Our Healthy Clarence: A Community-Driven Wellbeing Initiative
Abstract
1. Introduction
2. Methods
3. Results
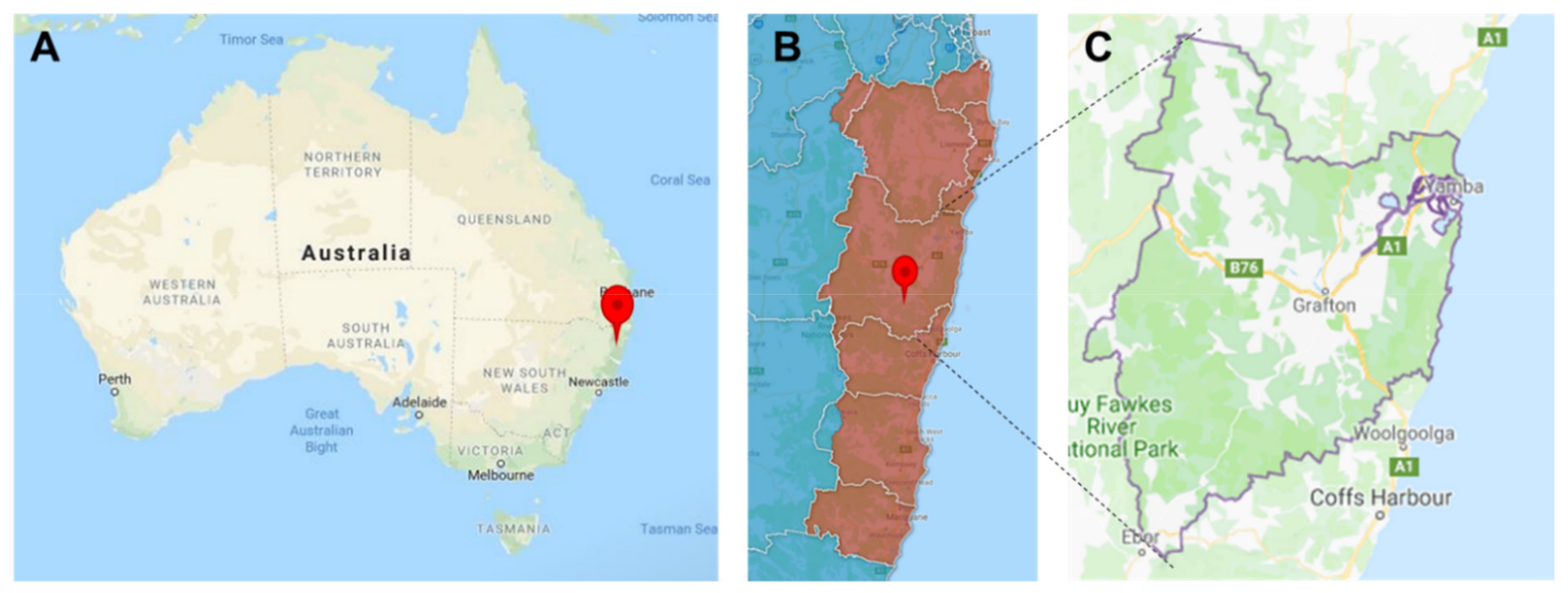
3.1. Clarence Valley Context
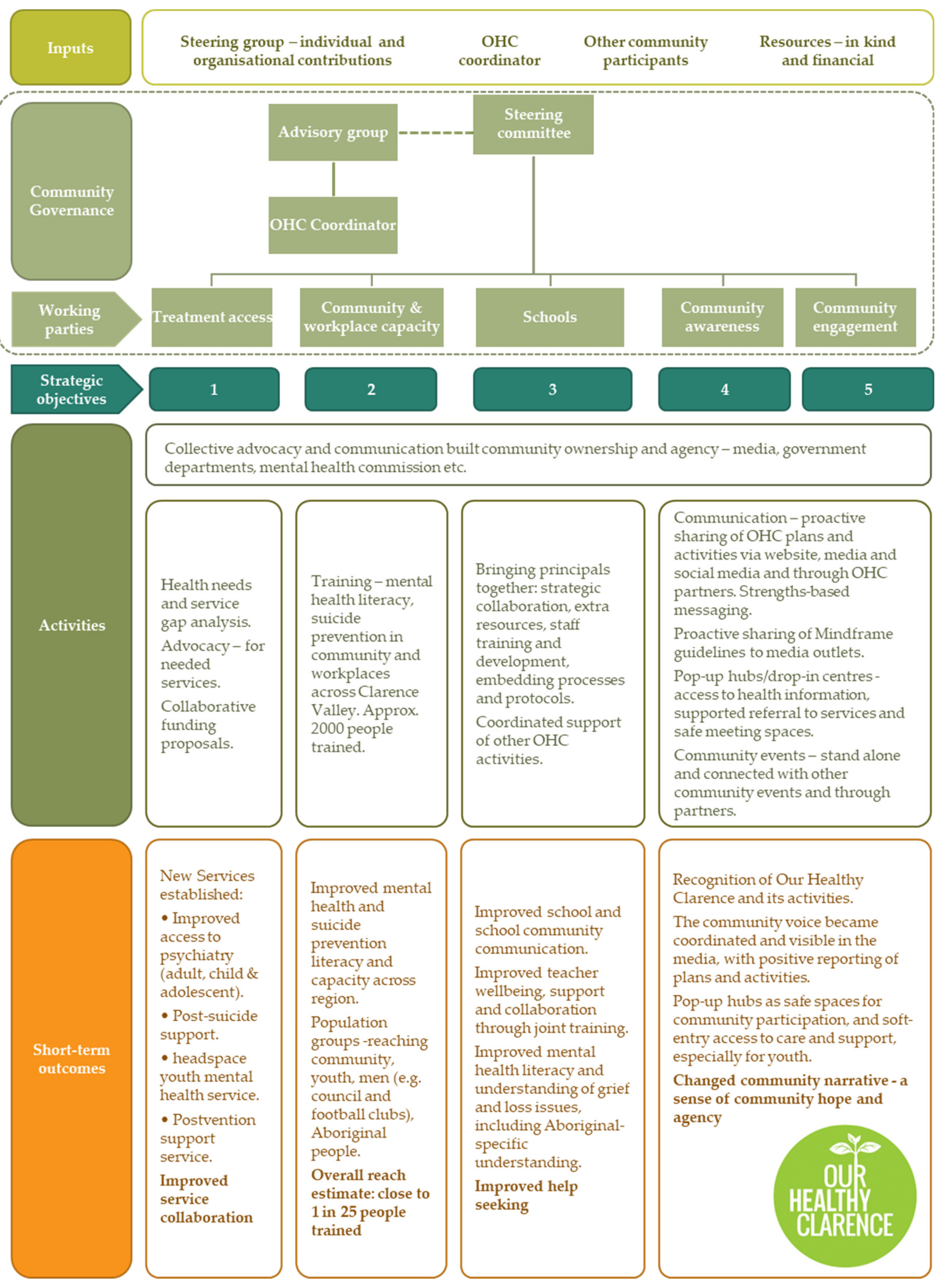
3.2. Our Healthy Clarence
- To improve access for people at risk of self-harm to treatment, crisis care and care after an attempt.
- To improve the ways in which workers and the community respond to people at risk of self-harm.
- To ensure that suitable mental health and wellbeing programs are available in schools.
- To improve community awareness of mental health. This includes how to access information and services.
- To improve our connection with the community. To improve early support for people who are at risk of self-harm and to help prevent self-harm.
