Compliance with the Very Integrated Program (VIP) for Smoking Cessation, Nutrition, Physical Activity and Comorbidity Education Among Patients in Treatment for Alcohol and Drug Addiction
Abstract
1. Introduction
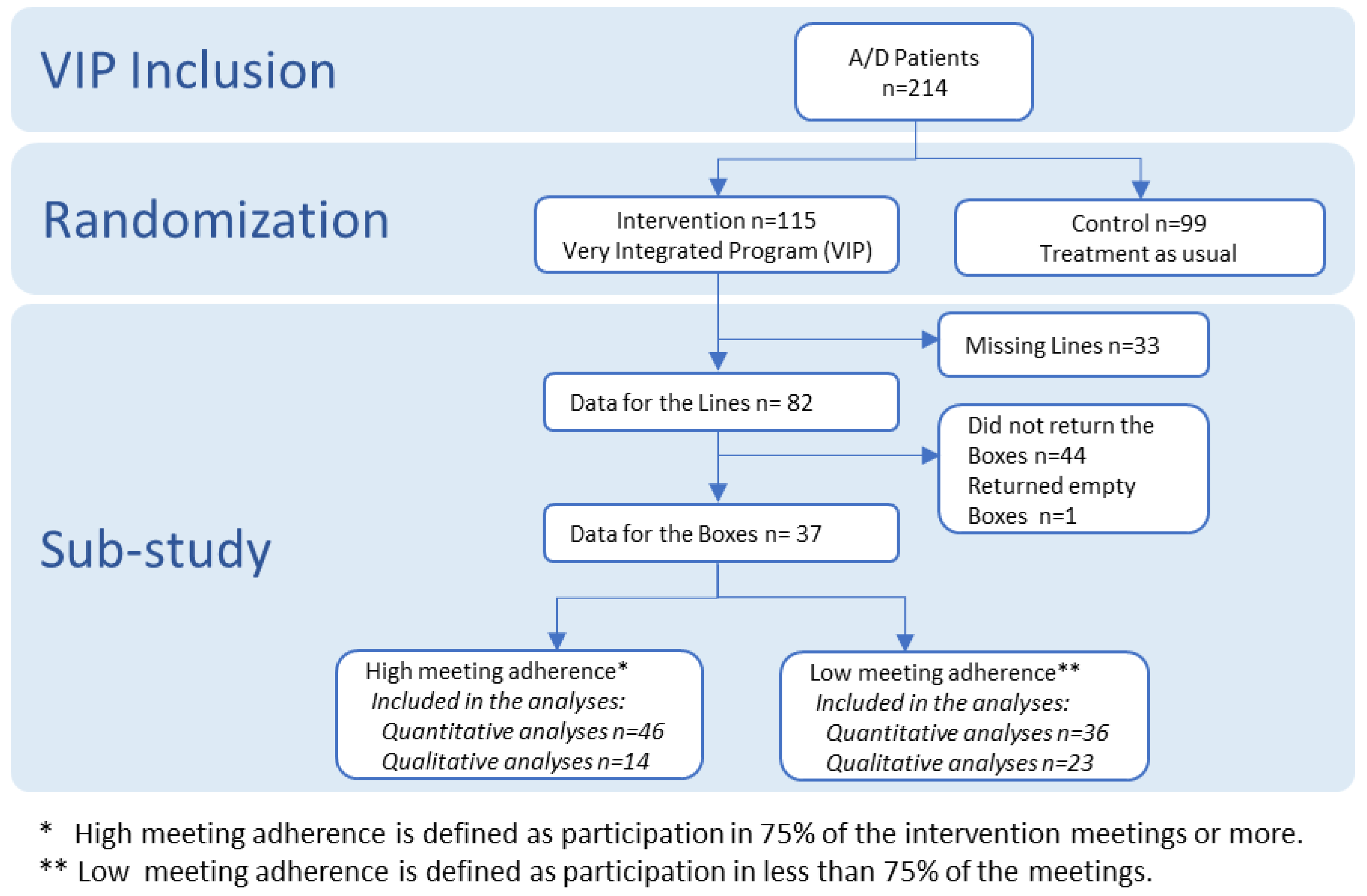
2. Materials and Methods
2.1. Data Collection
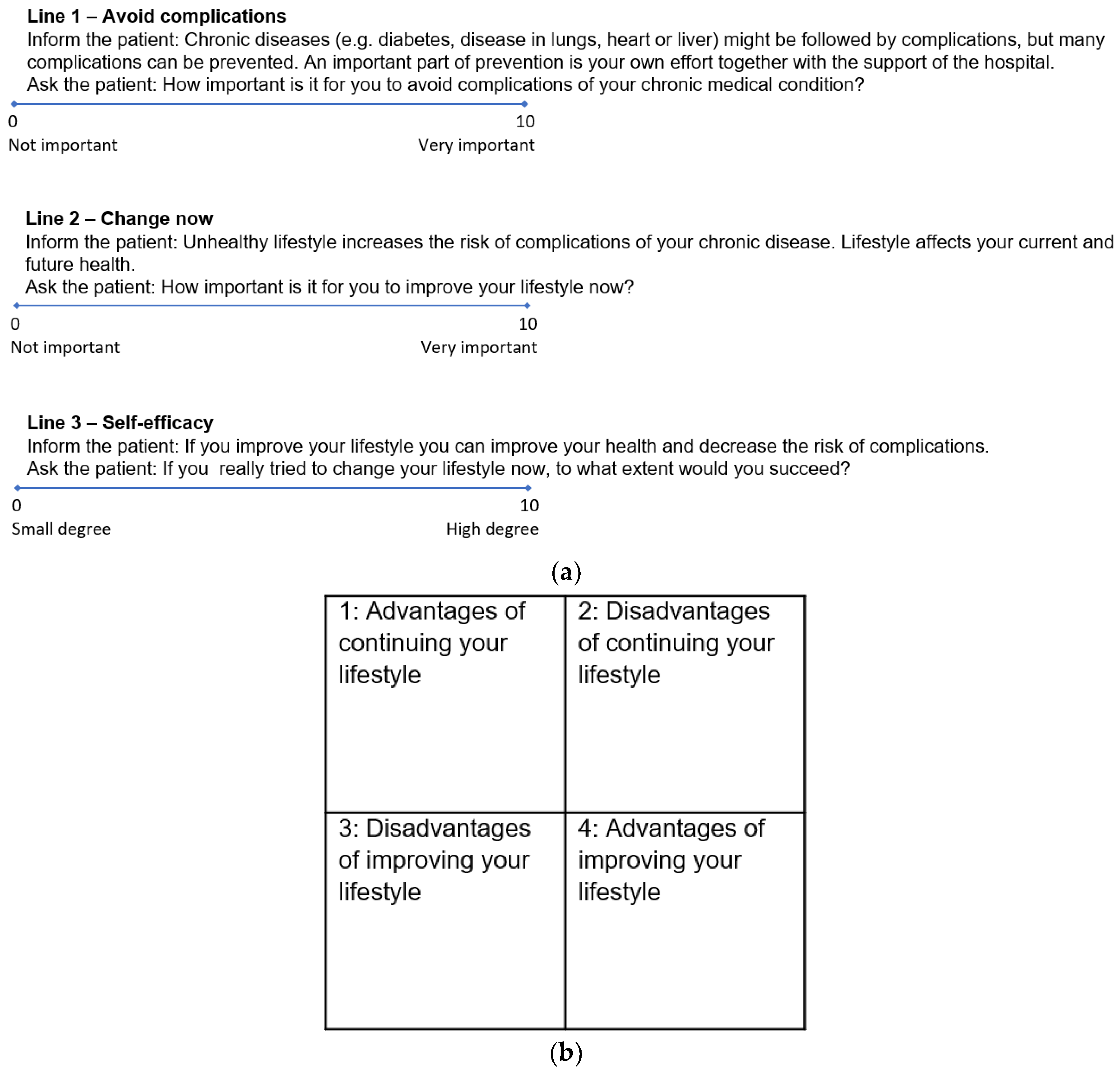
2.1.1. Quantitative Data
2.1.2. Qualitative Data
2.2. Data Analysis
2.2.1. Quantitative Analyses
2.2.2. Qualitative Analyses—Systematic Text Condensation
2.3. Comprehensiveness of the Available Data
2.3.1. Quantitative Data: Sample Size Estimation
2.3.2. Qualitative Data: Data Saturation
2.4. Ethical Issues
3. Results
3.1. Quantitative Data
3.2. Qualitative Data
4. Discussion
4.1. Methodological Implications
4.2. Clinical Implications
4.3. Research Implications
4.4. Suggestions for Future Research
4.5. Lessons Learned
4.6. Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Beynon, R.A.; Lang, S.; Schimansky, S.; Penfold, C.M.; Waylen, A.; Thomas, S.J.; Pawlita, M.; Waterboer, T.; Martin, R.M.; May, M.; et al. Tobacco smoking and alcohol drinking at diagnosis of head and neck cancer and all-cause mortality: Results from head and neck 5000, a prospective observational cohort of people with head and neck cancer. Int. J. Cancer 2018, 143, 1114–1127. [Google Scholar] [CrossRef] [PubMed]
- Bonevski, B.; Regan, T.; Paul, C.; Baker, A.L.; Bisquera, A. Associations between alcohol, smoking, socioeconomic status and comorbidities: Evidence from the 45 and Up Study. Drug Alcohol Rev. 2014, 33, 169–176. [Google Scholar] [CrossRef] [PubMed]
- Taylor, B.; Rehm, J. When risk factors combine: The interaction between alcohol and smoking for aerodigestive cancer, coronary heart disease, and traffic and fire injury. Addict. Behav. 2006, 31, 1522–1535. [Google Scholar] [CrossRef] [PubMed]
- Rasmussen, M.; Fernández, E.; Tønnesen, H. Effectiveness of the gold standard programme COMPARED with other smoking cessation interventions in Denmark: A cohort study. BMJ Open 2017, 7, e013553. [Google Scholar] [CrossRef] [PubMed]
- Neumann, T.; Rasmussen, M.; Heitmann, B.L.; Tønnesen, H. Gold standard program for heavy smokers in a real-life setting. Int. J. Environ. Res. Public Health 2013, 10, 4186–4199. [Google Scholar] [CrossRef] [PubMed]
- Thomsen, T.; Villebro, N.; Møller, A.M. Interventions for preoperative smoking cessation. Cochrane Database Syst. Rev. 2014, 27, CD002294. [Google Scholar] [CrossRef] [PubMed]
- Lauridsen, S.V.; Thomsen, T.; Thind, P.; Tønnesen, H. STOP smoking and alcohol drinking before OPeration for bladder cancer (the STOP-OP study), perioperative smoking and alcohol cessation intervention in relation to radical cystectomy: Study protocol for a randomised controlled trial. Trials 2017, 18, 329. [Google Scholar] [CrossRef]
