Characteristics of Non-Emergent Visits in Emergency Departments: Profiles and Longitudinal Pattern Changes in Taiwan, 2000–2010
Abstract
1. Introduction
2. Materials and Methods
2.1. Data Source and Ethical Concerns
2.2. Determining of Non-Emergent ED Visit
2.3. Systematic-Level Factor and Study Cohort
2.4. Personal- and ED Visit-Level Factors
2.5. Statistical Analysis
3. Results
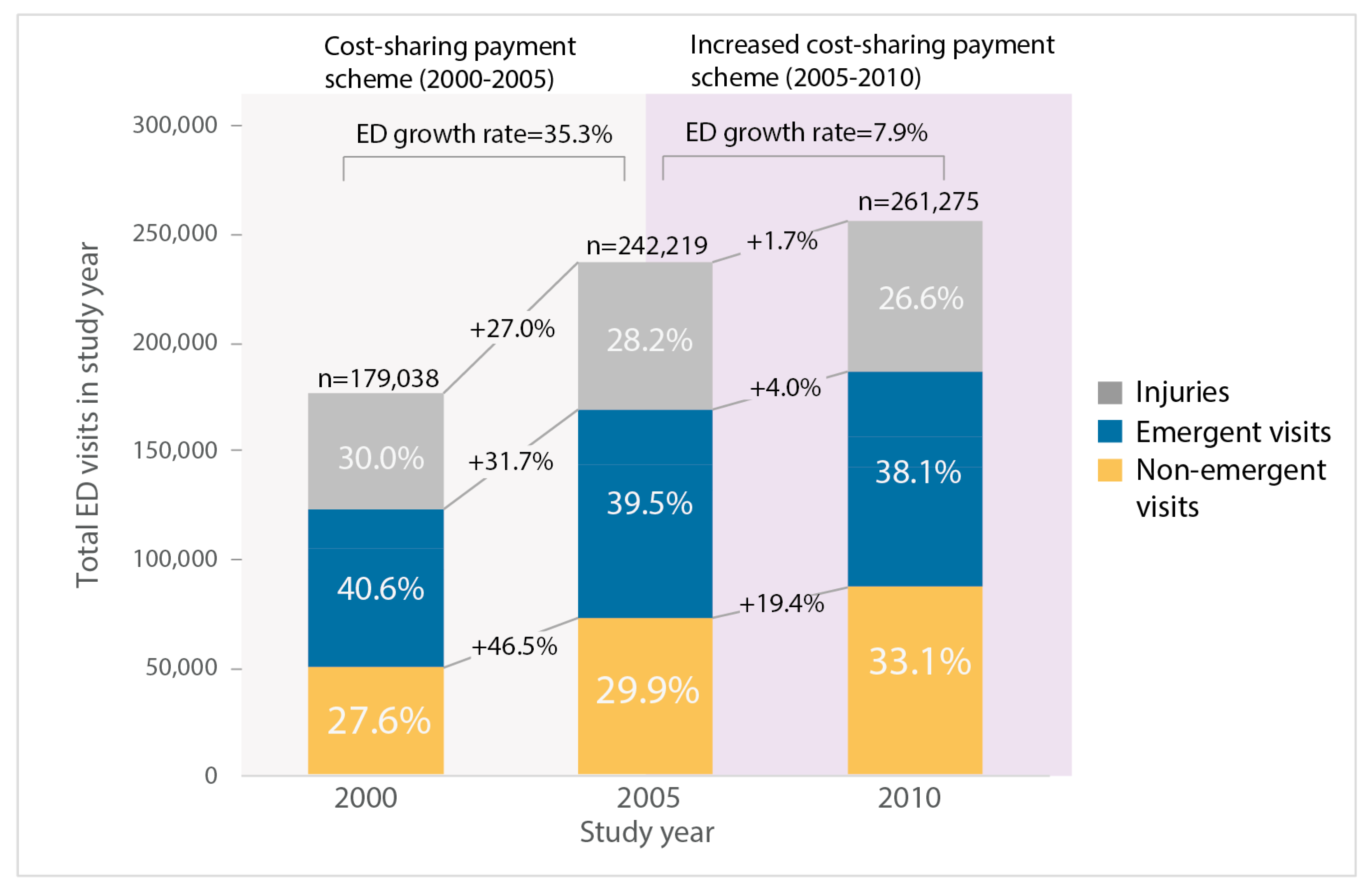
3.1. Annual ED Visit and Proportion of ED Visit
3.2. Emergernt Visits vs. Non-Emergent Visits
3.3. Characteristics of Non-Emergent Visits
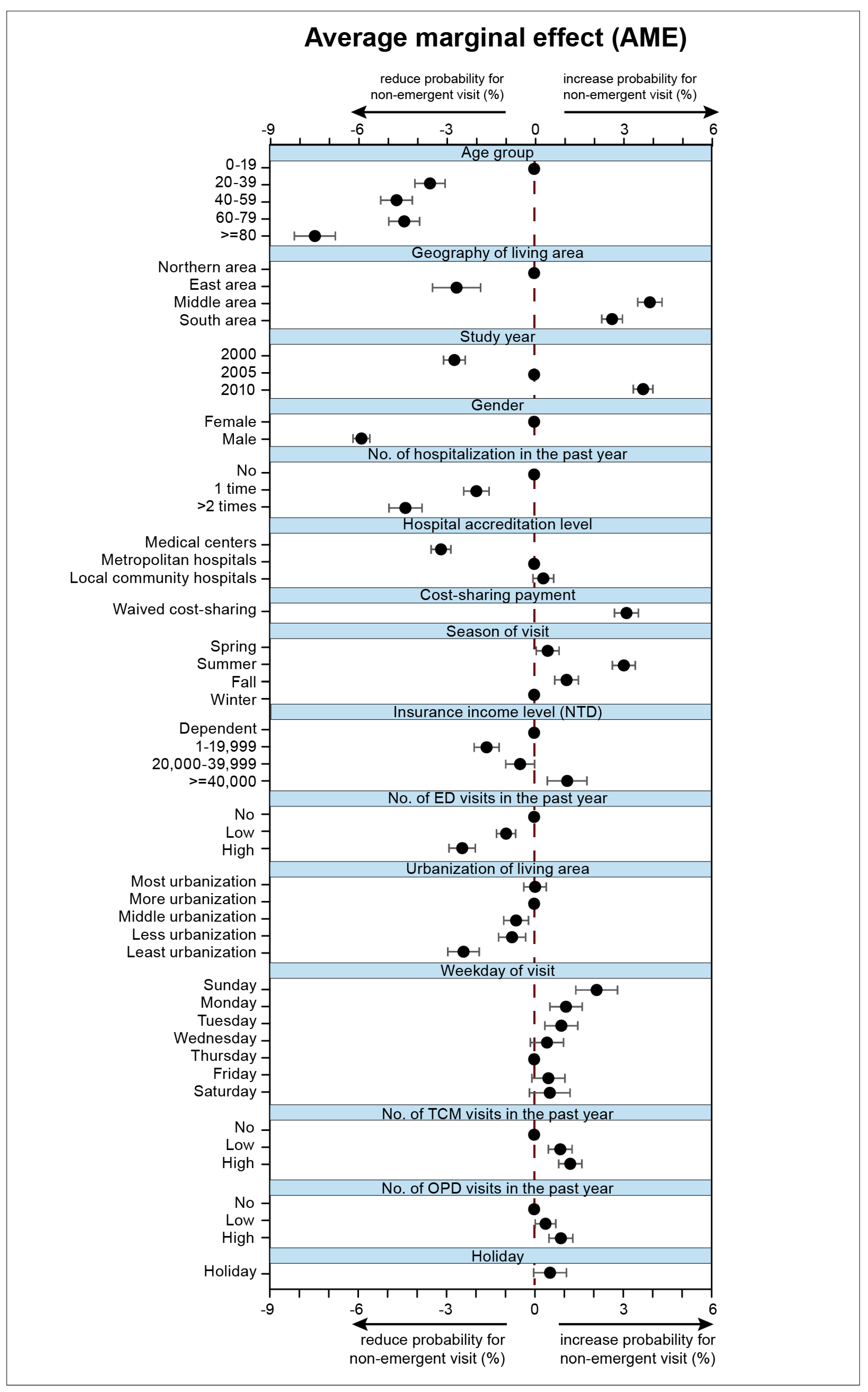
3.4. Average Marginal Effects of Factors Associated with Non-Emergent ED Visits
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Durand, A.C.; Gentile, S.; Devictor, B.; Palazzolo, S.; Vignally, P.; Gerbeaux, P.; Sambuc, R. Ed patients: How nonurgent are they? Systematic review of the emergency medicine literature. Am. J. Emerg. Med. 2011, 29, 333–345. [Google Scholar] [CrossRef] [PubMed]
- Van den Heede, K.; Van de Voorde, C. Interventions to reduce emergency department utilisation: A review of reviews. Health Policy 2016, 120, 1337–1349. [Google Scholar] [CrossRef] [PubMed]