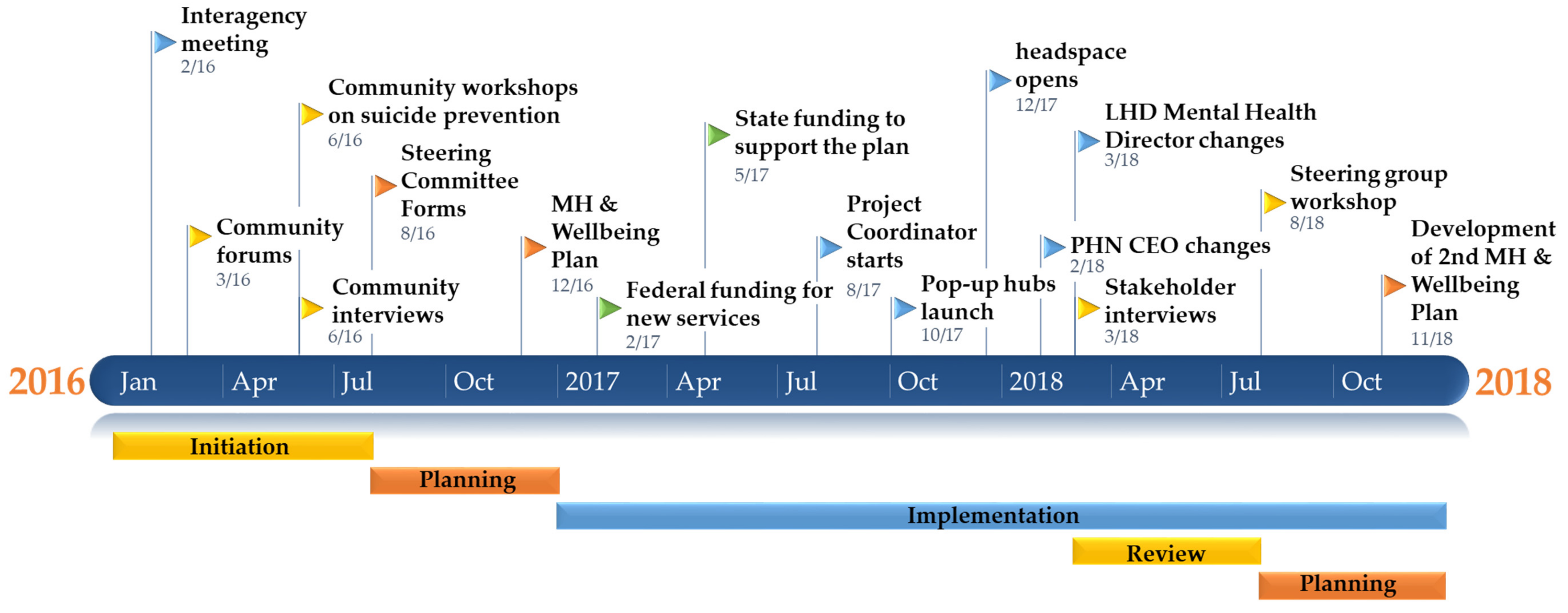
3.3. Description and Progress of Our Healthy Clarence
3.4. Summary of Key Contributory Processes and Identified in Documents and Interviews
3.4.1. The Community-Owned, Codesigned Approach Promoted Engagement and Empowerment
‘… there was a sense that, for it to be successful, it had to come from the community themselves and not someone coming in from a couple of hundred kilometres away, or two hours away, saying how to do things’—Participant 26
‘I think what hasn’t worked well is … keeping the community engaged. Because community were very engaged to start with, extremely engaged. They are the ones that drove that meeting or those three meetings where over 100 people came to each one. More and more, as experts came in, those community members petered out and just went, okay, so we now we know the experts are involved, as does happen, so the engagement didn’t continue.’—Participant 1
‘It actually needs to have a good cross-section of community engaged people sitting on steering, who are from community and not from the services... So I think… the steering membership should have a stronger community presence.’—Participant 18
‘I would say the opportunity missed, in my view, is harnessing the community passion in an effective way early on.’—Participant 6
3.4.2. The Initiative Took a Strengths-Based Approach to Suicide Prevention Via Wellbeing
‘I think it’s about taking the focus away from suicide and bringing that into resilience-building and fostering hope within a community and done through participation, different activities, activities available to young people, things that they can hook into and find meaning from.’—Participant 30
‘The overall effect has been to move … from a deficit kind of conversation to a strength-based hope-filled conversation.’—Participant 35
‘You never know what you’ve got until you actually look about what you have, as far as services go. I mean a lot of areas may or may not have a range of services but they will have some. So, find your strengths; find those local services that know your area, are made up of workers from your area, to really give that focus.’—Participant 2
3.4.3. Governance and Structure were Important to the Success of the Initiative and Matured over Time
‘I have been here a long time; I am completely embarrassed because I am going to a meeting I have no answers for. And then I think well, how would a community member feel?… But somebody has got to lead it. You can’t wait…’—Participant 27
‘My first response was of frustration, because I could see that around the table, we didn’t have the solution, because we didn’t have the decision-makers. But very quickly from there, the initiative grew into something that was actually actively led and supported by people who were more senior, in particular, government organisations.’—Participant 13
‘The early days of the steering committee was very labour-intensive, and it was, in the most part, an adjunct to our day jobs. So, a lot of energy went into it and at one point there was a core group of local service providers that had dubbed it Our Unhealthy Clarence, because we were almost obsessed with it. But it’s kind of that kind of energy, I think that’s needed to get things off the ground.’—Participant 35
‘I feel that what’s worked well is having a coordinator; that’s made a huge difference. I think a lot of the services are already quite strained … It’s helped in my old role to have the flexibility that I had to be able to respond to social issues.’—Participant 4
