Disability-Disaggregated Data Collection: Hospital-Based Application of the Washington Group Questions in an Eye Hospital in Paraguay
Abstract
:1. Introduction
2. Materials and Methods
- The WG Short Set (WG-SS) consists of a set of six single short questions on functional domains (which are seeing, hearing, walking or climbing stairs, remembering or concentrating, self-care, and communication). The questions were designed for applications in populations aged five years and older and will identify the large majority of people with disabilities. The answer options are “no difficulty”, “yes, some difficulty”, “yes, a lot of difficulty”, and “cannot do at all” (response pattern 1 according to the WG guidelines) [36].
- The WG Extended Set on Functioning (WG-ES 3) consists of the same questions as the WG-SS and adds four additional questions related to two domains of “affect” (anxiety and depression) for participants aged 13 years and older. The answer options regarding the frequency of feeling anxious or depressed are “daily”, “weekly”, monthly”, “a few times a year”, and “never”. The severity can be answered with “a little”, “a lot” and “somewhere between a little and a lot” (response patterns 5 and 6 according to WG guidelines) [36]. We excluded the “upper body” questions of the WG-ES 3 in order to improve the feasibility of the data collection [36].
2.1. Data Analysis WG-SS
2.2. Data Analysis WG-ES 3
3. Results
3.1. Short Set WG-SS
3.2. Extended Set WG-ES 3
3.2.1. Affect/Anxiety Domain
3.2.2. Affect/Depression Domain:
4. Discussion
4.1. WG-SS Results
4.1.1. Vision Domain
4.1.2. Communicating Domain
4.1.3. Remembering/Concentrating Domain
4.1.4. Self-Care Domain
4.1.5. Mobility Domain
4.1.6. Hearing Domain
4.2. WG-ES3 Results
4.3. The WG Questions in a Hospital Setting
4.4. Strengths
4.5. Limitations
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- World Health Organization. Universal Eye Health: A Global Action Plan 2014–2019; World Health Organization: Geneva, Switzerland, 2013. [Google Scholar]
- World Health Organization Regional Office for the Western Pacific. Sustainable Development Goals and Universal Health Coverage Regional Monitoring Framework: Applications, Analysis and Technical Information; World Health Organization Regional Office for the Western Pacific: Manila, Philippines, 2017. [Google Scholar]
- Kavanagh, J.; Oliver, S.; Lorenc, T. Reflections on developing and using PROGRESS-Plus. Equity Update 2008, 2, 3. [Google Scholar]
- Ramke, J.; Zwi, A.B.; Lee, A.C.; Blignault, I.; Gilbert, C.E. Inequality in cataract blindness and services: Moving beyond unidimensional analyses of social position. Br. J. Ophthalmol. 2017, 101, 395–400. [Google Scholar] [CrossRef] [PubMed]
- Matheson, A.; Bourke, C.; Verhoeven, A.; Khan, M.I.; Nkunda, D.; Dahar, Z.; Ellison-Loschmann, L. Lowering hospital walls to achieve health equity. BMJ 2018, 362, 4. [Google Scholar] [CrossRef] [PubMed]
- Shakespare, T.; Bright, T.; Kuper, H. Access to Health for Persons with Disabilities. 2018. Available online: https://webcache.googleusercontent.com/search?q=cache:8ALPbIFZUkMJ:https://www.ohchr.org/Documents/Issues/Disability/StandardHealth/BackgroundDoc_EGM_Righttohealth.docx+&cd=4&hl=en&ct=clnk (accessed on 24 August 2019).