- Mohiuddin, S.; Busby, J.; Savovic, J.; Richards, A.; Northstone, K.; Hollingworth, W.; Donovan, J.L.; Vasilakis, C. Patient flow within uk emergency departments: A systematic review of the use of computer simulation modelling methods. BMJ Open 2017, 7. [Google Scholar] [CrossRef] [PubMed]
- Tang, N.; Stein, J.; Hsia, R.Y.; Maselli, J.H.; Gonzales, R. Trends and characteristics of us emergency department visits, 1997–2007. JAMA 2010, 304, 664–670. [Google Scholar] [CrossRef] [PubMed]
- Hsia, R.Y.; Sabbagh, S.H.; Guo, J.; Nuckton, T.J.; Niedzwiecki, M.J. Trends in the utilisation of emergency departments in california, 2005–2015: A retrospective analysis. BMJ Open 2018, 8. [Google Scholar] [CrossRef] [PubMed]
- Taubman, S.L.; Allen, H.L.; Wright, B.J.; Baicker, K.; Finkelstein, A.N. Medicaid increases emergency-department use: Evidence from oregon’s health insurance experiment. Science 2014, 343, 263–268. [Google Scholar] [CrossRef] [PubMed]
- Uscher-Pines, L.; Pines, J.; Kellermann, A.; Gillen, E.; Mehrotra, A. Emergency department visits for nonurgent conditions: Systematic literature review. Am. J. Manag. Care 2013, 19, 47–59. [Google Scholar] [PubMed]
- Carret, M.L.V.; Fassa, A.G.; Domingues, M.R. Inappropriate use of emergency services: A systematic review of prevalence and associated factors. Cad. De Saude Publica 2009, 25, 7–28. [Google Scholar] [CrossRef]
- O’Keeffe, C.; Mason, S.; