Burden and Anxiety in Family Caregivers in the Hospital That Debut in Caregiving
Abstract
:1. Introduction
1.1. The Caregivers in the Hospital
1.2. Association between Burden and Anxiety
1.3. The Mediating Role of Subjective Burden
2. Materials and Methods
2.1. Design
2.2. Participants
2.3. Measurements
2.3.1. Sociodemographic Variables
2.3.2. Dependent Variable
2.3.3. Mediator Variable
2.3.4. Independent Variables
2.3.5. Control Variable
2.4. Data Collection
2.5. Data Analysis
3. Results
3.1. Sample Population Description
3.2. Levels of Burden and Anxiety
3.3. Bivariate Analysis
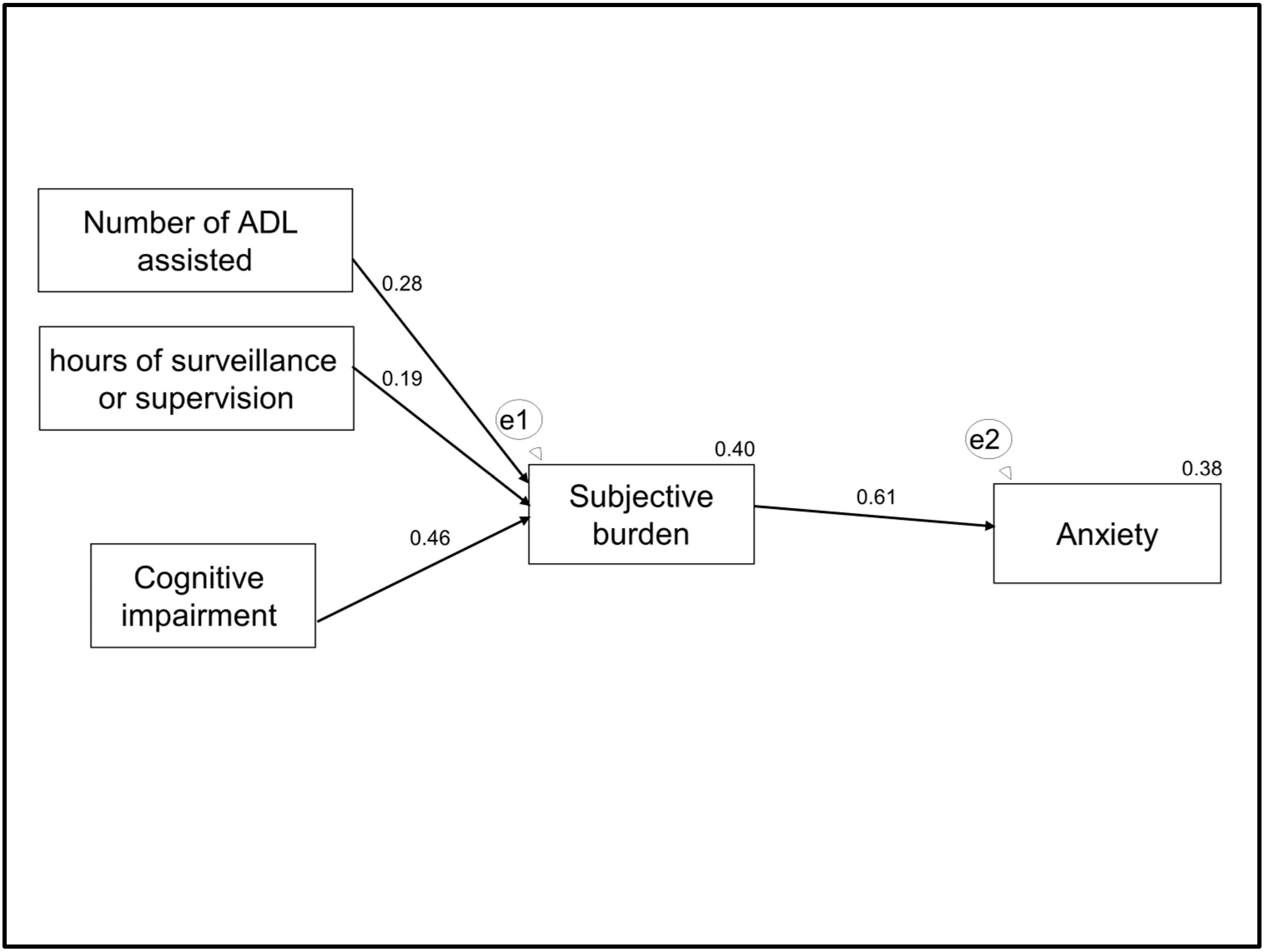
3.4. Multivariate Analysis
4. Discussion
4.1. Levels of Burden and Anxiety
4.2. Objective Burden, Burden, and Anxiety
5. Conclusions
- The levels of subjective burden and anxiety may be higher than in those that have not recently started caregiving, highlighting the importance of these problems and the need that debut caregivers in the hospital should be preferentially attended to in order to prevent these consequences.
