The Association between Bisphenol A Exposure and Obesity in Children—A Systematic Review with Meta-Analysis
Abstract
1. Introduction
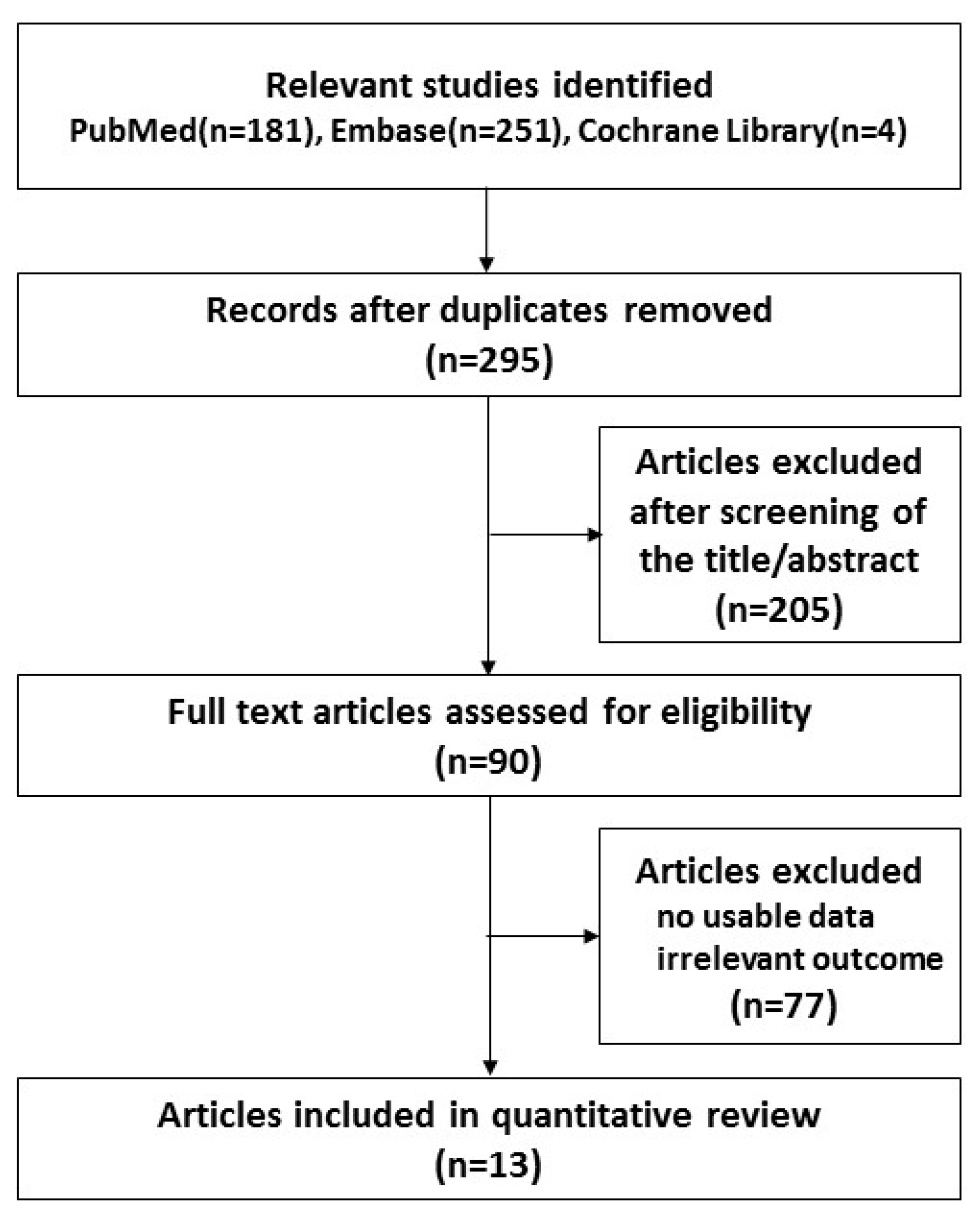
2. Materials and Methods
2.1. Literature Search
2.2. Selection Criteria
2.3. Data Extraction
2.4. Quality Evaluation
2.5. Data Analysis
3. Results
3.1. Characteristics of the Studies
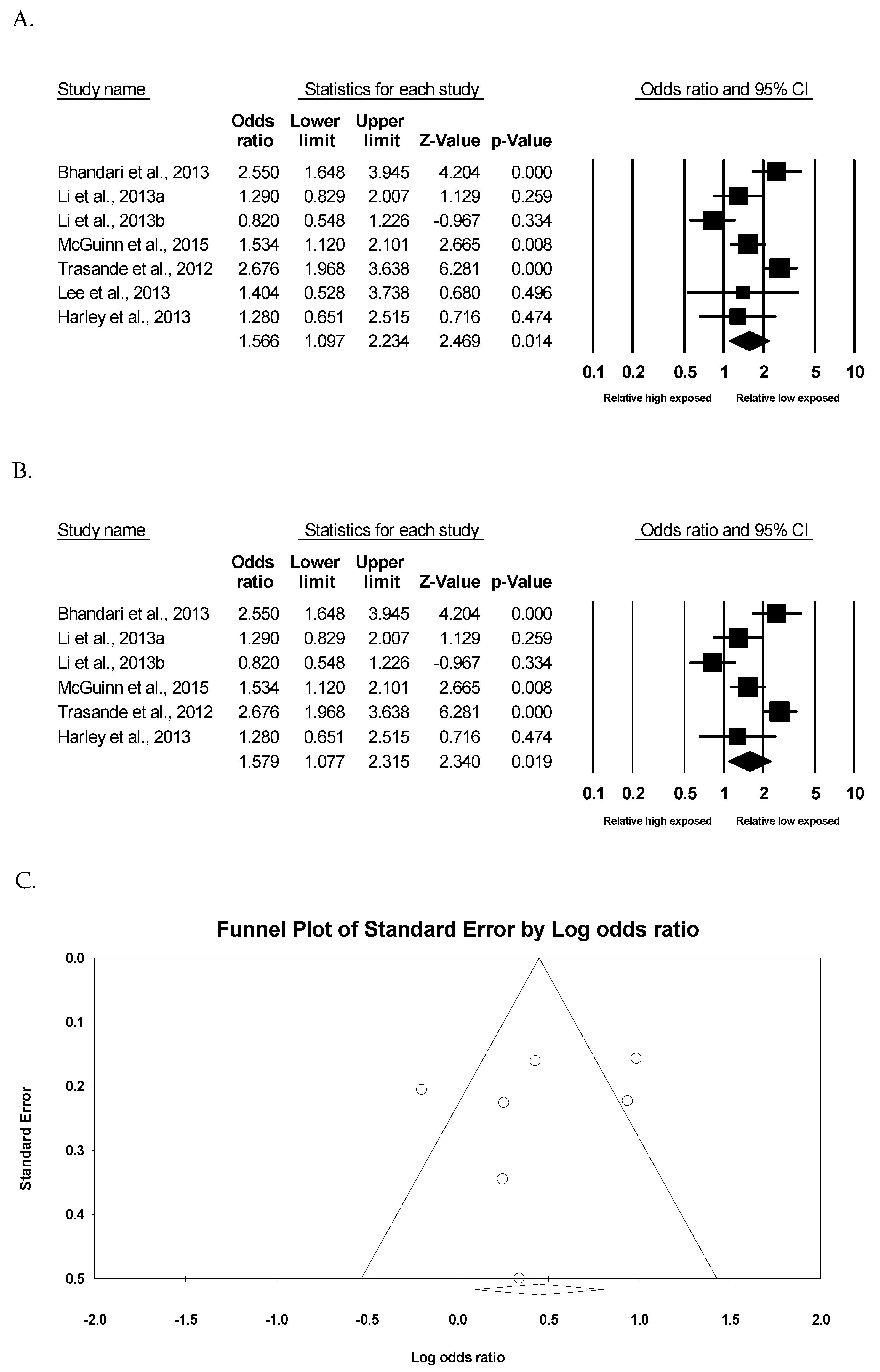
3.2. Meta-Analysis of Childhood Obesity by Exposure Groups
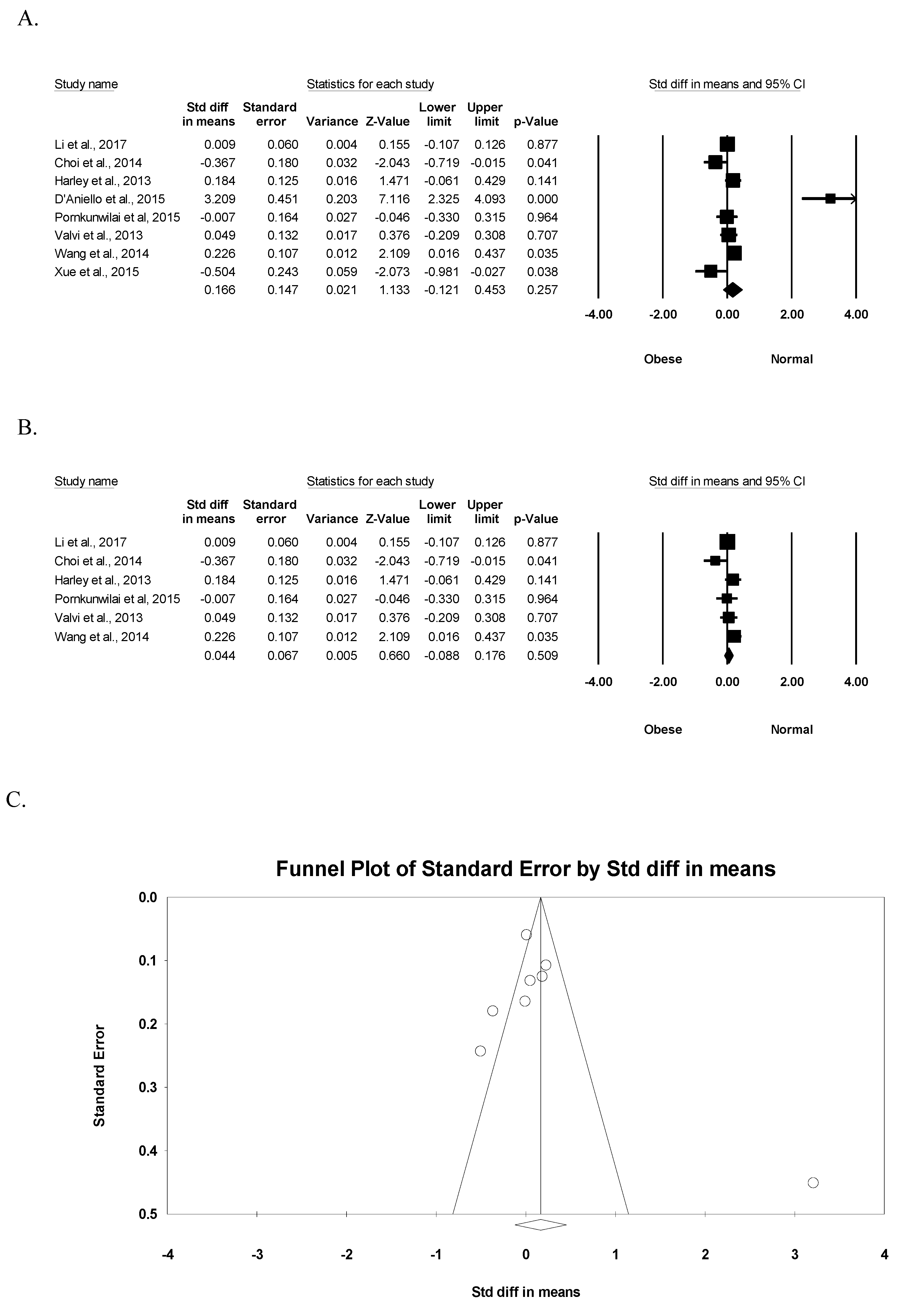
3.3. Meta-Analysis of BPA Exposure by Childhood Obesity
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Legeay, S.; Faure, S. Is bisphenol A an environmental obesogen? Fundam. Clin. Pharmacol. 