- Miller, W.R.; Rollnick, S. Motivational Interviewing: Preparing People to Change Addictive Behavior; Guilford Press: New York, NY, USA, 1991. [Google Scholar]
- Prochaska, J.O.; DiClemente, C.C.; Norcross, J.C. In search of how people change. Applications to addictive behaviors. Am. Psychol. 1992, 47, 1102–1114. [Google Scholar] [CrossRef] [PubMed]
- Tønnesen, H. Engage in the Process of Change: Facts and Methods; WHO Regional Office for Europe: Copenhagen, Denmark, 2012. [Google Scholar]
- Thomsen, T.; Villebro, N.; Moller, A.M. Interventions for preoperative smoking cessation. Cochrane Database Syst. Rev. 2010. [Google Scholar] [CrossRef]
- Rasmussen, M.; Klinge, M.; Krogh, J.; Nordentoft, M.; Tønnesen, H. Effectiveness of the Gold Standard Programme (GSP) for smoking cessation on smokers with and without a severe mental disorder: A Danish cohort study. BMJ Open 2018, 8, e021114. [Google Scholar] [CrossRef]
- Neumann, T.; Rasmussen, M.; Ghith, N.; Heitmann, B.L.; Tonnesen, H. The gold standard programme: Smoking cessation interventions for disadvantaged smokers are effective in a real-life setting. Tob. Control 2013, 22, e9. [Google Scholar] [CrossRef] [PubMed]
- Burgess, E.; Hassmén, P.; Welvaert, M.; Pumpa, K.L. Behavioural treatment strategies improve adherence to lifestyle intervention programmes in adults with obesity: A systematic review and meta-analysis. Clin. Obes. 2017, 7, 105–114. [Google Scholar] [CrossRef] [PubMed]
- Leung, A.W.Y.; Chan, R.S.M.; Sea, M.M.M.; Woo, J. An overview of factors associated with adherence to lifestyle modification programs for weight management in adults. Int. J. Environ. Res. Public Health 2017, 14. [Google Scholar] [CrossRef] [PubMed]
- Le Berre, A.P.; Rauchs, G.; la Joie, R.; Segobin, S.; Mézenge, F.; Boudehent, C.; Vabret, F.; Viader, F.; Eustache, F.; Pitel, A.L.; et al. Readiness to change and brain damage in patients with chronic alcoholism. Psychiatry Res. 2013, 213, 202–209. [Google Scholar] [CrossRef] [PubMed]
- Gwaltney, C.J.; Metrik, J.; Kahler, C.W.; Shiffman, S. Self-efficacy and smoking cessation: A meta-analysis. Psychol. Addict. Behav. 2009, 23, 56–66. [Google Scholar] [CrossRef] [PubMed]
- Bandura, A. Self-efficacy mechanism in human agency. Am. Psychol. 1982, 37, 122–147. [Google Scholar] [CrossRef]
- Irving, J.L.; Mann, L.M. Decision Making: A Psychological Analysis of Conflict, Choice, and Commitment; Free Press: New York, NY, USA, 1977. [Google Scholar]
- Hovhannisyan, K.; Adami, J.; Wikström, M.M.; Tønnesen, H. Very integrated program (VIP): Smoking and other lifestyles, co-morbidity and quality of life in patients undertaking treatment for alcohol and drug addiction in Sweden. Clin. Health Promot. 2018, 8, 14–19. [Google Scholar] [CrossRef]
- Hayes, M.H.S.; Patterson, D.G. Experimental development of the graphic rating method. Psychol. Bull. 1921, 18, 98–99. [Google Scholar]