3.4.4. The Culture of Collaboration Increased Trust, Coordination and Agency
‘I think the services themselves though provide a good starting point to enable action. I think any community is unaware of where to start, it’s quite overwhelming. I think that there needs to be initially that service collaboration to discuss where to from here, in the same way that we did.’—Participant 4
‘There’s been some leadership changes and unfortunately the people that were involved with this mustn’t have kept terribly good notes because [some organisations are now] largely unaware of what Our Heathy Clarence is about.’—Participant 16
3.4.5. The Activities of the Initiative Consistently Reflected the Community Vision
‘I wouldn’t know about half of the services if Our Healthy Clarence hadn’t happened. And that’s coming from someone who already was studying to work in the sector.’—Participant 2
‘The steering committee decided that no service provider at that time or community member really had the capacity to lead that plan, so it was decided that there was a need for a paid worker, and so five organisations committed to co-funding that [coordinator] position and that just made a significant difference…’—Participant 4
‘It has taken a little while just to get the young people used to the hub and used to the people that work here and to get to open up a bit, but what makes us different is we’re running with youth workers in charge as opposed to just volunteers or centre staff. So if we overhear a conversation or if a young person approaches us with concerns that they have we’re able to address them by referring them on to services.’—Participant 14
‘Activities, so many activities– having come from the Hunter Valley there is nothing- there are so many activities here for the kids and it’s really pushed quite effectively through all forms of social media. Having arrived here and new to the town and not knowing anyone – we don’t have any family here or anything—I accessed that information quite quickly and really easily.’—Participant 10
‘They act as a fantastic consultative body to—I mean, they’re part of the steering committee but if we’re thinking about doing a youth event, then we do it with them and they help us be on track and make sure that we’re hitting the objectives of what the young kids want. So that’s been a huge masterplan, the number of events that they’ve led and initiated.’—Participant 23
3.4.6. OHC Coincided with a Changed Community Narrative of Hope and Agency
‘The community narrative has certainly changed. No longer do I hear we’re a community that’s been forgotten; I’m not hearing about we’re a community where all our young people are dying, that it’s a suicide town, that there’s nothing here for the kids, why doesn’t government people do something for our community? That’s changed, that’s changed. There’s been a real change in narrative where it’s now shifting to, what can we do to ensure the mental health and wellbeing. That’s the focus and that’s hard to measure but it’s certainly out there happening.’—Participant 23
‘Now, with that collaborative stuff, there is that sense that we can work together, we can achieve anything. And that’s not just with mental health, that’s actually with a couple of other social issues that have come up recently, we’ve done it before so we can do it again.’—Participant 4