2017, 31, 594–609. [Google Scholar] [CrossRef] [PubMed]
- Calafat, A.M.; Ye, X.; Wong, L.Y.; Reidy, J.A.; Needham, L.L. Exposure of the U.S. population to bisphenol A and 4-tertiary-octylphenol: 2003–2004. Environ. Health Perspect. 2008, 116, 39–44. [Google Scholar] [CrossRef] [PubMed]
- Huang, Y.Q.; Wong, C.K.; Zheng, J.S.; Bouwman, H.; Barra, R.; Wahlstrom, B.; Neretin, L.; Wong, M.H. Bisphenol A (BPA) in China: A review of sources, environmental levels, and potential human health impacts. Environ. Int. 2012, 42, 91–99. [Google Scholar] [CrossRef] [PubMed]
- Braun, J.M.; Kalkbrenner, A.E.; Calafat, A.M.; Yolton, K.; Ye, X.; Dietrich, K.N.; Lanphear, B.P. Impact of early-life bisphenol A exposure on behavior and executive function in children. Pediatrics 2011, 128, 873–882. [Google Scholar] [CrossRef] [PubMed]
- Menale, C.; Piccolo, M.T.; Cirillo, G.; Calogero, R.A.; Papparella, A.; Mita, L.; Del Giudice, E.M.; Diano, N.; Crispi, S.; Mita, D.G. Bisphenol A effects on gene expression in adipocytes from children: Association with metabolic disorders. J. Mol. Endocrinol. 2015, 54, 289–303. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Health Topics. Obesity. Available online: https://www.who.int/topics/obesity/en/ (accessed on 1 July 2019).
