Association of Access to Healthcare with Self-Assessed Health and Quality of Life among Old Adults with Chronic Disease in China: Urban Versus Rural Populations
Abstract
1. Introduction
2. Methods
Data
3. Measurements
3.1. Outcome Variables
3.2. Explanatory Variables
3.3. Control Variables
3.4. Statistical Analysis
4. Results
4.1. Characteristics of Respondents
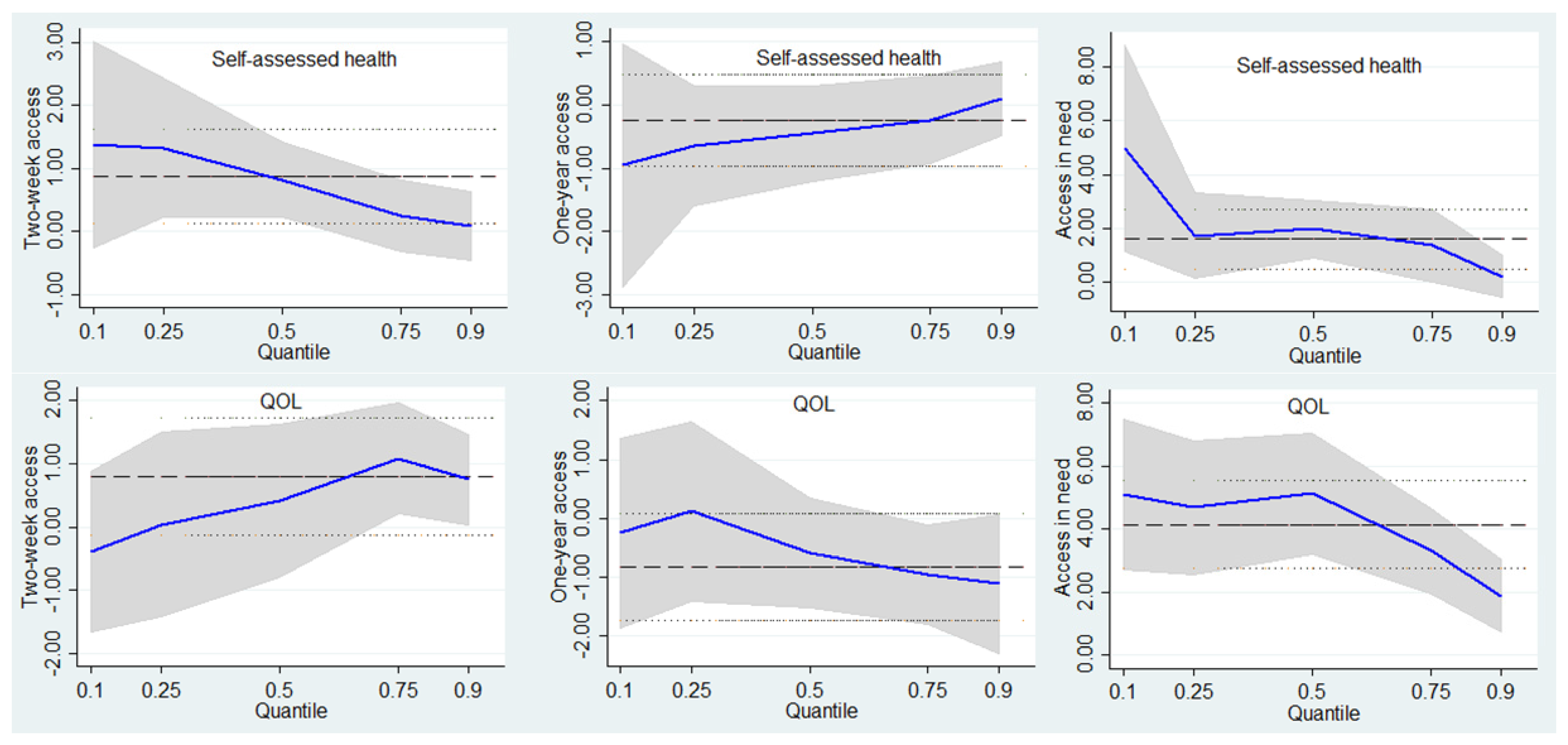
4.2. Associations of Access to Healthcare with Self-Assessed Health and QOL in Urban Respondents
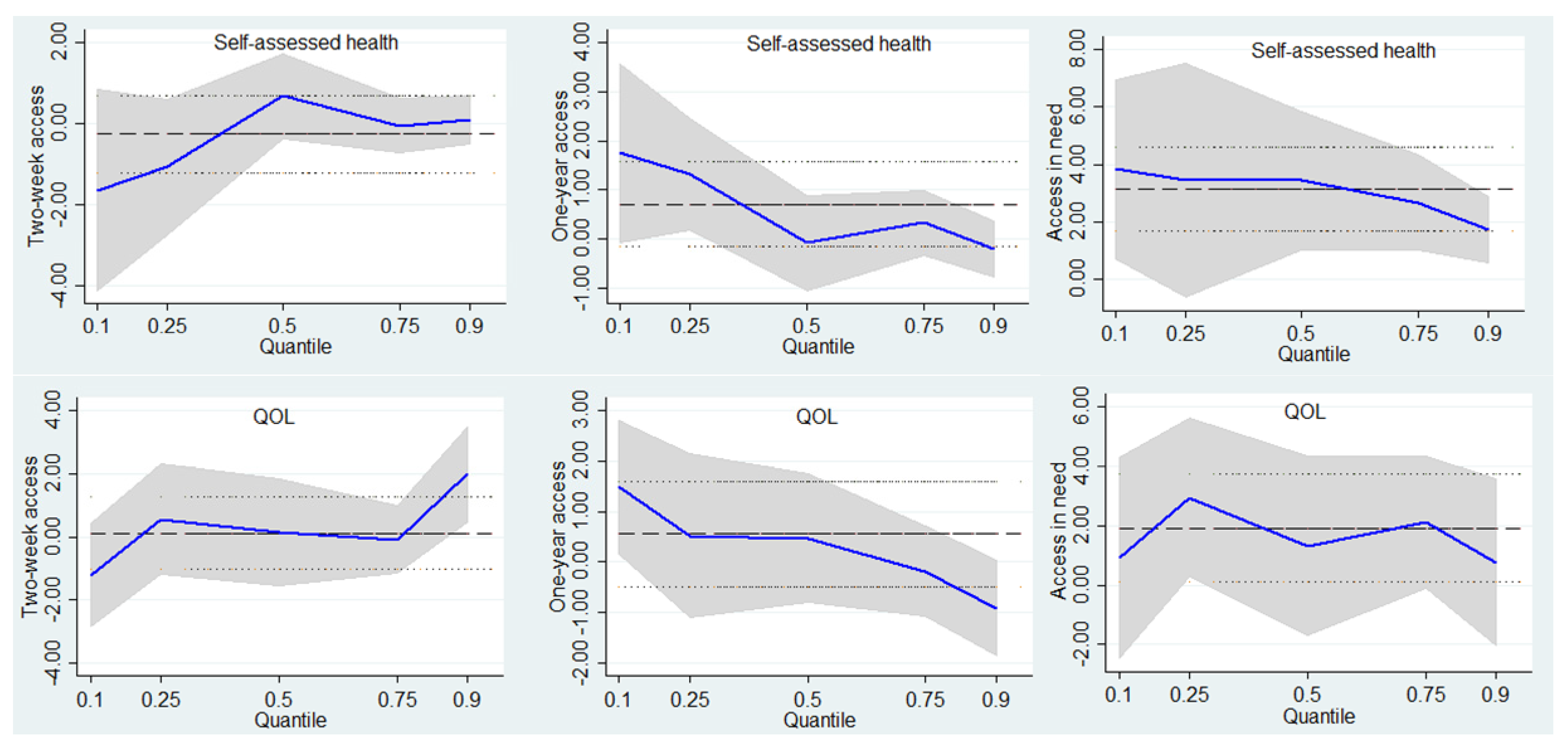
4.3. Associations of Access to Healthcare with Self-Assessed Health and QOL in Rural Respondents
5. Discussion
6. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Ethical Approval
References
- Westaway, M.S. The impact of chronic diseases on the health and well-being of South Africans in early and later old age. Arch. Gerontol. Geriatr. 2010, 50, 213–221. [Google Scholar] [CrossRef] [PubMed]
- Xie, H.; Cheng, C.; Tao, Y.; Zhang, J.; Robert, D.; Jia, J.; Su, Y. Quality of life in Chinese family caregivers for elderly people with chronic diseases. Health Qual. Life Outcomes 2016, 14, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Chen, M.; Wang, Z.; Si, L. Forgone care among middle aged and elderly with chronic diseases in China: Evidence from the China health and retirement longitudinal study baseline survey. BMJ Open 2018, 8, e019901. [Google Scholar] [CrossRef] [PubMed]
- Shanshan, J.; Aitian, Y.; Lizheng, S.; Jinan, L. Whether New Cooperative Mmedical Schemes reduce the economic burden of chronic disease in rural China. PLoS ONE 2013, 8, e53062. [Google Scholar]
- Wang, L.; Kong, L.; Wu, F.; Bai, Y.; Burton, R. Chronic diseases 4—Preventing chronic diseases in China. Lancet 2005, 366, 1821–1824. [Google Scholar] [CrossRef]
- Mendoza-Núñez, V.M.; Correa-Muñoz, E. Implementation of an active aging model in Mexico for prevention and control of chronic diseases in the elderly. BMC Geriatr. 2009, 9, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Juenger, J.; Schellberg, D.; Kraemer, S.; Haunstetter, A.; Zugck, C.; Herzog, W.; Haass, M. Health related quality of life in patients with congestive heart failure: Comparison with other chronic diseases and relation to functional variables. Heart 2002, 87, 235–241. [Google Scholar] [CrossRef] [PubMed]
- Kalantar-Zadeh, K.; Unruh, M. Health related quality of life in patients with chronic kidney disease. Int. Urol. Nephrol. 2005, 37, 367–378. [Google Scholar] [CrossRef]
- Lam, C.L.; Lauder, I.J.; Lam, T.P.D. Impact of chronic diseases on health services and quality of life of a Chinese population. Asia Pac. Fam. Med. 2015, 2, 98–106. [Google Scholar] [CrossRef][Green Version]
