Application of the Theory of Planned Behavior to Predict Dental Attendance and Caries Experience among Children of Newcomers
Abstract
1. Introduction
2. Methods
2.1. Setting and Sampling
2.2. Data Collection
2.3. Dental Examination
2.4. Statistical Analysis
3. Results
3.1. Participates Characteristics
3.2. Scale Reliability
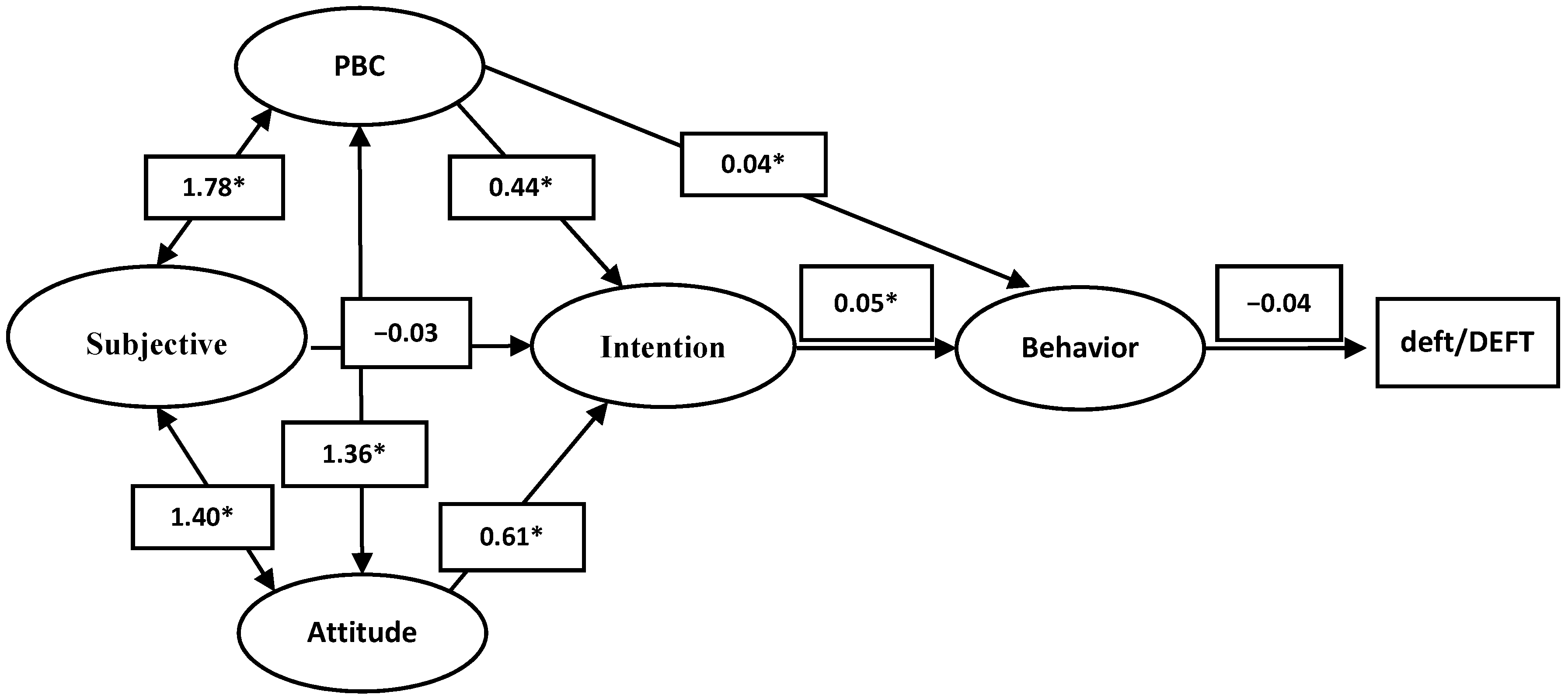
3.3. Structural Equation Modeling
4. Discussion
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Appendix A. Scale Reliability Measure
| Item | Scale Mean If Item Deleted | Scale Variance If Item Deleted | Corrected Item-Total Correlation | Squared Multiple Correlation | Cronbach’s Alpha If Item Deleted |
| PBC_1 | 85.01 | 360.271 | 0.436 | 0.380 | 0.884 |
| PBC_2 | 84.31 | 356.023 | 0.576 | 0.498 | 0.878 |
| PBC_3 | 83.91 | 357.743 | 0.653 | 0.585 | 0.876 |
| Subjective norm_1 | 83.99 | 362.047 | 0.548 | 0.446 | 0.879 |
| Subjective norm_2 | 84.08 | 353.942 | 0.656 | 0.513 | 0.876 |
| Subjective norm_3 | 84.70 | 349.850 | 0.638 | 0.577 | 0.876 |
| Subjective norm_4 | 84.85 | 357.151 | 0.620 | 0.547 | 0.877 |
| Subjective norm_5 | 84.25 | 351.559 | 0.653 | 0.464 | 0.875 |
| Subjective norm_6 | 85.15 | 358.736 | 0.478 | 0.593 | 0.882 |
| Subjective norm_7 | 84.92 | 367.513 | 0.427 | 0.309 | 0.884 |
| Subjective norm_8 | 84.45 | 353.897 | 0.591 | 0.524 | 0.878 |
| Subjective norm_9 | 84.83 | 359.649 | 0.466 | 0.540 | 0.883 |
| Attitude_1 | 83.91 | 363.959 | 0.494 | 0.374 | 0.881 |
| Attitude_2 | 84.32 | 367.492 | 0.460 | 0.392 | 0.883 |
| Attitude_3 | 83.49 | 364.573 | 0.644 | 0.554 | 0.877 |
| Attitude_4 | 84.78 | 384.936 | 0.195 | 0.242 | 0.892 |
| Attitude_5 | 83.91 | 364.703 | 0.554 | 0.486 | 0.879 |
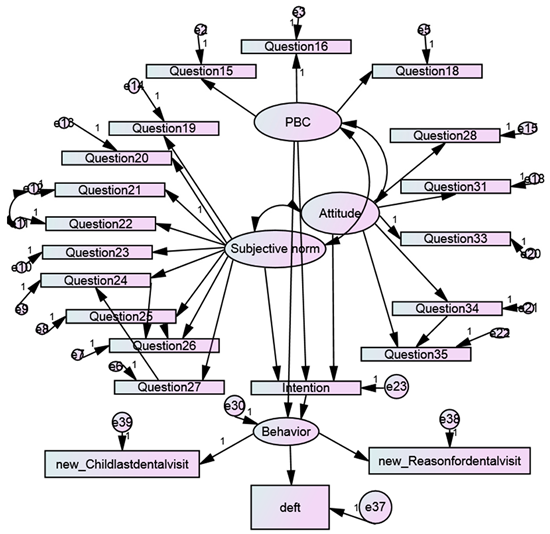
Appendix B. AMOS Model Diagram
References
- Amin, M.; Perez, A.; Nyachhyon, P. Parental Awareness and Dental Attendance of Children Among African Immigrants. J. Immigr. Minority Health Cent. Minor. Public Health 2013. [Google Scholar] [CrossRef] [PubMed]
- Vargas, C.M.; Ronzio, C.R. Disparities in early childhood caries. BMC Oral Health 2006, 6. [Google Scholar] [CrossRef] [PubMed]
- Gao, X.L.; McGrath, C. A review on the oral health impacts of acculturation. J. Immigr. Minor. Health Cent. Minor. Public Health 2011, 13, 202–213. [Google Scholar] [CrossRef] [PubMed]
- Sheiham, A. Is there a scientific basis for six-monthly dental examinations? Lancet 1977, 2, 442–444. [Google Scholar] [CrossRef]
- Newbold, K.B.; Patel, A. Use of dental services by immigrant Canadians. J. Can. Dent. Assoc. 2006, 72, 143. [Google Scholar] [PubMed]
- Badri, P.; Saltaji, H.; Flores-Mir, C.; Amin, M. Factors affecting children’s adherence to regular dental attendance: A systematic review. J. Am. Dent. Assoc. 2014, 145, 817–828. [Google Scholar] [CrossRef]