- Kuper, H.; Hanefeld, J. Debate: Can we achieve universal health coverage without a focus on disability? BMC Health Serv. Res. 2018, 18, 738. [Google Scholar] [CrossRef] [PubMed]
- McPherson, A.; Durham, J.; Richards, N.; Gouda, H.; Rampatige, R.; Whittaker, M. Strengthening health information systems for disability-related rehabilitation in LMICs. Health Policy Plan. 2017, 32, 384–394. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. World Report on Disability 2011; World Health Organization: Geneva, Switzerland, 2011. [Google Scholar]
- Bourne, R.R.A.; Flaxman, S.R.; Braithwaite, T.; Cicinelli, M.V.; Das, A.; Jonas, J.B.; Keeffe, J.; Kempen, J.H.; Leasher, J.; Limburg, H.; et al. Magnitude, temporal trends, and projections of the global prevalence of blindness and distance and near vision impairment: A systematic review and meta-analysis. Lancet Glob. Heal. 2017, 5, e888–e897. [Google Scholar] [CrossRef]
- Mactaggart, I.; Polack, S.; Murthy, G.; Kuper, H. A population-based survey of visual impairment and its correlates in Mahabubnagar district, Telangana State, India. Ophthalmic Epidemiol. 2017, 6586, 8. [Google Scholar] [CrossRef] [PubMed]
- Choi, H.G.; Lee, M.J.; Lee, S.M. Visual impairment and risk of depression: A longitudinal follow-up study using a national sample cohort. Sci. Rep. 2018, 8, 8. [Google Scholar] [CrossRef] [PubMed]
- Douglas, G.; Pavey, S.; Corcoran, C.; Eperjesi, F. Individual’s recollections of their experiences in eye clinics and understanding of their eye condition: Results from a survey of visually impaired people in Britain. Ophthalmic Physiol. Opt. 2010, 30, 748–757. [Google Scholar] [CrossRef]
- Li, J.C.; Wong, K.; Park, A.S.; Fricke, T.R.; Jackson, A.J. The challenges of providing eye care for adults with intellectual disabilities. Clin. Exp. Optom. 2015, 98, 420–429. [Google Scholar] [CrossRef]
- Iezzoni, L.I. Dangers of Diagnostic Overshadowing. N. Engl. J. Med. 2019, 380, 2092–2093. [Google Scholar] [CrossRef] [PubMed]
- Lagu, T.; Iezzoni, L.I.; Lindenauer, P.K. The Axes of Access—Improving Care for Patients with Disabilities. N. Engl. J. Med. 2019, 370, 1847–1851. [Google Scholar] [CrossRef] [PubMed]
- Sanchez, J.; Byfield, G.; Brown, T.T.; LaFavor, K.; Murphy, D.; Laud, P. Perceived Accessibility Versus Actual Physical Accessibility of Healthcare Facilities. Rehabil. Nurs. 2012, 25, 6–9. [Google Scholar] [CrossRef]
- Morris, M.A.; Lagu, T.; Maragh-Bass, A.; Liesinger, J.; Griffin, J.M. Development of Patient-Centered Disability Status Questions to Address Equity in Care. Jt. Comm. J. Qual. Patient Saf. 2017, 43, 642–650. [Google Scholar] [CrossRef] [PubMed]
- Watt, G. The inverse care law today. Lancet 2002, 360, 252–254. [Google Scholar] [CrossRef]
