Metabolic Unhealthiness Increases the Likelihood of Having Metabolic Syndrome Components in Normoweight Young Adults
Abstract
1. Introduction
2. Materials and Methods
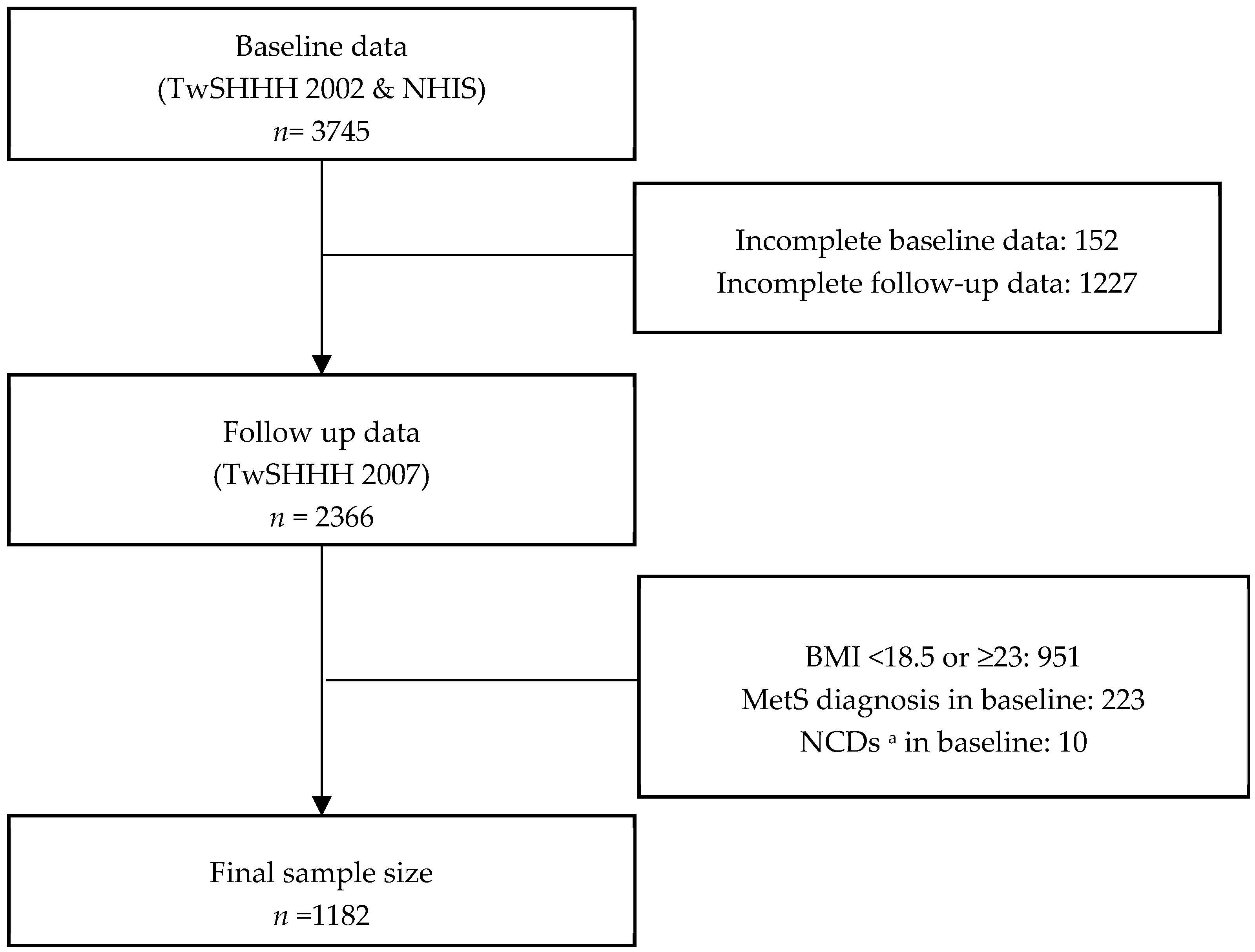
2.1. Study Population
2.2. MetS
2.3. Outcome
2.4. Covariates
2.5. Statistical Analysis
3. Results
3.1. Baseline and Follow-Up Characteristics
3.2. Baseline Prevalence, Follow-Up Prevalence, Incidence, and Remission Rate for MetS Components
3.3. Risk of Having ≥1 MetS Component
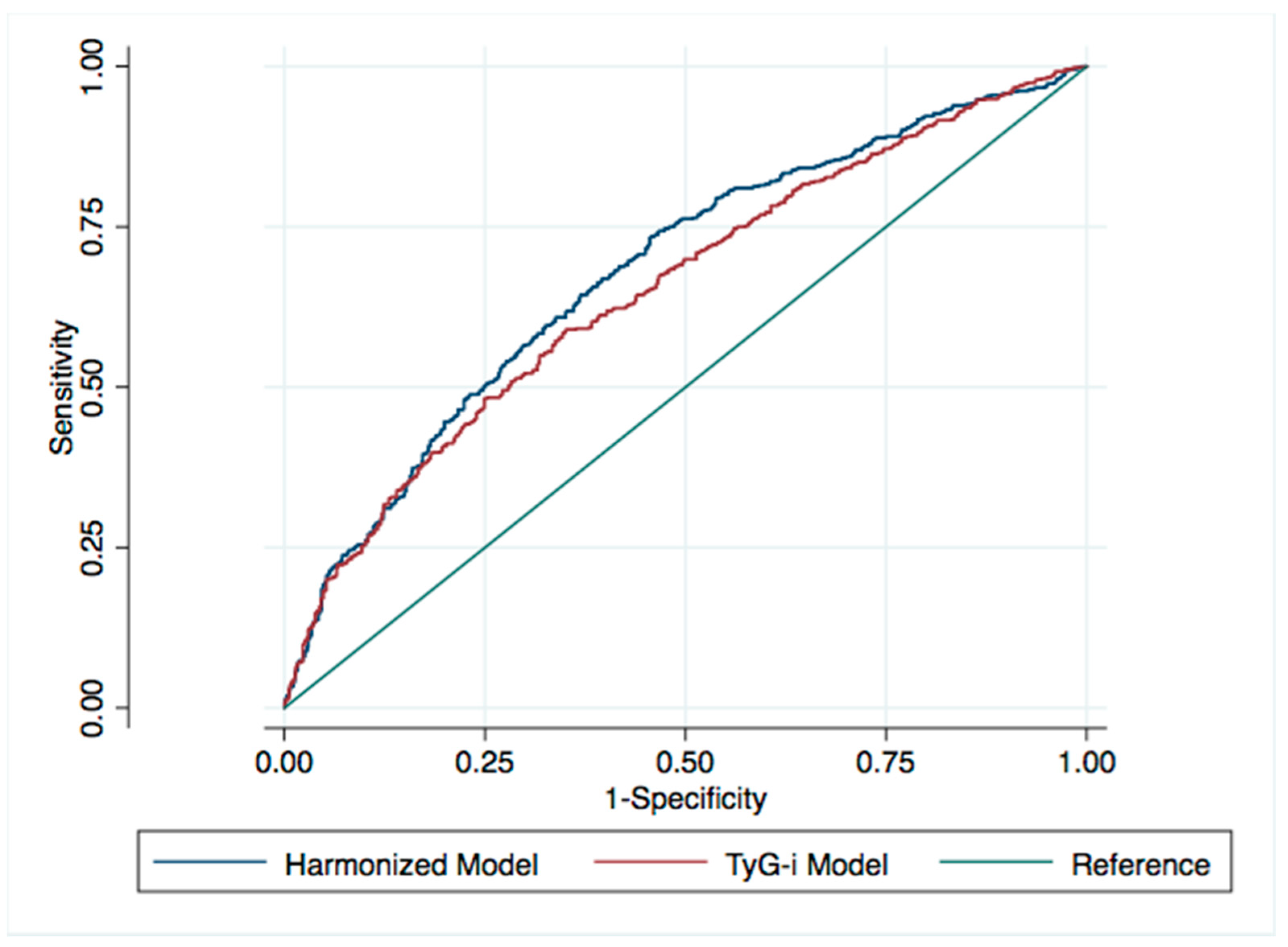
3.4. ROC Curves for the Risk of Having ≥1 MetS Component
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
Appendix A
| aOR | 95%CI | aOR | 95%CI | aOR | 95%CI | ||
|---|---|---|---|---|---|---|---|
| Sex Stratification | |||||||
| ≥1 MetS | Elevated TG | Elevated BP | |||||
| Female | Harmonized | 2.78 | (1.96–3.95) z | 3.33 | (1.60–6.94) y | 3.8 | (1.93–7.49) z |
| TyG-I | 2.06 | (1.40–3.05) z | 9.97 | (4.36–22.80) z | 1.21 | (0.59–2.48) | |
| Male | Harmonized | 2.29 | (1.47–3.57) z | 2.95 | (1.72–5.05) z | 1.56 | (0.95–2.58) |
| TyG-I | 2.24 | (1.42–3.53) z | 4.53 | (2.58–7.94) z | 1.62 | (0.96–2.73) | |
| Elevated WC | Reduced HDL | Elevated FPG | |||||
| Female | Harmonized | 1.75 | (1.01–3.04) x | 2.53 | (1.75–3.65) z | 2.93 | (1.00–8.55) x |
| TyG-I | 1.38 | (0.75–2.53) | 2.88 | (1.89–4.40) z | 2.24 | (0.75–6.70) | |
| Male | Harmonized | 1.37 | (0.63–2.96) | 2.41 | (1.28–4.56) y | 1.86 | (0.51–6.80) |
| TyG-I | 2.03 | (0.91–4.53) | 2.31 | (1.18–4.54) x | 1.64 | (0.44–6.12) | |
| Age Stratification | |||||||
| ≥1 MetS | Elevated TG | Elevated BP | |||||
| 15–25 | Harmonized | 2.77 | (1.72–4.46) z | 4.92 | (1.88–12.92) y | 2 | (0.95–4.18) |
| TyG-I | 1.87 | (1.04–3.38) x | 6.14 | (2.31–16.33) z | 2.81 | (1.25–6.30) x | |
| >25–35 | Harmonized | 2.5 | (1.50–4.16) z | 4.24 | (1.95–9.22) z | 1.3 | (0.54–3.12) |
| TyG-I | 2.97 | (1.75–5.03) z | 6.28 | (2.81–14.03) z | 2.16 | (0.91–5.13) | |
| >35–45 | Harmonized | 2.73 | (1.74–4.27) z | 2.05 | (1.02–4.12) x | 2.69 | (1.48–4.91) y |
| TyG-I | 1.71 | (1.09–2.69) x | 5.39 | (2.54–11.43) z | 0.86 | (0.46–1.63) | |
| Elevated WC | Reduced HDL | Elevated FPG | |||||
| 15–25 | Harmonized | 1.65 | (0.78–3.48) | 2.53 | (1.44–4.47) y | - | - |
| TyG-I | 1.73 | (0.72–4.16) | 2.29 | (1.08–4.83) x | - | - | |
| >25–35 | Harmonized | 1.68 | (0.65–4.35) | 2.77 | (1.57–4.89) z | 1.68 | (0.38–7.45) |
| TyG-I | 1.34 | (0.51–3.50) | 3.28 | (1.80–5.96) z | 1.33 | (0.33–5.37) | |
| >35–45 | Harmonized | 1.58 | (0.76–3.26) | 2.87 | (1.65–4.97) z | 3.88 | (1.16–13.03) x |
