Cataract Services are Leaving Widows Behind: Examples from National Cross-Sectional Surveys in Nigeria and Sri Lanka
Abstract
1. Introduction
2. Materials and Methods
2.1. Data Source
2.2. Variables
- Cataract blindness, defined as best-corrected visual acuity of <3/60 in the better eye where the principal cause was cataract;
- Cataract surgical coverage (CSC), which measures the number of people in a defined population with operated cataract as a proportion of those having operable plus operated cataract. We defined “operable cataract” as a cataract causing best-corrected visual acuity worse than 3/60; and
- Effective cataract surgical coverage (eCSC), which measures the number of people in a defined population with operated cataract and a good outcome (i.e., presenting visual acuity 6/18 or better) as a proportion of those having operable plus operated cataract [12].
2.3. Analysis
3. Results
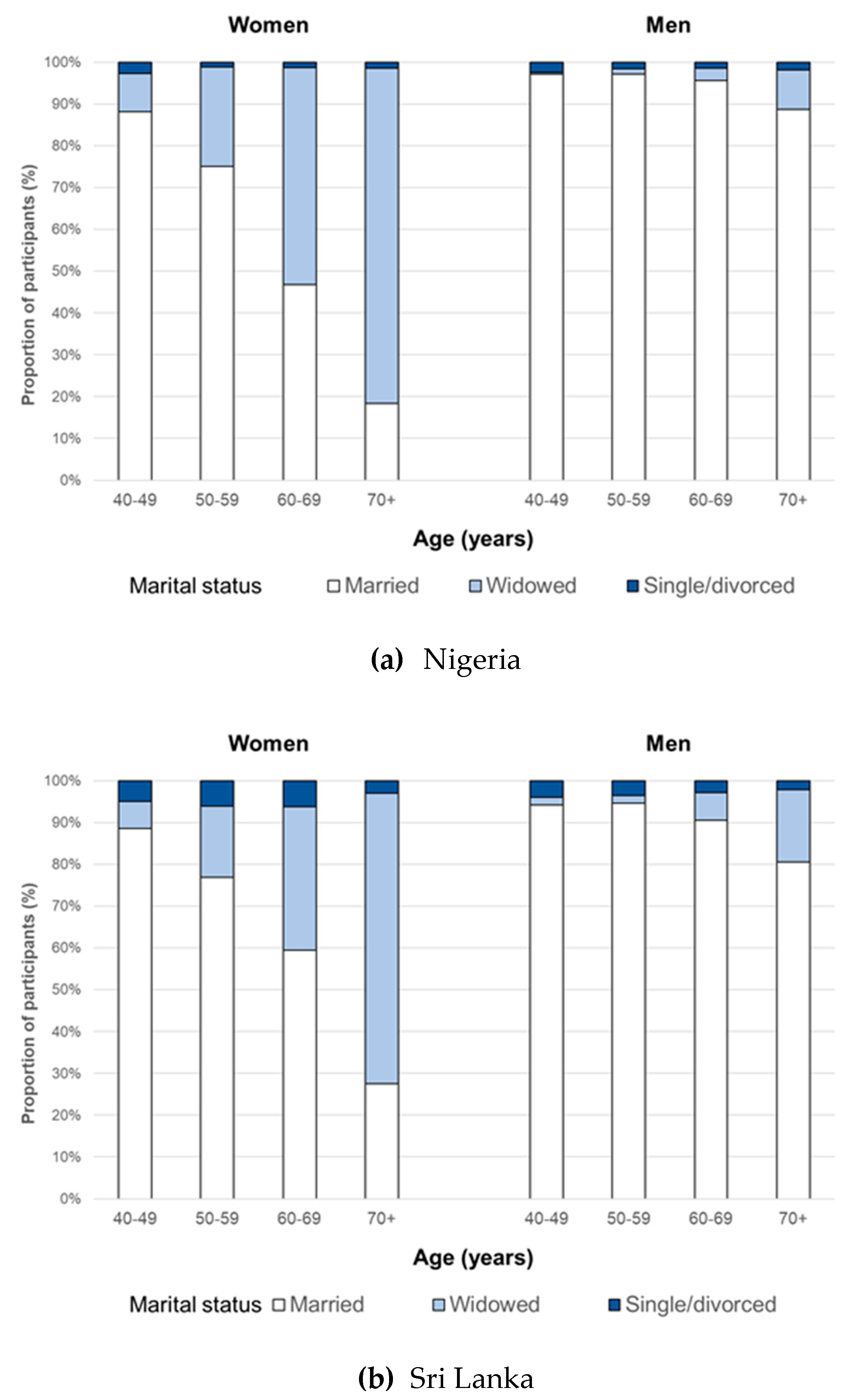
3.1. Marital Status
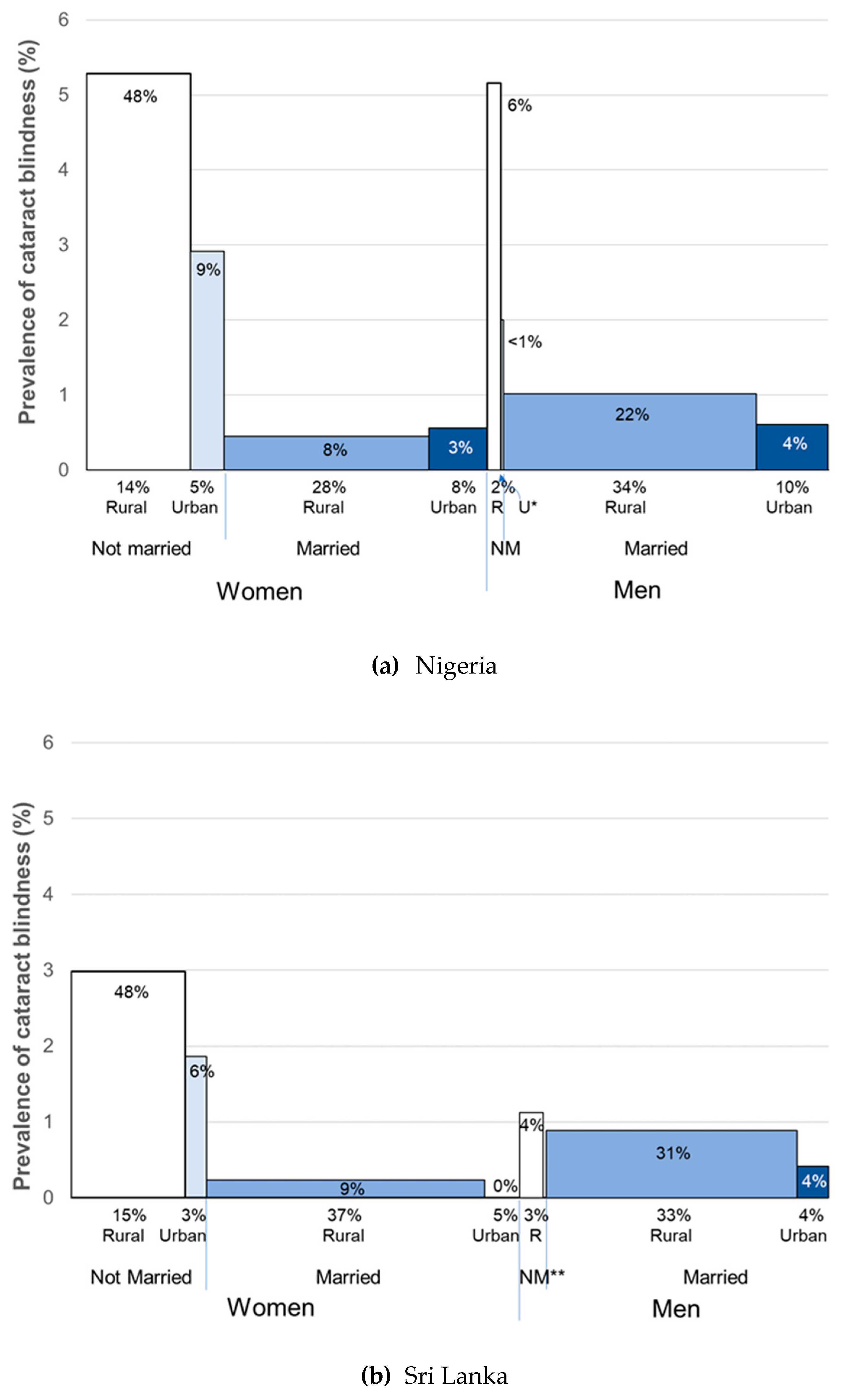
3.2. Cataract Blindness
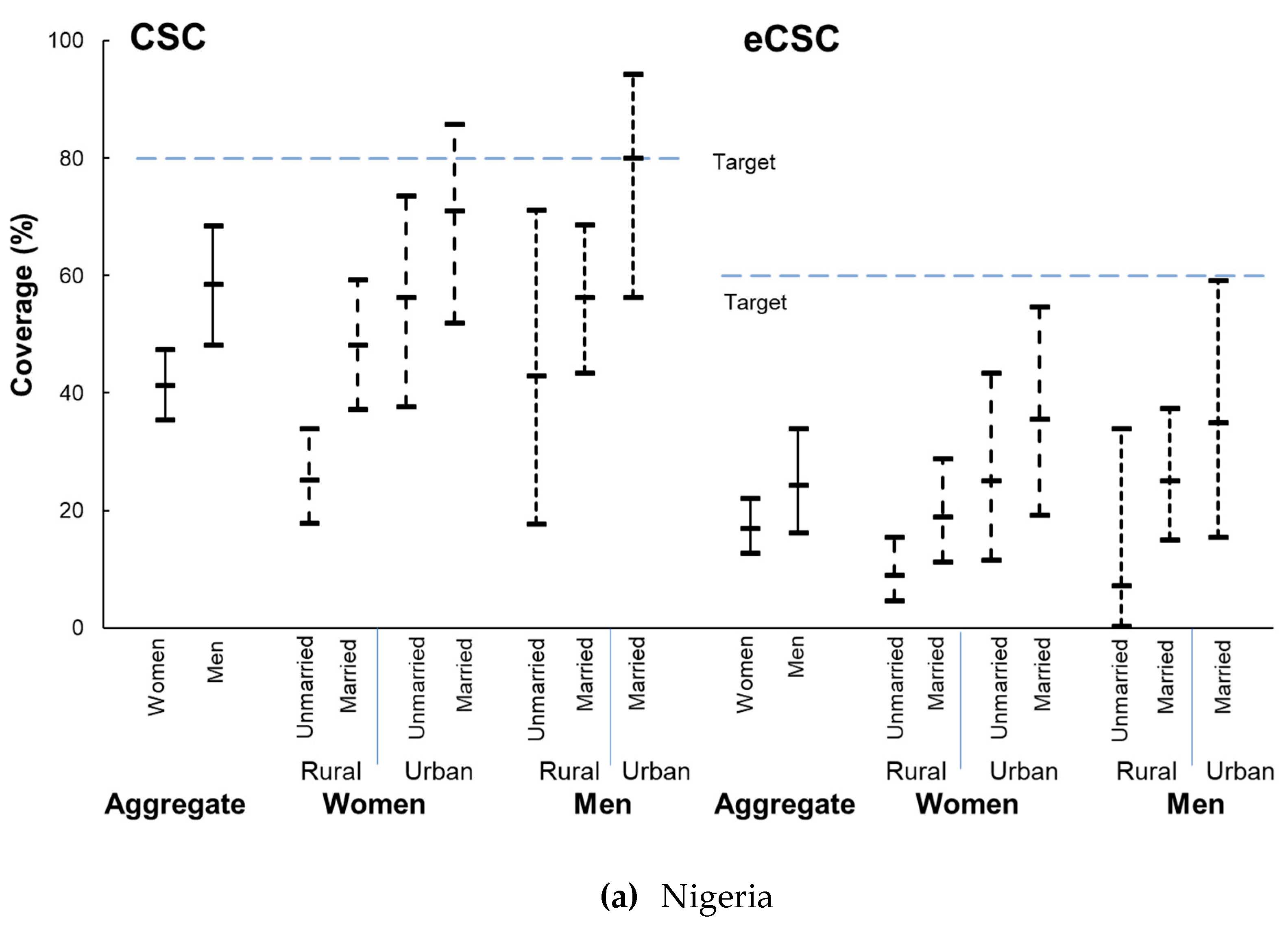
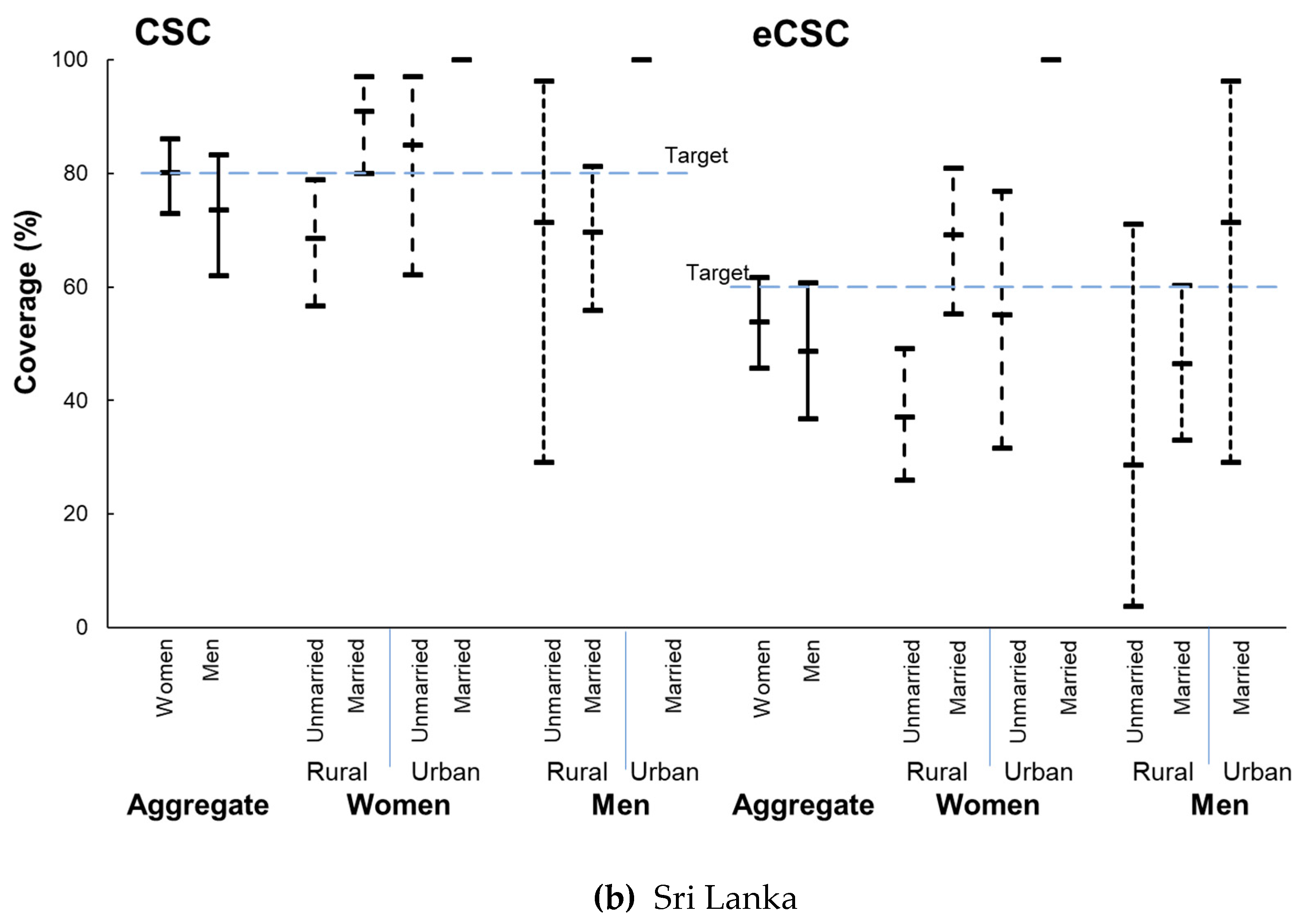
3.3. Cataract Services
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- United Nations General Assembly. Transforming our World: The 2030 Agenda for Sustainable Development. Resolution Adopted by the General Assembly on 25 September 2015. A/RES/70/1; United Nations General Assembly: New York, NY, USA, 2015. [Google Scholar]