- Yamada, T.; Chen, C.C.; Murata, C.; Hirai, H.; Ojima, T.; Kondo, K. Access disparity and health inequality of the elderly: unmet needs and delayed healthcare. Int. J. Environ. Res. Public Health 2015, 12, 1745–1772. [Google Scholar] [CrossRef]
- Xiong, X.; Zhang, Z.; Ren, J.; Zhang, J.; Pan, X.; Zhang, L.; Gong, S.; Jin, S. Impact of universal medical insurance system on the accessibility of medical service supply and affordability of patients in China. PLoS ONE 2018, 13, e0193273. [Google Scholar] [CrossRef] [PubMed]
- Hongmei, Y.; Linxiu, Z.; Kim, S.; Scott, R.; Scott, A. Health insurance and catastrophic illness: A report on the new cooperative medical system in rural China. Health Econ. 2010, 18, S119–S127. [Google Scholar]
- Yin, D.; Wong, S.T.; Wei, C.; Xin, Q.; Wang, L.; Cui, M.; Tao, Y.; Li, R.; Zheng, X.; Yang, H. A model to estimate the cost of the national essential public health services package in Beijing, China. BMC Health Serv. Res. 2015, 15, 222. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Zhang, W. The impacts of health insurance on health care utilization among the older people in China. Soc. Sci. Med. 2013, 85, 59–65. [Google Scholar] [CrossRef] [PubMed]
- Liu, H.; Zhao, Z. Does health insurance matter? Evidence from China’s urban resident basic medical insurance. J. Comp. Econ. 2014, 42, 1007–1020. [Google Scholar] [CrossRef]
- Alonso, J.; Orfila, F.; Ruigómez, A.; Ferrer, M.; Antó, J.M. Unmet health care needs and mortality among Spanish elderly. Am. J. Public Health 1997, 87, 365. [Google Scholar] [CrossRef] [PubMed]
- Porell, F.W.; Miltiades, H.B. Access to care and functional status change among aged medicare beneficiaries. J. Gerontol. 2001, 56, S69. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Dupre, M.E.; Qiu, L.; Zhou, W.; Zhao, Y.; Gu, D. Urban-rural differences in the association between access to healthcare and health outcomes among older adults in China. BMC Geriatr. 2017, 17, 151. [Google Scholar] [CrossRef]
- Li, Y.; Chi, I.; Zhang, K.; Guo, P. Comparison of health services use by Chinese urban and rural older adults in Yunnan province. Geriatr. Gerontol. Int. 2010, 6, 260–269. [Google Scholar] [CrossRef]
- Shi, L. Health care in China: A rural-urban comparison after the socioeconomic reforms. Bull. World Health Organ. 1993, 71, 723–736. [Google Scholar]
- Asmus-Szepesi, K.J.E.; de Vreede, P.L.; Flinterman, L.E.; Nieboer, A.P.; Bakker, T.J.E.M.; Borsboom, G.J.J.M.; Mackenbach, J.P.; Steyerberg, E.W. Prognosis of hospitalised older people with different levels of functioning: A prospective cohort study. Age Ageing 2013, 42, 803–809. [Google Scholar] [CrossRef][Green Version]
- Paul, K.; Somnath, C.; Nirmala, N.; Richard, B.; Wu, F.; Ruy, L.R.; Tamara, M.; Perianayagam, A.; Nancy, P.M.; Sharon, W. Data resource profile: The World Health Organization Study on global AGEing and adult health (SAGE). Int. J. Epidemiol. 2012, 41, 1639–1649. [Google Scholar]