| TyG-I | 1.72 | (0.80–3.66) | 2.64 | (1.47–4.74) y | 3.17 | (0.89–11.31) | |
| Outcome | ||||||
|---|---|---|---|---|---|---|
| ≥1 MetS | Elevated TG | Elevated BP | Elevated WC | Reduced HDL | Elevated FPG | |
| MetS comp. | cOR 95%CI | cOR 95%CI | cOR 95%CI | cOR 95%CI | cOR 95%CI | cOR 95%CI |
| 1 Comp. | 2.69 | 2.56 | 1.89 | 1.59 | 2.51 | 1.07 |
| (2.04–3.55) z | (1.68–3.89) z | (1.27–2.81) y | (1.01–2.50) x | (1.84–3.43) z | (0.38–3.00) | |
| 2 Comp. | 3.77 | 5.29 | 4.1 | 3 | 3.48 | 8.95 |
| (2.25–6.34) z | (2.92–9.59) z | (2.32–7.27) z | (1.55–5.79) y | (2.07–5.85) z | (3.72–21.53) z | |
| aOR 95%CI | aOR 95%CI | aOR 95%CI | aOR 95%CI | aOR 95%CI | aOR 95%CI | |
| 1 Comp. | 2.56 | 2.69 | 1.78 | 1.41 | 2.28 | 0.97 |
| (1.92–3.42) z | (1.69–4.28) z | (1.16–2.72) y | (0.87–2.27) | (1.63–3.19) z | (0.33–2.87) | |
| 2 Comp. | 3.01 | 4.28 | 2.89 | 2.2 | 3.93 | 7.73 |
| (1.77–5.14) z | (2.17–8.45) z | (1.54–5.42) z | (1.08–4.46) x | (2.23–6.92) z | (2.96–20.19) z | |
References
- Folsom, A.R.; Shah, A.M.; Lutsey, P.L.; Roetker, N.S.; Alonso, A.; Avery, C.L.; Miedema, M.D.; Konety, S.; Chang, P.P.; Solomon, S.D. American Heart Association’s Life’s Simple 7: Avoiding Heart Failure and Preserving Cardiac Structure and Function. Am. J. Med. 2015, 128, 970–976. [Google Scholar] [CrossRef] [PubMed]
- Ng, M.; Fleming, T.; Robinson, M.; Thomson, B.; Graetz, N.; Margono, C.; Mullany, E.C.; Biryukov, S.; Abbafati, C.; Abera, S.F.; et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980–2013: A systematic analysis for the Global Burden of Disease Study 2013. Lancet 2014, 384, 766–781. [Google Scholar] [CrossRef]
- Poyrazoglu, S.; Bas, F.; Darendeliler, F. Metabolic syndrome in young people. Curr. Opin. Endocrinol. Diabetes Obes. 2014, 21, 56–63. [Google Scholar] [CrossRef]
- Alberti, K.G.M.M.; Eckel, R.H.; Grundy, S.M.; Zimmet, P.Z.; Cleeman, J.I.; Donato, K.A.; Fruchart, J.C.; James, W.P.T.; Loria, C.M.; Smith, S.C. Harmonizing the metabolic syndrome: A joint interim statement of the international diabetes federation task force on epidemiology and prevention; National heart, lung, and blood institute; American heart association; World heart federation; International. Circulation 2009, 120, 1640–1645. [Google Scholar] [CrossRef] [PubMed]
- Wildman, R.P. The Obese Without Cardiometabolic Risk Factor Clustering and the Normal Weight With Cardiometabolic Risk Factor Clustering. Arch. Intern. Med. 2008, 168, 1617. [Google Scholar] [CrossRef]
