Parental Approach to the Management of Childhood Fever: Differences between Health Professional and Non-Health Professional Parents
Abstract
:1. Introduction
2. Methods
2.1. Participants/Sample
2.2. Data Collection
2.3. Data Analysis
2.4. Ethical Considerations
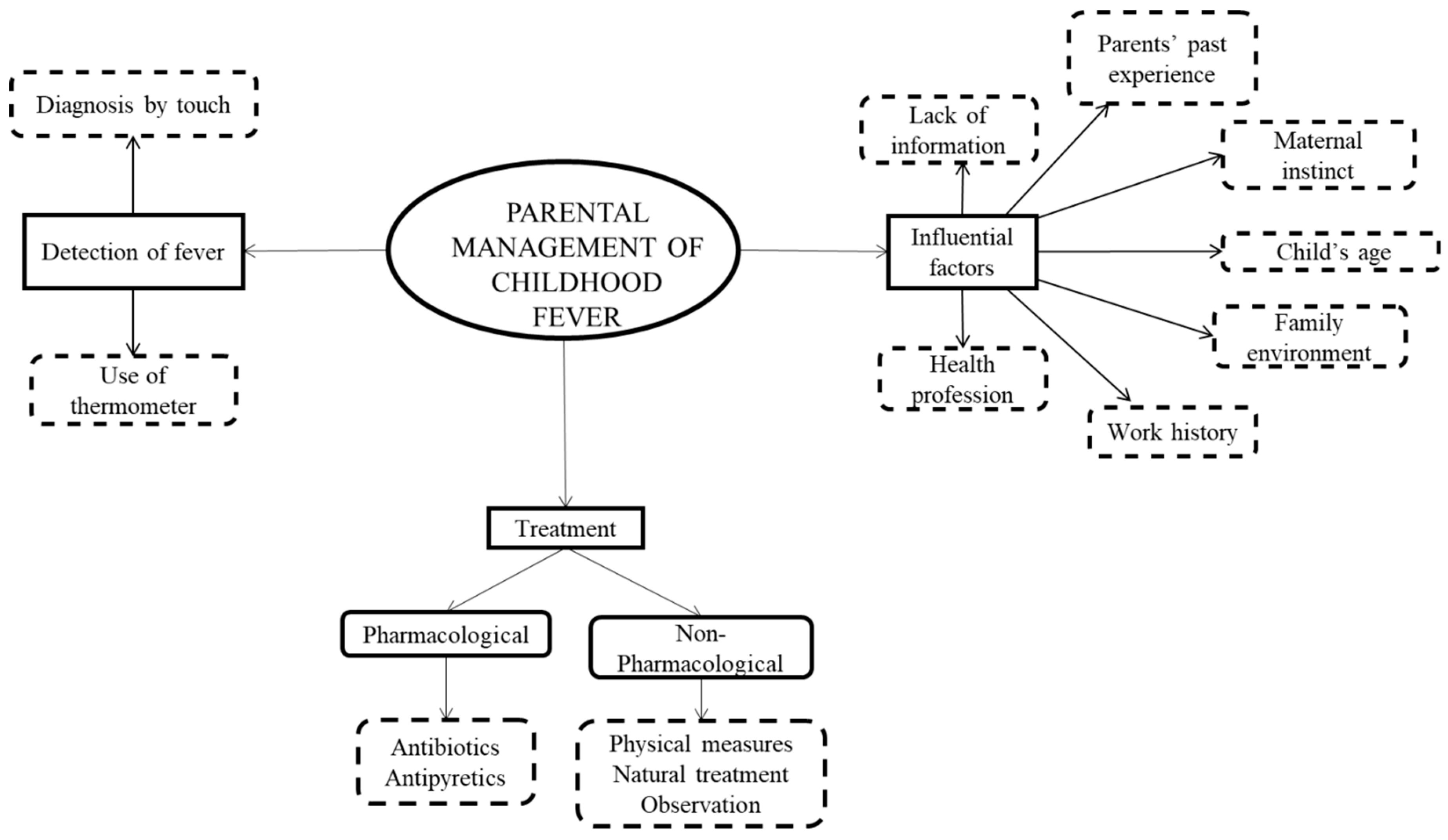
3. Results
3.1. Methods for Fever Detection
3.2. Fever Treatment
3.2.1. Pharmacological Treatment
3.2.2. Non-Pharmacological Treatment
3.3. Determinant Factors in Parents’ Management of Fever
4. Discussion
5. Study Strengths and Limitations
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- El-Radhi, A.S.; Barry, W. Thermometry in paediatric practice. Arch. Dis. Child. 2006, 91, 351–356. [Google Scholar] [CrossRef] [PubMed]
- Rajput, U.C.; Kulkarni, S.; Wagh, S.S. Parental Knowledge, Attitude and Practices Regarding Fever in Their Children: A Hospital Based Observational Study. Int. J. Recent Trends Sci. Technol. 2014, 10, 517–520. [Google Scholar]
- Sullivan, J.E.; Farrar, H.C. Fever and antipyretic use in children. Pediatrics 2011, 127, 580–587. [Google Scholar] [CrossRef] [PubMed]
- Fields, E.; Chard, J.; Murphy, M.S.; Richardson, M. Assessment and initial management of feverish illness in children younger than 5 years: Summary of updated NICE guidance. BMJ 2013, 346, 35–37. [Google Scholar] [CrossRef]
- Boivin, J.M.; Weber, F.; Fay, R.; Monin, P. Management of paediatric fever: Is parents’ skill appropriate? Arch. Pediatr. Organe Off. Soc. Fr. Pediatr. 2007, 14, 322–329. [Google Scholar] [CrossRef]
- Hoover, L. AAP reports on the use of antipyretics for fever in children. Am. Fam. Physician 2012, 1, 518–519. [Google Scholar]
- Nadal, C.; Garía de Miguel, M.; Campderá, A. Effectiveness and tolerability of ibuprofen-arginine versus paracetamol in children with fever of likely infectious origin. Acta Paediatr. 2002, 91, 383–390. [Google Scholar] [CrossRef]
- Schmitt, B.D. Fever in childhood. Pediatrics 1984, 74, 929–936. [Google Scholar]
- Crocetti, M.; Moghbeli, N.; Serwint, J. Fever phobia revisited: Have parental misconceptions about fever changed in 20 years. Pediatrics 2001, 107, 1241–1246. [Google Scholar] [CrossRef]
- Villarejo-Rodríguez, M.G.; Rodríguez-Martín, B. A Qualitative Study of Parents’ Conceptualizations on Fever in Children Aged 0 to 12 Years. Int. J. Environ. Res. Public Health 2019, 16, 29–59. [Google Scholar] [CrossRef]
- Cohee, L.; Crocetti, M.; Serwint, J.; Sabath, B.; Kapoor, S. Ethnic differences in parental perceptions and management of childhood fever. Clin. Pediatr. 2010, 49, 221–227. [Google Scholar] [CrossRef] [PubMed]