- Enid, S.; Xavier, G.O.; Margaret, R.; Jane, M.; Stephen, T. The impact of pensions on health and wellbeing in rural South Africa: does gender matter? Soc. Sci. Med. 2012, 75, 1864–1873. [Google Scholar]
- Kowal, P.; Kahn, K.; Ng, N.; Naidoo, N.; Abdullah, S.; Bawah, A.; Binka, F.; Chuc, N.T.K.; Debpuur, C.; Ezeh, A.; et al. Ageing and adult health status in eight lower-income countries: the INDEPTH WHO-SAGE collaboration. Global Health Action 2010, 3, 11–22. [Google Scholar] [CrossRef]
- Schmidt, S.; Muhlan, H.; Power, M. The EUROHIS-QOL 8-item index: Psychometric results of a cross-cultural field study. Eur. J. Public Health 2006, 16, 420–428. [Google Scholar] [CrossRef]
- Penchansky, R.; Thomas, J.W. The concept of access: definition and relationship to consumer satisfaction. Med. Care 1981, 19, 127–140. [Google Scholar] [CrossRef]
- Danan, G.; Zhenmei, Z.; Yi, Z. Access to healthcare services makes a difference in healthy longevity among older Chinese adults. Soc. Sci. Med. 2009, 68, 210–219. [Google Scholar]
- Andersen, R.M. Revisiting the behavioral model and access to medical care: Does it matter? J. Health Soc. Behav. 1995, 36, 1–10. [Google Scholar] [CrossRef]
- Andersen, R.M.; Yu, H.; Wyn, R.; Davidson, P.L.; Brown, E.R.; Teleki, S. Access to medical care for low-income persons: How do communities make a difference? Med. Care Res. Rev. 2002, 59, 384. [Google Scholar] [CrossRef]
- Grossman, M. On the concept of health capital and the demand for health. J. Political Econ. 1972, 80, 223–255. [Google Scholar] [CrossRef]
- Borgoni, R.; Del, B.P.; Salvati, N.; Schmid, T.; Tzavidis, N. Modelling the distribution of health-related quality of life of advanced melanoma patients in a longitudinal multi-centre clinical trial using M-quantile random effects regression. Stat. Methods Med. Res. 2016, 27, 549–563. [Google Scholar] [CrossRef]
- Koenker, R.; Bassett, G. Regression quantiles. Econometrica 1978, 46, 33–50. [Google Scholar] [CrossRef]
- Larson, R. Thirty years of research on the subjective well-being of older americans. J. Gerontol. 1978, 33, 109–125. [Google Scholar] [CrossRef]
- Tian, M.; Wang, H.; Tong, X.; Zhu, K.; Zhang, X.; Chen, X. Essential public health services’ accessibility and its determinants among adults with chronic diseases in China. PloS ONE 2015, 10, e0125262. [Google Scholar] [CrossRef]
- Gong, C.H.; Kendig, H.; He, X. Factors predicting health services use among older people in China: An analysis of the China health and retirement longitudinal study 2013. BMC Health Serv. Res. 2016, 16, 63. [Google Scholar] [CrossRef]
- Yang, Q.; Dong, H. Have health human resources become more equal between rural and urban areas after the new reform? Int. J. Health Policy Manage. 2014, 3, 359. [Google Scholar] [CrossRef]