- Pratley, P. Associations between quantitative measures of women’s empowerment and access to care and health status for mothers and their children: A systematic review of evidence from the developing world. Soc. Sci. Med. 2016, 169, 119–131. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Women and Health: Today’s Evidence Tomorrow’s Agenda; World Health Organization: Geneva, Switzerland, 2009. [Google Scholar]
- World Health Organization. World Report on Ageing and Health; World Health Organization: Geneva, Switzerland, 2015. [Google Scholar]
- Bourne, R.R.; Stevens, G.A.; White, R.A.; Smith, J.L.; Flaxman, S.R.; Price, H.; Jonas, J.B.; Keeffe, J.; Leasher, J.; Naidoo, K.; et al. Causes of vision loss worldwide, 1990–2010: A systematic analysis. Lancet Glob. Health 2013, 1, e339–e349. [Google Scholar] [CrossRef]
- West, S. Epidemiology of cataract: Accomplishments over 25 years and future directions. Ophthalmic Epidemiol. 2007, 14, 173–178. [Google Scholar] [CrossRef] [PubMed]
- Flaxman, S.; Bourne, R.; Resnikoff, S.; Ackland, P.; Braithwaite, T.; Cicinelli, M.V.; Das, A.; Jonas, J.B.; Keeffe, J.; Kempen, J.H.; et al. Global Causes of Distance Vision Loss: 1990–2015 and projections to 2020. Lancet Glob. Health 2017, 5, e1221–e1234. [Google Scholar] [CrossRef]
- Ravilla, T.D.; Gupta, S.; Ravindran, R.D.; Vashist, P.; Krishnan, T.; Maraini, G.; Chakravarthy, U.; Fletcher, A.E. Use of cooking fuels and cataract in a population-based study: The India Eye Disease Study. Environ. Health Perspect. 2016, 124, 1857–1862. [Google Scholar] [CrossRef]
- Minassian, D.; Mehra, V.; Reidy, A. Childbearing and risk of cataract in young women: An epidemiological study in central India. Br. J. Ophthalmol. 2002, 86, 548–550. [Google Scholar] [CrossRef]