- Villarejo-Rodríguez, M.G.; Rodríguez-Martín, B. Parents’ and primary caregivers’ conceptualizations of fever in children: A systematic review of qualitative studies. Nurs. Health Sci. 2019, 1–34. [Google Scholar] [CrossRef] [PubMed]
- Sherman, J.M.; Sood, S.K. Current challenges in the diagnosis and management of fever. Curr. Opin. Pediatr. 2012, 24, 400–406. [Google Scholar] [CrossRef] [PubMed]
- Bilenko, N.; Tessler, H.; Okbe, R.; Press, J.; Gorodischer, R. Determinants of antipyretic misuse in children up to 5 years of age: A cross-sectional study. Clin. Ther. 2006, 28, 783–793. [Google Scholar] [CrossRef]
- Purssell, E. Parental fever phobia and its evolutionary correlates. J. Clin. Nurs. 2009, 18, 210–218. [Google Scholar] [CrossRef]
- Monsma, J.; Richerson, J.; Sloand, E. Empowering parents for evidence-based fever management: An integrative review. J. Am. Assoc. Nurse Pract. 2015, 27, 222–229. [Google Scholar] [CrossRef]
- Peetoom, K.K.; Smits, J.J.; Ploum, L.J.; Verbakel, J.Y.; Dinant, G.J.; Cals, J.W. Does well-child care education improve consultations and medication management for childhood fever and common infections? A systematic review. Arch. Dis. Child. 2017, 102, 261–267. [Google Scholar] [CrossRef]
- Hay, A.D.; Heron, J.; Ness, A. The prevalence of symptoms and consultations in pre-school children in the Avon Longitudinal Study of Parents and Children (ALSPAC): A prospective cohort study. Fam. Pract. 2005, 22, 367–374. [Google Scholar] [CrossRef]
- Davidson, S.K.; Schattner, P.L. Doctors’ health-seeking behaviour: A questionnaire survey. Med. J. Aust. 2003, 179, 302–305. [Google Scholar] [CrossRef]
- Forsythe, M.; Calnan, M.; Wall, B. Doctors as patients: Postal survey examining consultants and general practitioners adherence to guidelines. BMJ 1999, 319, 605–608. [Google Scholar] [CrossRef]
- Tyssen, R. The physician-patient relationship when the patient is a physician. Tidsskr. Den Nor. Legeforening 2001, 121, 3533–3535. [Google Scholar]
- Strauss, A.; Corbin, J. Techniques and procedures for developing Grounded Theory. In Basic of Qualitative Research; Sage Publications: Thousand Oaks, CA, USA, 1998. [Google Scholar]
- Fram, S.M. The constant comparative analysis method outside of grounded theory. Qual. Rep. 2013, 18, 1–25. [Google Scholar]
- Carter, N.; Bryant-Lukosius, D.; DiCenso, A.; Blythe, J.; Neville, A. The Use of Triangulation in Qualitative Research. Oncol. Nurs. Forum 2014, 41, 545–547. [Google Scholar] [CrossRef] [PubMed]
- Hancock, M.E.; Amankwaa, L.; Revell, M.A.; Mueller, D. Focus Group Data Saturation: A New Approach to Data Analysis. Qual. Rep. 2016, 21, 2124–2130. [Google Scholar]
- Barbour, R.S. Using focus groups in general practice research. Fam. Pract. 1995, 12, 328–334. [Google Scholar] [CrossRef]
