Mental Strain of Immigrants in the Working Context
Abstract
1. Introduction
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders; American Psychiatric Association Publishing: Washington DC, USA, 2013. [Google Scholar]
- ICD. ICD-11 for Mortality and Morbidity Statistics. Available online: https://icd.who.int/browse11/l-m/en (accessed on 11 January 2019).
- Deutsches Institut für Medizinische Dokumentation und Information. ICD-10-GM Version 2017 Systematisches Verzeichnis Internationale Statistische Klassifikation der Krankheiten und Verwandter Gesundheitsprobleme, 10. Revision; DIMDI: Köln, Germany, 2017. [Google Scholar]
- OECD. Health at a Glance: Europe 2018; OECD: Paris, France, 2018; ISBN 9789264303348. [Google Scholar]
- Wittchen, H.-U.; Jacobi, F.; Rehm, J.; Gustavsson, A.; Svensson, M.; Jönsson, B.; Olesen, J.; Allgulander, C.; Alonso, J.; Faravelli, C.; et al. The size and burden of mental disorders and other disorders of the brain in Europe 2010. Eur. Neuropsychopharmacol. 2011, 21, 655–679. [Google Scholar] [CrossRef] [PubMed]
- Whiteford, H.A.; Degenhardt, L.; Rehm, J.; Baxter, A.J.; Ferrari, A.J.; Erskine, H.E.; Charlson, F.J.; Norman, R.E.; Flaxman, A.D.; Johns, N.; et al. Global burden of disease attributable to mental and substance use disorders: Findings from the Global Burden of Disease Study 2010. Lancet 2013, 382, 1575–1586. [Google Scholar] [CrossRef]
- Knieps, F.; Pfaff, H. BKK Gesundheitsreport 2018; Medizinisch Wissenschaftliche Verlagsgesellschaft (MWV): Berlin, Germany, 2018. [Google Scholar]
- BKK Bundesverband. BKK Gesundheitsreport 2008; BKK: Essen, Germany, 2008. [Google Scholar]
- Deutsche Rentenversicherung Bund. Rente 2017; DRV: Berlin, Germany, 2018. [Google Scholar]
- Marschall, J.; Hildebrandt, S.; Zich, K.; Tisch, T.; Sörensen, J.; Nolting, H.-D. DAK Gesundheitsreport 2018; DAK: Hamburg, Germany, 2018. [Google Scholar]
- Badura, B.; Ducki, A.; Schröder, H.; Klose, J.; Meyer, M. Fehlzeiten-Report 2018; Springer: Berlin/Heidelberg, Germany, 2018; ISBN 978-3-662-57387-7. [Google Scholar]
- Siegrist, J. Burn-out und Arbeitswelt. Psychother 2013, 58, 110–116. [Google Scholar] [CrossRef]
- Bundesministerium für Arbeit und Soziales (publisher). Arbeitsschutzgesetz vom 7. August 1996 (BGBl. I S. 1246), das Zuletzt Durch Artikel 427 der Verordnung vom 31. August 2015 (BGBl. I S. 1474) Geändert Worden Ist; In ArbSchG: Berlin, Germany, 1996. [Google Scholar]
- Rohmert, W.; Rutenfranz, J. Arbeitswissenschaftliche Beurteilung der Belastung und Beanspruchung an Unterschiedlichen Industriearbeitsplätzen; Bundesministerium für Arbeit und Sozialordnung: Bonn, Germany, 1975. [Google Scholar]