- Tian, Y.; Wu, J.; Xu, G.; Shen, L.; Yang, S.; Mandiwa, C.; Yang, H.; Liang, Y.; Wang, Y. Parity and the risk of cataract: A cross-sectional analysis in the Dongfeng-Tongji cohort study. Br. J. Ophthalmol. 2015, 99, 1650–1654. [Google Scholar] [CrossRef]
- Lewallen, S.; Mousa, A.; Bassett, K.; Courtright, P. Cataract surgical coverage remains lower in women. Br. J. Ophthalmol. 2009, 93, 295–298. [Google Scholar] [CrossRef]
- Ramke, J.; Gilbert, C.; Lee, A.C.L.; Ackland, P.; Limburg, H.; Foster, A. Effective cataract surgical coverage: An indicator for measuring quality-of-care in the context of Universal Health Coverage. PLoS ONE 2017, 12, e0172342. [Google Scholar] [CrossRef]
- Finger, R.P.; Ali, M.; Earnest, J.; Nirmalan, P.K. Cataract surgery in Andhra Pradesh state, India: An investigation into uptake following outreach screening camps. Ophthalmic Epidemiol. 2007, 14, 327–332. [Google Scholar] [CrossRef]
- Geneau, R.; Lewallen, S.; Bronsard, A.; Paul, I.; Courtright, P. The social and family dynamics behind the uptake of cataract surgery: Findings from Kilimanjaro region, Tanzania. Br. J. Ophthalmol. 2005, 89, 1399–1402. [Google Scholar] [CrossRef]
- Wyke, S.; Ford, G. Competing explanations for associations between marital status and health. Soc. Sci. Med. 1992, 34, 523–532. [Google Scholar] [CrossRef]
- Ibrahim, N.; Ramke, J.; Pozo-Martin, F.; Gilbert, C.E. Willingness to pay for cataract surgery is much lower than actual costs in Zamfara state, northern Nigeria. Ophthalmic Epidemiol. 2017, 25, 227–233. [Google Scholar] [CrossRef] [PubMed]
- Dineen, B.; Gilbert, C.E.; Rabiu, M.; Kyari, F.; Mahdi, A.M.; Abubakar, T.; Ezelum, C.C.; Gabriel, E.; Elhassan, E.; Abiose, A.; et al. The Nigerian National Blindness and Visual Impairment Survey: Rationale, objectives and detailed methodology. BMC Ophthalmol. 2008, 8, 17. [Google Scholar] [CrossRef] [PubMed]
- Murthy, G.; Gilbert, C.; Schmidt, E.; Mahipala, P.G.; Gamage, K.M.K.; Banagala, C.; Abeydeera, A.P.; Jeza, A. The Sri Lanka National Blindness, Visual Impairment and Disability Survey: Rationale, objectives and detailed methodology. Ceylon Med. J. 2018, 63, S3–S9. [Google Scholar] [CrossRef]
- Abdull, M.M.; Sivasubramaniam, S.; Murthy, G.V.S.; Gilbert, C.; Abubakar, T.; Ezelum, C.; Rabiu, M.M.; Kotecha, A.; Crabb, D.P.; Spratt, A.; et al. Causes of blindness and visual impairment in Nigeria: The Nigeria National Blindness and Visual Impairment Survey. Investig. Ophthalmol. Vis. Sci. 2009, 50, 4114–4120. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Informal Consultation on Analysis of Blindness Prevention Outcomes; World Health Organization: Geneva, Switzerland, 1998. [Google Scholar]
- Ramke, J.; Zwi, A.B.; Lee, A.C.; Blignault, I.; Gilbert, C.E. Inequality in cataract blindness and services: Moving beyond unidimensional analyses of social position. Br. J. Ophthalmol. 2017, 101, 395–400. [Google Scholar] [CrossRef] [PubMed]
- Tseng, V.L.; Chlebowski, R.T.; Yu, F.; Cauley, J.A.; Li, W.; Thomas, F.; Virnig, B.A.; Coleman, A.L. Association of Cataract Surgery with Mortality in Older Women: Findings from the Women’s Health Initiative. JAMA Ophthalmol. 2018, 136, 3–10. [Google Scholar] [CrossRef]