- Cheng, K.K.F.; Metcalfe, A. Qualitative methods and process evaluation in clinical trials context: Where to head to? Int. J. Qual. Methods 2018, 17, 1–4. [Google Scholar] [CrossRef]
- Moore, G.; Audrey, S.; Barker, M.; Bond, L.; Bonell, C.; Cooper, C.; Hardeman, W.; Moore, L.; O’Cathain, A.; Tinati, T.; et al. Process evaluation in complex public health intervention studies: The need for guidance. J. Epidemiol. Community Health 2014, 68, 101–102. [Google Scholar] [CrossRef]
- Ware, J.; Kosinski, M.; Gandek, B. SF36 Health Survey: Manual and Interpretation Guide; QualityMetric Incorporated: Lincoln, RI, USA, 2005. [Google Scholar]
- Ghith, N.; Ammari, A.; Rasmussen, M.; Frølich, A.; Cooper, K.; Tønnesen, H. Impact of compliance on quit rates in a smoking cessation intervention: Population study in Denmark. Clin. Health Promot. 2012, 2, 111–119. [Google Scholar] [CrossRef]
- Daeppen, J.B.; Krieg, M.A.; Burnand, B.; Yersin, B. MOS-SF-36 in evaluating health-related quality of life in alcohol-dependent patients. Am. J. Drug Alcohol Abus. 1998, 24, 685–694. [Google Scholar] [CrossRef]
- Chiu, E.C.; Hsueh, I.P.; Hsieh, C.H.; Hsieh, C.L. Tests of data quality, scaling assumptions, reliability, and construct validity of the SF-36 health survey in people who abuse heroin. J. Med. Assoc. 2014, 113, 234–241. [Google Scholar] [CrossRef] [PubMed]
- Sullivan, M.; Karlsson, J.; Ware, J.E., Jr. The Swedish SF-36 health Survey-I. Evaluation of data quality, scaling assumptions, reliability and construct validity across general populations in Sweden. Soc. Sci. Med. 1995, 41, 1349–1358. [Google Scholar] [PubMed]
- IBM. IBM SPSS Statistics for Windows; IBM Corp.: Armonk, NY, USA, 2013. [Google Scholar]
- QSR. NVivo Qualitative Data Analysis Software; QSR International Pty Ltd.: Melbourne, Australia, 2015. [Google Scholar]
- Malterud, K. Systematic text condensation: A strategy for qualitative analysis. Scand. J. Public Health 2012, 40, 795–805. [Google Scholar] [CrossRef] [PubMed]
- Jorgensen, T.; Christensen, E.; Kampmann, J.P. Clinical Research Methods—A Basic Book; Munksgaard: Copenhagen, Denmark, 2011. [Google Scholar]
- Saunders, B.; Sim, J.; Kingstone, T.; Baker, S.; Waterfield, J.; Bartlam, B.; Burroughs, H.; Jinks, C. Saturation in qualitative research: Exploring its conceptualization and operationalization. Qual. Quant. 2018, 52, 1893–1907. [Google Scholar] [CrossRef] [PubMed]
- Guest, G.; Bunce, A.; Johnson, L. How many interviews are enough? An experiment with data saturation and variability. Field Meth. 2006, 18, 59–82. [Google Scholar] [CrossRef]
- Kuusisto, K.; Knuuttila, V.; Saarnio, P. Clients’ self-efficacy and outcome expectations: Impact on retention and effectiveness in outpatient substance abuse treatment. Addict. Disord. Treat. 2011, 10, 157–168. [Google Scholar] [CrossRef]