- Kuwabara, M.; Kuwabara, R.; Hisatome, I.; Niwa, K.; Roncal-Jimenez, C.A.; Bjornstad, P.; Andres-Hernando, A.; Sato, Y.; Jensen, T.; Garcia, G.; et al. “Metabolically Healthy” Obesity and Hyperuricemia Increase Risk for Hypertension and Diabetes: 5-year Japanese Cohort Study. Obesity 2017, 25, 1997–2008. [Google Scholar] [CrossRef]
- Zheng, R.; Zhou, D.; Zhu, Y. The long-term prognosis of cardiovascular disease and all-cause mortality for metabolically healthy obesity: A systematic review and meta-analysis. J. Epidemiol. Community Health 2016, 70, 1024–1031. [Google Scholar] [CrossRef] [PubMed]
- Hashimoto, Y.; Hamaguchi, M.; Tanaka, M.; Obora, A.; Kojima, T.; Fukui, M. Metabolically healthy obesity without fatty liver and risk of incident type 2 diabetes: A meta-analysis of prospective cohort studies. Obes. Res. Clin. Pract. 2018, 12, 4–15. [Google Scholar] [CrossRef]
- Mongraw-Chaffin, M.; Foster, M.C.; Anderson, C.A.M.; Burke, G.L.; Haq, N.; Kalyani, R.R.; Ouyang, P.; Sibley, C.T.; Tracy, R.; Woodward, M.; et al. Metabolically Healthy Obesity, Transition to Metabolic Syndrome, and Cardiovascular Risk. J. Am. Coll. Cardiol. 2018, 71, 1857–1865. [Google Scholar] [CrossRef]
- Soriguer, F.; Gutiérrez-Repiso, C.; Rubio-Martín, E.; García-Fuentes, E.; Almaraz, M.C.; Colomo, N.; De Antonio, I.E.; De Adana, M.S.R.; Chaves, F.J.; Morcillo, S.; et al. Metabolically healthy but obese, a matter of time? Findings from the prospective pizarra study. J. Clin. Endocrinol. Metab. 2013, 98, 2318–2325. [Google Scholar] [CrossRef]
- Lee, S.H.; Han, K.; Yang, H.K.; Kim, H.S.; Cho, J.H.; Kwon, H.S.; Park, Y.M.; Cha, B.Y.; Yoon, K.H. A novel criterion for identifying metabolically obese but normal weight individuals using the product of triglycerides and glucose. Nutr. Diabetes 2015, 5, e149. [Google Scholar] [CrossRef]
- Guerrero-Romero, F.; Villalobos-Molina, R.; Jiménez-Flores, J.R.; Simental-Mendia, L.E.; Méndez-Cruz, R.; Murguía-Romero, M.; Rodríguez-Morán, M. Fasting Triglycerides and Glucose Index as a Diagnostic Test for Insulin Resistance in Young Adults. Arch. Med. Res. 2016, 47, 382–387. [Google Scholar] [CrossRef]
- Khan, S.H.; Sobia, F.; Niazi, N.K.; Manzoor, S.M.; Fazal, N.; Ahmad, F. Metabolic clustering of risk factors: Evaluation of Triglyceride-glucose index (TyG index) for evaluation of insulin resistance. Diabetol. Metab. Syndr. 2018, 10, 1–8. [Google Scholar] [CrossRef]
- Yu, X.; Wang, L.; Zhang, W.; Ming, J.; Jia, A.; Xu, S.; Li, Q.; Ji, Q. Fasting triglycerides and glucose index is more suitable for the identification of metabolically unhealthy individuals in the Chinese adult population: A nationwide study. J. Diabetes Investig. 2018, 10–12. [Google Scholar] [CrossRef]