- Tudor Hart, J. The inverse care law. Lancet 1971, 297, 405–412. [Google Scholar] [CrossRef]
- Mörchen, M.; Ormsby, G.; Bonn, T.S.; Lewis, D. Addressing disability in the health system at CARITAS Takeo Eye Hospital. Community Eye Health 2013, 26, 8–9. [Google Scholar]
- Mörchen, M.; Bush, A.; Kiel, P.; Lewis, D.; Qureshi, B. Leaving no one behind: Strengthening access to eye health programmes for people with disabilities in 6 low- and middle income countries. Asia-Pac. J. Ophthalmol. 2018, 7, 331–338. [Google Scholar]
- Ramke, J.; Zwi, A.B.; Silva, J.C.; Mwangi, N.; Rono, H.; Gichangi, M.; Qureshi, M.B.; Gilbert, C.E. Evidence for national universal eye health plans. Bull. World Health Organ. 2018, 96, 695–704. [Google Scholar] [CrossRef]
- Loeb, M. Disability statistics: An integral but missing (and misunderstood) component of development work. Nord. J. Hum. Rights 2013, 31, 306–324. [Google Scholar]
- Mactaggart, I.; Kuper, H.; Murthy, G.V.S.; Oye, J.; Polack, S. Measuring disability in population based surveys: The interrelationship between clinical impairments and reported functional limitations in Cameroon and India. PLoS ONE 2016, 11, 18. [Google Scholar] [CrossRef] [PubMed]
- Washington Group on Disability Statistics. The Washington Group Short Set on Functioning; Statistics Division United Nations: New York, NY, USA, 2017. [Google Scholar]
- Quigley, N.; Bird, E.; Turner, K.; Cook, G.; Thivillier, P. Disability Data Collection: A Summary Review of the Use of the Washington Group Questions by Development and Humanitarian Actors; Leonhard Cheshire: London, UK, 2018. [Google Scholar]
- Mörchen, M.; Bonn, T.S.; Lewis, D. Towards Universal Eye Health: Hospital-based disability-disaggregated data collection in Takeo province, Cambodia. Disabil. Health J. 2018, 11, 660–664. [Google Scholar] [CrossRef] [PubMed]
- Mopari, R.; Garg, B.; Puliyel, J.; Varughese, S. Measuring disability in an urban slum community in India using the Washington Group questionnaire. Disabil. Health J. 2019, 12, 263–268. [Google Scholar] [CrossRef] [PubMed]
- Sightsavers. Everybody Counts—Disability Disaggregation of Data Pilot Projects in India and Tanzania—Final Evaluation Report; Sightsavers: Chippenham, UK, 2016. [Google Scholar]
- Mitra, S.; Sambamoorthi, U. Disability prevalence among adults: Estimates for 54 countries and progress toward a global estimate. Disabil. Rehabil. 2014, 36, 940–947. [Google Scholar] [CrossRef] [PubMed]
- ParlGual; Disability Council International. Report on the Situation of Human Rights of Persons with Disabilities in Paraguay; Committee on the Rights of Persons with Disabilities: Geneva, Switzerland, 2013. [Google Scholar]
- World Health Organization. World Health Survey Report Paraguy; World Health Organization: Geneva, Switzerland, 2003. [Google Scholar]