- Silventoinen, K.; Rokholm, B.; Kaprio, J.; Sorensen, T.I. The genetic and environmental influences on childhood obesity: A systematic review of twin and adoption studies. Int. J. Obes (Lond). 2010, 34, 29–40. [Google Scholar] [CrossRef] [PubMed]
- Amin, M.M.; Ebrahim, K.; Hashemi, M.; Shoshtari-Yeganeh, B.; Rafiei, N.; Mansourian, M.; Kelishadi, R. Association of exposure to Bisphenol A with obesity and cardiometabolic risk factors in children and adolescents. Int. J. Environ. Health Res. 2019, 29, 94–106. [Google Scholar] [CrossRef] [PubMed]
- Lee, E.Y.; Yoon, K.H. Epidemic obesity in children and adolescents: Risk factors and prevention. Front. Med. 2018, 12, 658–666. [Google Scholar] [CrossRef] [PubMed]
- Simmonds, M.; Llewellyn, A.; Owen, C.G.; Woolacott, N. Predicting adult obesity from childhood obesity: A systematic review and meta-analysis. Obes. Rev. 2016, 17, 95–107. [Google Scholar] [CrossRef] [PubMed]
- Llewellyn, A.; Simmonds, M.; Owen, C.G.; Woolacott, N. Childhood obesity as a predictor of morbidity in adulthood: A systematic review and meta-analysis. Obes. Rev. 2016, 17, 56–67. [Google Scholar] [CrossRef] [PubMed]
- Vafeiadi, M.; Roumeliotaki, T.; Myridakis, A.; Chalkiadaki, G.; Fthenou, E.; Dermitzaki, E.; Karachaliou, M.; Sarri, K.; Vassilaki, M.; Stephanou, E.G.; et al. Association of early life exposure to bisphenol A with obesity and cardiometabolic traits in childhood. Environ. Res. 2016, 146, 379–387. [Google Scholar] [CrossRef] [PubMed]
- Vom Saal, F.S.; Nagel, S.C.; Coe, B.L.; Angle, B.M.; Taylor, J.A. The estrogenic endocrine disrupting chemical bisphenol A (BPA) and obesity. Mol. Cell. Endocrinol. 2012, 354, 74–84. [Google Scholar] [CrossRef] [PubMed]
- D’Aniello, R.; Troisi, J.; D’Amico, O.; Sangermano, M.; Massa, G.; Moccaldo, A.; Pierri, L.; Poeta, M.; Vajro, P. Emerging pathomechanisms involved in obesity. J. Pediatr. Gastroenterol. Nutr. 2015, 60, 113–119. [Google Scholar] [CrossRef] [PubMed]
- Wang, B.; Wang, H.; Zhou, W.; He, Y.; Zhou, Y.; Chen, Y.; Jiang, Q. Exposure to bisphenol A among school children in eastern China: A multicenter cross-sectional study. J. Expo. Sci. Environ. Epidemiol. 2014, 24, 657–664. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Lai, H.; Chen, S.; Zhu, H.; Lai, S. Gender differences in the associations between urinary bisphenol A and body composition among American children: The National Health and Nutrition Examination Survey, 2003–2006. J. Epidemiol. 2017, 27, 228–234. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; Group, P. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. J. Clin. Epidemiol. 2009, 62, 1006–1012. [Google Scholar] [CrossRef]
- Wells, G.; Shea, B.; O’connell, D.; Peterson, J.; Welch, V.; Losos, M. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analysis. Ott. Ott. Health Res. Inst. 2010, 25, 603–605. [Google Scholar]
- Pornkunwilai, S.; Nosoongnoen, W.; Jantarat, C.; Wachrasindhu, S.; Supornsilchai, V. Urinary bisphenol A detection is significantly associated with young and obese Thai children. Asian Biomed. 2015, 9, 363–372. [Google Scholar]
- Wang, J.; Sun, B.; Hou, M.; Pan, X.; Li, X. The environmental obesogen bisphenol A promotes adipogenesis by increasing the amount of 11beta-hydroxysteroid dehydrogenase type 1 in the adipose tissue of children. Int. J. Obes (Lond). 2013, 37, 999–1005. [Google Scholar] [CrossRef]