- Guo, M.; Aranda, M.P.; Silverstein, M. The impact of out-migration on the intergenerational support and psychological wellbeing of older adults in rural China. Ageing Soc. 2009, 29, 1085–1104. [Google Scholar] [CrossRef]
- Prigent, A.; Kamendjetchokobou, B.; Chevreul, K. Socio-demographic, clinical characteristics and utilization of mental health care services associated with SF-6D utility scores in patients with mental disorders: contributions of the quantile regression. Qual. Life Res. 2017, 26, 3035–3048. [Google Scholar] [CrossRef]
- Lindgren, B. EuroQol—A new facility for the measurement of health-related quality of life. Health Policy 1990, 16, 199–208. [Google Scholar]
- Hooker, K.; Siegler, I.C. Separating apples from oranges in health ratings: Perceived health includes psychological well-being. Behav. Health Aging 1991, 2, 81–92. [Google Scholar]
- Baiden, P.; Dunnen, W.D.; Fallon, B. Examining the independent effect of social support on unmet mental healthcare needs among Canadians: Findings from a population-based study. Soc. Indic. Res. 2017, 130, 1229–1246. [Google Scholar] [CrossRef]
- Liu, L.F.; Tian, W.H.; Yao, H.P. Utilization of health care services by elderly people with National Health Insurance in Taiwan: The heterogeneous health profile approach. Health Policy 2012, 108, 246–255. [Google Scholar] [CrossRef]
- Guimarães, R.M. Health capital, life course and ageing. Gerontology 2007, 53, 96–101. [Google Scholar] [CrossRef]
- Chen, Y.; Zhou, Y.; Xie, Q. Suggestions to ameliorate the inequity in urban/rural allocation of healthcare resources in China. Int. J. Equity Health 2014, 13, 34. [Google Scholar] [CrossRef]
- Luo, J.; Tian, L.; Luo, L.; Yi, H.; Wang, F. Two-Step optimization for spatial accessibility improvement: A case study of health care planning in rural China. Bio. Med. Res. Int. 2017, 2017, 2094654. [Google Scholar] [CrossRef]
| Variables | Description | Urban (n = 3194) | Rural (n = 2602) | p |
|---|---|---|---|---|
| Outcome variables | ||||
| Self-assessed health | Mean ± SD | 89.29 ± 8.96 | 86.79 ± 10.05 | <0.001 |
| Quality of life | Mean ± SD | 71.91 ± 11.10 | 69.46 ± 12.21 | <0.001 |
| Explanatory variables | ||||
| Two-week access | To medications or treatment for chronic conditions over the past 2 weeks (n, %) | 1247 (39.00) | 750 (28.80) | <0.001 |
| One-year access | To medications or treatment for chronic conditions over the past 12 months (n, %) | 1751 (54.80) | 1318 (50.70) | 0.002 |
| Access in need | Received healthcare services when needed (n, %) | 2970 (93.00) | 2410 (92.60) | 0.592 |
| Control variables | ||||
| Sex | Male (n, %) | 1356 (42.50) | 1179 (45.30) | 0.029 |
| Female (n, %) | 1838 (57.50) | 1423 (54.70) | ||
| Age | Years (mean ± SD) | 65.81 ± 9.39 | 63.76 ± 9.00 | <0.001 |
| Marital status | Never married (n, %) | 22 (0.70) | 19 (0.70) | 0.029 |