- Hapke, U.; Maske, U.E.; Scheidt-Nave, C.; Bode, L.; Schlack, R.; Busch, M.A. Chronischer Stress bei Erwachsenen in Deutschland: Ergebnisse der Studie zur Gesundheit Erwachsener in Deutschland (DEGS1). Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz 2013, 56, 749–754. [Google Scholar] [CrossRef] [PubMed]
- McEwen, B.S. Stress and the individual. Mechanisms leading to disease. Arch. Intern. Med. 1993, 153, 2093–2101. [Google Scholar] [CrossRef] [PubMed]
- Karasek, R.A. Job Demands, Job Decision Latitude, and Mental Strain: Implications for Job Redesign. Adm. Sci. Q. 1979, 24, 285. [Google Scholar] [CrossRef]
- Johnson, J. Control, Collectivity and Psychological Work Environment. Job Control Work. Health 1989, 55–74. [Google Scholar]
- Siegrist, J. Adverse health effects of high-effort/low-reward conditions. J. Occup. Heal. Psychol. 1996, 1, 27–41. [Google Scholar] [CrossRef]
- Warr, P. Environmental “Vitamins”, Personal Judgments, Work Values, and Happiness. In The Oxford Handbook of Organizational Well Being; Cartwright, S., Cooper, C.L., Eds.; Oxford University Press: Oxford, UK, 2009. [Google Scholar]
- Kaschka, W.P.; Korczak, D.; Broich, K. Burnout: A Fashionable Diagnosis. Dtsch. Aerzteblatt Online 2011, 108, 781–787. [Google Scholar]
- Korczak, D.; Kister, C.; Huber, B. Differentialdiagnostik des Burnout-Syndroms; HTA Bericht 105, 1. Auflage; Deutsches Instituts für Medizinische Dokumentation und Information (DIMDI): München/Köln, Germany, 2010. [Google Scholar]
- Maslach, C.; Jackson, S.; Leiter, M. The Maslach Burnout Inventory Manual. In Evaluating Stress: A Book of Resources; Zalaquett, C., Wood, R., Eds.; The Scarecrow Press: New York, NY, USA, 1996; pp. 191–218. [Google Scholar]
- Kristensen, T.S.; Borritz, M.; Villadsen, E.; Christensen, K.B. The Copenhagen Burnout Inventory: A new tool for the assessment of burnout. Work Stress 2005, 19, 192–207. [Google Scholar] [CrossRef]
- Statistisches Bundesamt. Pressemitteilung Nr. 396 vom 15. Oktober 2018; Destatis: Wiesbaden, Germany, 2018. [Google Scholar]
- Schunck, R.; Reiss, K.; Razum, O. Pathways between perceived discrimination and health among immigrants: Evidence from a large national panel survey in Germany. Ethn. Health 2015, 20, 493–510. [Google Scholar] [CrossRef] [PubMed]
- Hogh, A.; Carneiro, I.G.; Giver, H.; Rugulies, R. Are immigrants in the nursing industry at increased risk of bullying at work? A one-year follow-up study. Scand. J. Psychol. 2011, 52, 49–56. [Google Scholar] [CrossRef] [PubMed]
- Hofstede, G. National Cultures in Four Dimensions: A Research-Based Theory of Cultural Differences among Nations. Int. Stud. Manag. Organ. 1983, 13, 46–74. [Google Scholar] [CrossRef]
- Rogler, L.H.; Cortés, D.E.; Malgady, R.G. Acculturation and mental health status among Hispanics: Convergence and new directions for research. Am. Psychol. 1991, 46, 585–597. [Google Scholar] [CrossRef] [PubMed]
