014 | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| WI | EI | WI | EI | WI | EI | WI | EI | WI | EI | |
| 65–74 years old | 0.0870 | 0.0826 | 0.0595 | 0.0567 | 0.1060 | 0.1030 | 0.0734 | 0.0716 | 0.0379 | 0.0360 |
| 75–84 years old | 0.0557 | 0.0534 | 0.0818 | 0.0790 | 0.0474 | 0.0455 | 0.0063 | 0.0061 | 0.0784 | 0.0763 |
| 85–94 years old | 0.0517 | 0.0516 | 0.0322 | 0.0322 | 0.0352 | 0.0351 | 0.0031 | 0.0031 | 0.0035 | 0.0035 |
| Above 95 years old | 0.0379 | 0.0377 | 0.0575 | 0.0574 | 0.0124 | 0.0123 | 0.0232 | 0.0231 | 0.0279 | 0.0276 |
| Dimensions | Variables | Shapley Decomposition | RIF-I-OLS Decomposition | ||
|---|---|---|---|---|---|
| Health (QWB) | Contribution (rate, %) | RifWI | RifEI | ||
| Demographic characteristics | Male | 0.0083 | 0.0054 (6.40%) | −0.0058 | −0.0064 |
| (0.4263) | (−0.8537) | (−1.0205) | |||
| Age group1 (65–74) | 0.0293 | 0.0664 *** | 0.0545 *** | ||
| (0.8888) | (4.9352) | (4.3412) | |||
| Age group2 (75–84) | −0.1525 *** | 0.0263 *** | 0.0198 ** | ||
| (-5.6868) | (2.6841) | (2.1718) | |||
| Age group3 (85–94) | −0.0962 *** | 0.0084 | 0.0057 | ||
| (−4.6733) | (1.2847) | (0.9398) | |||
| Married | −0.0264 | 0.0176 ** | 0.0156 * | ||
| (−1.1330) | (2.0328) | (1.9386) | |||
| Socioeconomic status (SES) | Gini coefficient | −1.2790 *** | 0.0130 (15.39%) | 0.5882 *** | 0.5440 *** |
| (−4.0629) | (5.1053) | (5.0656) | |||
| Years of education | 0.0130 *** | 0.0041 *** | 0.0037 *** | ||
| (3.5411) | (2.8928) | (2.8011) | |||
| Central China | −0.1482 *** | 0.0091 | 0.0084 | ||
| (−7.0585) | (1.2016) | (1.1894) | |||
| Western China | −0.1238 *** | −0.0338 *** | −0.0323 *** | ||
| (−4.6590) | (−3.4009) | (−3.4806) | |||
| Health care access | Timely medical treatment | 0.4802 *** | 0.0442 (52.41%) | −0.0286 *** | −0.0284 *** |
| (16.6442) | (-3.1046) | (−3.2866) | |||
| Medical facilities | 0.0679 *** | −0.0131 * | −0.0116 * | ||
| (3.0847) | (−1.7954) | (−1.7222) | |||
| Medical expenses | −4.3496 *** | −0.5795 *** | −0.5206 *** | ||
| (−9.0786) | (−5.6915) | (−5.5188) | |||
| Insurance payment | 0.0438 * | 0.0167 * | 0.0153 * | ||
| (1.9154) | (1.7990) | (1.7748) | |||
| Quality of later life | Living in nursing homes | −0.0826 | 0.0218 (25.80%) | −0.1111 *** | −0.1031 *** |
| (−1.0760) | (−3.4715) | (−3.4544) | |||
| Pension | 0.0745 * | 0.0612 *** | 0.0575 *** | ||
| (1.9425) | (3.8966) | (3.9514) | |||
| Physical exercise | 0.3221 *** | 0.0257 *** | 0.0216 *** | ||
| (15.4757) | (3.1152) | (2.8047) | |||
| Constant | 3.5439 *** | — | −0.1451 *** | −0.1295 *** | |
| (26.8070) | — | (−3.0643) | (−2.9365) | ||
| Time fixed effect | Controlled | — | Controlled | Controlled | |
| Total Contribution | — | — | 0.0844 (100%) | — | — |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pan, C.; Fan, Q.; Yang, J.; Deng, D. Health Inequality Among the Elderly in Rural China and Influencing Factors: Evidence from the Chinese Longitudinal Healthy Longevity Survey. Int. J. Environ. Res. Public Health 2019, 16, 4018. https://doi.org/10.3390/ijerph16204018
Pan C, Fan Q, Yang J, Deng D. Health Inequality Among the Elderly in Rural China and Influencing Factors: Evidence from the Chinese Longitudinal Healthy Longevity Survey. International Journal of Environmental Research and Public Health. 2019; 16(20):4018. https://doi.org/10.3390/ijerph16204018
Chicago/Turabian StylePan, Changjian, Qiuyan Fan, Jing Yang, and Dasong Deng. 2019. "Health Inequality Among the Elderly in Rural China and Influencing Factors: Evidence from the Chinese Longitudinal Healthy Longevity Survey" International Journal of Environmental Research and Public Health 16, no. 20: 4018. https://doi.org/10.3390/ijerph16204018
APA StylePan, C., Fan, Q., Yang, J., & Deng, D. (2019). Health Inequality Among the Elderly in Rural China and Influencing Factors: Evidence from the Chinese Longitudinal Healthy Longevity Survey. International Journal of Environmental Research and Public Health, 16(20), 4018. https://doi.org/10.3390/ijerph16204018




