Evaluation of the Biases in the Studies that Assess the Effects of the Great Recession on Health. A Systematic Review
Abstract
1. Introduction
2. Materials and Methods
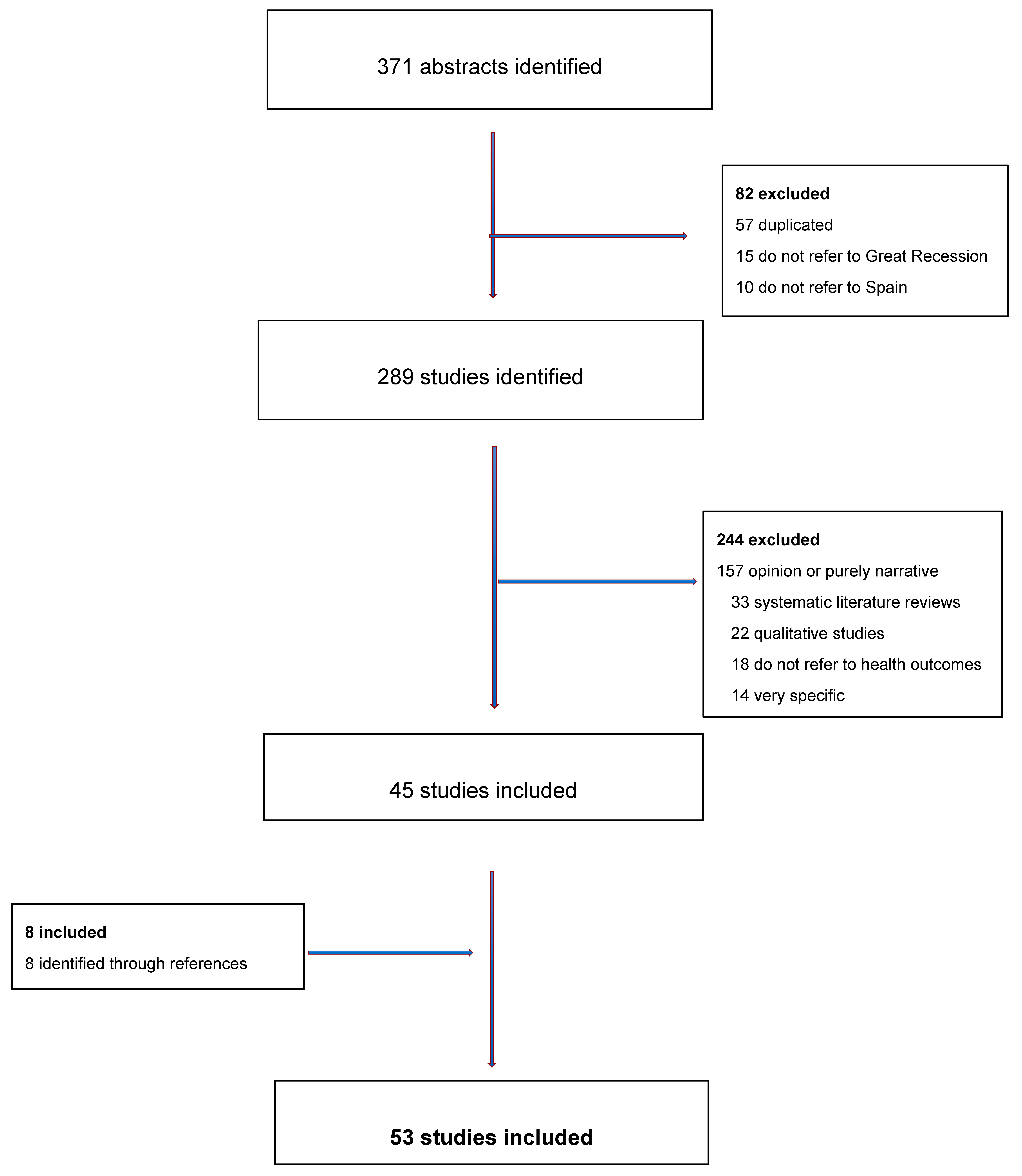
2.1. Systematic Review
2.2. Evaluation of Biases
3. Results
3.1. Systematic Review
3.2. Risk Assessment
3.3. Evaluation Problem
3.4. Time Bias
3.5. Other Biases
4. Discussion
5. Conclusions
Key points
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Data sharing statement
References
- International Monetary Fund (IMF). World Economic Outlook—April 2009: Crisis and Recovery; IMF: Washington DC, USA, 2009; Available online: http://www.imf.org/external/pubs/ft/weo/2009/01/pdf/text.pdf (accessed on 10 July 2019).
- Parmar, D.; Stavropoulou, C.; Ioannidis, J.P. Health outcomes during the 2008 financial crisis in Europe: Systematic literature review. BMJ 2016, 354, i4588. [Google Scholar] [CrossRef]
- Organisation for Economic Co-Operation and Development. OECD. Quarterly National Accounts. Quarterly Growth Rates of Real GDP, Change over Previous Quarter. Available online: http://stats.oecd.org/Index.aspx?QueryName=350&QueryType=View&Lang=en (accessed on 3 February 2018).