- Palmer, J.J.; Chinanayi, F.; Gilbert, A.; Pillay, D.; Fox, S.; Jaggernath, J.; Naidoo, K.; Graham, R.; Patel, D.; Blanchet, K. Mapping human resources for eye health in 21 countries of sub-Saharan Africa: Current progress towards VISION 2020. Hum. Resour. Health 2014, 12, 44. [Google Scholar] [CrossRef]
- Estopinal, C.B.; Ausayakhun, S.; Ausayakhun, S.; Jirawison, C.; Bhosai, S.J.; Margolis, T.P.; Keenan, J.D. Access to Ophthalmologic Care in Thailand: A Regional Analysis. Ophthalmic Epidemiol. 2013, 20, 267–273. [Google Scholar] [CrossRef]
- Bourne, R.; Dineen, B.; Jadoon, Z.; Lee, P.S.; Khan, A.; Johnson, G.J.; Foster, A.; Khan, D. Outcomes of cataract surgery in Pakistan: Results from the Pakistan National Blindness and Visual Impairment Survey. Br. J. Ophthalmol. 2007, 91, 420–426. [Google Scholar] [CrossRef] [PubMed]
- Ibrahim, N.; Pozo-Martin, F.; Gilbert, C. Direct non-medical costs double the total direct costs to patients undergoing cataract surgery in Zamfara state, Northern Nigeria: A case series. BMC Health Serv. Res. 2015, 15, 163. [Google Scholar] [CrossRef] [PubMed]
- Mganga, H.; Lewallen, S.; Courtright, P. Overcoming gender inequity in prevention of blindness and visual impairment in Africa. Middle East Afr. J. Ophthalmol. 2011, 18, 98–101. [Google Scholar] [PubMed]
- Courtright, P.; Kanjaloti, S.; Lewallen, S. Barriers to acceptance of cataract surgery among patients presenting to district hospitals in rural Malawi. Trop. Geogr. Med. 1995, 47, 15–18. [Google Scholar]