- Forcehimes, A.A.; Tonigan, J.S. Self-efficacy as a factor in abstinence from alcohol/other drug abuse: A meta-analysis. Alcohol. Treat. Q. 2008, 26, 480–489. [Google Scholar] [CrossRef]
- Strecher, V.J.; DeVellis, B.M.; Becker, M.H.; Rosenstock, I.M. The role of self-efficacy in achieving health behavior change. Health Educ. Q. 1986, 13, 73–92. [Google Scholar] [CrossRef]
- Bertholet, N.; Gaume, J.; Faouzi, M.; Gmel, G.; Daeppen, J.B. Predictive value of readiness, importance, and confidence in ability to change drinking and smoking. BMC Public Health 2012, 12, 708. [Google Scholar] [CrossRef] [PubMed]
- Abdollahi, Z.; Taghizadeh, F.; Bahramzad, O. Relationship between addiction relapse and self-efficacy rates in injection drug users referred to Maintenance Therapy Center of Sari, 1391. Glob. J. Health Sci. 2014, 6, 138–144. [Google Scholar] [CrossRef] [PubMed]
- Burling, T.A.; Reilly, P.M.; Moltzen, J.O.; Ziff, D.C. Self-efficacy and relapse among inpatient drug and alcohol abusers: A predictor of outcome. J. Stud. Alcohol 1989, 50, 354–360. [Google Scholar] [CrossRef] [PubMed]
- Fiorentine, R.; Hillhouse, M.P. Self-efficacy, expectancies, and abstinence acceptance: Further evidence for the addicted-self model of cessation of alcohol- and drug-dependent behavior. Am. J. Drug Alcohol Abus. 2000, 26, 497–521. [Google Scholar] [CrossRef]
- Romero, J.C.; Pérez, E.J.P.; López, M.P. Coping self-efficacy against alcohol and other drugs use as treatment outcome predictor and its relation with personality dimensions: Evaluation of a sample of addicts using DTCQ, VIP and MCM-II. Adicciones 2007, 19, 141–151. [Google Scholar]
- Vassy, J.L.; O’Brien, K.E.; Waxler, J.L.; Park, E.R.; Delahanty, L.M.; Florez, J.C.; Meigs, J.B.; Grant, R.W. Impact of literacy and numeracy on motivation for behavior change after diabetes genetic risk testing. Med. Decis. Mak. 2012, 32, 606–615. [Google Scholar] [CrossRef] [PubMed]
- Berkman, N.D.; Sheridan, S.L.; Donahue, K.E.; Halpern, D.J.; Viera, A.; Crotty, K.; Holland, A.; Brasure, M.; Lohr, K.N.; Harden, E.; et al. Health literacy interventions and outcomes: An updated systematic review. Evid. Rep. Technol. Assess. 2011, 199, 941. [Google Scholar]
- Ramsay, P.; Huby, G.; Merriweather, J.; Salisbury, L.; Rattray, J.; Griffith, D.; Walsh, T.; On behalf of the RECOVER collaborators. Patient and carer experience of hospital-based rehabilitation from intensive care to hospital discharge: Mixed methods process evaluation of the RECOVER randomized clinical trial. BMJ Open 2016, 6, e012041. [Google Scholar] [CrossRef]
- Taylor, G.; McNeill, A.; Girling, A.; Farley, A.; Lindson-Hawley, N.; Aveyard, P. Change in mental health after smoking cessation: Systematic review and meta-analysis. BMJ 2014, 348, g1151. [Google Scholar] [CrossRef]