- Subjective burden is a possible risk factor for anxiety, independent of the objective burden.
- Subjective burden may buffer the effects of objective burden on anxiety.
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- OECD. Health at a Glance 2017: OECD Indicators; OECD Publishing: Paris, France, 2017. [Google Scholar]
- Bom, J.; Bakx, P.; Schut, F.; van Doorslaer, E. The Impact of Informal Caregiving for Older Adults on the Health of Various Types of Caregivers: A Systematic Review. Gerontologist 2018. [Google Scholar] [CrossRef] [PubMed]
- Sociedad Española de Geriatría y Gerontología (SEGG). Análisis y Evaluación de la Red de Servicios Sanitarios Dedicados a la Dependencia: Programas de Prevención, Atención Domiciliaria y Hospitalización; SEGG: Madrid, Spain, 2005. (In Spainish) [Google Scholar]
- Mora López, G.; Ferré-Grau, C. La invisibilidad del cuidador familiar en el hospital comarcal. Ética de los Cuidados 2013, 6, 11. (In Spainish) [Google Scholar]
- Perez Marmol, J.M.; Flores Antiguedad, M.L.; Castro Sanchez, A.M.; Tapia Haro, R.M.; Garcia Rios, M.D.C.; Aguilar Ferrandiz, M.E. Inpatient dependency in activities of daily living predicts informal caregiver strain: A cross-sectional study. J. Clin. Nurs. 2018, 27, e177–e185. [Google Scholar] [CrossRef] [PubMed]
- Hanzeliková Pogrányivá, A.; López Muñóz, F.; Fusté Moreno, R. Perfil socio-demográfico de los cuidadores de los pacientes geriátricos hospitalizados mayores de 75 años y su relación con la satisfacción. Enferm. Glob. 2017, 16, 375–388. (In Spainish) [Google Scholar]
- Villavicencio, M.E.F.; Laguna, H.L.F.; Pérez, G.J.G.; Flores, I.J.M.; Cardona, G.A.C.; Barbosa, M.A.V. Características principales del cuidador primario informal de adultos mayores hospitalizados. NURE Inv. 2017, 14, 1–16. (In Spainish) [Google Scholar]
- Hsu, T.; Nathwani, N.; Loscalzo, M.; Chung, V.; Chao, J.; Karanes, C.; Koczywas, M.; Forman, S.; Lim, D.; Siddiqi, T.; et al. Understanding Caregiver Quality of Life in Caregivers of Hospitalized Older Adults with Cancer. J. Am. Geriatr. Soc. 2019, 67, 978–986. [Google Scholar] [CrossRef]
- Hung, J.W.; Huang, Y.C.; Chen, J.H.; Liao, L.N.; Lin, C.J.; Chuo, C.Y.; Chang, K.C. Factors associated with strain in informal caregivers of stroke patients. Chang. Gung. Med. J. 2012, 35, 392–401. [Google Scholar]
- La Invisibilidad de Las Personas Cuidadoras: Un Enfoque Discursivo del Personal de Enfermería del Hospital de Antequera. Available online: http://www.index-f.com/eticuidado/n10/et7919.php (accessed on 18 March 2019).
- Plank, A.; Mazzoni, V.; Cavada, L. Becoming a caregiver: New family carers’ experience during the transition from hospital to home. J. Clin. Nurs. 2012, 21, 2072–2082. [Google Scholar] [CrossRef]
- Bradshaw, L.E.; Goldberg, S.E.; Schneider, J.M.; Harwood, R.H. Carers for older people with co-morbid cognitive impairment in general hospital: Characteristics and psychological well-being. Int. J. Geriatr. Psychiatry 2013, 28, 681–690. [Google Scholar] [CrossRef]
- Marrujo-Pérez, K.J.; Berumen-Burciaga, L.V.; Mejía-Mejía, Y.; Palacios-Ceña, D. El significado de la hospitalización desde la mirada del cuidador: Estudio cualitativo. Enferm. Clin. 2016, 26, 102–110. (In Spainish) [Google Scholar] [CrossRef]
- Jeong, Y.G.; Myong, J.P.; Koo, J.W. The modifying role of caregiver burden on predictors of quality of life of caregivers of hospitalized chronic stroke patients. Disabil. Health J. 2015, 8, 619–625. [Google Scholar] [CrossRef] [PubMed]
- Shankar, K.N.; Hirschman, K.B.; Hanlon, A.L.; Naylor, M.D. Burden in caregivers of cognitively impaired elderly adults at time of hospitalization: A cross-sectional analysis. J. Am. Geriat. Soc. 2014, 62, 276–284. [Google Scholar] [CrossRef] [PubMed]
- Moral-Fernández, L.; Frías-Osuna, A.; Moreno-Cámara, S.; Palomino-Moral, P.A.; Del-Pino-Casado, R. The start of caring for an elderly dependent family member: A qualitative metasynthesis. BMC Geriatr. 2018, 18, 228. [Google Scholar] [CrossRef] [PubMed]
- Faronbi, J.O.; Faronbi, G.O.; Ayamolowo, S.J.; Olaogun, A.A. Caring for the seniors with chronic illness: The lived experience of caregivers of older adults. Arch. Gerontol. Geriatr. 2019, 82, 8–14. [Google Scholar] [CrossRef]
- Moreno-Cámara, S.; Palomino-Moral, P.; Moral-Fernández, L.; Frías-Osuna, A.; Parra-Anguita, L.; del-Pino-Casado, R. Perceived Needs of The Family Caregivers of People with Dementia in a Mediterranean Setting: A Qualitative Study. Int. J. Environ. Res. Public Health 2019, 16, 993. [Google Scholar] [CrossRef]
- Loh, A.Z.; Tan, J.S.; Zhang, M.W.; Ho, R.C. The Global Prevalence of Anxiety and Depressive Symptoms Among Caregivers of Stroke Survivors. J. Am. Med. Dir. Assoc. 2017, 18, 111–116. [Google Scholar] [CrossRef]
- Sallim, A.B.; Sayampanathan, A.A.; Cuttilan, A.; Chun-Man Ho, R. Prevalence of Mental Health Disorders Among Caregivers of Patients with Alzheimer Disease. J. Am. Med. Dir. Assoc. 2015, 16, 1034–1041. [Google Scholar] [CrossRef]
- Watson, B.; Tatangelo, G.; McCabe, M. Depression and Anxiety among Partner and Offspring Carers of People With Dementia: A Systematic Review. Gerontologist 2018, 59, e597–e610. [Google Scholar] [CrossRef]
- Abajo, M.; Rodríguez-Sanz, M.; Malmusi, D.; Salvador, M.; Borrell, C. Gender and socio-economic inequalities in health and living conditions among co-resident informal caregivers: A nationwide survey in Spain. J. Adv. Nurs. 2017, 73, 700–715. [Google Scholar] [CrossRef]
- Lazarus, R.S.; Folkman, S. Stress, Appraisal and Coping; Springer: New York, NY, USA, 1984. [Google Scholar]
- Kim, H.; Chang, M.; Rose, K.; Kim, S. Predictors of caregiver burden in caregivers of individuals with dementia. J. Adv. Nurs. 2012, 68, 846–855. [Google Scholar] [CrossRef]
- Pearlin, L.I.; Mullan, J.T.; Semple, S.J.; Skaff, M.M. Caregiving and the stress process: An overview of concepts and their measures. Gerontologist 1990, 30, 583–594. [Google Scholar] [CrossRef] [PubMed]
- Del-Pino-Casado, R.; Millán-Cobo, M.D.; Palomino-Moral, P.A.; Frías-Osuna, A. Cultural Correlates of Burden in Primary Caregivers of Older Relatives: A Cross-sectional Study. J. Nurs. Scholarsh. 2014, 46, 176–186. [Google Scholar] [CrossRef] [PubMed]
- Del-Pino-Casado, R.; Pérez-Cruz, M.; Frías-Osuna, A. Coping, subjective burden and anxiety among family caregivers of older dependents. J. Clin. Nurs. 2014, 23, 3335–3344. [Google Scholar] [CrossRef] [PubMed]
- Zarit, S.H.; Reever, K.E.; Bach-Peterson, J. Relatives of the impaired elderly: Correlates of feelings of burden. Gerontologist 1980, 20, 649–654. [Google Scholar] [CrossRef] [PubMed]
- Del-Pino-Casado, R.; Frías-Osuna, A.; Palomino-Moral, P.A.; Pancorbo-Hidalgo, P.L. Coping and subjective burden in caregivers of older relatives: A quantitative systematic review. J. Adv. Nurs. 2011, 67, 2311–2322. [Google Scholar] [CrossRef] [PubMed]
- Pérez-Ordoñez, F.; Frías-Osuna, A.; Romero-Rodríguez, Y.; Del-Pino-Casado, R. Coping strategies and anxiety in caregivers of palliative cancer patients. Eur. J. Cancer Care (Engl.) 2016, 25, 600–607. [Google Scholar] [CrossRef]
- Cooper, C.; Balamurali, T.B.; Livingston, G. A systematic review of the prevalence and covariates of anxiety in caregivers of people with dementia. Int. Psychogeriatr. 2007, 19, 175–195. [Google Scholar] [CrossRef]
- Li, R.; Cooper, C.; Bradley, J.; Shulman, A.; Livingston, G. Coping strategies and psychological morbidity in family carers of people with dementia: A systematic review and meta-analysis. J. Affect. Disord. 2012, 3, 1–11. [Google Scholar] [CrossRef]
- Pérez-Cruz, M.; Muñoz-Martínez, M.A.; Parra-Anguita, L.; Del-Pino-Casado, R. Afrontamiento y carga subjetiva en cuidadores primarios de adultos mayores dependientes de Andalucía, España. Aten. Prim. 2017, 49, 281–288. (In Spainish) [Google Scholar] [CrossRef]
- Pinquart, M.; Sorensen, S. Associations of stressors and uplifts of caregiving with caregiver burden and depressive mood: A meta-analysis. J. Gerontol. B Psychol. Sci. Soc. Sci. 2003, 58, 112–128. [Google Scholar] [CrossRef]
- Knight, B.G.; Sayegh, P. Cultural values and caregiving: The updated Sociocultural Stress and Coping Model. J. Gerontol. B Psychol. Sci. Soc. Sci. 2010, 65, 5–13. [Google Scholar] [CrossRef] [PubMed]
- Zegwaard, M.I.; Aartsen, M.J.; Cuijpers, P.; Grypdonck, M.H. Review: A conceptual model of perceived burden of informal caregivers for older persons with a severe functional psychiatric syndrome and concomitant problematic behaviour. J. Clin. Nurs. 2011, 20, 2233–2258. [Google Scholar] [CrossRef] [PubMed]
- van der Lee, J.; Bakker, T.J.; Duivenvoorden, H.J.; Droes, R.M. Multivariate models of subjective caregiver burden in dementia; a systematic review. Ageing Res. Rev. 2014, 15, 76–93. [Google Scholar] [CrossRef] [PubMed]
- Nunnally, J.; Bernstein, N. Psychometric Theory, 3rd ed.; McGraw-Hill: New York, NY, USA, 1994. [Google Scholar]
- Hamilton, M. The assessment of anxiety states by rating. Br. J. Med. Psychol. 1959, 32, 50–55. [Google Scholar] [CrossRef] [PubMed]
- Bech, P. Rating Scales for Psychopathology, Health Status and Quality of Life: A Compendium on Documentation in Accordance with the DSM-III-R and WHO Systems; Springer: New York, NY, USA, 1993. [Google Scholar]
- Kobak, K.A.; Reynolds, W.M.; Greist, J.H. Development and validation of a computer-administered version of the Hamilton Rating Scale. Psychol. Assess. 1993, 5, 487–492. [Google Scholar] [CrossRef]