- Elizabeth, M.; Kuck, B.; Moreno, L.A. Anuario Estadístico del Paraguay; Dirección General de Estadística, Encuestas y Censos (DGEEC): Asunción, Paraguay, 2013. [Google Scholar]
- Washington Group on Disability Statistics. Translation of the Washington Group Tools; Statistics Division United Nations: New York, NY, USA, 2017. [Google Scholar]
- Washington Group on Disability Statistics. Analytic Guidelines: Creating Disability Identifiers Using the Washington Group Short Set (WG-SS) SPSS Syntax; Statistics Division United Nations: New York, NY, USA, 2019. [Google Scholar]
- Duerksen, R.; Limburg, H.; Lansingh, V.C.; Silva, J.C. Review of blindness and visual impairment in Paraguay: Changes between 1999 and 2011. Ophthalmic Epidemiol. 2013, 20, 301–307. [Google Scholar] [CrossRef] [PubMed]
- Puras, D. Country Visit to Paraguay, 23 September to 6 October 2015 by the UN Special Rapporteur on the Right of Everyone to the Enjoyment of the Highest Attainable Standard of Physical and Mental Health; Office of the United Nations High Commissioner for Human Rights (OHCHR): Geneva, Switzerland, 2015. [Google Scholar]
- Washington Group on Disability Statistics. Appendix 3: Cognitive Interview Testing Guide; Statistics Division United Nations: New York, NY, USA, 2006. [Google Scholar]
- Miller, K.; Mont, D.; Maitland, A.; Altman, B.; Madans, J. Results of a cross-national structured cognitive interviewing protocol to test measures of disability. Qual. Quant. 2011, 45, 801–815. [Google Scholar] [CrossRef]
- Sharby, N.; Martire, K.; Iversen, M.D. Decreasing health disparities for people with disabilities through improved communication strategies and awareness. Int. J. Environ. Res. Public Health 2015, 12, 3301–3316. [Google Scholar] [CrossRef]
- Crossley, M. Disability Cultural Competence in the Medical Profession. Saint Louis Univ. J. Heal. Law Policy 2015, 9, 89–109. [Google Scholar]
- Stanford, P.; Morgan, J.; Waterman, H.; Spencer, A.F.; Read, S.; Harper, R. Glaucoma, dementia, and the “precipice of care”: Transitions between states of medication adherence. Patient Prefer. Adherence 2018, 12, 1315–1325. [Google Scholar]
- Friedman, D.S.; Munoz, B.; Roche, K.B.; Massof, R.; Broman, A.; West, S.K. Poor uptake of cataract surgery in nursing home residents: The Salisbury Eye Evaluation in Nursing Home Groups study. Arch. Ophthalmol. 2005, 123, 1581–1587. [Google Scholar] [CrossRef]
- Lagu, T.; Hannon, N.S.; Rothberg, M.B.; Wells, A.S.; Green, L.; Windom, M.O.; Dempsey, K.R.; Pekow, P.S.; Avrunin, J.S.; Chen, A.; et al. Original Research Access to Subspecialty Care for Patients with Mobility Impairment. Ann. Intern. Med. 2013, 158, 442–447. [Google Scholar] [CrossRef] [PubMed]