- Moon, S.; Park, J.S.; Ahn, Y. The Cut-off Values of Triglycerides and Glucose Index for Metabolic Syndrome in American and Korean Adolescents. J. Korean Med. Sci. 2017, 32, 427–433. [Google Scholar] [CrossRef]
- Zheng, R.; Mao, Y. Triglyceride and glucose (TyG) index as a predictor of incident hypertension: A 9-year longitudinal population-based study. Lipids Health Dis. 2017, 16, 1–7. [Google Scholar] [CrossRef]
- Martinez, J.A.; Navarro-González, D.; Fernández-Montero, A.; Sánchez-Íñigo, L.; Pastrana-Delgado, J. Triglyceride-glucose index (TyG index) in comparison with fasting plasma glucose improved diabetes prediction in patients with normal fasting glucose: The Vascular-Metabolic CUN cohort. Prev. Med. (Baltim.) 2016, 86, 99–105. [Google Scholar]
- Low, S.; Khoo, K.C.J.; Irwan, B.; Sum, C.F.; Subramaniam, T.; Lim, S.C.; Wong, T.K.M. The role of triglyceride glucose index in development of Type 2 diabetes mellitus. Diabetes Res. Clin. Pract. 2018, 143, 43–49. [Google Scholar] [CrossRef]
- Sánchez-Íñigo, L.; Navarro-González, D.; Fernández-Montero, A.; Pastrana-Delgado, J.; Martínez, J.A. The TyG index may predict the development of cardiovascular events. Eur. J. Clin. Investig. 2016, 46, 189–197. [Google Scholar] [CrossRef]
- Ho, J.S.; Cannaday, J.J.; Barlow, C.E.; Mitchell, T.L.; Cooper, K.H.; FitzGerald, S.J. Relation of the Number of Metabolic Syndrome Risk Factors With All-Cause and Cardiovascular Mortality. Am. J. Cardiol. 2008, 102, 689–692. [Google Scholar] [CrossRef]
- Sperling, L.S.; Mechanick, J.I.; Neeland, I.J.; Herrick, C.J.; Després, J.P.; Ndumele, C.E.; Vijayaraghavan, K.; Handelsman, Y.; Puckrein, G.A.; Araneta, M.R.G.; et al. The CardioMetabolic Health Alliance Working Toward a New Care Model for the Metabolic Syndrome. J. Am. Coll. Cardiol. 2015, 66, 1050–1067. [Google Scholar] [CrossRef]
- Hadjiyannakis, S. The metabolic syndrome in children and adolescents. Paediatr. Child Health (Oxf.) 2005, 10, 41–47. [Google Scholar] [CrossRef]
- Nolan, P.B.; Carrick-Ranson, G.; Stinear, J.W.; Reading, S.A.; Dalleck, L.C. Prevalence of metabolic syndrome and metabolic syndrome components in young adults: A pooled analysis. Prev. Med. Rep. 2017, 7, 211–215. [Google Scholar] [CrossRef]
- Piepoli, M.F.; Hoes, A.W.; Agewall, S.; Albus, C.; Brotons, C.; Catapano, A.L.; Cooney, M.T.; Corrà, U.; Cosyns, B.; Deaton, C.; et al. 2016 European Guidelines on cardiovascular disease prevention in clinical practice. Eur. Heart J. 2016, 37, 2315–2381. [Google Scholar] [CrossRef]