| Currently married (n, %) | 2589 (81.10) | 2102 (80.80) | ||
| Cohabiting (n, %) | 6 (0.20) | 7 (0.30) | ||
| Separated/divorced (n, %) | 62 (1.90) | 25 (1.00) | ||
| Widowed (n, %) | 515 (16.10) | 449 (17.30) | ||
| Ethnicity | Han (n, %) | 3131 (98.00) | 2577 (99.00) | 0.002 |
| Others (n, %) | 63 (2.00) | 25 (1.00) | ||
| Education | Years of school (mean ± SD) | 7.42 ± 4.67 | 3.09 ± 3.25 | <0.001 |
| Living arrangement | Moved from somewhere else (n, %) | 2271 (71.10) | 779 (29.90) | <0.001 |
| Always lived in the same village/town/city (n, %) | 923 (28.90) | 1823 (70.10) | ||
| Work | At least two days during the last seven days (n, %) | 2590 (81.10) | 1813 (69.70) | <0.001 |
| Less than two days during the last seven days (n, %) | 604 (18.90) | 789 (30.30) | ||
| Smoking | No (n, %) | 2626 (82.20) | 1840 (70.70) | <0.001 |
| Yes (n, %) | 568 (17.80) | 762 (29.30) | ||
| Drinking | No alcohol consumption in the last 30 days (n, %) | 2748 (86.00) | 2028 (77.90) | <0.001 |
| Consumed alcohol in the last 30 days (n, %) | 446 (14.00) | 574 (22.10) | ||
| Exercise | No (n, %) | 2365 (74.00) | 2382 (91.50) | <0.001 |
| Yes (n, %) | 829 (26.00) | 220 (8.50) | ||
| Household size | Total number of people living in the household (metric variable) (mean ± SD) | 2.72 ± 1.29 | 2.71 ± 1.35 | 0.914 |
| Social support | In the last 12 months, household did not receive any financial or in-kind support (n, %) | 2952 (92.40) | 1977 (76.70) | <0.001 |
| In the last 12 months, household received some financial or in-kind support (n, %) | 242 (7.60) | 605 (23.30) | ||
| Regular income | Regular source of income (n, %) | 3109 (97.30) | 1358 (52.20) | <0.001 |
| Regular but seasonal source of income (n, %) | 37 (1.20) | 825 (31.70) | ||
| No regular source of income (n, %) | 48 (1.50) | 419 (16.10) | ||
| Debt or loans | Household or any members of the household have current debt or outstanding loans (n, %) | 178 (5.60) | 469 (18.0) | <0.001 |
| Household or any members of the household have no current debt or outstanding loans (n, %) | 3016 (94.40) | 2133 (82.00) | ||
| Household’s financial situation | Very good (n, %) | 59 (1.80) | 18 (0.70) | <0.001 |
| Good (n, %) | 599 (18.80) | 227 (8.70) | ||
| Moderate (n, %) | 1983 (62.10) | 1588 (61.00) | ||
| Bad (n, %) | 478 (15.00) | 681 (26.20) | ||
| Very bad (n, %) | 75 (2.30) | 88 (3.40) | ||
| Healthcare expenditure | As a percentage (%) of annual household income (mean ± SD) | 0.91 ± 0.29 | 0.45 ± 0.40 | 0.048 |
| Variables | Self-Assessed Health | QOL | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| q10 | q50 | q90 | q10 | q50 | q90 | |||||||
| Coef. | p | Coef. | p | Coef. | p | Coef. | p | Coef. | p | Coef. | p | |
| Two-week access (ref. = No) | ||||||||||||
| Yes | 1.37 | 0.019 | 1.82 | 0.005 | 0.08 | 0.760 | −0.39 | 0.522 | 0.41 | 0.457 | 0.75 | 0.089 |