- Armitage, C.J.; Conner, M. Efficacy of the Theory of Planned Behaviour: A meta-analytic review. Br. J. Soc. Psychol. 2001, 40, 471–499. [Google Scholar] [CrossRef]
- Ajzen, I. The theory of planned behavior. Organ. Behav. Hum. Decis. Process. 1991, 50, 179–211. [Google Scholar] [CrossRef]
- Astrom, A.N.; Lie, S.A.; Gulcan, F. Applying the theory of planned behavior to self-report dental attendance in Norwegian adults through structural equation modelling approach. BMC Oral Health 2018, 18, 95. [Google Scholar] [CrossRef]
- Luzzi, L.; Spencer, A.J. Factors influencing the use of public dental services: An application of the Theory of Planned Behaviour. BMC Health Serv. Res. 2008, 8, 93. [Google Scholar] [CrossRef]
- Dahlan, R.; Badri, P.; Saltaji, H.; Amin, M. Impact of acculturation on oral health among immigrants and ethnic minorities: A systematic review. PLoS ONE 2019, 14, e0212891. [Google Scholar] [CrossRef] [PubMed]
- Amin, M.; ElSalhy, M. Factors Affecting Dental Attendance of Children of New Immigrant Parents: A Cross-Sectional Study. J. Immigr. Minority Health Cent. Minor. Public Health 2017, 19, 1351–1361. [Google Scholar] [CrossRef] [PubMed]
- Elyasi, M.; Abreu, L.G.; Olsen, C.; Baker, S.R.; Lai, H.; Major, P.W.; Amin, M. Parent’s Sense of Coherence and Children’s Oral Health-Related Behaviors: Is There an Association? Pediatr. Dent. 2018, 40, 23–29. [Google Scholar] [PubMed]
- Van den Branden, S.; Van den Broucke, S.; Leroy, R.; Declerck, D.; Hoppenbrouwers, K. Measuring determinants of oral health behaviour in parents of preschool children. Community Dent. Health 2013, 30, 19–25. [Google Scholar] [PubMed]
- World Health Organization. Oral Health Surveys: Basic Methods, 5th ed.; World Health Organization: Geneva, Switzerland, 2013. [Google Scholar]
- Brown, T.A. Confirmatory Factor Analysis for Applied Research, 2nd ed.; The Guilford Press: New York, NY, USA, 2015; p. 462. [Google Scholar]
- Hu, L.; Bentler, P.M. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Struct. Equ. Model. A Multidiscip. J. 1999, 6, 1–55. [Google Scholar] [CrossRef]
- Santos, J.R.A. Cronbach’s alpha: A tool for assessing the reliability of scales. J. Ext. 1999, 37, 88–92. [Google Scholar]
- Beirne, P.; Clarkson, J.E.; Worthington, H.V. Recall intervals for oral health in primary care patients. Cochrane Database Syst. Rev. 2007. [Google Scholar] [CrossRef]
- Riley, P.; Worthington, H.V.; Clarkson, J.E.; Beirne, P.V. Recall intervals for oral health in primary care patients. Cochrane Database Syst Rev. 2013. [Google Scholar] [CrossRef]
