Toileting Behaviors Related to Urination in Women: A Scoping Review
Abstract
1. Introduction
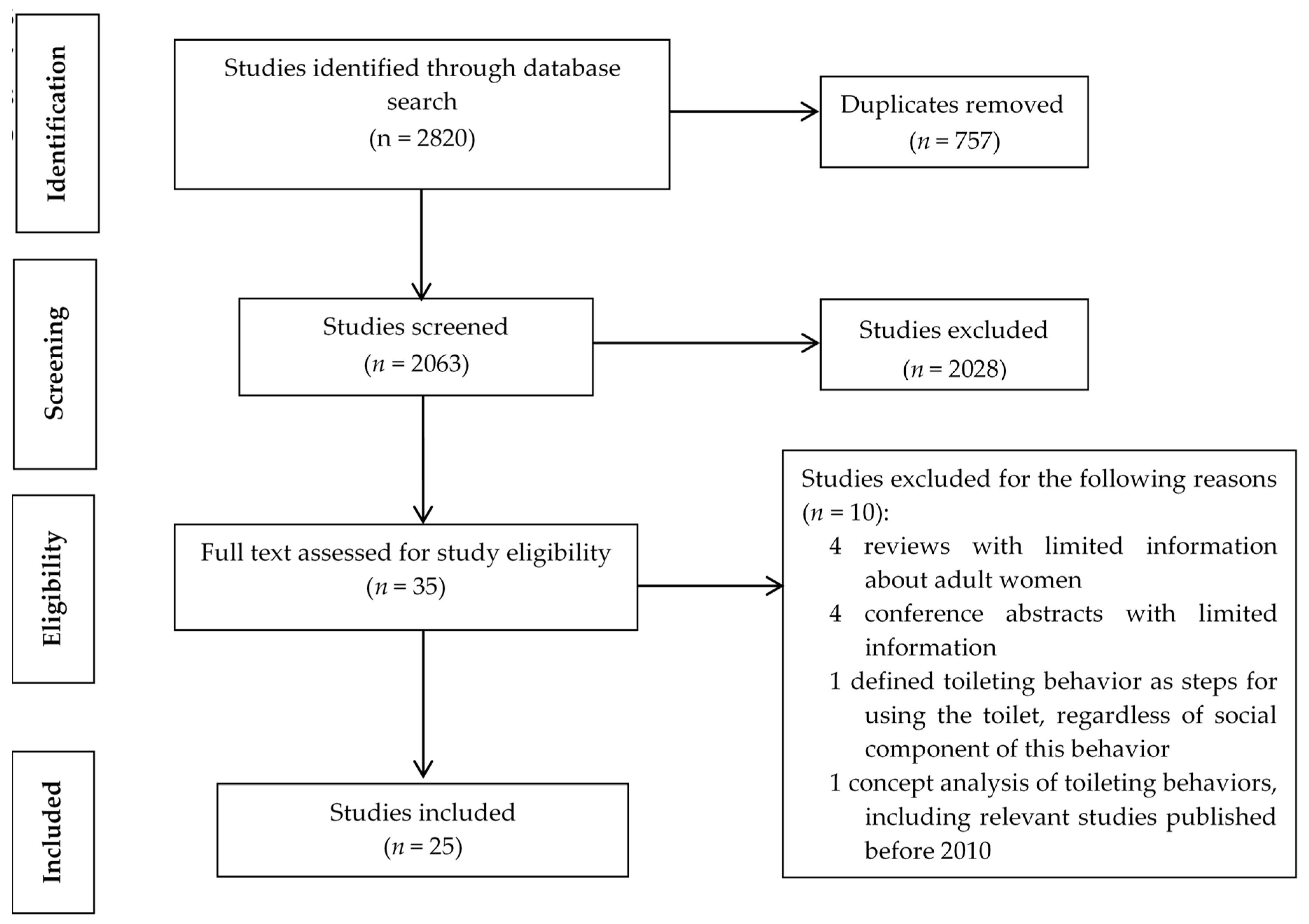
2. Methods
2.1. Inclusion and Exclusion Criteria
2.2. Search Strategy
2.3. Screening Strategy
2.4. Information Extracting and Synthesis Strategy
3. Results
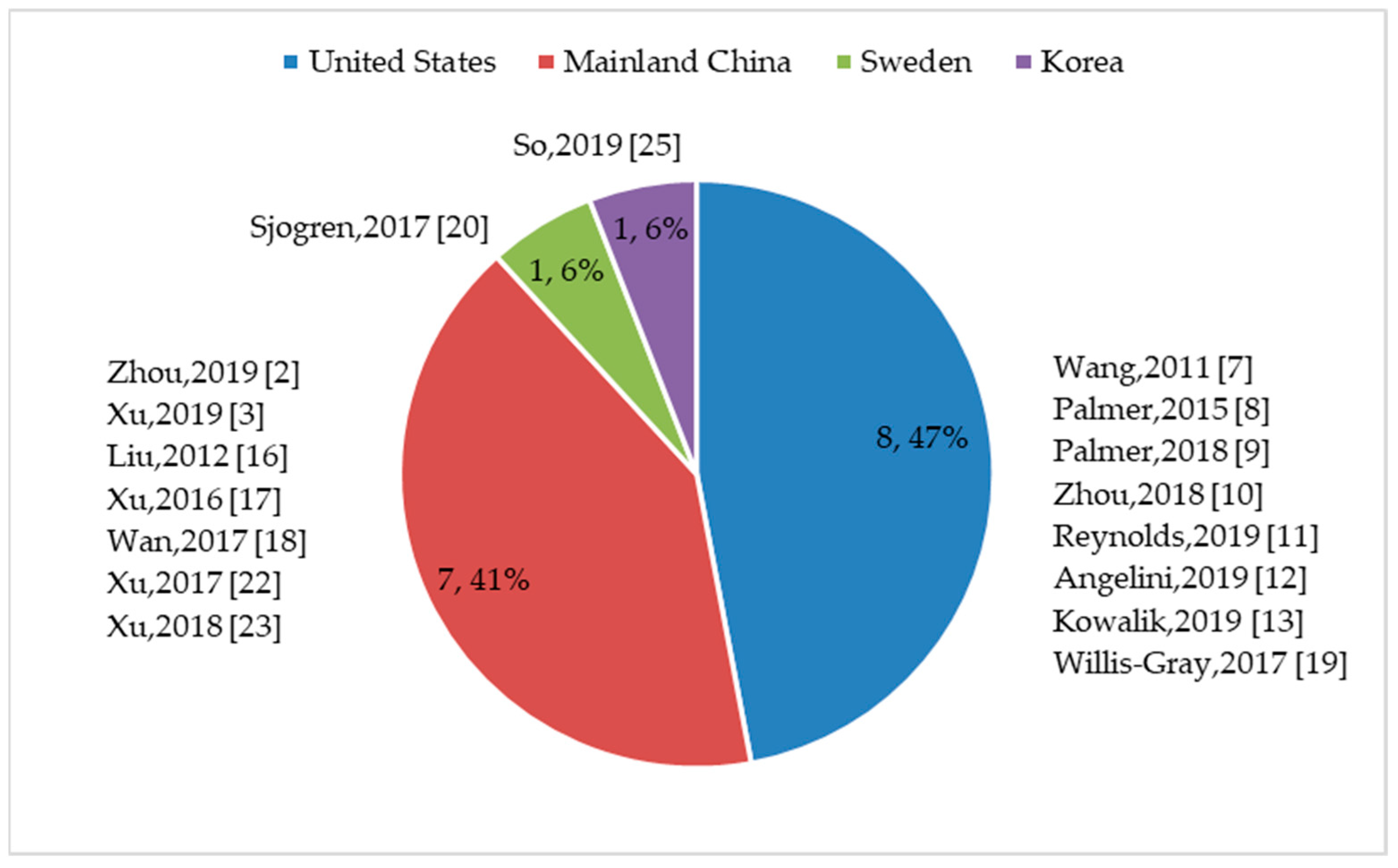
3.1. Sample Characteristics
3.2. Measures of Toileting Behaviors
3.2.1. Available Measures
3.2.2. TB–WEB Scale Development and Application
3.3. Toileting Behaviors and Their Determinants
3.3.1. Place Preference and Position Preference for Voiding
3.3.2. Premature and Delayed Voiding
3.3.3. Straining to Void
3.3.4. Determinants of Toileting Behaviors
3.4. Outcomes of Toileting Behaviors
4. Discussion
4.1. The TB–WEB Scale
4.2. Toileting Behaviors and Their Determinants
4.3. Outcomes of Toileting Behaviors
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Wang, K.; Palmer, M.H. Women’s toileting behaviour related to urinary elimination: Concept analysis. J. Adv. Nurs. 2010, 66, 1874–1884. [Google Scholar] [CrossRef] [PubMed]
- Zhou, F.; Xue, K.; Liu, Y.; Zhuo, L.; TU, S.; Palmer, M.H. Toileting behaviors and factors associated with urinary incontinence in college-aged female students in China. Int. Urogynecol. J. 2019, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Xu, D.; Zhu, S.; Li, H.; Gao, J.; Mou, H.; Wang, K. Relationships among occupational stress, toileting behaviors, and overactive bladder in nurses: A multiple mediator model. J. Adv. Nurs. 2019, 75, 1263–1271. [Google Scholar] [CrossRef] [PubMed]
- Peters, M.D.; Godfrey, C.M.; McInerney, P.; Soares, C.B.; Khalil, H.; Parker, D. The Joanna Briggs Institute Reviewers’ Manual 2015: Methodology for JBI Scoping Reviews. Available online: http://joannabriggs.org/assets/docs/sumari/Reviewers-Manual_Methodology-for-JBI-Scoping-Reviews_2015_v2.pdf (accessed on 18 October 2019).
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.; Horsley, T.; Weeks, L. PRISMA extension for scoping reviews (PRISMA-ScR): Checklist and explanation. Ann. Intern. 2018, 169, 467–473. [Google Scholar] [CrossRef]
- Arksey, H.; O’Malley, L. Scoping studies: Towards a methodological framework. Int. J. Soc. Res. Methodol. 2005, 8, 19–32. [Google Scholar] [CrossRef]
- Wang, K.; Palmer, M.H. Development and validation of an instrument to assess women’s toileting behavior related to urinary elimination: preliminary results. Nurs. Res. 2011, 60, 158–164. [Google Scholar] [CrossRef]
- Palmer, M.H.; Newman, D.K. Women’s toileting behaviours: An online survey of female advanced practice providers. Int. J. Clin. Pract. 2015, 69, 429–435. [Google Scholar] [CrossRef]
- Palmer, M.H.; Willis-Gray, M.G.; Zhou, F.; Newman, D.K.; Wu, J.M. Self-reported toileting behaviors in employed women: Are they associated with lower urinary tract symptoms? Neurourol. Urodynam. 2018, 37, 735–743. [Google Scholar] [CrossRef]
- Zhou, F.; Newman, D.K.; Palmer, M.H. Urinary urgency in working women: What factors are associated with urinary urgency progression? J. Womens Health 2018, 27, 575–583. [Google Scholar] [CrossRef]
- Reynolds, W.S.; Kowalik, C.; Delpe, S.D.; Kaufman, M.; Fowke, J.H.; Dmochowski, R. Toileting behaviors and bladder symptoms in women who limit restroom use at work: A cross-sectional study. J. Urol. 2019, 202, 1008–1014. [Google Scholar] [CrossRef]
- Angelini, K.J.; Newman, D.K.; Palmer, M.H. Psychometric evaluation of the toileting behaviors: Women’s Elimination Behaviors scale in a sample of college women. Female Pelvic. Med. Reconstr. Surg. 2019. [Google Scholar] [CrossRef] [PubMed]
- Kowalik, C.G.; Daily, A.; Delpe, S.; Kaufman, M.R.; Fowke, J.; Dmochowski, R.R.; Reynolds, W.S. Toileting behaviors of women—What is healthy? J. Urol. 2019, 201, 129–134. [Google Scholar] [CrossRef] [PubMed]
- Yang, K.N.; Chen, S.C.; Chen, S.Y.; Chang, C.H.; Wu, H.C.; Chou, E.C.L. Female voiding postures and their effects on micturition. Int. Urogynecol. J. 2010, 21, 1371–1376. [Google Scholar] [CrossRef] [PubMed]
- Chou, E.C.L.; Yang, P.Y.; Hsueh, W.H.; Chang, C.H.; Meng, N.H. Urinating in the standing position: A feasible alternative for elderly women with knee osteoarthritis. J. Urol. 2011, 186, 949–953. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Wang, K.; Palmer, M.H. Reliability and validity of the Chinese version of women’s toileting behavior scale in community-dwelling women with urinary incontinence. In International Continence Society (ICS) Annual Meeting; Neurourol. Urodynam: Beijing, China, 2012. [Google Scholar]
- Xu, D.; Chen, L.Q.; Wan, X.; Zhang, Y.; Liu, N.; Wang, K. Toileting behaviour and related health beliefs among Chinese female nurses. Int. J. Clin. Pract. 2016, 70, 416–423. [Google Scholar] [CrossRef] [PubMed]
- Wan, X.; Wu, C.; Xu, D.; Huang, L.; Wang, K. Toileting behaviours and lower urinary tract symptoms among female nurses: A cross-sectional questionnaire survey. Int. J. Nurs. Stud. 2017, 65, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Willis-Gray, M.G.; Wu, J.M.; Sripad, A.; Newman, D.; Palmer, M.H. Toileting behaviors in women presenting to a urogynecology clinic. Urol. Nurs. 2017, 37, 251–265. [Google Scholar] [CrossRef]
- Sjögren, J.; Malmberg, L.; Stenzelius, K. Toileting behavior and urinary tract symptoms among younger women. Int. Urogynecol. J. 2017, 28, 1677–1684. [Google Scholar] [CrossRef]
- Yang, P.Y.; Chen, C.C.; Chang, C.Y.Y.; Chou, E.C.L.; Meng, N.H. Cross-sectional study of the feasibility of urinating in a standing position among women in the third trimester of pregnancy. Int. J. Gynaecol. Obstet. 2017, 138, 226–227. [Google Scholar] [CrossRef]
- Xu, D.; Cheng, R.; Ma, A.; Zhao, M.; Wang, K. Toileting behaviors and overactive bladder in patients with Type 2 diabetes: A cross-sectional study in China. BMC Urol. 2017, 17, 42. [Google Scholar] [CrossRef]
- Xu, D.; Huang, L.; Gao, J.; Li, J.; Wang, X.; Wang, K. Effects of an education program on toileting behaviors and bladder symptoms in overactive bladder patients with Type 2 diabetes: A randomized clinical trial. Int. J. Nurs. Stud. 2018, 87, 131–139. [Google Scholar] [CrossRef] [PubMed]
- Shannon, M.B.; Tjaden, A.; Adams, W.; Brubaker, L.; Brincat, C. Toileting habits of nurses. Urol. Nurs. 2018, 38, 73–79. [Google Scholar] [CrossRef]
- So, A.; De Gagne, J.C.; Park, S. Validity and reliability of the Korean version of the Women’s Toileting Behavior scale. Int. Neurourol. J. 2019, 23, 151–160. [Google Scholar] [CrossRef] [PubMed]
- Pierce, H.; Perry, L.; Gallagher, R.; Chiarelli, P. Delaying voiding, limiting fluids, urinary symptoms and work productivity: A survey of female nurses and midwives. J. Adv. Nurs. 2019. [Google Scholar] [CrossRef] [PubMed]
- Pierce, H.; Perry, L.; Gallagher, R.; Chiarelli, P. Culture, teams, and organizations: A qualitative exploration of female nurses’ and midwives’ experiences of urinary symptoms at work. J. Adv. Nurs. 2019, 75, 1284–1295. [Google Scholar] [CrossRef]
- Palmer, M.H.; Wu, J.M.; Marquez, C.S.; Rupp, B.; Conover, M.M.; Newman, D.K. ‘A secret club’: Focus groups about women’s toileting behaviors. BMC Womens Health 2019, 19, 44. [Google Scholar] [CrossRef]
- Harvey, J.; Finney, S.; Stewart, L.; Gillespie, J. The relationship between cognition and sensation in determining when and where to void: The concept of cognitive voiding. BJU international 2012, 110, 1756–1761. [Google Scholar] [CrossRef]
- Cheng, S.; Li, Z.; Uddin, S.M.N.; Mang, H.P.; Zhou, X.; Zhang, J.; Zheng, L.; Zhang, L. Toilet revolution in China. J. Environ. Manag. 2018, 216, 347–356. [Google Scholar] [CrossRef]
- Su, Z.; Peng, S. The change of public toilets and city civilization—With modern Shanghai as an example. Hist. Rev. 2006, 3, 12–19. (In Chinese) [Google Scholar]
- O’Reilly, K. From toilet insecurity to toilet security: Creating safe sanitation for women and girls. WIREs Water 2016, 3, 19–24. [Google Scholar] [CrossRef]
- Norling, M.; Stenzelius, K.; Ekman, N.; Wennick, A. High school students’ experiences in school toilets or restrooms. J. Sch. Nurs. 2016, 3, 164–171. [Google Scholar] [CrossRef] [PubMed]
- Anthony, K.H.; Dufresne, M. Potty parity in perspective: Gender and family issues in planning and designing public restrooms. J. Plan. Lit. 2007, 21, 267–294. [Google Scholar] [CrossRef]
- Curtis, V.A. Dirt, disgust and disease: A natural history of hygiene. J. Epidemiol. Community Health 2007, 61, 660–664. [Google Scholar] [CrossRef] [PubMed]
- Lukacz, E.; Sampselle, C.; Gray, M.; Macdiarmid, S.; Rosenberg, M.; Ellsworth, P.; Palmer, M.H. A healthy bladder: A consensus statement. Int. J. Clin. Pract. 2011, 65, 1026–1036. [Google Scholar] [CrossRef]
| First Author (Year) Country | Sample (Female unless Otherwise Noted, Age Defined as Average Age ± Standard Deviation, unless Otherwise Noted) | Version of TB–WEB Scale | Domain (Number of Items): Scores of Domains within Score Range of 1–5 | Scaling Format of Item Frequency | Psychometric Characteristics | |
|---|---|---|---|---|---|---|
| Reliability | Validity | |||||
| Zhou (2019) [2] China | College/university students Age: 20.5 ± 1.6 years | 22-item Chinese version | Premature voiding (5) Straining to void (4) Place preference for voiding (4) Delayed voiding (3) Position preference for voiding (4) Emptying bladder completely (2) | ‘Often’ and ‘always’ were summarized as habitual behavior. | Cronbach’s alpha for each dimension was more than 0.7. Overall Cronbach’s alpha was 0.80. | N/A |
| Xu (2019) [3] China | Operating room nurses. Males were included in the sample. Overall age: 30.2 ± 7.1 years; female age unknown | 15-item Chinese (male/female) version | Both male and female participants: Premature voiding (4): 2.3 ± 0.9 Straining to void (4): 2.2 ± 0.9 Place preference for voiding (4): 3.0 ± 1.0 Delayed voiding (3): 3.3 ± 0.9 | Never/rarely Sometimes Often/always | Not reported | N/A |
| Wang (2011) [7] USA | Employees of a large university and academic medical center Age: 51.2 ± 6.8 years | 18-item English version | Premature voiding (5): 1.75 ± 0.11 Straining to void (4): 1.91 ± 0.06 Place preference for voiding (4): 2.81 ± 0.61 Delayed voiding (3): 2.79 ± 0.25 Position preference for voiding (2): 2.01 ± 0.16 | N/A | Cronbach’s alpha: Premature voiding (α = 0.88) Straining to void (α = 0.86) Place preference for voiding (α = 0.71) Delayed voiding (α = 0.70) Position preference for voiding (α = 0.73) | Construct validity: Five subscales explained 67% variance of latent toileting behaviors. Criterion-related validity: Incontinent vs. continent group: straining (t = 2.12, p < 0.05), place preference (t = 2.24, p < 0.05), delayed (t = 2.70, p < 0.01), position preference (t = 2.07, p < 0.05). Total scale (t = 3.79, p < 0.01) is significant and premature voiding is nonsignificant (t = 1.39, p > 0.05). |
| Palmer (2015) [8] USA | Advanced practice providers Age: 45.1 ± 10.6 years | 19-item English version | Premature voiding (5) Straining to void (4) Place preference for voiding (4) Delayed voiding (3) Position preference for voiding (3) | Never Rarely/sometimes Often/always | Not reported | N/A |
| Palmer (2018) [9] USA | Employees of a large academic medical center Age: 47.3 ± 13.6 years | 22-item English version | Premature voiding (5) Straining to void (4) Delayed voiding (3) Place preference for voiding (4) Position preference (4) Two additional items tested the intentional or unintentional complete emptying of bladder. | ‘Often/always’ was regarded as having the behavior, otherwise, not having the behavior. | Not reported | N/A |
| Zhou (2018) [10] USA | Employees of a large academic medical center Age: 46.9 ± 12.9 years | 22-item English version | Premature voiding (5) Straining to void (4) Delayed voiding (3) Place preference for voiding (4) Position preference (4) Two additional items tested the intentional or unintentional complete emptying of bladder. | ‘Often/always’ was regarded as having the behavior, otherwise, not having the behavior. | Not reported | N/A |
| Reynolds (2019) [11] USA | Full-time working women Age: 38.7 ± 12.2 years | 19-item English version | Premature voiding (5) Straining to void (4) Place preference for voiding (4) Delayed voiding (3) Position preference for voiding (3) | ‘Often’ and ‘always’ were summarized as habitual behavior. | Not reported | N/A |
| Angelini (2019) [12] USA | Private college undergraduates Age: 21.2 ± 0.46 years | 18-item English version | Premature voiding (5) Straining to void (4) Place preference for voiding (4) Delayed voiding (3) Position preference for voiding (2) | ‘Rarely’, ‘sometimes’, ‘often’, and ‘always’ were summarized as having the behavior. | Cronbach’s alpha: 0.846 for entire scale Premature voiding (α = 0.868) Straining to void (α = 0.919) Place preference for voiding (α = 0.731) Delayed voiding (α = 0.834) Position preference for voiding (α = 0.582) | Construct validity: Four subscales explained 72.8% variance of latent toileting behavior. Convergent and discriminant validity: Confirmed by establishing significant associations between toileting behaviors and stress urinary incontinence (r = 0.293, p = 0.015), urgency urinary incontinence (r = 0.342, p < 0.001), stress urinary incontinence related to sport or physical activity (r = 0.350, p < 0.001), and urinary urgency (r = 0.334, p < 0.001). |