- Capella-McDonnall, M.E. The effects of single and dual sensory loss on depression, subjective health and activity of daily living in the elderly. Int. J. Geriatr. Psychiatry 2005, 20, 855–861. [Google Scholar] [CrossRef] [PubMed]
- Brabyn, J.A.; Schneck, M.E.; Haegerstrom-Portnoy, G.; Lott, L.A. Dual sensory loss: Overview of problems, visual assessment, and rehabilitation. Trends Amplif. 2007, 11, 219–226. [Google Scholar] [CrossRef] [PubMed]
- Shah, S.R.; Newton, V.E.; Mulligan, D. Improving communication with patients with a hearing impairment. Community Eye Heal. J. 2013, 26, 6–7. [Google Scholar]
- Disability Rights Commission of England and Wales. Equal Treatment: Closing the Gap. A Formal Investigation into Physical Health Inequalities Experienced by People with Learning Disabilities and/or Mental Health Problems; Disability Rights Commission: Stratford upon Avon, UK, 2006. [Google Scholar]
- World Health Organization. Training Manual on Disability Statistics; World Health Organization: Geneva, Switzerland, 2008; ISBN 9789211205480. [Google Scholar]
| English | Paraguayan Spanish | Guarani | |
|---|---|---|---|
| 1 | Do you have difficulty seeing, even if wearing glasses? a. No, no difficulty b. Yes, some difficulty c. Yes, a lot of difficulty d. Cannot do it at all | ¿Ves con dificultad incluso usando lentes? a. No. Veo bien. b. Si. A veces tengo dificultad. c. Si. Tengo mucha dificultad. d. No veo nada. | ¿Rehecha asy piko reipururamo jepe lente? a. Nahaniri, ahecha porä b. Heë, sapy’a py’a c. Heë, aguereko hetá. d. Ndahechaiete voi |
| 2 | Do you have difficulty hearing, even if using a hearing aid? a. No, no difficulty b. Yes, some difficulty c. Yes, a lot of difficulty d. Cannot do it at all | ¿No escuchas bien, inclusive usando audífonos? a. No. Escucho bien. b. Si. A veces tengo dificultad. c. Si. Tengo mucha dificultad. d. No escucho para nada. | ¿Nerehendu poraipa reipururamo jepe audífono? a. Nahaniri, ahendua porä b. Heë, sapy’a py’a c. Heë, aguereko hetá. d. Nahenduiete voi |
| 3 | Do you have difficulty walking or climbing steps? a. No, no difficulty b. Yes, some difficulty c. Yes, a lot of difficulty d. Cannot do it at all | ¿Caminas con dificultad o subes escaleras con dificultad? a. No. Camino bien. b. Si. A veces tengo dificultad. c. Si. Tengo mucha dificultad. d. No puedo caminar. | ¿Reguatá asy pa o ejupi asy escalerape? a. Nahaniri, aguatá’ porä b. Heë, sapy’a py’a c. Heë, aguereko hetá. d. Ndaikatuiete aguata o ejupi escalerape |
| 4 | Do you have difficulty remembering or concentrating? a. No, no difficulty b. Yes, some difficulty c. Yes, a lot of difficulty d. Cannot do it at all | ¿Tiene dificultad para aprender o para recordar? a. No, mi inteligencia está bien. b. Si. A veces tengo dificultad. c. Si. Tengo mucha dificultad. d. No puedo aprender o recordar. | ¿Hasy iko ndeve Eaprende haguá, nemandu’a, haguá? a. Nahaniri, che Ivale. b. Heë, sapy’a py’a c. Heë, aguereko hetá. d. Ndaikatuietevoi o aprendé |