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef]
- Mullahy, J.; Manning, W. Statistical issues in cost-effectiveness analysis. In Valuing Health Care; Sloan, F.A., Ed.; Cambridge University Press: Cambridge, UK, 1996; pp. 149–184. [Google Scholar]
- Aguilar-Palacio, I.; Carrera-Lasfuentes, P.; Rabanaque, M.J. Youth unemployment and economic recession in Spain: Influence on health and lifestyles in young people (16–24 years old). Int. J. Public Health 2015, 60, 427–435. [Google Scholar] [CrossRef]
- Arroyo-Borrell, E.; Renart, G.; Saurina, C.; Saez, M. Influence maternal background has on children’s mental health. Int. J. Equity Health 2017, 16, 63. [Google Scholar] [CrossRef]
- Bacigalupe, A.; Shahidi, F.V.; Muntaner, C.; Martín, U.; Borrell, C. Why is there so much controversy regarding the population health impact of the Great Recession? Reflections on three case studies. Int. J. Health Serv. 2016, 46, 5–35. [Google Scholar] [CrossRef]
- Barceló, M.A.; Coll-Negre, M.; Coll-de-Tuero, G.; Saez, M. Effects of the financial crisis on psychotropic drug consumption in a cohort from a semi-urban region in Catalonia, Spain. PLoS ONE 2016, 11, e0148594. [Google Scholar] [CrossRef]
- Bartoll, X.; Pale, L.; Malmusi, D.; Suhrcke, M.; Borrell, C. The evolution of mental health in Spain during the economic crisis. Eur. J. Public Health 2014, 24, 415–418. [Google Scholar] [CrossRef]
- Basterra, V. Prevalence trends of high risk of mental disorders in the Spanish adult population: 2006–2012. Gac. Sanit. 2017, 31, 324–326. (In Spanish) [Google Scholar] [CrossRef]
- Córdoba-Doña, J.A.; Escolar-Pujolar, A.; San Sebastián, M.; Gustafsson, P.E. How are the employed and unemployed affected by the economic crisis in Spain? Educational inequalities, life conditions and mental health in a context of high unemployment. BMC Public Health 2016, 16, 267. [Google Scholar] [CrossRef]
- Fernández-García, M.A.; Olry-de-Labry-Lima, A.; Ferrer-López, I.; Bermúdez-Tamayo, C. Analysis of changes in trends in the consumption rates of benzodiazepines and benzodiazepine-related drugs. J. Pharm. Policy Pract. 2018, 11, 1. [Google Scholar] [CrossRef]
- Gili, M.; Roca, M.; Basu, S.; McKee, M.; Stuckler, D. The mental health risks of economic crisis in Spain: Evidence from primary care centres, 2006 and 2010. Eur. J. Public Health. 2013, 23, 103–108. [Google Scholar] [CrossRef]
- Gili, M.; García-Campayo, J.; Roca, M. Economic crisis and mental health. SESPAS Report. Gac. Sanit. 2014, 28, 104–108. (In Spanish) [Google Scholar] [CrossRef]
- Gili, M.; López-Navarro, E.; Castro, A.; Homar, C.; Navarro, C.; García-Toro, M.; García-Campayo, J.; Roca, M. Gender differences in mental health during the economic crisis. Psicothema 2016, 28, 407–413. [Google Scholar]
- Gotsens, M.; Malmusi, D.; Villarroel, N.; Vives-Cases, C.; García-Subirats, I.; Hernando, C.; Borrell, C. Health inequality between immigrants and natives in Spain: The loss of the healthy immigrant effect in times of economic crisis. Eur. J. Public Health 2015, 25, 923–929. [Google Scholar] [CrossRef]
- Iglesias-García, C.; Sáiz-Martínez, P.; García-Portilla, M.P.; Bousoño-García, M.; Jiménez-Treviño, L.; Sánchez-Lasheras, F.; Bobes, J. Effects of the economic crisis on demand due to mental disorders in Asturias: Data from the Asturias Cumulative Psychiatric Case Register (2000–2010). Actas Esp. Psiquiatr. 2014, 42, 108–115. [Google Scholar]
- Medel-Herrero, A.; Gómez-Beneyto, M. The impact of the 2008 economic crisis on the increasing number of psychiatric inpatients. Rev. Psiquiatr. Salud. Ment. 2017, 12, 28–36. [Google Scholar] [CrossRef]