- Brilliant, G.E.; Lepkowski, J.M.; Zurita, B.; Thulasiraj, R.D. Social determinants of cataract surgery utilization in south India. Arch. Ophthalmol. 1991, 109, 584–589. [Google Scholar] [CrossRef]
- Joseph, S.; Ravilla, T.; Bassett, K. Gender Issues in a Cataract Surgical Population in South India. Ophthalmic Epidemiol. 2013, 20, 96–101. [Google Scholar] [CrossRef]
- Mercer, G.D.; Lyons, P.; Bassett, K. Interventions to improve gender equity in eye care in low-middle income countries: A systematic review. Ophthalmic Epidemiol. 2019, 26, 189–199. [Google Scholar] [CrossRef]
- Polack, S.; Eusebio, C.; Mathenge, W.; Wadud, Z.; Rashid, M.; Foster, A.; Kuper, H. The impact of cataract surgery on activities and time-use: Results from a longitudinal study in Kenya, Bangladesh and the Philippines. PLoS ONE 2010, 5, e10913. [Google Scholar] [CrossRef]
- Sear, R.; Mace, R.; McGregor, I.A. Maternal grandmothers improve nutritional status and survival of children in rural Gambia. Proc. R. Soc. Lond. B Biol. Sci. 2000, 267, 1641–1647. [Google Scholar] [CrossRef]
- Snopkowski, K.; Sear, R. Grandparental help in Indonesia is directed preferentially towards needier descendants: A potential confounder when exploring grandparental influences on child health. Soc. Sci. Med. 2015, 128, 105–114. [Google Scholar] [CrossRef]
- Östlin, P.; Schrecker, T.; Sadana, R.; Bonnefoy, J.; Gilson, L.; Hertzman, C.; Kelly, M.P.; Kjellstrom, T.; Labonté, R.; Lundberg, O.; et al. Priorities for research on equity and health: Towards an equity-focused health research agenda. PLoS Med. 2011, 8, e1001115. [Google Scholar] [CrossRef] [PubMed]