- Tran, D.M.T.; Zimmerman, L.M. Cardiovascular Risk Factors in Young Adults: A Literature Review. J. Cardiovasc. Nurs. 2015, 30, 298–310. [Google Scholar] [CrossRef]
- Barba, C.; Cavalli-Sforza, T.; Cutter, J.; Darnton-Hill, I.; Deurenberg, P.; Deurenberg-Yap, M.; Gill, T.; James, P.; Ko, G.; Nishida, C. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet 2004, 363, 157–163. [Google Scholar]
- Hwang, L.C.; Bai, C.H.; Chen, C.J. Prevalence of obesity and metabolic syndrome in Taiwan. J. Formos. Med. Assoc. 2006, 105, 626–635. [Google Scholar] [CrossRef]
- Simental-Mendía, L.E.; Rodríguez-Morán, M.; Guerrero-Romero, F. The Product of Fasting Glucose and Triglycerides As Surrogate for Identifying Insulin Resistance in Apparently Healthy Subjects. Metab. Syndr. Relat. Disord. 2008, 6, 299–304. [Google Scholar] [CrossRef]
- Wu, Y.C.; Lee, W.C. Alternative performance measures for prediction models. PLoS ONE 2014, 9, e91249. [Google Scholar] [CrossRef]
- Jiang, Y.D.; Chang, C.H.; Tai, T.Y.; Chen, J.F.; Chuang, L.M. Incidence and prevalence rates of diabetes mellitus in Taiwan: Analysis of the 2000-2009 Nationwide Health Insurance database. J. Formos. Med. Assoc. 2012, 111, 599–604. [Google Scholar] [CrossRef]
- Einhorn, D.; Reaven, G.M.; Cobin, R.H.; Ford, E.; Ganda, O.P.; Handelsman, Y.; Hellman, R.; Jellinger, P.S.; Kendall, D.; Krauss, R.M.; et al. American College of Endocrinology position statement on the insulin resistance syndrome. Endocr. Pract. 2003, 9, 237–252. [Google Scholar]
- Sun, H.L.; Pei, D.; Lue, K.H.; Chen, Y.L. Uric acid levels can predict metabolic syndrome and hypertension in adolescents: A 10-year longitudinal study. PLoS ONE 2015, 10, 1–10. [Google Scholar] [CrossRef]
- Lee, S.H.; Yang, H.K.; Ha, H.S.; Lee, J.H.; Kwon, H.S.; Park, Y.M.; Yim, H.W.; Kang, M.I.; Lee, W.C.; Son, H.Y.; et al. Changes in metabolic health status over time and risk of developing type 2 diabetes a prospective cohort study. Medicine (USA) 2015, 94, 1–8. [Google Scholar]
- Hosseinpanah, F.; Nazeri, P.; Ghareh, S.; Tohidi, M.; Azizi, F. Predictors of the incident metabolic syndrome in healthy obese subjects: A decade of follow-up from the Tehran Lipid and Glucose Study. Eur. J. Clin. Nutr. 2014, 68, 295–299. [Google Scholar] [CrossRef][Green Version]
- Lin, C.C.; Liu, C.S.; Lai, M.M.; Li, C.I.; Chen, C.C.; Chang, P.C.; Lin, W.Y.; Lee, Y.D.; Lin, T.; Li, T.C. Metabolic syndrome in a Taiwanese metropolitan adult population. BMC Public Health 2007, 7, 1–5. [Google Scholar] [CrossRef]
- Ärnlöv, J.; Ingelsson, E.; Sundström, J.; Lind, L. Impact of body mass index and the metabolic syndrome on the risk of cardiovascular disease and death in middle-aged men. Circulation 2010, 121, 230–236. [Google Scholar] [CrossRef]