- Taylor, G.; McNeill, A.; Aveyard, P. Does deterioration in mental health after smoking cessation predict relapse to smoking? BMC Public Health 2015, 15, 1150. [Google Scholar] [CrossRef]
- Pedersen, B.K. Physical activity and muscle-brain crosstalk. Nat. Rev. Endocrinol. 2019. [Google Scholar] [CrossRef] [PubMed]
- Biddle, S. Physical activity and mental health: Evidence is growing. World Psychiatry 2016, 15, 176–177. [Google Scholar] [CrossRef] [PubMed]
- Berman, A.H.; Wennberg, P.; Sinadinovic, K. Changes in mental and physical well-being among problematic alcohol and drug users in 12-month internet-based intervention trials. Psychol. Addict. Behav. 2015, 29, 97–105. [Google Scholar] [CrossRef] [PubMed]
- Egholm, J.W.; Pedersen, B.; Møller, A.M.; Adami, J.; Juhl, C.B.; Tønnesen, H. Perioperative alcohol cessation intervention for postoperative complications. Cochrane Database Syst. Rev. 2018, 8. [Google Scholar] [CrossRef]
| Variables | Total (n = 82) |
|---|---|
| Line 1—Avoid Complications (median (range)) | 10 (2–10) |
| Line 2—Change now (median (range)) | 9 (3–10) |
| Line 3—Self-efficacy (median (range)) | 7 (0–10) |
| Age in years (median (range)) | 53 (27–72) |
| Years of addiction (median (range)) | 25 (1–60) |
| Men (n (%)) | 49 (60%) |
| Alcohol addiction (n (%)) | 44 (54%) |
| Living alone (n (%)) | 64 (78%) |
| Higher educational level (n (%)) | 29 (35%) |
| No housing (n (%)) | 13 (16%) |
| Unemployed * (n (%)) | 19 (23%) |
| Number of health determinants (≥2) | 53 (65%) |
| Number of co-morbidities (≥2) | 24 (29%) |
| Physical health (median (range)) | 54 (0–100) |
| Mental Health (median (range)) | 38 (0–100) |
| Variables | Total n = 82 | High MA * n = 46 | Low MA * n = 36 | OR (95% CI) Unadjusted | OR (95% CI) Adjusted |
|---|---|---|---|---|---|
| Line 1—Avoid Complications (median (range)) | 10 (2–10) | 10 (2–10) | 10 (5–10) | 0.75 (0.54–1.07) | 0.51 (0.29–0.90) |
| Line 2—Change now (median (range)) | 9 (3–10) | 9 (6–10) | 9 (3–10) | 1.24 (0.90–1.70) | 1.69 (0.91–3.13) |
| Line 3—Self-efficacy (median (range)) | 7 (0–10) | 8 (1–10) | 6 (0–10) | 1.23 (1.01–1.51) | 1.28 (1.00–1.63) |
| Age in years (median (range)) | 53 (27–72) | 54 (27–72) | 52 (27–72) | 1.01 (0.97–1.04) | 1.02 (0.97–1.07) |
| Years of addiction (median (range)) | 25 (1–60) | 27 (3–57) | 21 (1–60) | 1.01 (0.98–1.04) | 1.02 (0.98–1.06) |
| Men (n (%)) | 49 (60%) | 27 (55%) | 22 (45%) | 0.90 (0.37–2.20) | 0.95 (0.33–2.67) |
| Themes (Capital Letters), Sub-Themes (Bold), Condensations, Authentic Illustrative Quotations (Italic) |
|---|
| HEALTH AND WELLBEING |
| Improved health is an advantage of improving lifestyle |
| The patients expressed, that they expect a major advantage of improving their lifestyle to be that they will feel better, that their health will be better, and that their strength will improve—both physically and mentally. As examples they mention getting rid of high blood pressure, asthma will improve, and weight loss. They also expect lifestyle change will help them recover, feel refreshed, get a better self-image and be more positive. They also expect to get a better old age and live longer. “Feel better physically and mentally and improved strength”. |