- Grzywacz, J.G.; Quandt, S.A.; Early, J.; Tapia, J.; Graham, C.N.; Arcury, T.A. Leaving Family for Work: Ambivalence and Mental Health Among Mexican Migrant Farmworker Men. J. Immigr. Minor. Heal. 2006, 8, 85–97. [Google Scholar] [CrossRef]
- Roland, A. The familial self, the individualized self, and the transcendent self: Psychoanalytic reflections on India and America. Psychoanal. Rev. 1987, 74, 237–250. [Google Scholar] [PubMed]
- Razum, O.; Wenner, J. Social and health epidemiology of immigrants in Germany: Past, present and future. Public Heal. Rev. 2016, 37, 141. [Google Scholar] [CrossRef]
- Mösko, M.-O.; Pradel, S.; Schulz, H. Die Versorgung von Menschen mit Migrationshintergrund in der psychosomatischen Rehabilitation. Bundesgesundheitsblatt Gesundh. Gesundh. 2011, 54, 465–474. [Google Scholar] [CrossRef]
- Gäbel, U.; Ruf, M.; Schauer, M.; Odenwald, M.; Neuner, F. Prävalenz der Posttraumatischen Belastungsstörung (PTSD) und Möglichkeiten der Ermittlung in der Asylverfahrenspraxis. Z. Klin. Psychol. Psychother. 2006, 35, 12–20. [Google Scholar] [CrossRef]
- Richter, K.; Lehfeld, H.; Niklewski, G. Warten auf Asyl: Psychiatrische Diagnosen in der zentralen Aufnahmeeinrichtung in Bayern. Das Gesundh. 2015, 77, 834–838. [Google Scholar] [CrossRef]
- Krueger, D.E.; Moriyama, I.M. Mortality of the foreign born. Am. J. Public Health Nations Health 1967, 57, 496–503. [Google Scholar] [CrossRef] [PubMed]
- Pablos-Méndez, A. Mortality among Hispanics. JAMA 1994, 271, 1237. [Google Scholar] [CrossRef] [PubMed]
- Wallace, M.; Kulu, H. Low immigrant mortality in England and Wales: A data artefact? Soc. Sci. Med. 2014, 120, 100–109. [Google Scholar] [CrossRef] [PubMed]
- Zeeb, H.; Rohrmann, S.; Razum, O. The ‘healthy migrant effect’—Not merely a fallacy of inaccurate denominator figures. Int. J. Epidemiol. 2000, 29, 191–192. [Google Scholar]
- Budhwani, H.; Hearld, K.R.; Chavez-Yenter, D. Depression in Racial and Ethnic Minorities: The Impact of Nativity and Discrimination. J. Racial Ethn. Health Disparities 2015, 2, 34–42. [Google Scholar] [CrossRef]
- Alegría, M.; Canino, G.; Shrout, P.E.; Woo, M.; Duan, N.; Vila, D.; Torres, M.; Chen, C.-N.; Meng, X.-L. Prevalence of mental illness in immigrant and non-immigrant U.S. Latino groups. Am. J. Psychiatry 2008, 165, 359–369. [Google Scholar] [CrossRef]
- Breslau, J.; Chang, D.F. Psychiatric disorders among foreign-born and US-born Asian-Americans in a US national survey. Soc. Psychiatry Psychiatr. Epidemiol. 2006, 41, 943–950. [Google Scholar] [CrossRef]
- Vega, W.A.; Sribney, W.M.; Aguilar-Gaxiola, S.; Kolody, B. 12-Month Prevalence of DSM-III-R Psychiatric Disorders among Mexican Americans: Nativity, Social Assimilation, and Age Determinants. J. Nerv. Ment. Dis. 2004, 192, 532–541. [Google Scholar] [CrossRef]