| 5 | Do you have difficulty (with self-care such as) washing all over or dressing? a. No, no difficulty b. Yes, some difficulty c. Yes, a lot of difficulty d. Cannot do it at all | ¿Es difícil para vos limpiarte y vestirte solo? a. No. You puedo solo. b. Si. A veces tengo dificultad. c. Si. Tengo mucha dificultad. d. No puedo hacer nada, necesito a alguien que me ayude. | ¿Hasy iko ndeve eñemopoti ha eñemonde haguá ne añó? a. Nahaniri, che ikatu che añó. b. Heë, sapy’a py’a c. Heë, aguereko hetá. d. Ndoikatuiete ajapo aikoteve che ayúda va’eräre |
| 6 | Using your usual (customary) language, do you have difficulty communicating, for example understanding or being understood? a. No, no difficulty b. Yes, some difficulty c. Yes, a lot of difficulty d. Cannot do it at all | ¿Es difícil para usted hablar o entender a los demás, en nuestro idioma castellano/guaraní? a. No. Capto y hablo bien. b. Si. A veces tengo dificultad. c. Si. Tengo mucha dificultad. d. Poco entiendo, no puedo hablar bien. | ¿Hasy iko ndeve eñemongeta haguá ha entende haguá oñeéva nedivepe, ha ña nde ñe’e tepe guaraní/castellano? a. Nahaniri. A pillá pora, añe’e porä b. Heë, sapy’a py’a c. Heë, aguereko hetá. d. Sa’i entende. Ndaikatuí añeë pova |
| English | Paraguayan Spanish | Guarani | |
|---|---|---|---|
| 7 | How often do you feel worried, nervous, or anxious? a. Never b. A few times a year c. Monthly d. Weekly e. Daily | ¿En qué momento te sentís muy preocupado, enojado o ansioso? a. Nunca b. De vez en cuando en el año c. De vez en cuando cada mes d. De vez en cuando cada semana e. A diario | Mba’eicha jave eñeñandú ejepy’apy, o nde pochy o nde py’a tarová? a. Mba’eicha vevo b. Sapy’a py’a Ary c. Sapy’a py’a Ary jasykuéra d. Sapy’a py’a Arapoköindy rehegua e. Tapiaite |
| 8 | Level of feelings when you last felt worried, nervous or anxious? a. A little b. Somewhere in between a little and a lot c. A lot | Cuando te sentías preocupado, enojado o ansioso. ¿Cómo te sentías? a. Muy poco preocupado, enojado o ansioso. b. Poco o mucho c. Muchísimo | Pe reï ramo guare ejepy’apy, o nde pochy o nde py’a tarová. ¿mba’eicha eñeñandu? a. Michimimi ejepy’apy, pochy o py’a tarová b. Michimi o Heta avei c. Heta iterei |
| 9 | How often do you feel depressed? a. Never b. A few times a year c. Monthly d. Weekly e. Daily | ¿En qué momento te sentís demasiado o muy deprimido? a. Nunca b. De vez en cuando en el año c. De vez en cuando cada mes d. De vez en cuando cada semana e. A diario | ¿Mba’eicha jave eñeñandú ñembyasyeterei? a. Mba’eicha vevo b. Sapy’a py’a Ary c. Sapy’a py’a Ary jasykuéra d. Sapy’a py’a Arapoköindy rehegua e. Tapiaite |