| Continuing current lifestyle causes poor health and future health risks |
| The major disadvantage experienced by the patients of their current lifestyle is their deteriorated physical and mental health. They are often ill, they have a cough and high blood pressure. They feel in bad shape; they are overweight and fear not being able to breathe. Their stress and concern increase, and they struggle with anxiety. They are aware of the risk of getting COPD, a stroke, cancer, chronic diseases or problems with their heart. They know, that their current lifestyle does not lead to a long and healthy life. “I do not give myself the chance to live a longer and healthier life”. |
| Continuing current lifestyle might lead to a premature death |
| The patients are aware that a disadvantage of their current lifestyle is, that it might shorten their lifespan and that their children consequently would be without a parent should they die prematurely. “Running the risk of a premature death”. |
| PERSONAL ECONOMY |
| Improving lifestyle will improve personal economy |
| Spending money on other things is seen as an advantage of changing lifestyle by the patients. They expect that it will improve their living conditions, and that they perhaps would have a surplus. “More money over to other things”. |
| Continuing current lifestyle restrains individuals in poor economy |
| Living with poor economy is experienced as a disadvantage of the patients’ current lifestyle. It costs them too much and they live a poor and depleted life. “It costs too much”. |
| ACCEPTANCE OF CHANGE |
| There are no advantages of continuing current lifestyle |
| The patients find it difficult to see advantages of their current lifestyle. “There are no advantages, actually”. |
| There are no disadvantages of improving lifestyle |
| The patients see no disadvantages of changing their lifestyle. “There are no disadvantages”. |
| EMOTIONS RELATED TO LIFESTYLE CHANGE |
| Status quo is easier than changing routine |
| The patients must not change lifestyle and they see this as an advantage. They find it difficult to begin something new and to make an effort to break a habit. They find it convenient not to do anything, not to care or to think about their flaws. Their current lifestyle feels safe to them because some of them fear changes. They know, that changing lifestyle will demand a commitment from them, they think nicotine abstinences will cause anxiety and they will lose the opportunity to sleep all day. “Escape changes and all the effort it implies, peace of mind”. |