- Tsai, S.P.; Wen, C.P.; Chan, H.T.; Chiang, P.H.; Tsai, M.K.; Cheng, T.Y.D. The effects of pre-disease risk factors within metabolic syndrome on all-cause and cardiovascular disease mortality. Diabetes Res. Clin. Pract. 2008, 82, 148–156. [Google Scholar] [CrossRef]
- Tie, H.T.; Shi, R.; Li, Z.H.; Zhang, M.; Zhang, C.; Wu, Q.C. Risk of major adverse cardiovascular events in patients with metabolic syndrome after revascularization: A meta-analysis of eighteen cohorts with 18457 patients. Metabolism 2015, 64, 1224–1234. [Google Scholar] [CrossRef]
- Fan, Y.C.; Chou, C.C.; You, S.L.; Sun, C.A.; Chen, C.J.; Bai, C.H. Impact of Worsened Metabolic Syndrome on the Risk of Dementia: A Nationwide Cohort Study. J. Am. Heart Assoc. 2017, 6, e004749. [Google Scholar] [CrossRef]
- Den Engelsen, C.; Gorter, K.J.; Salomé, P.L.; Van Den Donk, M.; Rutten, G.E. Remission of screen-detected metabolic syndrome and its determinants: An observational study. BMC Public Health 2012, 12, 778. [Google Scholar] [CrossRef]
- Najam, O.; Ray, K.K. Where to now in cardiovascular disease prevention. Atherosclerosis 2016, 251, 483–489. [Google Scholar] [CrossRef]
- Lemieux, I. Metabolic Syndrome Diagnosis: The Sooner the Better. Metab. Syndr. Relat. Disord. 2018, 16, 205–207. [Google Scholar] [CrossRef]
- Yeh, C.J.; Chang, H.Y.; Pan, W.H. Time trend of obesity, the metabolic syndrome and related dietary pattern in Taiwan: From NAHSIT 1993–1996 to NAHSIT 2005–2008. Asia Pac. J. Clin. Nutr. 2011, 20, 292–300. [Google Scholar]
- Bradshaw, P.T.; Reynolds, K.R.; Wagenknecht, L.E.; Ndumele, C.E.; Stevens, J. Incidence of components of metabolic syndrome in the metabolically healthy obese over 9 years follow-up: The Atherosclerosis Risk in Communities study. Int. J. Obes. 2018, 42, 295–301. [Google Scholar] [CrossRef]
- Pan, W.H.; Chang, H.Y.; Yeh, W.Y.; Hsiao, S.Y.; Hung, Y.T. Prevalence, awareness, treatment and control of hypertension in Taiwan: Results of Nutrition and Health Survey in Taiwan (NAHSIT) 1993–1996. J. Hum. Hypertens. 2001, 15, 793–798. [Google Scholar] [CrossRef]
| Variables | Harmonized Criteria | TyG-Index | Total (n = 1182) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Healthy (n = 835) (0 MetS Component) | Unhealthy (n = 347) (1–2 MetS Component) | p-Value | Healthy (n = 887) (TyG-i ≤ 8.41) | Unhealthy (n = 295) (TyG-i > 8.41) | p-Value | |||||||
| % | % | % | % | % | ||||||||
| Baseline | ||||||||||||
| Male | 39.8 | 39.2 | 0.85 | 37.2 | 46.8 | 0.004 | 39.6 | |||||