‘I think that heat has gone out, if you like, or the anxiety has gone out of the community, but it would return very quickly if there was another teenager take their own life down there again. But what I do think is much better now, is the network of people, and they would together really, really quickly and look at a community response, rather than an ad-hoc, lots of different, smaller responses …I think that would be an improvement as a result of Our Healthy Clarence.’—Participant 26
4. Discussion
Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Ziersch, A.M.; Baum, F.; Darmawan, I.G.N.; Kavanagh, A.M.; Bentley, R.J. Social capital and health in rural and urban communities in South Australia. Aust. N. Z. J. Public Health 2009, 33, 7–16. [Google Scholar] [CrossRef] [PubMed]
- Onyx, J.; Bullen, P. Measuring social capital in five communities. J. Appl. Behav. Sci. 2000, 36, 23–42. [Google Scholar] [CrossRef]
- Sørensen, J.F. Rural–urban differences in bonding and bridging social capital. Reg. Stud. 2016, 50, 391–410. [Google Scholar] [CrossRef]
- Sørensen, J.F. Rural–urban differences in life satisfaction: Evidence from the European Union. Reg. Stud. 2014, 48, 1451–1466. [Google Scholar] [CrossRef]
- Beard, J.R.; Tomaska, N.; Earnest, A.; Summerhayes, R.; Morgan, G. Influence of socioeconomic and cultural factors on rural health. Aust. J. Rural Health 2009, 17, 10–15. [Google Scholar] [CrossRef] [PubMed]
- Judd, F.; Cooper, A.-M.; Fraser, C.; Davis, J. Rural suicide—People or place effects? Aust. N. Z. J. Psychiatry 2006, 40, 208–216. [Google Scholar] [PubMed]
- Meadows, G.N.; Enticott, J.C.; Inder, B.; Russell, G.M.; Gurr, R. Better access to mental health care and the failure of the Medicare principle of universality. Med. J. Aust. 2015, 202, 190–194. [Google Scholar] [CrossRef] [PubMed]
- Collins, J.; Ward, B.M.; Snow, P.; Kippen, S.; Judd, F. Compositional, contextual, and collective community factors in mental health and well-being in Australian rural communities. Qual. Health Res. 2017, 27, 677–687. [Google Scholar] [CrossRef]
- Vos, T.; Begg, S.; Chen, Y.; Magnus, A. Socioeconomic differentials in life expectancy and years of life lost in Victoria, 1992–1996. N. S. W. Public Health Bull. 2001, 12, 126–130. [Google Scholar] [CrossRef] [PubMed]
- Singh, G.K.; Siahpush, M. Widening rural–urban disparities in life expectancy, US, 1969–2009. Am. J. Prev. Med. 2014, 46, e19–e29. [Google Scholar] [CrossRef]
- Heathcote, K.E.; Armstrong, B.K. Disparities in cancer outcomes in regional and rural Australia. Cancer Forum 2017, 31, 70–74. [Google Scholar]
- Pong, R.W.; DesMeules, M.; Lagacé, C. Rural–urban disparities in health: How does Canada fare and how does Canada compare with Australia? Aust. J. Rural Health 2009, 17, 58–64. [Google Scholar] [CrossRef] [PubMed]
- Australian Institute of Health and Welfare. Rural & Remote Health; AIHW: Canberra, Australia, 2017. [Google Scholar]
- Hazell, T.; Dalton, H.; Caton, T.; Perkins, D. Rural Suicide and Its Prevention: A CRRMH Position Paper; Centre for Rural and Remote Mental Health: Orange, Australia; University of Newcastle: Callaghan, Australia, 2017. [Google Scholar]
- Australian Bureau of Statistics. Socio-Economic Advantage and Disadvantage. Available online: https://www.abs.gov.au/ausstats/abs@.nsf/Lookup/by%20Subject/2071.0~2016~Main%20Features~Socio-Economic%20Advantage%20and%20Disadvantage~123 (accessed on 17 July 2019).
- National Rural Health Alliance. Mental Health in Rural and Remote Australia. Available online: https://www.ruralhealth.org.au/sites/default/files/publications/nrha-mental-health-factsheet-dec-2017.pdf (accessed on 16 July 2019).