- Stagg, B.C.; Choi, H.; Woodward, M.A.; Ehrlich, J.R. Association of Social Support Network Size with Receipt of Cataract Surgery in Older Adults. JAMA Ophthalmol. 2018, 136, 423–427. [Google Scholar] [CrossRef] [PubMed]
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ramke, J.; Kyari, F.; Mwangi, N.; Piyasena, M.; Murthy, G.; Gilbert, C.E. Cataract Services are Leaving Widows Behind: Examples from National Cross-Sectional Surveys in Nigeria and Sri Lanka. Int. J. Environ. Res. Public Health 2019, 16, 3854. https://doi.org/10.3390/ijerph16203854
Ramke J, Kyari F, Mwangi N, Piyasena M, Murthy G, Gilbert CE. Cataract Services are Leaving Widows Behind: Examples from National Cross-Sectional Surveys in Nigeria and Sri Lanka. International Journal of Environmental Research and Public Health. 2019; 16(20):3854. https://doi.org/10.3390/ijerph16203854
Chicago/Turabian StyleRamke, Jacqueline, Fatima Kyari, Nyawira Mwangi, MMPN Piyasena, GVS Murthy, and Clare E Gilbert. 2019. "Cataract Services are Leaving Widows Behind: Examples from National Cross-Sectional Surveys in Nigeria and Sri Lanka" International Journal of Environmental Research and Public Health 16, no. 20: 3854. https://doi.org/10.3390/ijerph16203854
APA StyleRamke, J., Kyari, F., Mwangi, N., Piyasena, M., Murthy, G., & Gilbert, C. E. (2019). Cataract Services are Leaving Widows Behind: Examples from National Cross-Sectional Surveys in Nigeria and Sri Lanka. International Journal of Environmental Research and Public Health, 16(20), 3854. https://doi.org/10.3390/ijerph16203854