- Hutchinson, G.; Haasen, C. Migration and schizophrenia: The challenges for European psychiatry and implications for the future. Soc. Psychiatry Psychiatr. Epidemiol. 2004, 39, 350–357. [Google Scholar] [CrossRef]
- Van Der Ven, E.; Selten, J.-P. Migrant and ethnic minority status as risk indicators for schizophrenia. Curr. Opin. Psychiatry 2018, 31, 231–236. [Google Scholar] [CrossRef]
- Cantor-Graae, E.; Selten, J.-P. Schizophrenia and Migration: A Meta-Analysis and Review. Am. J. Psychiatry 2005, 162, 12–24. [Google Scholar] [CrossRef]
- Constant, A.F. The Healthy Immigrant Paradox and Health Convergence; GLO Discussion Paper; Global Labor Organization: Princeton, NJ, USA, 2017. [Google Scholar]
- Eschbach, K.; Stimpson, J.P.; Kuo, Y.-F.; Goodwin, J.S. Mortality of Foreign-Born and US-Born Hispanic Adults at Younger Ages: A Reexamination of Recent Patterns. Am. J. Public Heal. 2007, 97, 1297–1304. [Google Scholar] [CrossRef]
- Ng, E.; Wilkins, R.; Gendron, F.; Berthelot, J.-M. Dynamics of immigrants’ health: Evidence from Canada, 1994–95 to 2002–03. Summary Report. Can. Stud. Popul. 2005, 32, 131–133. [Google Scholar] [CrossRef]
- Grigg, D. EG Ravenstein and the “laws of migration”. J. Hist. Geogr. 1977, 3, 41–54. [Google Scholar] [CrossRef]
- Borjas, G.J. Self-Selection and the Earnings of Immigrants; National Bureau of Economic Research: Cambridge, MA, USA, 1987. [Google Scholar]
- Clasen, J.; Busch, C.; Vowinkel, J.; Winkler, E. Arbeitssituation und Gesundheit von geringqualifizierten Beschäftigten in kulturell diversen Belegschaften. Grup. Organ. 2013, 44, 91–110. [Google Scholar] [CrossRef]
- Mountford, A. Can a brain drain be good for growth in the source economy? J. Dev. Econ. 1997, 53, 287–303. [Google Scholar] [CrossRef]
- Nübling, M.; Stössel, U.; Michaelis, M. Messung von Führungsqualität und Belastungen am Arbeitsplatz: Die deutsche Standardversion des COPSOQ (Copenhagen Psychosocial Questionnaire). In Fehlzeiten-Report 2009; Springer Science and Business Media LLC: Berlin/Heidelberg, Germany, 2010; pp. 253–261. [Google Scholar]
- Nübling, M. Methoden zur Erfassung Psychischer Belastungen. Erprobung Eines Messinstrumentes (COPSOQ); Projekt F 1885; Wirtschaftsverl. NW Verl. für Neue Wiss: Bremerhaven, Germany, 2005. (In Germany) [Google Scholar]
- Hoebel, J.; Kuntz, B.; Moor, I.; Kroll, L.E.; Lampert, T. Post-millennial trends of socioeconomic inequalities in chronic illness among adults in Germany. BMC Res. Notes 2018, 11, 200. [Google Scholar] [CrossRef]
- Statistisches Bundesamt. Bevölkerung mit Migrationshintergrund—Ergebnisse des Mikrozensus 2017 vom 01. August 2018; Destatis: Wiesbaden, Germany, 2018; p. 34. [Google Scholar]