- Haggerty, R.J.; Mrazek, P.J. Reducing Risks for Mental Disorders: Frontiers for Preventive Intervention Research; National Academies Press: Washington, DC, USA, 1994. [Google Scholar]
- Everymind. Prevention First (Adapted): A Framework for Suicide Prevention; Everymind: Newcastle, Australia, 2015. [Google Scholar]
- Allen, J.; Balfour, R.; Bell, R.; Marmot, M. Social determinants of mental health. Int. Rev. Psychiatry 2014, 26, 392–407. [Google Scholar] [CrossRef]
- Australian Bureau of Statistics. Causes of Death 2017; Australian Bureau of Statistics: Canberra, Australia, 2018. [Google Scholar]
- World Health Organization. Preventing Suicide: A Global Imperative; World Health Organization: Geneva, Switzerland, 2014. [Google Scholar]
- Lasker, R.D.; Weiss, E.S. Broadening participation in community problem solving: A multidisciplinary model to support collaborative practice and research. J. Urban Health 2003, 80, 14–47. [Google Scholar] [CrossRef] [PubMed]
- Nikkhah, H.A.; Redzuan, M. Participation as a medium of empowerment in community development. Eur. J. Soc. Sci. 2009, 11, 170–176. [Google Scholar]
- Laverack, G. Improving Health Outcomes through Community Empowerment: A Review of the Literature. J. Health Popul. Nutr. 2006, 24, 113–120. [Google Scholar] [PubMed]
- Baum, F. Cracking the nut of health equity: Top down and bottom up pressure for action on the social determinants of health. Promot. Educ. 2007, 14, 90–95. [Google Scholar] [CrossRef] [PubMed]
- Stetler, C.B.; Legro, M.W.; Wallace, C.M.; Bowman, C.; Guihan, M.; Hagedorn, H.; Kimmel, B.; Sharp, N.D.; Smith, J.L. The role of formative evaluation in implementation research and the QUERI experience. J. Gen. Intern. Med. 2006, 21, S1. [Google Scholar] [CrossRef] [PubMed]
- QSR International Pty Ltd. NVivo Qualitative Data Analysis Software; QSR International Pty Ltd.: Warrington, UK, 2015. [Google Scholar]
- Braun, V.; Clarke, V. Using thematic analysis in psychology. Qual. Res. Psychol. 2006, 3, 77–101. [Google Scholar] [CrossRef]
- Braun, V.; Clarke, V. What can “thematic analysis” offer health and wellbeing researchers? Int. J. Qual. Stud. Health Well Being 2014, 9. [Google Scholar] [CrossRef]
- Ezzy, D. Qualitative Analysis: Practice and Innovation/Douglas Ezzy; Allen & Unwin: Crows Nest, Australia, 2002. [Google Scholar]
- Carroll, J.B.; McKenna, J. Theory to practice: Using the Logic Model to organize and report research results in a collaborative project. J. Fam. Consum. Sci. 2001, 93, 63. [Google Scholar]
- Kaplan, S.A.; Garrett, K.E. The use of logic models by community-based initiatives. Eval. Program Plan. 2005, 28, 167–172. [Google Scholar] [CrossRef]
- Northern NSW Local Health District. About the NNSWLHD. Available online: https://nnswlhd.health.nsw.gov.au/about/northern-nsw-local-health-district/ (accessed on 5 July 2019).
- North Coast Primary Health Network. Our Region. Available online: https://ncphn.org.au/our-region (accessed on 5 July 2019).
- Australian Bureau of Statistics. Census of Population and Housing: Socio-Economic Indexes for Areas (SEIFA). Available online: https://www.abs.gov.au/ausstats/abs@.nsf/Lookup/by%20Subject/2033.0.55.001~2016~Main%20Features~SOCIO-ECONOMIC%20INDEXES%20FOR%20AREAS%20(SEIFA)%202016~1 (accessed on 5 July 2019).
- NSW Government. HealthStats NSW. Available online: http://www.healthstats.nsw.gov.au/ (accessed on 5 July 2019).
- Black Dog Insititute. About LifeSpan. Available online: https://www.blackdoginstitute.org.au/research/lifespan/overview (accessed on 6 September 2019).
- Donovan, R.J.; James, R.; Jalleh, G.; Sidebottom, C. Implementing Mental Health Promotion: The Act–Belong–Commit Mentally Healthy WA Campaign in Western Australia. Int. J. Ment. Health Promot. 2006, 8, 33–42. [Google Scholar] [CrossRef]
- World Health Organisation. Risks to Mental Health: An Overview of Vulnerabilities and Risk Factors; World Health Organisation: Geneva, Switzerland, 2012. [Google Scholar]
- NSW Department of Health. NSW Community Mental Health Strategy 2007–2012: From Prevention and Early Intervention to Recovery; NSW Department of Health: Sydney, Australia, 2008. [Google Scholar]
- Our Healthy Clarence. Our Healthy Clarence. Available online: https://www.ourhealthyclarence.org.au/minutes-literature (accessed on 25 June 2019).