| 10 | How depressed you felt when last time you were depressed? a. A little b. Somewhere in between a little and a lot c. A lot | Pensando en la última vez que se sintió deprimido, ¿qué tan deprimido se sintió? a. Muy poco deprimido. b. Poco o mucho c. Muchísimo | Pe reï ramo guare ñembyasyeterei? ¿mba’eicha eñeñandu? a. Michimimi ejepy’apy, pochy o py’a tarová b. Michimi o Heta avei c. Heta iterei |
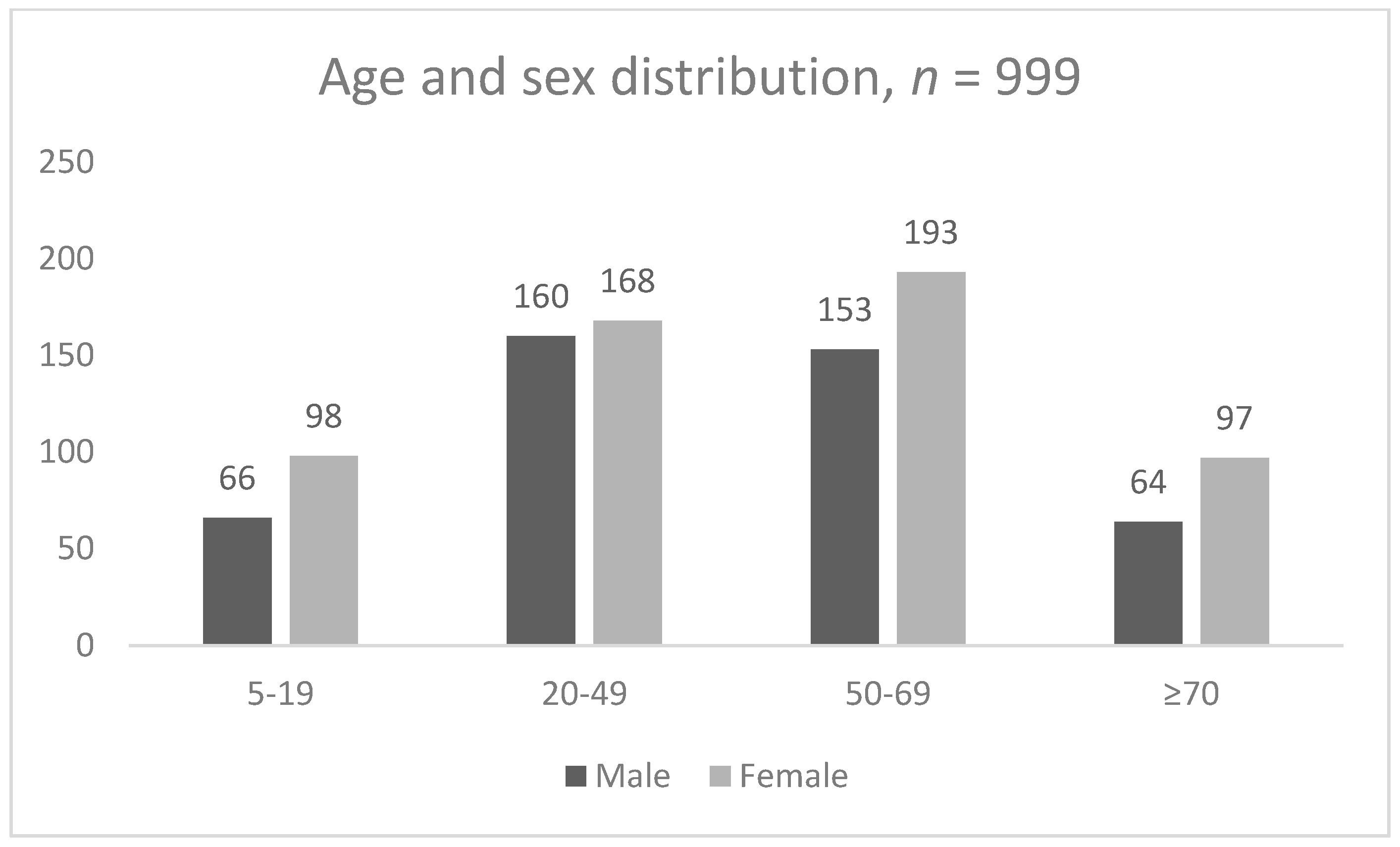
| Male (n = 443) | Female (n = 556) | Total (n = 999) | ||||||
|---|---|---|---|---|---|---|---|---|
| Domain | N | % (95% CI) | N | % (95% CI) | N | % (95% CI) | OR (95%CI) | |
| 1 | Visual | 67 | 15.1 (11.9–18.8) | 97 | 17.4 (14.4–20.9) | 164 | 16.4 (14.2–18.9) | 0.85 (0.6–1.2) |
| 2 | Hearing | 14 | 3.2 (1.7–5.2) | 21 | 3.8 (2.4–5.7) | 35 | 3.5 (2.5–4.8) | 0.84 (0.39–1.75) |
| 3 | Mobility | 15 | 3.4 (1.9–5.3) | 23 | 4.1 (2.6–6.1) | 38 | 3.8 (2.7–5.2) | 0.82 (0.39–1.65) |
| 4 | Remembering/Concentrating | 15 | 3.4 (1.9–5.5) | 44 | 7.9 (5.8–10.5) | 59 | 5.9 (4.5–7.6) | 0.41 (0.21–0.76) |
| 5 | Self-care | 8 | 1.8 (0.8–3.5) | 11 | 1.4 (0.6–2.8) | 19 | 1.9 (1.1–3.0) | 0.91 (0.32–2.51) |
| 6 | Communicating | 45 | 10.2 (7.5–13.4) | 51 | 9.2 (7.0–11.9) | 96 | 9.6 (7.9–11.6) | 1.2 (0.72–1.74) |
| Disability | 113 | 25.5 (21.5–30.0) | 163 | 29.3 (25.6–33.3) | 276 | 27.7 (24.9–30.3) | 0.83 (0.62–1.1) | |
| Domain | 5–19 years (n = 164) | 20–49 years (n = 328) | 50–69 years (n = 346) | ≥ 70 years (n = 161) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N | % (95% CI) | N | % (95% CI) | Adjusted OR (95% CI) | N | % (95% CI) | Adjusted OR (95% CI) | N | % (95% CI) | Adjusted OR (95% CI) | ||
| 1 | Visual | 18 | 10.9 (6.6–16.8) | 30 | 9.1 (6.3–12.8) | 0.8 (0.4–1.5) | 57 | 16.5 (12.7–20.8) | 1.6 (0.9–2.8) | 59 | 36.7 (29.2–44.6) | 4.7 (2.6–8.4) |
| 2 | Hearing | 2 | 1.2 (0.2–4.3) | 3 | 0.9 (0.2–2.6) | 0.8 (0.1–4.6) | 11 | 3.2 (1.6–5.6) | 2.7 (0.6–12.1) | 19 | 11.8 (7.3–17.8) | 10.8 (2.5–47.3) |
| 3 | Walking | 1 | 0.6 (0.02–3.4) | 3 | 0.9 (0.2–2.6) | 1.5 (0.2–14.8) | 10 | 2.9 (1.4–5.3) | 4.9 (0.6–38.4) | 24 | 14.9 (9.8–21.4) | 28.5 (3.8–213.7) |
| 4 | Remembering/ Concentrating | 10 | 6.1 (3.0–10.9) | 7 | 2.1 (0.9–4.3) | 0.4 (0.1–1.0) | 26 | 7.6 (5.0–10.8) | 1.3 (0.6–2.7) | 16 | 9.9 (5.8–15.6) | 1.7 (0.7–3.9) |
| 5 | Self-care | 4 | 2.4 (0.7–6.1) | 2 | 0.6 (0.1–2.2) | 0.2 (0.04–1.4) | 3 | 0.9 (0.2–2.5) | 0.4 (0.08–1.6) | 10 | 6.2 (3.0–11.1) | 2.6 (0.8–8.6) |
| 6 | Communicating | 6 | 3.6 (1.4–7.8) | 17 | 5.2 (3.1–8.2) | 1.4 (0.5–3.7) | 36 | 10.4 (7.4–14.1) | 3.0 (1.3–7.4) | 37 | 23.0 (16.7–30.3) | 7.9 (3.2–19.3) |
| Disability | 26 | 15.8 (10.6–22.4) | 48 | 14.6 (11.0–19.0) | 0.9 (0.5–1.5) | 103 | 29.8 (25.0–34.9) | 2.3 (1.4–3.7) | 99 | 61.5 (53.5–69.0) | 8.5 (5.0–14.4) | |