| Smoking (yes) | 15.9 | 19.0 | 0.19 | 15.2 | 21.7 | 0.01 | 16.8 | |||||
| Alcohol (no) | 81.9 | 77.2 | 0.14 | 81.6 | 77.3 | 0.102 | 80.5 | |||||
| Vegetable & Fruit (daily) | 86.2 | 82.4 | 0.09 | 84.8 | 86.1 | 0.581 | 85.1 | |||||
| Fatty food (low) | 56.9 | 56.9 | 1.00 | 54.7 | 51.5 | 0.347 | 53.9 | |||||
| Exercise (routine) | 78.5 | 79.5 | 0.71 | 78.7 | 79.3 | 0.819 | 78.9 | |||||
| PDH (yes) | 44.1 | 53.6 | 0.003 | 44.4 | 54.2 | 0.003 | 53.1 | |||||
| SDH (yes) | 9.0 | 12.4 | 0.075 | 8.5 | 14.6 | 0.002 | 10.0 | |||||
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | |||
| Age | 30.1 | 8.4 | 30.8 | 8.8 | 0.19 | 29.5 | 8.5 | 32.8 | 8.0 | <0.001 | 30.3 | 8.5 |
| BMI | 20.7 | 1.2 | 21.0 | 1.2 | <0.001 | 20.6 | 1.2 | 21.2 | 1.2 | <0.001 | 20.8 | 1.2 |
| TG a | 76.0 | 34.0 | 95.0 | 32.0 | <0.001 | 71.0 | 27.0 | 130.0 | 42.0 | <0.001 | 90.0 | 46.1 |
| SBP | 103.9 | 9.7 | 107.6 | 13.7 | <0.001 | 104.0 | 10.9 | 108.0 | 11.4 | <0.001 | 104.9 | 11.1 |
| DBP | 67.9 | 7.7 | 72.1 | 10.2 | <0.001 | 68.4 | 8.5 | 71.5 | 8.7 | <0.001 | 69.1 | 8.7 |
| WC | 71.1 | 6.1 | 73.7 | 7.5 | <0.001 | 71.0 | 6.3 | 74.4 | 7.1 | <0.001 | 71.8 | 6.6 |
| HDL | 60.4 | 11.0 | 47.6 | 12.1 | <0.001 | 57.5 | 12.2 | 54.2 | 14.2 | <0.001 | 56.6 | 12.7 |
| FPG | 84.1 | 6.6 | 88.2 | 10.8 | <0.001 | 84.4 | 7.6 | 88.2 | 9.4 | <0.001 | 85.3 | 8.2 |
| Follow-up | ||||||||||||
| BMI | 21.8 | 2.4 | 22.3 | 2.4 | 0.001 | 21.7 | 2.4 | 22.5 | 2.4 | <0.001 | 21.9 | 2.4 |
| TG a | 77.0 | 42.0 | 90.0 | 70.0 | <0.001 | 72.0 | 37.0 | 110.0 | 69.0 | <0.001 | 94.2 | 55.2 |
| SBP | 109.9 | 11.5 | 113.6 | 15.0 | <0.001 | 110.0 | 12.2 | 114.0 | 13.6 | <0.001 | 110.8 | 12.7 |
| DBP | 70.4 | 8.5 | 73.7 | 11.1 | <0.001 | 70.5 | 9.0 | 73.9 | 10.2 | <0.001 | 71.2 | 9.4 |
| WC | 74.6 | 7.3 | 76.3 | 7.9 | <0.001 | 74.3 | 7.2 | 77.5 | 7.9 | <0.001 | 75.1 | 7.5 |
| HDL | 55.8 | 10.7 | 50.3 | 9.5 | <0.001 | 55.3 | 10.8 | 51.0 | 9.9 | <0.001 | 54.3 | 10.8 |
| FPG | 82.4 | 7.5 | 85.2 | 10.1 | <0.001 | 82.2 | 7.4 | 86.3 | 10.4 | <0.001 | 83.1 | 8.4 |
| Outcome | |||||||
|---|---|---|---|---|---|---|---|
| ≥1 MetS | Elevated TG | Elevated BP | Elevated WC | Reduced HDL | Elevated FPG | ||
| Baseline | n/N | 347/1182 | 87/1182 | 55/1182 | 21/1182 | 211/1182 | 41/1182 |
| % | 29.4 | 7.4 | 4.7 | 1.8 | 17.9 | 3.5 | |
| Follow-up | n/N | 475/1182 | 120/1182 | 142/1182 | 105/1182 | 250/1182 | 28/1182 |
| % | 40.2 | 10.2 | 12.0 | 8.9 | 21.2 | 2.4 | |
| Incidence | per 1000 | 327 | 76 | 103 | 82 | 166 | 18 |
| Remission | per 1000 | 418 | 575 | 527 | 524 | 578 | 829 |
| Outcome | ||||||