| One-year access (ref. = No) | ||||||||||||
| Yes | −0.95 | 0.274 | −0.44 | 0.332 | 0.09 | 0.739 | −0.25 | 0.785 | −0.58 | 0.197 | −1.11 | 0.052 |
| Access in need (ref. = No) | ||||||||||||
| Yes | 4.97 | 0.020 | 1.98 | 0.001 | 0.23 | 0.544 | 5.11 | <0.001 | 5.12 | <0.001 | 1.89 | 0.046 |
| Sex (ref. = Male) | ||||||||||||
| Female | 0.17 | 0.800 | −0.61 | 0.071 | 0.02 | 0.892 | 1.71 | 0.214 | 0.21 | 0.678 | 0.60 | 0.183 |
| Age | −0.36 | <0.001 | −0.24 | <0.001 | −0.11 | <0.001 | −0.03 | 0.470 | 0.01 | 0.821 | −0.01 | 0.914 |
| Marital status (ref. = Never married) | ||||||||||||
| Currently married | 6.40 | 0.008 | 5.02 | 0.032 | 4.97 | 0.044 | 6.54 | 0.112 | 3.82 | 0.235 | 4.09 | 0.391 |
| Cohabiting | 3.37 | 0.557 | 3.84 | 0.169 | 4.36 | 0.189 | −2.96 | 0.728 | −2.79 | 0.686 | −0.83 | 0.888 |
| Separated/ divorced | 2.07 | 0.463 | 2.32 | 0.339 | 2.29 | 0.365 | 3.50 | 0.477 | 0.98 | 0.803 | 2.95 | 0.580 |
| Widowed | 4.03 | 0.119 | 3.43 | 0.146 | 4.40 | 0.067 | 6.39 | 0.110 | 2.73 | 0.412 | 3.05 | 0.533 |
| Ethnicity (ref. = Han) | ||||||||||||
| Others | −5.49 | 0.095 | −2.84 | 0.003 | −0.09 | 0.858 | 4.48 | 0.148 | 0.322 | 0.792 | −2.11 | 0.055 |
| Education | 0.41 | <0.001 | 0.23 | <0.001 | 0.12 | <0.001 | 0.51 | <0.001 | 0.260 | <0.001 | 0.217 | <0.001 |
| Living arrangement (ref. = Moved from elsewhere) | ||||||||||||
| The same place | 2.91 | <0.001 | 1.16 | <0.001 | 0.24 | 0.256 | 2.29 | 0.026 | 1.34 | 0.004 | 0.99 | 0.046 |
| Work (ref. = Yes) | ||||||||||||
| No | −5.66 | 0.002 | −3.00 | <0.001 | −1.97 | 0.010 | −3.51 | 0.049 | −3.14 | 0.019 | −0.53 | 0.643 |
| Smoking (ref. = No) | ||||||||||||
| Yes | −0.38 | 0.691 | −0.19 | 0.699 | −0.07 | 0.769 | −0.34 | 0.647 | −1.22 | 0.039 | 0.48 | 0.446 |
| Drinking (ref. = No) | ||||||||||||
| Yes | 2.23 | 0.012 | 1.54 | <0.001 | 0.34 | 0.269 | 3.31 | <0.001 | 1.04 | 0..064 | 1.12 | 0.124 |
| Exercise (ref. = No) | ||||||||||||
| Yes | 3.46 | <0.001 | 1.67 | <0.001 | 0.58 | 0.020 | 2.47 | 0.001 | 1.62 | <0.001 | 0.39 | 0.307 |
| Household size | −0.13 | 0.516 | −0.37 | 0.010 | −0.25 | 0.012 | −0.16 | 0.460 | −0.54 | 0.001 | −0.10 | 0.402 |
| Social support (ref = No) | ||||||||||||
| Yes | −1.51 | 0.424 | −0.93 | 0.150 | 0.16 | 0.638 | −1.75 | 0.235 | −1.82 | 0.066 | −0.31 | 0.751 |
| Regular income (ref. = Regular) | ||||||||||||
| Regular but seasonal | −0.75 | 0.860 | 0.33 | 0.836 | −0.99 | 0.355 | 5.51 | 0.044 | 2.87 | 0.177 | 2.89 | 0.045 |
| No | −4.00 | 0.364 | −0.50 | 0.803 | −2.83 | <0.001 | −2.39 | 0.459 | −5.73 | 0.159 | −0.52 | 0.892 |
| Debt or loans (ref. = Yes) | ||||||||||||
| No | 3.00 | 0.086 | 0.83 | 0.349 | 1.05 | 0.138 | 1.64 | 0.412 | 0.24 | 0.726 | 0.09 | 0.935 |
| Financial situation (ref. = Very good) | ||||||||||||