- Navarro-Mateu, F.; Tormo, M.J.; Salmerón, D.; Vilagut, G.; Navarro, C.; Ruíz-Merino, G.; Escámez, T.; Júdez, J.; Martínez, S.; Kessler, R.C.; et al. Prevalence of mental disorders in the South-East of Spain, one of the European regions most affected by the economic crisis: The cross-sectional PEGASUS-Murcia Project. PLoS ONE 2015, 10, e0137293. [Google Scholar] [CrossRef]
- Pérez-Romero, S.; Gascón-Cánovas, J.J.; de la Cruz-Sánchez, E.; Sánchez-Ruíz, J.F.; Parra-Hidalgo, P.; Monteagudo-Piqueras, O. Economic recession (2006–2012) and changes in the health status of the Spanish population. Salud. Publica Mex. 2016, 58, 41–48. (In Spanish) [Google Scholar] [CrossRef][Green Version]
- Rajmil, L.; Medina-Bustos, A.; Fernández de Sanmamed, M.J.; Mompart-Penina, A. Impact of the economic crisis on children’s health in Catalonia: A before-after approach. BMJ Open 2013, 3, e003286. [Google Scholar] [CrossRef]
- Rajmil, L.; Siddigi, A.; Taylor-Robinson, D.; Spencer, N. Understanding the impact of the economic crisis on child health: The case of Spain. Int. J. Equity Health 2015, 14, 95. [Google Scholar] [CrossRef]
- Robert, G.; Martínez, J.M.; García, A.M.; Benavides, F.G.; Ronda, E. From the boom to the crisis: Changes in employment conditions of immigrants in Spain and their effects on mental health. Eur. J. Public Health 2014, 24, 404–409. [Google Scholar] [CrossRef]
- Ruíz-Pérez, I.; Rodríguez-Barranco, M.; Rojas-García, A.; Mendoza-García, O. Economic crisis and suicides in Spain. Socio-demographic and regional variability. Eur. J. Health Econ. 2017, 18, 313–320. [Google Scholar] [CrossRef]
- Sicras-Mainar, A.; Navarro-Artieda, R. Use of antidepressants in the treatment of major depressive disorder in primary care during a period of economic crisis. Neuropsychiatr. Dis. Treat. 2015, 12, 29–40. [Google Scholar] [CrossRef][Green Version]
- Utzet, M.; Navarro, A.; Llorens, C.; Muntaner, C.; Moncada, S. Is the worsening of psychosocial exposures associated with mental health? Comparing two population-based cross-sectional studies in Spain, 2005. Am. J. Ind. Med. 2016, 59, 399–407. [Google Scholar] [CrossRef]
- Zapata-Moya, A.R.; Buffel, V.; Navarro-Yáñez, C.J.; Bracke, P. Social inequality in morbidity, framed within the current economic crisis in Spain. Int. J. Equity Health 2015, 14, 131. [Google Scholar] [CrossRef]
- Arroyo-Borrell, E.; Renart, G.; Saez, M. How the economic recession has changed the likelihood of reporting por self-rated health in Spain. Int. J. Equity Health 2015, 14, 149. [Google Scholar] [CrossRef]
- Barroso, C.; Abásolo, I.; Cáceres, J.J. Health inequalities by socioeconomic characteristics in Spain: The economic crisis effect. Int. J. Equity Health. 2016, 15, 62. [Google Scholar] [CrossRef]
- Bartoll, X.; Toffolutti, V.; Malmusi, D.; Palència, L.; Borrell, C.; Suhrcke, M. Health and health behaviours before and during the Great Recession, overall and by socioeconomic status, using data from four repeated cross-sectional health surveys in Spain (2001–2012). BMC Public Health 2015, 15, 865. [Google Scholar] [CrossRef]
- Calzón-Fernández, S.; Fernández-Ajuria, A.; López-del-Amo-González, M.P.; Martín-Martín, J.J. Sex differences of perceived health before and during the economic crisis (2007 and 2011). Spain. Rev. Esp. Salud Publica 2017, 16, 91. (In Spanish) [Google Scholar]
- Fornell, B.; Correa, M.; López del Amo, M.P.; Martín, J.J. Influence of changes in the Spanish labor market during the economic crisis (2007–2011) on perceived health. Qual. Life Res. 2018, 27, 2095–2105. [Google Scholar] [CrossRef]
- López-del-Amo, M.P.; Benítez, V.; Martín-Martín, J.J. Long term unemployment, income, poverty, and social public expenditure, and their relationship with self-perceived health in Spain (2007–2011). BMC Public Health 2018, 18, 133. [Google Scholar] [CrossRef]