| Level of Feelings Last Time You Felt Worried, Nervous or Anxious | How Often do You Feel Worried, Nervous or Anxious | |||||
|---|---|---|---|---|---|---|
| Daily | Weekly | Monthly | Annually | Never | Total | |
| Not asked | 0 | 0 | 0 | 0 | 87 | 87 |
| A little | 15 | 19 | 18 | 56 | 0 | 108 |
| In between a little and a lot | 22 | 59 | 71 | 83 | 0 | 235 |
| A lot | 18 | 12 | 9 | 8 | 0 | 47 |
| Total | 55 | 90 | 98 | 147 | 87 | 477 |
| Indicator Affect/Anxiety Domain | N | % |
|---|---|---|
| 1 | 234 | 46.7 |
| 2 | 191 | 38.1 |
| 3 | 34 | 6.8 |
| 4 (category for having disability) | 18 | 3.6 |
| Excluded | 24 | 4.8 |
| Total | 501 | 100 |
| How Depressed You Felt when Last Time You Were Depressed? | How Often do You Feel Depressed? | |||||
|---|---|---|---|---|---|---|
| Daily | Weekly | Monthly | Annually | Never | Total | |
| Not asked | 0 | 0 | 0 | 0 | 68 | 68 |
| A little | 2 | 7 | 10 | 51 | 0 | 70 |
| In between a little and a lot | 13 | 26 | 48 | 86 | 0 | 170 |
| A lot | 7 | 17 | 6 | 9 | 0 | 39 |
| Total | 22 | 50 | 64 | 146 | 68 | 350 |
| Indicator Affect/Depression Domain | n | % |
|---|---|---|
| 1 | 214 | 42.7 |
| 2 | 99 | 19.8 |
| 3 | 30 | 6.0 |
| 4 (category for having disability) | 7 | 1.4 |
| Excluded | 151 | 30.1 |
| Total | 501 | 100 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mörchen, M.; Zambrano, O.; Páez, A.; Salgado, P.; Penniecook, J.; Brandt von Lindau, A.; Lewis, D. Disability-Disaggregated Data Collection: Hospital-Based Application of the Washington Group Questions in an Eye Hospital in Paraguay. Int. J. Environ. Res. Public Health 2019, 16, 3085. https://doi.org/10.3390/ijerph16173085
Mörchen M, Zambrano O, Páez A, Salgado P, Penniecook J, Brandt von Lindau A, Lewis D. Disability-Disaggregated Data Collection: Hospital-Based Application of the Washington Group Questions in an Eye Hospital in Paraguay. International Journal of Environmental Research and Public Health. 2019; 16(17):3085. https://doi.org/10.3390/ijerph16173085
Chicago/Turabian StyleMörchen, Manfred, Olmedo Zambrano, Alexander Páez, Paola Salgado, Jason Penniecook, Andrea Brandt von Lindau, and David Lewis. 2019. "Disability-Disaggregated Data Collection: Hospital-Based Application of the Washington Group Questions in an Eye Hospital in Paraguay" International Journal of Environmental Research and Public Health 16, no. 17: 3085. https://doi.org/10.3390/ijerph16173085
APA StyleMörchen, M., Zambrano, O., Páez, A., Salgado, P., Penniecook, J., Brandt von Lindau, A., & Lewis, D. (2019). Disability-Disaggregated Data Collection: Hospital-Based Application of the Washington Group Questions in an Eye Hospital in Paraguay. International Journal of Environmental Research and Public Health, 16(17), 3085. https://doi.org/10.3390/ijerph16173085