- Mann, J.J.; Apter, A.; Bertolote, J.; Beautrais, A.; Currier, D.; Haas, A.; Hegerl, U.; Lonnqvist, J.; Malone, K.; Marusic, A. Suicide prevention strategies: A systematic review. JAMA 2005, 294, 2064–2074. [Google Scholar] [CrossRef] [PubMed]
- Reynolds, J.; DiLiberto, D.; Mangham-Jefferies, L.; Ansah, E.K.; Lal, S.; Mbakilwa, H.; Bruxvoort, K.; Webster, J.; Vestergaard, L.S.; Yeung, S. The practice of ‘doing’ evaluation: Lessons learned from nine complex intervention trials in action. Implement. Sci. 2014, 9, 75. [Google Scholar] [CrossRef]
- Moore, G.F.; Audrey, S.; Barker, M.; Bond, L.; Bonell, C.; Hardeman, W.; Moore, L.; O’Cathain, A.; Tinati, T.; Wight, D. Process evaluation of complex interventions: Medical Research Council guidance. BMJ 2015, 350, h1258. [Google Scholar] [CrossRef] [PubMed]
- Kagan, C.; Kilroy, A. Psychology in the community. In Well-Being; Springer: Berlin, Germany, 2007; pp. 93–109. [Google Scholar]
- Gilligan, C.; Sanson-Fisher, R.; Shakeshaft, A. Appropriate Research Designs for Evaluating Community-level Alcohol Interventions: What Next? Alcohol Alcohol. 2010, 45, 481–487. [Google Scholar] [CrossRef]
| Theme | Sub-Theme |
|---|---|
| The community-owned, codesigned approach promoted engagement and empowerment | The community decided priorities which promoted buy-in |
| Multiple channels of engagement promoted representation | |
| Engagement should be harnessed while it is present | |
| Community readiness can arise from a variety of circumstances | |
| The initiative took a strengths-based approach to suicide prevention via wellbeing | The wellbeing approach helped the community build after tragedy |
| The wellbeing approach gave a broader reach into community | |
| The strengths-based approach got the community to realise its assets | |
| Policy and programs focused on suicide prevention as a negative construct conflicted with the community desire to focus on community wellbeing as a positive approach | |
| Governance and structure were important to the success of the initiative and matured over time | Early forums made it clear that community were drivers |
| Professional support assisted the governance of the initiative | |
| Collaboration helped to realise the vision | |
| Positions were given the flexibility to adapt to community needs | |
| The committee had to balance inclusivity and size | |
| The committee had to balance transparency, sensitivity and confidentiality | |
| The culture of collaboration increased trust, coordination and agency | Service collaboration was an approachable goal to begin |
| The experience of collaboration built empowerment within the group | |
| Consistency between institutions improved services | |
| Personnel changes created challenges for collaboration | |
| The activities of the initiative consistently reflected the community vision | Services became more accessible as the vision developed |
| The pop-up hubs go beyond traditional community centres | |
| Existing community networks were used to reach into community | |
| Willingness for mental health training helped to build awareness and capacity | |
| OHC coincided with a changed community narrative of hope and agency | The community transitioned from fear to hope |
| The community became more willing to solve problems in the context of their strengths | |
| The community developed the perception that their concerns were heard and addressed | |
| Positive stories across the community were important to build hope | |
| Community hope could be threatened in the event of a suicide |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Powell, N.; Dalton, H.; Perkins, D.; Considine, R.; Hughes, S.; Osborne, S.; Buss, R. Our Healthy Clarence: A Community-Driven Wellbeing Initiative. Int. J. Environ. Res. Public Health 2019, 16, 3691. https://doi.org/10.3390/ijerph16193691
Powell N, Dalton H, Perkins D, Considine R, Hughes S, Osborne S, Buss R. Our Healthy Clarence: A Community-Driven Wellbeing Initiative. International Journal of Environmental Research and Public Health. 2019; 16(19):3691. https://doi.org/10.3390/ijerph16193691
Chicago/Turabian StylePowell, Nicholas, Hazel Dalton, David Perkins, Robyn Considine, Sue Hughes, Samantha Osborne, and Richard Buss. 2019. "Our Healthy Clarence: A Community-Driven Wellbeing Initiative" International Journal of Environmental Research and Public Health 16, no. 19: 3691. https://doi.org/10.3390/ijerph16193691
APA StylePowell, N., Dalton, H., Perkins, D., Considine, R., Hughes, S., Osborne, S., & Buss, R. (2019). Our Healthy Clarence: A Community-Driven Wellbeing Initiative. International Journal of Environmental Research and Public Health, 16(19), 3691. https://doi.org/10.3390/ijerph16193691