- Fisher-Owens, S.A.; Gansky, S.A.; Platt, L.J.; Weintraub, J.A.; Soobader, M.J.; Bramlett, M.D.; Newacheck, P.W. Influences on children’s oral health: A conceptual model. Pediatrics 2007, 120, 510–520. [Google Scholar] [CrossRef]
- Crocombe, L.A.; Broadbent, J.M.; Thomson, W.M.; Brennan, D.S.; Poulton, R. Impact of dental visiting trajectory patterns on clinical oral health and oral health-related quality of life. J. Public Health Dent. 2012, 72, 36–44. [Google Scholar] [CrossRef]
- Elyasi, M.; Abreu, L.G.; Badri, P.; Saltaji, H.; Flores-Mir, C.; Amin, M. Impact of Sense of Coherence on Oral Health Behaviors: A Systematic Review. PLoS ONE 2015, 10, e0133918. [Google Scholar] [CrossRef] [PubMed]
- Antonovsky, A. The structure and properties of the sense of coherence scale. Soc. Sci Med. 1993, 36, 725–733. [Google Scholar] [CrossRef]
- Beran, T.N.; Violato, C. Structural equation modeling in medical research: A primer. BMC Res. Notes 2010, 3, 267. [Google Scholar] [CrossRef] [PubMed]
| Child’s age | deft/DEFT (Caries experience) | ||
|---|---|---|---|
| Mean | 4.53 | Mean | 3.28 |
| Median | 4 | Median | 2 |
| SD (range) | 2.98 (1–12) | SD (range) | 3.76 (0–16) |
| Children of a female gender (N) (%) | 150 (55.0) | Children with dental insurance (N) (%) | 116 (42.3) |
| Children born in Canada (N) (%) | 148 (54.9) | Children’s last dental visit within a year (N) (%) | 94 (34.3) |
| Mother’s age | Reason for visit (N) (%) | ||
| Mean | 34.92 | Check up | 63 (23.0) |
| Median | 34 | Treatment | 32 (11.6) |
| SD | 6.35 | Tooth brushing frequency (N) (%) | |
| <twice/day | 172 (62.8) | ||
| ≥twice/day | 102 (37.2) | ||
| Number of Children in family (N) (%) | Sugar intake frequency (N) (%) | ||
| ≤2 | 218 (79.5) | ≤once/day | 179 (65.3) |
| 3 or more | 56 (20.5) | ≥twice/day | 95 (34.7) |
| Mother’s education level (N) (%) | Monthly income (N) (%) | ||
| High school | 117 (42.7) | ≤1999 | 103 (37.5) |
| College | 51 (18.6) | 2000–3999 | 107 (39.0) |
| University | 106 (38.6) | ≥4000 | 64 (23.3) |
| Living with both parents | Years in Canada (N) (%) | ||
| N (%) | 235 (85.7) | ≤5 years | 112 (40.9) |
| Estimate | S.E. | C.R. | P | |||
|---|---|---|---|---|---|---|
| PBC | <--> | Subjective Norm | 1.788 | 0.246 | 7.274 | 0.001 |
| PBC | <--> | Attitude | 1.366 | 0.188 | 7.247 | 0.001 |
| Subjective Norm | <--> | Attitude | 1.405 | 0.174 | 5.630 | 0.001 |
| Items | Estimate | SE | CR | p-Value | ||
|---|---|---|---|---|---|---|
| PBC_1 | <---> | PBC | 0.579 | 0.099 | 8.861 | 0.001 |
| PBC_2 | <---> | PBC | 0.757 | |||
| PBC_3 | <---> | PBC | 0.774 | 0.076 | 11.698 | 0.001 |
| Subjective norm_1 | <---> | Subjective norm | 0.604 | 0.094 | 8.676 | 0.001 |