| Kowalik (2019) [13] USA | Living in a community Age: 41.4 ± 15 years | 24-item English version | Convenience voiding (5) Straining to void (4) Place preference for voiding (4) Delayed voiding (3) Position preference for voiding (8) | ‘Sometimes’, ‘often’, and ‘always’ were regarded as having the behavior, otherwise, not having the behavior. | Not reported | N/A |
| Liu (2012) [16] China | Living in a community and reported having urinary incontinence Age: unknown | 14-item Chinese version | Premature voiding (4) Straining to void (4) Place preference for voiding (3) Delayed voiding (3) | N/A | Cronbach’s alpha: Premature voiding (α = 0.92) Straining to void (α = 0.95) Place preference for voiding (α = 0.75) Delayed voiding (α = 0.8) | Construct validity: Four subscales explained 79% variance of latent toileting behaviors. |
| Xu (2016) [17] China | Clinical nurses from three hospitals Age: 30.6 ± 7.9 years | 17-item Chinese version | Premature voiding (4): 2.30 ± 0.92 Straining to void (4): 1.89 ± 0.87 Place preference for voiding (4): 2.90 ± 0.84 Delayed voiding (3): 3.12 ± 0.77 Position preference for voiding (2): 2.45 ± 1.06 | Never/rarely Sometimes Often/always | Not reported | N/A |
| Wan (2017) [18] China | Clinical nurses Age: 30.6 ± 7.9 years | 17-item Chinese version | Premature voiding (4): 2.30 ± 0.92 Straining to void (4): 1.89 ± 0.87 Place preference for voiding (4): 2.90 ± 0.84 Delayed voiding (3): 3.12 ± 0.77 Position preference for voiding (2): 2.45 ± 1.06 | Never Rarely Sometimes Often Always | Not reported | N/A |
| Willis-Gray (2017) [19] USA | Patients in a urogynecology clinic Age: mean = 60.4 years | 22-item English version, with 4 pictorial images | Premature voiding (5) Straining to void (5) Attitudes towards public bathrooms (4) Delayed voiding (4) Position preference for voiding (4) Four pictorial descriptions: sitting, crouching, squatting, or standing | Never, rarely, or never/rarely Unreported Sometimes/often/always | Not reported | N/A |
| Sjogren (2017) [20] Sweden | University students Age: mean = 21.6 years, ranging from 18 to 25 | 19-item Swedish version | Premature voiding (5): 2.0 ± 0.8 Straining to void (4): 1.9 ± 0.8 Place preference for voiding (4): 3.63 ± 0.85 Delayed voiding (3): 2.63 ± 0.83 Position preference for voiding (3): 1.1 ± 0.47 | Never Rarely Sometimes Often Always The latter three options were summarized as ‘at least sometimes’. | Cronbach’s alpha: Premature voiding (α = 0.84) Straining to void (α = 0.82) Place preference for voiding (α = 0.81) Delayed voiding (α = 0.71) Position preference for voiding (α = 0.54) | Construct validity: Five subscales explained 66% variance of latent toileting behaviors. |