|---|---|---|---|---|---|---|
| ≥1 MetS | Elevated TG | Elevated BP | Elevated WC | Reduced HDL | Elevated FPG | |
| cOR (95%CI) | cOR (95%CI) | cOR (95%CI) | cOR (95%CI) | cOR (95%CI) | cOR (95%CI) | |
| Unhealthy-Har | 2.87 | 3.03 | 2.27 | 1.84 | 2.68 | 2.47 |
| (2.22–3.71) z | (2.06–4.44) z | (1.59–3.24) z | (1.22–2.78) y | (2.01–3.59) z | (1.16–5.23) x | |
| Unhealthy-TyG | 2.32 | 7.88 | 2.11 | 1.98 | 1.73 | 3.11 |
| (1.77–3.03) z | (5.24–11.85) z | (1.46–3.04) z | (1.31–3.01) y | (1.28–2.34) z | (1.46–6.60) y | |
| aOR (95%CI) | aOR (95%CI) | aOR (95%CI) | aOR (95%CI) | aOR (95%CI) | aOR (95%CI) | |
| Unhealthy-Har | 2.64 | 3.01 | 1.99 | 1.56 | 2.53 | 2.21 |
| (2.02-3.45) z | (1.96-4.61) z | (1.35-2.94) z | (1.01-2.42) x | (1.85-3.46) z | (0.99-4.91) | |
| Unhealthy-TyG | 2.11 | 5.64 | 1.45 | 1.59 | 2.63 | 1.93 |
| (1.57-2.82) z | (3.58-8.87) z | (0.96-2.19) | (0.99-2.56) | (1.85-3.74) z | (0.83-4.48) | |
| Model | AU-ROC | Lower 95%CI | Upper 95%CI |
|---|---|---|---|
| Harmonized | 0.679 | 0.647 | 0.710 |
| TyG-Index y | 0.652 | 0.619 | 0.684 |
| Elevated FPG y,z | 0.631 | 0.598 | 0.663 |
| Elevated BP y | 0.659 | 0.627 | 0.690 |
| Elevated TG y | 0.651 | 0.619 | 0.683 |
| Elevated WC y,z | 0.631 | 0.599 | 0.663 |
| Low HDL y | 0.639 | 0.607 | 0.672 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bintoro, B.S.; Fan, Y.-C.; Chou, C.-C.; Chien, K.-L.; Bai, C.-H. Metabolic Unhealthiness Increases the Likelihood of Having Metabolic Syndrome Components in Normoweight Young Adults. Int. J. Environ. Res. Public Health 2019, 16, 3258. https://doi.org/10.3390/ijerph16183258
Bintoro BS, Fan Y-C, Chou C-C, Chien K-L, Bai C-H. Metabolic Unhealthiness Increases the Likelihood of Having Metabolic Syndrome Components in Normoweight Young Adults. International Journal of Environmental Research and Public Health. 2019; 16(18):3258. https://doi.org/10.3390/ijerph16183258
Chicago/Turabian StyleBintoro, Bagas Suryo, Yen-Chun Fan, Chia-Chi Chou, Kuo-Liong Chien, and Chyi-Huey Bai. 2019. "Metabolic Unhealthiness Increases the Likelihood of Having Metabolic Syndrome Components in Normoweight Young Adults" International Journal of Environmental Research and Public Health 16, no. 18: 3258. https://doi.org/10.3390/ijerph16183258
APA StyleBintoro, B. S., Fan, Y.-C., Chou, C.-C., Chien, K.-L., & Bai, C.-H. (2019). Metabolic Unhealthiness Increases the Likelihood of Having Metabolic Syndrome Components in Normoweight Young Adults. International Journal of Environmental Research and Public Health, 16(18), 3258. https://doi.org/10.3390/ijerph16183258