- Regidor, E.; Barrio, G.; Bravo, M.J.; de la Fuente, L. Has health in Spain been declining since the economic crisis? J. Epidemiol. Community Health 2014, 68, 280–282. [Google Scholar] [CrossRef]
- Urbanos-Garrido, R.M.; López-Valcárcel, B.G. The influence of the economic crisis on the association between unemployment and health: An empirical analysis for Spain. Eur. J. Health Econ. 2015, 16, 175–184. [Google Scholar] [CrossRef]
- Vásquez-Vera, H.; Rodríguez-Sanz, M.; Palència, L.; Borrell, C. Foreclosure and health in Southern Europe: Results from the platform for people affected by mortgages. J. Urban. Health 2016, 93, 312–330. [Google Scholar] [CrossRef]
- Álvarez-Gálvez, J.; Salinas-Pérez, J.A.; Rodero-Cosano, M.L.; Salvador-Carulla, L. Methodological barriers to studying the association between the economic crisis and suicide in Spain. BMC Public Health 2017, 17, 694. [Google Scholar] [CrossRef]
- Borrell, C.; Marí-Dell’Olmo, M.; Gotsens, M.; Calvo, M.; Rodríguez-Sanz, M.; Bartoll, X.; Esnaola, S. Socioeconomic inequalities in suicide mortality before and after the economic recession in Spain. BMC Public Health 2017, 17, 772. [Google Scholar] [CrossRef]
- Córdoba-Doña, J.A.; San Sebastián, M.; Escolar-Pujolar, A.; Martínez-Faure, J.E.; Gustafsson, P.E. Economic crisis and suicidal behaviour: The role of unemployment, sex and age in Andalusia, southern Spain. Int. J. Equity Health. 2014, 13, 55. [Google Scholar] [CrossRef]
- López-Bernal, J.A.; Gasparrini, A.; Artundo, C.M.; McKee, M. The effect of the late 2000s financial crisis on suicides in Spain: An interrupted time-series analysis. Eur. J. Public Health. 2013, 23, 732–736. [Google Scholar] [CrossRef]
- Miret, M.; Caballero, F.F.; Huerta-Ramírez, R.; Moneta, M.V.; Olaya, B.; Chatterji, S.; Haro, J.M.; Ayuso-Mateos, J.L. Factors associated with suicidal ideation and attempts in Spain for different age groups. Prevalence before and after the onset of the economic crisis. J. Affect. Disord. 2014, 163, 1–9. [Google Scholar] [CrossRef]
- Rivera, B.; Casal, B.; Currais, L. Crisis, suicide and labour productivity losses in Spain. Eur. J. Health Econ. 2017, 18, 83–96. [Google Scholar] [CrossRef]
- Saurina, C.; Marzo, M.; Saez, M. Inequalities in suicide mortality rates and the economic recession in the municipalities of Catalonia, Spain. Int. J. Equity Health. 2015, 14, 75. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Alonso, I.; Vallejo, F.; Regidor, E.; Belza, M.J.; Sordo, L.; Otero-García, L.; Barrio, G. Changes in directly alcohol-attributable mortality during the great recession by employment status in Spain: A population cohort of 22 million people. J. Epidemiol. Community Health 2017, 71, 736–744. [Google Scholar] [CrossRef] [PubMed]
- Benmarhnia, T.; Zunzunegui, M.V.; Llàcer, A.; Béland, F. Impact of the economic crisis on the health of older persons in Spain: Research clues based on an analysis of mortality. SESPAS Report. Gac. Sanit. 2014, 28 (Suppl. S1), 137–141. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Ferrando, J.; Palència, L.; Gotsens, M.; Puig-Barrachina, V.; Marí-Dell’Olmo, M.; Rodríguez-Sanz, M.; Bartoll, X.; Borrell, C. Trends in cancer mortality in Spain: The influence of the financial crisis. Gac. Sanit. 2018, 33, 229–234. [Google Scholar] [CrossRef] [PubMed]
- Llàcer, A.; Fernández-Cuenca, R.; Martínez-Navarro, F. Economic crisis and communicable diseases. SESPAS Report 2014. Gac Sanit. 2014, 28 (Suppl. S1), 97–103. (In Spanish) [Google Scholar] [CrossRef][Green Version]
- Maynou, L.; Saez, M.; López-Casasnovas, G. Has the economic crisis widened the intraurban socioeconomic inequalities in mortality? The case of Barcelona, Spain. J. Epidemiol. Community Health 2016, 70, 114–124. [Google Scholar] [CrossRef]