| Subjective norm_2 | <---> | Subjective norm | 0.731 | 0.099 | 10.179 | 0.001 |
| Subjective norm_3 | <---> | Subjective norm | 0.658 | |||
| Subjective norm_4 | <---> | Subjective norm | 0.635 | 0.071 | 12.074 | 0.001 |
| Subjective norm_5 | <---> | Subjective norm | 0.704 | 0.103 | 9.877 | 0.001 |
| Subjective norm_6 | <---> | Subjective norm | 0.166 | 0.087 | 3.107 | 0.002 |
| Subjective norm_7 | <---> | Subjective norm | 0.472 | 0.098 | 6.965 | 0.001 |
| Subjective norm_8 | <---> | Subjective norm | 0.399 | 0.094 | 6.371 | 0.001 |
| Subjective norm_9 | <---> | Subjective norm | 0.436 | 0.11 | 6.466 | 0.001 |
| Attitude_1 | <---> | Attitude | 0.609 | 0.091 | 10.127 | 0.001 |
| Attitude_2 | <---> | Attitude | 0.601 | 0.089 | 9.969 | 0.001 |
| Attitude_3 | <---> | Attitude | 0.842 | |||
| Attitude_4 | <---> | Attitude | 0.29 | 0.101 | 4.482 | 0.001 |
| Attitude_5 | <---> | Attitude | 0.593 | 0.077 | 10.407 | 0.001 |
| Last child dental visit | <---> | Behavior | −0.228 | 0.292 | −0.208 | 0.835 |
| Reason for dental visit | <---> | Behavior | 3.321 | |||
| Intention | <---> | Subjective norm | −0.301 | 0.241 | −1.598 | 0.11 |
| Intention | <---> | Attitude | 0.61 | 0.167 | 5.032 | 0.001 |
| Intention | <---> | PBC | 0.441 | 0.174 | 2.904 | 0.004 |
| Behavior | <---> | PBC | 0.042 | 0.022 | 1.993 | 0.046 |
| Behavior | <---> | Intention | 0.049 | 0.019 | −2.365 | 0.018 |
| DEFT/deft | <---> | Behavior | −0.037 | 0.439 | −0.197 | 0.844 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Amin, M.; Elyasi, M.; Bohlouli, B.; ElSalhy, M. Application of the Theory of Planned Behavior to Predict Dental Attendance and Caries Experience among Children of Newcomers. Int. J. Environ. Res. Public Health 2019, 16, 3661. https://doi.org/10.3390/ijerph16193661
Amin M, Elyasi M, Bohlouli B, ElSalhy M. Application of the Theory of Planned Behavior to Predict Dental Attendance and Caries Experience among Children of Newcomers. International Journal of Environmental Research and Public Health. 2019; 16(19):3661. https://doi.org/10.3390/ijerph16193661
Chicago/Turabian StyleAmin, Maryam, Maryam Elyasi, Babak Bohlouli, and Mohamed ElSalhy. 2019. "Application of the Theory of Planned Behavior to Predict Dental Attendance and Caries Experience among Children of Newcomers" International Journal of Environmental Research and Public Health 16, no. 19: 3661. https://doi.org/10.3390/ijerph16193661
APA StyleAmin, M., Elyasi, M., Bohlouli, B., & ElSalhy, M. (2019). Application of the Theory of Planned Behavior to Predict Dental Attendance and Caries Experience among Children of Newcomers. International Journal of Environmental Research and Public Health, 16(19), 3661. https://doi.org/10.3390/ijerph16193661