| Xu (2017) [22] China | Participants from an endocrinology department in one hospital who had Type 2 diabetes mellitus. Men were included in the sample. Overall age: 59.1 ± 11.7 years; female age unknown | 15-item Chinese (male/female) version | Both male and female participants: Premature voiding (4): 2.41 ± 1.00 Straining to void (4): 1.49 ± 0.88 Place preference for voiding (4): 2.18 ± 1.14 Delayed voiding (3): 2.06 ± 0.74 | Never/rarely Sometimes Often/always | Cronbach’s alpha: 0.71 for entire scale | N/A |
| Xu (2018) [23] China | Participants from an endocrinology department in one hospital who had overactive bladder and Type 2 diabetes mellitus. Men were included in the sample. Overall age: 66.4 ± 8.2 years; female age unknown | 15-item Chinese (male/female) version | Both male and female participants: Premature voiding (4): 2.41 ± 1.00 Straining to void (4): 1.49 ± 0.88 Place preference for voiding (4): 2.18 ± 1.14 Delayed voiding (3): 2.06 ± 0.74 | Never/rarely Sometimes Often/always | Not reported | N/A |
| So (2019) [25] Korea | Participants aged 50 years and over who had urinary incontinence Age: 74.35 ± 9.36 years | 17-item Korean version | Premature voiding (5) Straining to void (4) Place preference for voiding (3) Delayed voiding (3) Position preference for voiding (2) | N/A | Cronbach’s alpha: 0.78 for entire scale Premature voiding (α = 0.79) Straining to void (α = 0.94) Place preference for voiding (α = 0.81) Delayed voiding (α = 0.83) Position preference for voiding (α = 0.83) | Construct validity: Five subscales explained 74.24% variance of the latent toileting behavior. Concurrent validity: Supported by establishing significant association with responses to the International Consultation on Incontinence Questionnaire Short Form (r = 0.146, p = 0.011). |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wu, C.; Xue, K.; Palmer, M.H. Toileting Behaviors Related to Urination in Women: A Scoping Review. Int. J. Environ. Res. Public Health 2019, 16, 4000. https://doi.org/10.3390/ijerph16204000
Wu C, Xue K, Palmer MH. Toileting Behaviors Related to Urination in Women: A Scoping Review. International Journal of Environmental Research and Public Health. 2019; 16(20):4000. https://doi.org/10.3390/ijerph16204000
Chicago/Turabian StyleWu, Chen, Kaikai Xue, and Mary H. Palmer. 2019. "Toileting Behaviors Related to Urination in Women: A Scoping Review" International Journal of Environmental Research and Public Health 16, no. 20: 4000. https://doi.org/10.3390/ijerph16204000
APA StyleWu, C., Xue, K., & Palmer, M. H. (2019). Toileting Behaviors Related to Urination in Women: A Scoping Review. International Journal of Environmental Research and Public Health, 16(20), 4000. https://doi.org/10.3390/ijerph16204000