- Whitehead, J.P.; Richards, A.A.; Hickman, I.J.; Macdonald, G.A.; Prins, J.B. AdiponectinA key adipokine in the metabolic syndrome. Diabetes Obes. Metab. 2006, 8, 264–280. [Google Scholar] [CrossRef]
- Ariemma, F.; D’Esposito, V.; Liguoro, D.; Oriente, F.; Cabaro, S.; Liotti, A.; Cimmino, I.; Longo, M.; Beguinot, F.; Formisano, P.; et al. Low-Dose Bisphenol-A Impairs Adipogenesis and Generates Dysfunctional 3T3-L1 Adipocytes. PLoS ONE 2016, 11, e0150762. [Google Scholar] [CrossRef] [PubMed]
- Vandenberg, L.N.; Chahoud, I.; Heindel, J.J.; Padmanabhan, V.; Paumgartten, F.J.; Schoenfelder, G. Urinary, circulating, and tissue biomonitoring studies indicate widespread exposure to bisphenol A. Environ. Health Perspect. 2010, 118, 1055–1070. [Google Scholar] [CrossRef] [PubMed]
- Tuduri, E.; Marroqui, L.; Dos Santos, R.S.; Quesada, I.; Fuentes, E.; Alonso-Magdalena, P. Timing of Exposure and Bisphenol-A: Implications for Diabetes Development. Front. Endocrinol. 2018, 9, 648. [Google Scholar] [CrossRef] [PubMed]
- Li, D.K.; Miao, M.; Zhou, Z.; Wu, C.; Shi, H.; Liu, X.; Wang, S.; Yuan, W. Urine bisphenol-A level in relation to obesity and overweight in school-age children. PLoS ONE 2013, 8, e65399. [Google Scholar] [CrossRef] [PubMed]
- Bhandari, R.; Xiao, J.; Shankar, A. Urinary bisphenol A and obesity in U.S. children. Am. J. Epidemiol. 2013, 177, 1263–1270. [Google Scholar] [CrossRef] [PubMed]
- Harley, K.G.; Aguilar Schall, R.; Chevrier, J.; Tyler, K.; Aguirre, H.; Bradman, A.; Holland, N.T.; Lustig, R.H.; Calafat, A.M.; Eskenazi, B. Prenatal and postnatal bisphenol A exposure and body mass index in childhood in the CHAMACOS cohort. Environ. Health Perspect. 2013, 121, 514–520. [Google Scholar] [CrossRef]
- Lee, H.A.; Kim, Y.J.; Lee, H.; Gwak, H.S.; Park, E.A.; Cho, S.J.; Kim, H.S.; Ha, E.H.; Park, H. Effect of urinary bisphenolA on androgenic hormones and insulin resistance in preadolescent girls: A pilot study from the Ewha Birth & Growth Cohort. Int. J. Environ. Res. Public Health 2013, 10, 5737–5749. [Google Scholar]
- McGuinn, L.A.; Ghazarian, A.A.; Joseph Su, L.; Ellison, G.L. Urinary bisphenol A and age at menarche among adolescent girls: Evidence from NHANES 2003–2010. Environ. Res. 2015, 136, 381–386. [Google Scholar] [CrossRef]
- Trasande, L.; Attina, T.M.; Blustein, J. Association between urinary bisphenol A concentration and obesity prevalence in children and adolescents. JAMA 2012, 308, 1113–1121. [Google Scholar] [CrossRef]
- Xue, J.; Wu, Q.; Sakthivel, S.; Pavithran, P.V.; Vasukutty, J.R.; Kannan, K. Urinary levels of endocrine-disrupting chemicals, including bisphenols, bisphenol A diglycidyl ethers, benzophenones, parabens, and triclosan in obese and non-obese Indian children. Environ. Res. 2015, 137, 120–128. [Google Scholar] [CrossRef]
- Choi, J.; Eom, J.; Kim, J.; Lee, S.; Kim, Y. Association between some endocrine-disrupting chemicals and childhood obesity in biological samples of young girls: A cross-sectional study. Environ. Toxicol. Pharmacol. 2014, 38, 51–57. [Google Scholar] [CrossRef] [PubMed]
- Valvi, D.; Casas, M.; Mendez, M.A.; Ballesteros-Gomez, A.; Luque, N.; Rubio, S.; Sunyer, J.; Vrijheid, M. Prenatal bisphenol a urine concentrations and early rapid growth and overweight risk in the offspring. Epidemiology 2013, 24, 791–799. [Google Scholar] [CrossRef] [PubMed]
| Study | Study Type | Participants | Location | Age | Outcome | Quality * |
|---|---|---|---|---|---|---|