| Good | −1.18 | 0.741 | −2.10 | 0.003 | 0.69 | 0.402 | −9.29 | <0.001 | −3.14 | <0.001 | −10.91 | <0.001 |
| Moderate | −2.76 | 0.411 | −2.38 | 0.001 | 0.14 | 0.865 | −13.85 | <0.001 | −6.05 | <0.001 | −12.87 | <0.001 |
| Bad | −5.80 | 0.093 | −4.49 | <0.001 | −0.98 | 0.262 | −23.26 | <0.001 | −14.67 | <0.001 | −15.51 | <0.001 |
| Very bad | −8.10 | 0.060 | −7.55 | <0.001 | −3.25 | 0.025 | −26.72 | <0.001 | −17.06 | <0.001 | −14.86 | <0.001 |
| Healthcare expenditure | −0.02 | 0.988 | −0.01 | 0.964 | −0.01 | 0.958 | −0.01 | 0.788 | −0.01 | 0.988 | −0.01 | 0.787 |
| Pseudo R2 | 0.15 | 0.13 | 0.07 | 0.17 | 0.12 | 0.05 | ||||||
| Variables | Self-Assessed Health | QOL | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| q10 | q50 | q90 | q10 | q50 | q90 | |||||||
| Coef. | p | Coef. | p | Coef. | p | Coef. | p | Coef. | p | Coef. | p | |
| Two-week access (ref. = No) | ||||||||||||
| Yes | −1.63 | 0.087 | 0.67 | 0.157 | 0.10 | 0.796 | −1.26 | 0.206 | 0.20 | 0.806 | 2.10 | 0.042 |
| One-year access (ref. = No) | ||||||||||||
| Yes | 1.74 | 0.097 | −0.08 | 0.878 | −0.19 | 0.635 | 1.44 | 0.032 | 0.05 | 0.927 | −1.45 | 0.360 |
| Access in need (ref. = No) | ||||||||||||
| Yes | 3.83 | 0.006 | 3.43 | <0.001 | 1.73 | 0.004 | 1.27 | 0.493 | 1.23 | 0.379 | 0.87 | 0.555 |
| Sex (ref. = Male) | ||||||||||||
| Female | −0.61 | 0.645 | −0.57 | 0.344 | −1.05 | 0.041 | −1.25 | 0.188 | 1.15 | 0.186 | 0.88 | 0.392 |
| Age | −0.52 | <0.001 | −0.26 | <0.001 | −0.13 | <0.001 | −0.21 | <0.001 | −0.13 | 0.002 | −0.04 | 0.355 |
| Marital status (ref. = Never married) | ||||||||||||
| Currently married | 18.45 | 0.013 | 8.59 | 0.016 | −3.00 | 0.543 | 3.61 | 0.564 | 6.38 | 0.023 | −0.65 | 0.909 |
| Cohabiting | 5.36 | 0.695 | 12.40 | 0.002 | −3.14 | 0.489 | 4.15 | 0.710 | 13.92 | 0.026 | 12.49 | 0.133 |
| Separated/divorced | 22.98 | 0.007 | 7.96 | 0.032 | −2.28 | 0.665 | 3.84 | 0.574 | 4.47 | 0.277 | −3.42 | 0.563 |
| Widowed | 18.03 | 0.020 | 8.24 | 0.025 | −3.25 | 0.513 | 3.71 | 0.562 | 5.71 | 0.058 | −1.32 | 0.821 |
| Ethnicity (ref. = Han) | ||||||||||||
| Others | 1.73 | 0.678 | 1.00 | 0.351 | 1.74 | 0.400 | 1.50 | 0.698 | 2.43 | 0.436 | −0.54 | 0.891 |
| Education | 0.21 | 0.061 | 0.13 | 0.037 | 0.07 | 0.114 | 0.16 | 0.123 | 0.29 | 0.007 | 0.39 | 0.006 |
| Living arrangement (ref. = Moved from elsewhere) | ||||||||||||
| The same place | 1.50 | 0.056 | 0.94 | 0.101 | 0.16 | 0.609 | −0.57 | 0.440 | −0.06 | 0.937 | 0.377 | 0.643 |
| Work (ref. = Yes) | ||||||||||||
| No | −5.17 | 0.004 | −3.57 | <0.001 | −0.75 | 0.096 | −3.51 | 0.034 | −5.25 | <0.001 | −0.92 | 0.431 |
| Smoking (ref. = No) | ||||||||||||
| Yes | 0.44 | 0.755 | 0.53 | 0.411 | −0.63 | 0.245 | −1.83 | 0.056 | 0.21 | 0.819 | −0.26 | 0.779 |
| Drinking (ref = No) | ||||||||||||
| Yes | 3.48 | <0.001 | 1.28 | 0.008 | 0.22 | 0.615 | 3.14 | 0.001 | 2.48 | 0.001 | 1.45 | 0.097 |