- Lobo, A.; Chamorro, L.; Luque, A.; Dal-Ré, R.; Badia, X.; Baró, E. Validación de las versiones en español de la Montgomery-Asberg Depression Rating Scale y la Hamilton Anxiety Rating Scale para la evaluación de la depresión y de la ansiedad. Med. Clin. (Barc.) 2002, 118, 493–499. (In Spainish) [Google Scholar] [CrossRef]
- Robinson, B.C. Validation of a Caregiver Strain Index. J. Gerontol. 1983, 38, 344–348. [Google Scholar] [CrossRef]
- López Alonso, S.; Moral Serrano, M. Validación del Índice de Esfuerzo del Cuidador en la población española. Enferm. Comun. 2005, 1, 12–17. (In Spainish) [Google Scholar]
- Mahoney, F.I.; Barthel, D.W. Functional evaluation: The Barthel Index. Md. State Med. J. 1965, 14, 61–65. [Google Scholar]
- Baztán, J.; Pérez, J.; Alarcón, T.; San Cristóbal, E.; Izquierdo, G.; Manzarbeitia, I. Índice de Barthel: Instrumento válido para la valoración funcional de pacientes con enfermedad cerebrovascular. Rev. Esp. Geriatr. Gerontol. 1993, 28, 32–40. (In Spainish) [Google Scholar]
- Pfeiffer, E. A short portable mental status questionnaire for the assessment of organic brain deficit in elderly patients. J. Am. Geriatr. Soc. 1975, 23, 433–441. [Google Scholar] [CrossRef] [PubMed]
- Martínez de la Iglesia, J.; Dueñas Herrero, R.; Vilches, O.; Aguado Taberné, C.; Albert Colomer, C.; Luque Luque, R. Adaptación y validación al castellano del cuestionario de Pfeiffer (SPMSQ) para detectar la existencia de deterioro cognitivo en personas mayores de 65 años. Med. Clín. 2001, 117, 129–134. (In Spainish) [Google Scholar] [CrossRef]
- Holmes, T.H.; Rahe, R.H. The Social Readjustment Rating Scale. J. Psychosom. Res. 1967, 11, 213–218. [Google Scholar] [CrossRef]
- MacKinnon, D. Introduction to Statistical Mediation Analysis; Routledge: Abingdon, UK, 2008. [Google Scholar]
- Hooper, D.; Coughlan, J.; Mullen, M.R. Structural equation modelling: Guidelines for determining model fit. J. Bus. Res. 2008, 6, 53–60. [Google Scholar]
- MacKinnon, D.P.; Fairchild, A.J.; Fritz, M.S. Mediation analysis. Ann. Rev. Psychol. 2007, 58, 593–614. [Google Scholar] [CrossRef]
- Instituto de Mayores y Servicios Sociales (IMSERSO). Cuidados a las Personas Mayores en los Hogares Españoles. El Entorno Familiar, 1st ed.; Ministerio de Trabajo y Asuntos Sociales Secretaría de Estado de Servicios Sociales, Familias y Discapacidad. Instituto de Mayores y Servicios Sociales (IMSERSO): Madrid, Spain, 2005. (In Spainish)
- Marvardi, M.; Mattioli, P.; Spazzafumo, L.; Mastriforti, R.; Rinaldi, P.; Polidori, M.C.; Cherubini, A.; Quartesan, R.; Bartorelli, L.; Bonaiuto, S.; et al. The Caregiver Burden Inventory in evaluating the burden of caregivers of elderly demented patients: Results from a multicenter study. Aging Clin. Exp. Res. 2005, 17, 46–53. [Google Scholar] [CrossRef]
- McCullagh, E.; Brigstocke, G.; Donaldson, N.; Kalra, L. Determinants of caregiving burden and quality of life in caregivers of stroke patients. Stroke 2005, 36, 2181–2186. [Google Scholar] [CrossRef]


| Mean (SD) | Theoretical Range | Practical Range | n (%) | 95% CI | |
|---|---|---|---|---|---|
| Care recipient | |||||
| Age | 75.5 (8.2) | 60–92 | 73.27–77.73 | ||
| Gender | |||||
| Male | 46 (63.9%) | 52.10–75.67 | |||
| Female | 26 (36.1%) | 24.32–47.90 | |||
| Main pathology | |||||