| Bhandari et al., 2013 [26] | Cross-sectional | 2200 | USA | 6–18 y | Positive association was observed between BPA levels and obesity, independent of age, sex, race/ethnicity, education, physical activity, serum cotinine, and urinary creatinine. | 9 |
| Lee et al., 2013 [28] | Cohort (pilot study) | 80 | Korea | 7–8 y | BPA exposure affected hormone level such as estradiol, androstenedione, testosterone, insulin, and homeostasis model assessment of insulin resistance index. | 7 |
| Li et al., 2013 [25] | Cross-sectional | 1326 | China | 9–12 y | A higher urine BPA level (≥2 µg/L) increased 2-fold more in the risk of obesity. | 9 |
| McGuinn et al., 2015 [29] | Cross-sectional | 987 | USA | 12–19 y | BPA was associated with early onset of menarche and the association was modulated by obesity status. | 9 |
| Trasande et al., 2012 [30] | Cross-sectional | 2838 | USA | 6–19 y | Urinary BPA concentration was significantly associated with obesity in children and adolescents. | 9 |
| Harley et al., 2013 [27] | Cohort | 311 | USA | 5–9 y | Urinary BPA concentration at 5 years was not associated with BMI, but BPA concentration at 9 years was positively associated with BMI. | 8 |
| D’Aniello et al., 2015 [14] | Case-control (pilot study) | 54 | Italy | 5–16 y | Free and total BPA levels were associated with the increase in BMI and conjugated BPA was related to the decrease in BMI. | 6 |
| Li et al., 2017 [16] | Cross-sectional | 1860 | USA | 8–19 y | Higher BPA levels were related to elevated lean body mass in boys, but not in girls, while higher BPA was associated with increased fat mass in girls, but not in boys. | 9 |
| Xue et al., 2015 [31] | Case-control (pilot study) | 76 | India | 2–14 y | Target chemicals including BPA had no significant association with childhood obesity. | 7 |
| Choi et al., 2014 [32] | Cross-sectional | 127 | Korea | 6–14 y | BPA had no significant association with childhood obesity. | 8 |
| Wang et al., 2014 [15] | Cross-sectional | 666 | China | 9–12 y | BPA level was not associated with age, and there was no significant association between BPA level and obesity. | 9 |
| Pornkunwilai et al., 2015 [19] | Cross-sectional | 376 | Thailand | 3–18 y | BPA detection was significantly associated with obesity, but not with other demographic data or BPA exposure risks. | 9 |
| Valvi et al., 2013 [33] | Cohort | 402 | Spain | 14 m–4 y | BPA exposure was weakly associated with obesity at 4 years. | 7 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, K.Y.; Lee, E.; Kim, Y. The Association between Bisphenol A Exposure and Obesity in Children—A Systematic Review with Meta-Analysis. Int. J. Environ. Res. Public Health 2019, 16, 2521. https://doi.org/10.3390/ijerph16142521
Kim KY, Lee E, Kim Y. The Association between Bisphenol A Exposure and Obesity in Children—A Systematic Review with Meta-Analysis. International Journal of Environmental Research and Public Health. 2019; 16(14):2521. https://doi.org/10.3390/ijerph16142521
Chicago/Turabian StyleKim, Ka Young, Eunil Lee, and Yanghee Kim. 2019. "The Association between Bisphenol A Exposure and Obesity in Children—A Systematic Review with Meta-Analysis" International Journal of Environmental Research and Public Health 16, no. 14: 2521. https://doi.org/10.3390/ijerph16142521
APA StyleKim, K. Y., Lee, E., & Kim, Y. (2019). The Association between Bisphenol A Exposure and Obesity in Children—A Systematic Review with Meta-Analysis. International Journal of Environmental Research and Public Health, 16(14), 2521. https://doi.org/10.3390/ijerph16142521