- Regidor, E.; Vallejo, F.; Granados, J.A.T.; Viciana-Fernández, F.J.; de la Fuente, L.; Barrio, G. Mortality decrease according to socioeconomic groups during the economic crisis in Spain: A cohort study of 36 million people. Lancet 2016, 388, 2642–2652. [Google Scholar] [CrossRef]
- Ruíz-Ramos, M.; Córdoba-Donña, J.A.; Bacigalupe, A.; Juárez, S.; Escolar-Pujolar, A. The economic crisis at the beginning of the XXI century and mortality in Spain. Trend and impact on social inequalities. SESPAS Report 2014. Gac Sanit. 2014, 28 (Suppl. S1), 89–96. (In Spanish) [Google Scholar] [CrossRef]
- Bosque-Prous, M.; Kunst, A.E.; Brugal, M.T.; Espelt, A. Changes in alcohol consumption in the 50- to 64-year-old European economically active population during an economic crisis. Eur. J. Public Health 2017, 27, 711–716. [Google Scholar] [CrossRef]
- Collell, E.; Sánchez-Niubò, A.; Delclós, G.L.; Benavides, F.G.; Domingo-Salvany, A. Economic crisis and changes in drug use in the Spanish economically active population. Addiction 2015, 110, 1129–1137. [Google Scholar] [CrossRef]
- Martin-Bassols, N.; Vall-Castelló, J. Effects of the great recession on drugs consumption in Spain. Econ. Hum. Biol. 2016, 22, 103–116. [Google Scholar] [CrossRef] [PubMed]
- Abásolo, I.; Saez, M.; López-Casasnovas, G. Financial crisis and income-related inequalities in the universal provision of a public service: The case of healthcare in Spain. Int. J. Equity Health. 2017, 16, 134. [Google Scholar] [CrossRef]
- Coveney, M.; García-Gómez, P.; Van Doorslaer, E.; Van Ourti, T. Health disparities by income in Spain before and after the economic crisis. Health Econ. 2016, 25 (Suppl. 2), 141–158. [Google Scholar] [CrossRef] [PubMed]
- Córdoba-Doña, J.A.; Escolar-Pujolar, A.; San Sebastián, M.; Gustafsson, P.E. Withstanding austerity: Equity in health services utilisation in the first stage of the economic recession in Southern Spain. PLoS ONE 2018, 13, e0195293. [Google Scholar] [CrossRef] [PubMed]
- García-Subirats, I.; Vargas, I.; Sanz, B.; Malmusi, D.; Ronda, E.; Ballesta, M.; Luisa Vázquez, M. Changes in access to health services of the immigrant and native-born population in Spain in the context of economic crisis. Int. J. Environ. Res. Public Health. 2014, 11, 10182–10201. [Google Scholar] [CrossRef]
- Lostao, L.; Geyer, S.; Albaladejo, R.; Moreno-Lostao, A.; Santos, J.M.; Regidor, E. Socioeconomic position and health services use in Germany and Spain during the Great Recession. PLoS ONE 2017, 12, e0183325. [Google Scholar] [CrossRef] [PubMed]
- Calzón-Fernández, S.; Fernández-Ajuría, A.; Martín, J.J.; Murphy, M.J. The impact of the economic crisis on unmet dental care needs in Spain. J. Epidemiol. Community Health. 2015, 69, 880–885. [Google Scholar] [CrossRef]
- Fernández, A.; García-Alonso, J.; Royo-Pastor, C.; Garrell-Corbera, I.; Rengel-Chica, J.; Agudo-Ugena, J.; Ramos, A.; Mendive, J. Effects of the economic crisis and social support on health-related quality of life: First wave of a longitudinal study in Spain. Br. J. Gen. Pract. 2015, 65, e198–e203. [Google Scholar] [CrossRef]
- Larrañaga, I.; Martín, U.; Bacigalupe, A. Sexual and reproductive health and the economic crisis in Spain. SESPAS report Gac Sanit. 2014, 28 (Suppl. S1), 109–115. [Google Scholar] [CrossRef]
- Lorenzo-Carrascosa, L. The health of the elderly in Spain during the economic crisis. Rev. Esp. Geriatr. Gerontol. 2016, 53, 12–14. (In Spanish) [Google Scholar] [CrossRef]
- Palència, L.; Puig-Barrachina, V.; Marí-Dell’Olmo, M.; Gotsens, M.; Rodríguez-Sanz, M.; Bartoll, X.; Pérez, G.; IMCRISES members. Trends in small-for-gestational age before and after the economic crisis in Spain. Eur. J. Public Health 2018, 28, 325–327. [Google Scholar] [CrossRef]