| Stroke | 35 (48.6%) | 36.37–60.85 | |||
| Cancer | 15 (20.8%) | 10.75–30.90 | |||
| Dementia | 1 (1.4%) | 0.03–7.49 | |||
| Other | 21 (29.2%) | 17.97–40.36 | |||
| Functional capacity | 22 (20.9) | 0–100 | 0–90 | 16.27–27.66 | |
| Cognitive impairment | 3.8 (3.1) | 0–10 | 0–10 | 4.00–4.71 | |
| Caregiver | |||||
| Age | 56 (14.7) | 23–4 | 52.57–59.49 | ||
| Gender | |||||
| Female | 57 (79.2%) | 69.09–89.24 | |||
| Male | 15 (20.8%) | 10.75–30.90 | |||
| Relationship | |||||
| Spouse | 34 (47.2%) | 34.99–59.44 | |||
| Offspring | 32 (44.4%) | 32.27–56.61 | |||
| Other | 6 (8.3%) | 1.25–15.44 | |||
| Education level | |||||
| No primary school | 43 (59.7%) | 47.69–71.74 | |||
| Secondary school | 21 (29.2%) | 17.93–40.36 | |||
| University | 8 (11.1%) | 3.15–19.06 | |||
| Employment status | |||||
| Active | 20 (27.8%) | 16.73–38.81 | |||
| Unemployed | 12 (16.7%) | 7.36–25.696 | |||
| Retired | 10 (13.9%) | 5.20–22.57 | |||
| Housewife | 29 (40.3%) | 28.25–52.30 | |||
| Other | 1 (1.4%) | 0.03–7.49 | |||
| Common residence | 47 (65.3%) | 53.58–76.96 | |||
| Number of ADLs assisted | 4.8 (3.1) | 1–10 | 4.06–5.52 | ||
| Hours of surveillance or supervision | 5.5 (4.9) | 1–10 | 4.37–6.69 | ||
| Stressful life events | 96.2 (47.3) | 44–239 | 85.11–107.36 | ||
| Anxiety | 15.4 (10) | 0–56 | 0–46 | 13.03–17.72 | |
| Subjective burden | 5.4 (3.1) | 0–13 | 0–12 | 4.67–6.11 | |
| 2 | 3 | 4 | 5 | 6 | 7 | |
|---|---|---|---|---|---|---|
| 1. Anxiety | 0.614 ** | 0.212 | 0.225 | 0.012 | −0.135 | 0.232 |
| 2. Subjective burden | 0.397 ** | 0.305 ** | 0.010 | −0.220 | 0.510 ** | |
| 3. Number of ADL assisted | 0.433 ** | 0.114 | −0.088 | 0.121 | ||
| 4. Hours of surveillance or supervision | 0.079 | 0.222 | 0.080 | |||
| 5. Stressful life event | 0.032 | −0.196 | ||||
| 6. Functional capacity | −0.452 ** | |||||
| 7. Cognitive impairment |
| Direct Effects | Indirect Effects | Total Effect | |
|---|---|---|---|
| Subjective burden | 0.61 | 0 | 0.61 |
| Number of ADL assisted | 0 | 0.17 | 0.17 |
| Hours of surveillance or supervision | 0 | 0.11 | 0.11 |
| Cognitive impairment | 0 | 0.24 | 0.24 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pérez-Cruz, M.; Parra-Anguita, L.; López-Martínez, C.; Moreno-Cámara, S.; del-Pino-Casado, R. Burden and Anxiety in Family Caregivers in the Hospital That Debut in Caregiving. Int. J. Environ. Res. Public Health 2019, 16, 3977. https://doi.org/10.3390/ijerph16203977
Pérez-Cruz M, Parra-Anguita L, López-Martínez C, Moreno-Cámara S, del-Pino-Casado R. Burden and Anxiety in Family Caregivers in the Hospital That Debut in Caregiving. International Journal of Environmental Research and Public Health. 2019; 16(20):3977. https://doi.org/10.3390/ijerph16203977
Chicago/Turabian StylePérez-Cruz, Margarita, Laura Parra-Anguita, Catalina López-Martínez, Sara Moreno-Cámara, and Rafael del-Pino-Casado. 2019. "Burden and Anxiety in Family Caregivers in the Hospital That Debut in Caregiving" International Journal of Environmental Research and Public Health 16, no. 20: 3977. https://doi.org/10.3390/ijerph16203977
APA StylePérez-Cruz, M., Parra-Anguita, L., López-Martínez, C., Moreno-Cámara, S., & del-Pino-Casado, R. (2019). Burden and Anxiety in Family Caregivers in the Hospital That Debut in Caregiving. International Journal of Environmental Research and Public Health, 16(20), 3977. https://doi.org/10.3390/ijerph16203977