| Positive social implications of lifestyle improvement especially improved contact with children |
| The patients believe, that they will become more social if they change lifestyle. They think of how they could do more together with their children and how they would have a longer future together. They also envision how they might find a partner, how they would not smell of smoke all the time, how they might become a role model for others and support family members in smoking cessation. “My daughter worries so much”. |
| Current lifestyle is associated with positive emotions |
| The current lifestyle of the patients makes them calm inside and helps them suppress their anxiety. They experience that they become less aggressive, and it makes them feel good. They also think of it as a pleasant social activity. “Makes me calm inside and suppresses my anxiety”. |
| Improving lifestyle is expected to cause negative emotions |
| The patients expect lifestyle change to influence their mood negatively. They think they will get a lot of “do’s”, for example about what they eat and with whom they socialise. In that way, they imagine they would feel their life would be limited compared to their current life. “Bad mood”. |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hovhannisyan, K.; Günther, M.; Raffing, R.; Wikström, M.; Adami, J.; Tønnesen, H. Compliance with the Very Integrated Program (VIP) for Smoking Cessation, Nutrition, Physical Activity and Comorbidity Education Among Patients in Treatment for Alcohol and Drug Addiction. Int. J. Environ. Res. Public Health 2019, 16, 2285. https://doi.org/10.3390/ijerph16132285
Hovhannisyan K, Günther M, Raffing R, Wikström M, Adami J, Tønnesen H. Compliance with the Very Integrated Program (VIP) for Smoking Cessation, Nutrition, Physical Activity and Comorbidity Education Among Patients in Treatment for Alcohol and Drug Addiction. International Journal of Environmental Research and Public Health. 2019; 16(13):2285. https://doi.org/10.3390/ijerph16132285
Chicago/Turabian StyleHovhannisyan, Karen, Michelle Günther, Rie Raffing, Maria Wikström, Johanna Adami, and Hanne Tønnesen. 2019. "Compliance with the Very Integrated Program (VIP) for Smoking Cessation, Nutrition, Physical Activity and Comorbidity Education Among Patients in Treatment for Alcohol and Drug Addiction" International Journal of Environmental Research and Public Health 16, no. 13: 2285. https://doi.org/10.3390/ijerph16132285
APA StyleHovhannisyan, K., Günther, M., Raffing, R., Wikström, M., Adami, J., & Tønnesen, H. (2019). Compliance with the Very Integrated Program (VIP) for Smoking Cessation, Nutrition, Physical Activity and Comorbidity Education Among Patients in Treatment for Alcohol and Drug Addiction. International Journal of Environmental Research and Public Health, 16(13), 2285. https://doi.org/10.3390/ijerph16132285