- Varea, C.; Terán, J.M.; Bernís, B.; Bogin, B.; González-González, A. Is the economic crisis affecting birth outcome in Spain? Evaluation of temporal trend in underweight at birth (2003–2012). Ann. Hum. Biol. 2016, 43, 169–182. [Google Scholar] [CrossRef] [PubMed]
- Baumbach, A.; Gulis, G. Impact of financial crisis on selected health outcomes in Europe. Eur. J. Public Health 2014, 24, 399–403. [Google Scholar] [CrossRef] [PubMed]
- Lostao, L.; Geyer, S.; Albadalejo, R.; Moreno-Lostao, A.; Ronda, E.; Regidor, E. Use of health services according to income before and after the elimination of copayment in Germany and restriction of universal health coverage in Spain. Int. J. Equity Health 2018, 17, 11. [Google Scholar] [CrossRef] [PubMed]
- Palladino, R.; Lee, J.T.; Hone, T.; Filippidis, F.T.; Millett, C. The Great Recession and increased cost sharing in European Health Systems. Health Aff. (Millwood) 2016, 35, 1204–1213. [Google Scholar] [CrossRef]
| Bias Domain 1 | Question to Consider | Indicator | Score (1: Low Risk of Bias; 2: Medium Risk; 3: High risk) |
|---|---|---|---|
| 1. Confounding | Did the study analysis adjust potential confounders appropriately? | Confounders adjusted | 1: most confounders |
| 2: some confounders | |||
| 3: none or cannot tell | |||
| 2. Measurement error in health outcome | What was the heterogeneity of indicators used in the study? | Health outcome | 1: clinical indicator 2 |
| 2: self-reported validated tool | |||
| 3: self-reported tool but not clear if it had been validated 2 | |||
| 3. Measurement error in exposure variable | Did the study consider macroeconomic variables in the analysis? | Number of macroeconomic variables | 1: >1 variable |
| 2: 1 variable | |||
| 3: none | |||
| 4. Ecological fallacy | Were inferences about individuals deduced from inference for the group to which those individuals belonged? | Study design | 1: non-ecological |
| 3: ecological | |||
| 5. Time bias | Were there sufficiently long numbers of time periods in order to obtain reliable estimates? | Factors to be considered: >10 years of data; ≥3 years of data post crisis: potential lag effects | 1: 3 factors were considered |
| 2: ≥2 | |||
| 3: one or none | |||
| 6. Evaluation problem | Was an event (e.g., the Great Recession) evaluated using data in a different form from a cross section (e.g., health surveys) before and after that event? | Number of methods used to control bias | 1: >1 method |
| 2: 1 method | |||
| 3: none | |||
| 7. Unobserved confounding | Did the study control the heterogeneity (i.e., unobserved confounding) and temporal extra variability? | Number of methods used to control bias | 1: >1 method |
| 2: 1 method | |||
| 3: none | |||
| Study Overall Rating | Strong (low risk of bias): none of the domains is rated as 3 | ||
| Moderate: up to 2 domains were rated as 3 | |||
| Weak (high risk of bias): ≥3 domains were rated as 3 | |||
| Selection | Evaluation | Ecological Fallacy | Confounding | Unobserved Confounding | Time | Measurement Error | Number of 3 (High Risk) | Overall Rating | ||
|---|---|---|---|---|---|---|---|---|---|---|
| Exposure | Outcome | |||||||||
| Mental Health | ||||||||||
| Aguilar-Palacio, 2015 [6] | 1 | 3 | 1 | 2 | 3 | 3 | 2 | 2 | 3 | 3 |
| Arroyo-Borrell, 2017 [7] | 1 | 2 | 1 | 1 | 1 | 3 | 3 | 2 | 2 | 2 |
| Bacigalupe, 2016 [8] | 1 | 3 | 1 | 2 | 3 | 1 | 3 | 2 | 3 | 3 |
| Barceló, 2016 [9] | 1 | 1 | 1 | 1 | 1 | 1 | 2 | 1 | 0 | 1 |
| Bartoll, 2014 [10] | 1 | 3 | 1 | 2 | 3 | 3 | 3 | 2 | 4 | 3 |
| Basterra, 2017 [11] | 1 | 3 | 1 | 2 | 3 | 3 | 3 | 2 | 4 | 3 |
| Córdoba-Doña, 2016 [12] | 1 | 3 | 1 | 1 | 3 | 3 | 3 | 2 | 4 | 3 |
| Fernández-García, 2018 [13] | 1 | 1 | 3 | 3 | 3 | 2 | 3 | 1 | 4 | 3 |
| Gili, 2013 [14] | 1 | 2 | 1 | 2 | 3 | 3 | 1 | 2 | 2 | 2 |
| Gili, 2014 [15] | 1 | 1 | 3 | 3 | 3 | 1 | 3 | 1 | 4 | 3 |
| Gili, 2016 [16] | 1 | 3 | 1 | 2 | 3 | 3 | 1 | 2 | 3 | 3 |
| Gotsens, 2015 [17] | 2 | 3 | 1 | 2 | 3 | 3 | 1 | 2 | 3 | 3 |
| Iglesias-García, 2014 [18] | 2 | 1 | 1 | 3 | 3 | 1 | 2 | 2 | 2 | 2 |
| Medel-Herreros, 2017 [19] | 1 | 1 | 3 | 3 | 3 | 1 | 3 | 1 | 4 | 3 |
| Navarro-Mateu, 2015 [20] | 2 | 3 | 1 | 1 | 3 | 3 | 3 | 2 | 4 | 3 |
| Pérez-Romero, 2016 [21] | 2 | 3 | 1 | 1 | 3 | 3 | 3 | 2 | 4 | 3 |
| Rajmil, 2013 [22] | 1 | 3 | 1 | 2 | 3 | 3 | 2 | 2 | 3 | 3 |
| Rajmil, 2015 [23] | 1 | 3 | 1 | 3 | 3 | 2 | 1 | 2 | 3 | 3 |
| Robert, 2014 [24] | 3 | 3 | 1 | 1 | 3 | 3 | 3 | 2 | 5 | 3 |
| Ruíz-Pérez, 2017 [25] | 1 | 2 | 3 | 1 | 1 | 3 | 1 | 2 | 2 | 2 |
| Sicras-Mainar, 2015 [26] | 1 | 1 | 1 | 3 | 3 | 3 | 3 | 1 | 4 | 3 |
| Utzet, 2016 [27] | 2 | 3 | 1 | 3 | 3 | 3 | 3 | 2 | 5 | 3 |
| Zapata-Moya, 2015 [28] | 1 | 2 | 1 | 2 | 1 | 2 | 3 | 2 | 2 | 2 |
| Self-Perceived Health | ||||||||||
| Aguilar-Palacio, 2015 [5] | 1 | 3 | 1 | 2 | 3 | 3 | 2 | 2 | 3 | 3 |
| Arroyo-Borrell, 2015 [29] | 1 | 1 | 1 | 1 | 1 | 3 | 3 | 2 | 2 | 2 |
| Barroso, 2016 [30] | 2 | 3 | 1 | 1 | 3 | 3 | 3 | 2 | 4 | 3 |
| Bartoll, 2015 [31] | 1 | 3 | 1 | 2 | 3 | 2 | 2 | 2 | 2 | 2 |
| Calzón-Fernández, 2017 [32] | 2 | 3 | 1 | 1 | 3 | 3 | 3 | 2 | 3 | 3 |
| Fornell, 2018 [33] | 1 | 2 | 1 | 2 | 1 | 2 | 3 | 2 | 2 | 2 |
| Gotsens, 2015 [17] | 2 | 3 | 1 | 2 | 3 | 3 | 1 | 2 | 3 | 3 |
| López-del-Amo, 2018 [34] | 1 | 2 | 1 | 1 | 1 | 3 | 1 | 2 | 1 | 2 |
| Pérez-Romero, 2016 [21] | 2 | 2 | 1 | 1 | 3 | 3 | 3 | 2 | 3 | 3 |
| Rajmil, 2013 [22] | 1 | 3 | 1 | 2 | 3 | 3 | 2 | 2 | 3 | 3 |
| Rajmil, 2015 [23] | 1 | 2 | 1 | 3 | 3 | 2 | 1 | 2 | 2 | 2 |
| Regidor, 2014 [35] | 1 | 3 | 3 | 3 | 3 | 1 | 3 | 1 | 4 | 3 |
| Urbanos-Garrido, 2015 [36] | 1 | 1 | 1 | 1 | 3 | 3 | 3 | 2 | 3 | 3 |
| Vásquez-Vera, 2016 [37] | 3 | 2 | 1 | 1 | 3 | 3 | 3 | 2 | 4 | 3 |
| Zapata-Moya, 2015 [28] | 1 | 2 | 1 | 2 | 1 | 2 | 3 | 2 | 2 | 2 |
| Suicides | ||||||||||
| Álvarez-Gálvez, 2017 [38] | 1 | 1 | 3 | 2 | 3 | 1 | 1 | 1 | 2 | 2 |
| Borrell, 2017 [39] | 1 | 1 | 3 | 2 | 3 | 1 | 3 | 1 | 3 | 3 |
| Córdoba-Doña, 2014 [40] | 1 | 1 | 3 | 2 | 2 | 2 | 2 | 1 | 1 | 2 |
| Gili, 2014 [15] | 1 | 1 | 3 | 3 | 3 | 1 | 3 | 1 | 4 | 3 |
| López-Bernal, 2013 [41] | 2 | 1 | 3 | 2 | 2 | 3 | 3 | 1 | 3 | 3 |
| Miret, 2014 [42] | 3 | 3 | 1 | 2 | 3 | 3 | 3 | 2 | 5 | 3 |
| Rivera, 2016 [43] | 1 | 2 | 3 | 2 | 1 | 1 | 1 | 1 | 1 | 2 |
| Ruíz-Pérez, 2017 [25] | 1 | 1 | 3 | 3 | 3 | 1 | 3 | 1 | 4 | 3 |
| Saurina, 2015 [44] | 1 | 1 | 3 | 3 | 1 | 1 | 2 | 1 | 2 | 2 |
| Mortality | ||||||||||
| Alonso 2017 [45] | 1 | 1 | 1 | 3 | 3 | 2 | 3 | 1 | 3 | 3 |
| Benmarhnia, 2014 [46] | 1 | 1 | 3 | 3 | 2 | 2 | 3 | 1 | 3 | 3 |
| Ferrando, 2018 [47] | 1 | 1 | 3 | 3 | 1 | 2 | 3 | 1 | 3 | 3 |
| Llàcer, 2014 [48] | 2 | 1 | 1 | 3 | 3 | 1 | 3 | 1 | 3 | 3 |
| Maynou, 2016 [49] | 1 | 1 | 3 | 2 | 1 | 3 | 2 | 1 | 2 | 2 |
| Regidor, 2014 [35] | 1 | 1 | 3 | 3 | 3 | 1 | 3 | 1 | 4 | 3 |
| Regidor 2016 [50] | 1 | 1 | 1 | 3 | 3 | 2 | 3 | 1 | 3 | 3 |
| Ruíz-Ramos, 2014 [51] | 1 | 1 | 3 | 3 | 2 | 2 | 3 | 1 | 3 | 3 |
| Alcohol and Illegal Drugs | ||||||||||
| Bosque-Prous, 2017 [52] | 1 | 3 | 1 | 1 | 3 | 3 | 3 | 2 | 4 | 3 |
| Collell, 2015 [53] | 2 | 3 | 1 | 1 | 3 | 3 | 3 | 2 | 4 | 3 |
| Gili, 2013 [14] | 1 | 2 | 1 | 2 | 3 | 3 | 1 | 2 | 2 | 2 |
| Martín-Bassols, 2016 [54] | 2 | 3 | 1 | 1 | 2 | 3 | 2 | 2 | 2 | 2 |
| Health Inequalities | ||||||||||
| Abásolo, 2017 [55] | 1 | 2 | 1 | 1 | 1 | 3 | 3 | 2 | 2 | 2 |
| Coveney, 2016 [56] | 1 | 1 | 1 | 1 | 2 | 1 | 3 | 2 | 1 | 2 |
| Maynou, 2016 [49] | 1 | 1 | 3 | 2 | 1 | 3 | 2 | 1 | 2 | 2 |
| Use of and Access to Health Services | ||||||||||
| Abásolo, 2017 [55] | 1 | 2 | 1 | 1 | 1 | 3 | 3 | 2 | 2 | 2 |
| Córdoba-Doña, 2018 [57] | 1 | 3 | 1 | 1 | 3 | 3 | 3 | 2 | 4 | 3 |
| García-Subirats, 2014 [58] | 1 | 3 | 1 | 1 | 3 | 3 | 3 | 2 | 4 | 3 |
| Lostao, 2017 [59] | 1 | 3 | 1 | 2 | 3 | 3 | 3 | 2 | 4 | 3 |
| Other | ||||||||||
| Calzón-Fernández, 2015 [60] | 1 | 3 | 1 | 1 | 3 | 3 | 3 | 2 | 4 | 3 |
| Fernández, 2015 [61] | 3 | 1 | 1 | 1 | 3 | 3 | 3 | 2 | 4 | 3 |
| Llàcer, 2014 [48] | 2 | 1 | 1 | 3 | 3 | 1 | 3 | 1 | 3 | 3 |
| Larrañaga, 2014 [62] | 2 | 3 | 1 | 3 | 3 | 1 | 3 | 2 | 4 | 3 |
| Lorenzo-Carrascosa,2016 [63] | 1 | 1 | 3 | 3 | 3 | 1 | 3 | 1 | 4 | 3 |
| Palència, 2018 [64] | 1 | 1 | 1 | 2 | 1 | 2 | 3 | 1 | 1 | 2 |
| Varea, 2016 [65] | 1 | 1 | 1 | 2 | 3 | 1 | 1 | 1 | 1 | 2 |
| Health Outcome | Selection | Evaluation | Ecological Fallacy | Confounding | Unobserved Confounding | Time | Measurement Error Exposure | Measurement Error Outcome | Overall Rating | Total | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Mental health | n | 1 | 13 | 4 | 7 | 19 | 15 | 14 | 0 | 17 | 23 |
| % | 4.3% | 56.5% | 17.4% | 30.4% | 82.6% | 65.2% | 60.9% | 0.0% | 73.9% | 32.4% | |
| Self-perceived health | n | 1 | 7 | 1 | 2 | 11 | 10 | 8 | 0 | 9 | 14 |
| % | 7.1% | 50.0% | 7.1% | 14.3% | 78.6% | 71.4% | 57.1% | 0.0% | 64.3% | 19.7% | |
| Suicides | n | 1 | 1 | 8 | 3 | 5 | 2 | 5 | 0 | 5 | 9 |
| % | 11.1% | 11.1% | 88.9% | 33.3% | 55.6% | 22.2% | 55.6% | 0.0% | 55.6% | 12.7% | |
| Mortality | n | 0 | 0 | 5 | 7 | 4 | 1 | 7 | 0 | 7 | 8 |
| % | 0.0% | 0.0% | 62.5% | 87.5% | 50.0% | 12.5% | 87.5% | 0.0% | 87.5% | 11.3% | |
| Alcohol and illegal drugs | n | 0 | 3 | 0 | 0 | 3 | 4 | 2 | 0 | 2 | 4 |
| % | 0.0% | 75.0% | 0.0% | 0.0% | 75.0% | 100.0% | 50.0% | 0.0% | 50.0% | 5.6% | |
| Health inequalities | n | 0 | 0 | 1 | 0 | 0 | 2 | 2 | 0 | 0 | 3 |
| % | 0.0% | 0.0% | 33.3% | 0.0% | 0.0% | 66.7% | 66.7% | 0.0% | 0.0% | 4.2% | |
| Use and access of health services | n | 0 | 2 | 0 | 0 | 2 | 3 | 3 | 0 | 2 | 3 |
| % | 0.0% | 66.7% | 0.0% | 0.0% | 66.7% | 100.0% | 100.0% | 0.0% | 66.7% | 4.2% | |
| Other | n | 1 | 2 | 1 | 3 | 6 | 2 | 6 | 0 | 5 | 7 |
| % | 14.3% | 28.6% | 14.3% | 42.9% | 85.7% | 28.6% | 85.7% | 0.0% | 71.4% | 9.9% | |
| Total | n | 4 | 28 | 20 | 22 | 50 | 39 | 47 | 0 | 47 | 71 |
| % | 5.6% | 39.4% | 28.2% | 31.0% | 70.4% | 54.9% | 66.2% | 0.0% | 66.2% | 100.0% | |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Saez, M.; Barceló, M.A.; Saurina, C.; Cabrera, A.; Daponte, A. Evaluation of the Biases in the Studies that Assess the Effects of the Great Recession on Health. A Systematic Review. Int. J. Environ. Res. Public Health 2019, 16, 2479. https://doi.org/10.3390/ijerph16142479
Saez M, Barceló MA, Saurina C, Cabrera A, Daponte A. Evaluation of the Biases in the Studies that Assess the Effects of the Great Recession on Health. A Systematic Review. International Journal of Environmental Research and Public Health. 2019; 16(14):2479. https://doi.org/10.3390/ijerph16142479
Chicago/Turabian StyleSaez, Marc, Maria Antònia Barceló, Carme Saurina, Andrés Cabrera, and Antonio Daponte. 2019. "Evaluation of the Biases in the Studies that Assess the Effects of the Great Recession on Health. A Systematic Review" International Journal of Environmental Research and Public Health 16, no. 14: 2479. https://doi.org/10.3390/ijerph16142479
APA StyleSaez, M., Barceló, M. A., Saurina, C., Cabrera, A., & Daponte, A. (2019). Evaluation of the Biases in the Studies that Assess the Effects of the Great Recession on Health. A Systematic Review. International Journal of Environmental Research and Public Health, 16(14), 2479. https://doi.org/10.3390/ijerph16142479