- Krueger, R.A.; Casey, M.A. Focus Groups: A Practical Guide for Applied Research, 3rd ed.; Sage Publications: Thousand Oaks, CA, USA, 2000. [Google Scholar]
- Thomas, D.R. A general inductive approach for analyzing qualitative evaluation data. Am. J. Eval. 2006, 27, 237–246. [Google Scholar] [CrossRef]
- Spanish Personal Data Protection Law. Organic law 15/1999, of December 13. Official Bulletin of the State, nº 298 (14 December 1999). Available online: https://www.boe.es/buscar/pdf/1999/BOE-A-1999-23750-consolidado.pdf (accessed on 15 June 2019).
- Sahm, L.J.; Kelly, M.; McCarthy, S.; O’Sullivan, R.; Shiely, F.; Rømsing, J. Knowledge, attitudes and beliefs of parents regarding fever in children: A Danish interview study. Acta Paediatr. 2016, 105, 69–73. [Google Scholar] [CrossRef]
- Walsh, A.; Edwards, H.; Fraser, J. Influences on parents’ fever management: Beliefs, experiences and information sources. J. Clin. Nurs. 2007, 16, 2331–2340. [Google Scholar] [CrossRef]
- Wun, Y.; Lam, T.P.; Lam, K.F.; Sun, K.S. Antibiotic use: Do parents act differently for their children? Int. J. Clin. Pract. 2012, 66, 1197–1203. [Google Scholar] [CrossRef]
- Vernacchio, L.; Kelly, J.; Kaufman, D.; Mitchell, A. Medication use among children 12 years of age in the United States: Results from the Slone Survey. Pediatrics 2009, 124, 446–454. [Google Scholar] [CrossRef]
- Sa’ed, H.Z.; Al-Jabi, S.W.; Sweileh, W.M.; Nabulsi, M.M.; Tubaila, M.F.; Awang, R.; Sawalha, A.F. Beliefs and practices regarding childhood fever among parents: A cross-sectional study from Palestine. BMC Pediatr. 2013, 13, 66–73. [Google Scholar] [CrossRef]
- Fallah Tafti, B.; Salmani, N.; Afshari, S. The Maternal Experiences of Child Care with Fever: A Qualitative Study. Int. J. Pediatr. 2017, 5, 4429–4437. [Google Scholar] [CrossRef]
- Meremikwu, M.; Oyo-Ita, A. Paracetamol versus placebo or physical methods for treating fever in children. Cochrane Libr. 2009, 2, 1–3. [Google Scholar] [CrossRef] [PubMed]
- De Bont, E.G.; Peetoom, K.K.; Moser, A.; Francis, N.A.; Dinant, G.J.; Cals, J.W. Childhood fever: A qualitative study on GPs’ experiences during out-of-hours care. Fam. Pract. 2015, 32, 449–455. [Google Scholar] [CrossRef]
- Delgado, M.F.; Sierra, C.H.; Calvache, J.A.; Ríos, Á.M.; Mosquera, C.; Salas, I.; Agredo, F.; Meneses, R. Maternal knowledge about children’s danger signs in acute diarrhoea in an IMCI’s frame. Colomb. Méd. 2006, 37, 293–298. [Google Scholar]
- Tong, A.; Sainsbury, P.; Craig, J. Consolidated criteria for reporting qualitative research (COREQ): A 32-item checklist for interviews and focus groups. Int. J. Qual. Health Care 2007, 19, 349–357. [Google Scholar] [CrossRef]
- Morse, J.M.; Barrett, M.; Mayan, M.; Olson, K.; Spiers, J. Verification strategies for establishing reliability and validity in qualitative research. Int. J. Qual. Methods 2002, 1, 13–22. [Google Scholar] [CrossRef]
- Mays, N.; Pope, C. Assessing quality in qualitative research. BMJ 2000, 320, 50–52. [Google Scholar] [CrossRef]
| Sex | 27 Men | 30 Women | ||||
|---|---|---|---|---|---|---|
| Age | <30 years | 0 | 4 | |||
| 30–40 years | 15 | 14 | ||||
| >40 years | 12 | 12 | ||||
| Civil status | Single | 0 | 0 | |||
| Married | 26 | 30 | ||||
| Divorced | 1 | 0 | ||||
| Number of children | 1 | 7 | 12 | |||
| 2 | 11 | 13 | ||||
| 3–4 | 7 | 5 | ||||
| >4 | 2 | 0 | ||||
| Level of studies | No studies | 0 | 0 | |||
| Primary studies | 4 | 2 | ||||
| Secondary studies | 6 | 9 | ||||
| University education: diploma, degree, bachelor’s degree | 16 | 18 | ||||
| Master/doctorate | 1 | 1 | ||||
| Place of residence (environment) | Rural | 13 | 16 | |||
| Urban | 14 | 14 | ||||
| Profession | Active | Not active | Active | Not active | ||
| Non-health professional | 11 | 3 | 10 | 5 | ||
| Health professional | Doctor | 7 | 0 | 7 | 0 | |
| Nurse | 4 | 0 | 8 | 0 | ||
| Nurse aid/Health technician | 2 | 0 | 0 | 0 | ||
| Parents with Health Education | Parents Without Health Education | ||
|---|---|---|---|
| Rural area | Mothers | 8 | 8 |
| Fathers | 6 | 7 | |
| Urban area | Mothers | 7 | 7 |
| Fathers | 7 | 7 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Villarejo-Rodríguez, M.G.; Rodríguez-Martín, B. Parental Approach to the Management of Childhood Fever: Differences between Health Professional and Non-Health Professional Parents. Int. J. Environ. Res. Public Health 2019, 16, 4014. https://doi.org/10.3390/ijerph16204014
Villarejo-Rodríguez MG, Rodríguez-Martín B. Parental Approach to the Management of Childhood Fever: Differences between Health Professional and Non-Health Professional Parents. International Journal of Environmental Research and Public Health. 2019; 16(20):4014. https://doi.org/10.3390/ijerph16204014
Chicago/Turabian StyleVillarejo-Rodríguez, María Gloria, and Beatriz Rodríguez-Martín. 2019. "Parental Approach to the Management of Childhood Fever: Differences between Health Professional and Non-Health Professional Parents" International Journal of Environmental Research and Public Health 16, no. 20: 4014. https://doi.org/10.3390/ijerph16204014
APA StyleVillarejo-Rodríguez, M. G., & Rodríguez-Martín, B. (2019). Parental Approach to the Management of Childhood Fever: Differences between Health Professional and Non-Health Professional Parents. International Journal of Environmental Research and Public Health, 16(20), 4014. https://doi.org/10.3390/ijerph16204014