- Chin, R.W.A.; Chua, Y.Y.; Chu, M.N.; Mahadi, N.F.; Wong, M.S.; Yusoff, M.S.; Lee, Y.Y.; Yusoff, M.S.B. Investigating validity evidence of the Malay translation of the Copenhagen Burnout Inventory. J. Taibah Univ. Med Sci. 2018, 13, 1–9. [Google Scholar]
- Lin, L.-P.; Wu, T.-Y.; Lin, J.-D. Comparison of job burnout and life satisfaction between native and foreign female direct care workers in disability institutions. Work 2015, 52, 803–809. [Google Scholar] [CrossRef]
- Jaekel-Reinhard, A.; Weber, A. Burnout Syndrome: A Disease of Modern Societies? Occup. Med. 2000, 50, 512–517. [Google Scholar]
- Bundeszentrale für Politische Bildung. Zahlen zu Asyl in Deutschland. Available online: https://www.bpb.de/gesellschaft/migration/flucht/265707/zahlen-zu-asyl-in-deutschland (accessed on 28 May 2019).
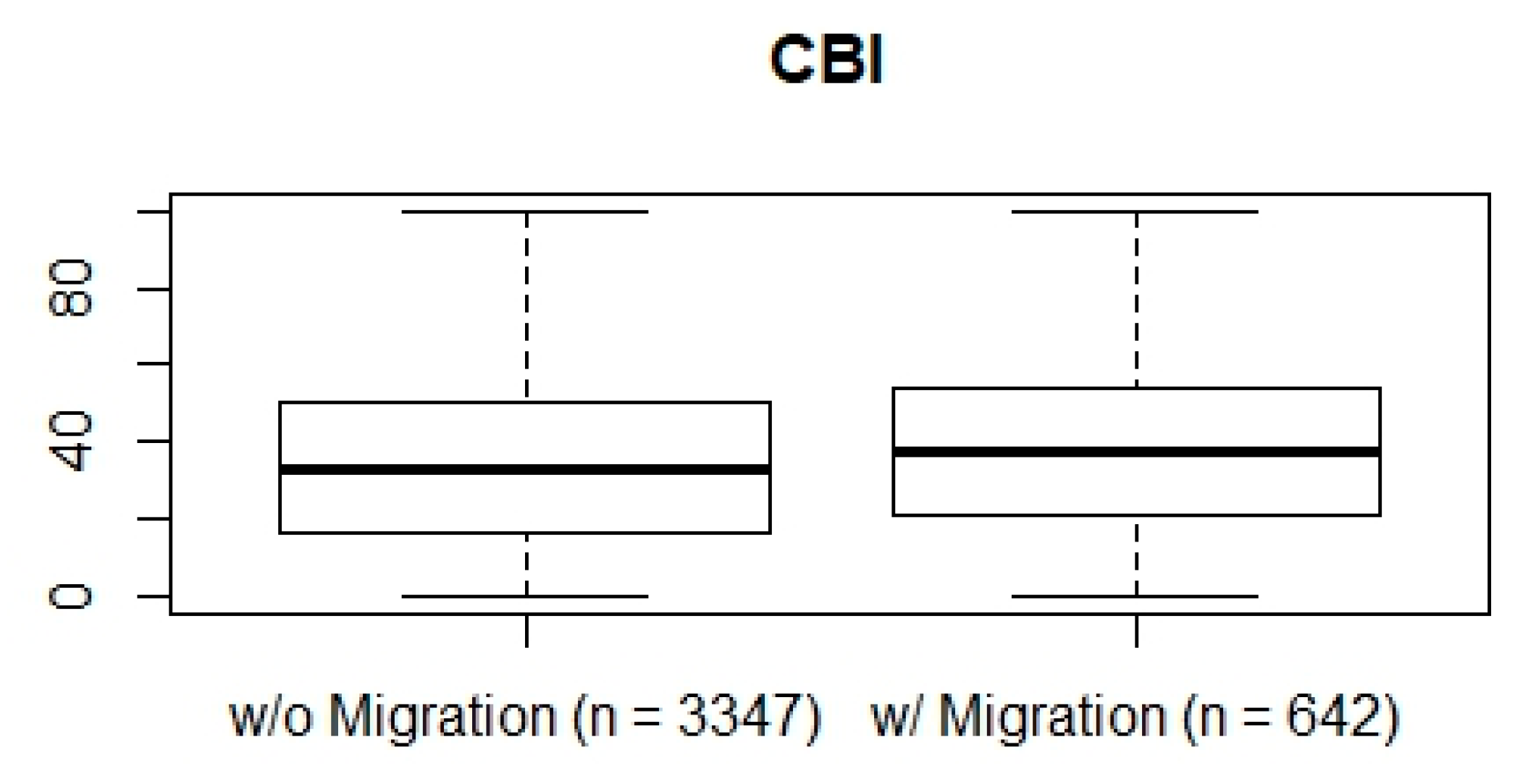
| Variable | Without Migration Background | With Migration Background |
|---|---|---|
| n= | 3347 | 642 |
| Mean Age in Years | 41.90 ± 11.60 | 39.38 ± 11.40 |
| Men % | 55 | 48 |
| Full Time % | 87 | 84 |
| University Degree % | 27 | 29 |
| Satisfied with One’s General Health % | 55 | 56 |
| Satisfied with One’s Wage % | 47 | 48 |
| Satisfied with Sense of Community at Work % | 51 | 51 |
| Mean Count of Children below 16 Years | 0.48 ± 0.78 | 0.46 ± 0.83 |
| Taking Care of Other Relatives % | 0.10 | 0.11 |
| Variable | Estimate | Significance |
|---|---|---|
| n= | 3858 | p= |
| Intercept | 15.06 | <0.001 |
| Migration Background (binary) | 3.01 | <0.001 |
| Part Time Work (binary) | 0.51 | 0.542 |
| Male Sex (binary) | –9.67 | <0.001 |
| Age | –0.1 | <0.001 |
| Sense of Community at Work(decreasing from 1 to 5) | 1.94 | <0.001 |
| Educational attainment | 0.16 | 0.468 |
| General Health(decreasing from 1 to 5) | 6.53 | <0.001 |
| Wage Satisfaction (decreasing from 1 to 5) | 3.08 | <0.001 |
| Care-dependent Relatives (binary) | 4.75 | <0.001 |
| Children below 16 Years | 1.22 | 0.002 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Claassen, K.; Broding, H.C. Mental Strain of Immigrants in the Working Context. Int. J. Environ. Res. Public Health 2019, 16, 2875. https://doi.org/10.3390/ijerph16162875
Claassen K, Broding HC. Mental Strain of Immigrants in the Working Context. International Journal of Environmental Research and Public Health. 2019; 16(16):2875. https://doi.org/10.3390/ijerph16162875
Chicago/Turabian StyleClaassen, Kevin, and Horst Christoph Broding. 2019. "Mental Strain of Immigrants in the Working Context" International Journal of Environmental Research and Public Health 16, no. 16: 2875. https://doi.org/10.3390/ijerph16162875
APA StyleClaassen, K., & Broding, H. C. (2019). Mental Strain of Immigrants in the Working Context. International Journal of Environmental Research and Public Health, 16(16), 2875. https://doi.org/10.3390/ijerph16162875