| Exercise (ref. = No) | ||||||||||||
| Yes | 3.95 | 0.003 | 0.85 | 0.285 | 0.67 | 0.319 | 4.41 | 0.002 | 3.34 | <0.001 | 1.61 | 0.244 |
| Household size | 0.59 | 0.134 | 0.61 | <0.001 | 0.32 | 0.011 | 0.19 | 0.413 | 0.42 | 0.067 | 0.64 | 0.019 |
| Social support (ref. = No) | ||||||||||||
| Yes | −1.53 | 0.134 | −2.54 | <0.001 | −1.36 | 0.004 | 0.60 | 0.544 | 0.64 | 0.347 | −0.37 | 0.665 |
| Regular income (ref. = Regular) | ||||||||||||
| Regular but seasonal | −0.54 | 0.660 | −0.40 | 0.376 | −0.48 | 0.205 | −2.49 | 0.001 | −1.21 | 0.084 | −2.15 | 0.005 |
| No | −4.19 | 0.041 | −2.41 | <0.001 | −1.09 | 0.010 | −4.70 | <0.001 | −2.41 | 0.018 | −2.69 | 0.012 |
| Debt or loans (ref. = Yes) | ||||||||||||
| No | 5.30 | <0.001 | 1.82 | <0.001 | 0.73 | 0.167 | 3.56 | 0.001 | 2.90 | 0.015 | 1.83 | 0.048 |
| Financial situation (ref. = Very good) | ||||||||||||
| Good | 0.60 | 0.901 | −0.98 | 0.469 | −0.60 | 0.691 | −4.91 | 0.488 | 0.65 | 0.855 | −9.26 | 0.170 |
| Moderate | −2.01 | 0.698 | −3.28 | 0.008 | −1.65 | 0.242 | −9.99 | 0.147 | −4.00 | 0.255 | −14.37 | 0.028 |
| Bad | −4.70 | 0.375 | −4.75 | <0.001 | −3.10 | 0.028 | −13.97 | 0.044 | −10.06 | 0.005 | −16.62 | 0.010 |
| Very bad | −9.90 | 0.059 | −9.52 | <0.001 | −3.33 | 0.019 | −21.66 | 0.004 | −15.86 | <0.001 | −21.70 | 0.002 |
| Healthcare expenditure | 0.05 | 0.832 | −0.03 | 0.408 | −0.04 | 0.151 | −0.02 | 0.813 | −0.08 | 0.285 | −0.17 | <0.001 |
| Pseudo R2 | 0.19 | 0.12 | 0.07 | 0.13 | 0.10 | 0.06 | ||||||
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhang, T.; Liu, C.; Ni, Z. Association of Access to Healthcare with Self-Assessed Health and Quality of Life among Old Adults with Chronic Disease in China: Urban Versus Rural Populations. Int. J. Environ. Res. Public Health 2019, 16, 2592. https://doi.org/10.3390/ijerph16142592
Zhang T, Liu C, Ni Z. Association of Access to Healthcare with Self-Assessed Health and Quality of Life among Old Adults with Chronic Disease in China: Urban Versus Rural Populations. International Journal of Environmental Research and Public Health. 2019; 16(14):2592. https://doi.org/10.3390/ijerph16142592
Chicago/Turabian StyleZhang, Tao, Chaojie Liu, and Ziling Ni. 2019. "Association of Access to Healthcare with Self-Assessed Health and Quality of Life among Old Adults with Chronic Disease in China: Urban Versus Rural Populations" International Journal of Environmental Research and Public Health 16, no. 14: 2592. https://doi.org/10.3390/ijerph16142592
APA StyleZhang, T., Liu, C., & Ni, Z. (2019). Association of Access to Healthcare with Self-Assessed Health and Quality of Life among Old Adults with Chronic Disease in China: Urban Versus Rural Populations. International Journal of Environmental Research and Public Health, 16(14), 2592. https://doi.org/10.3390/ijerph16142592






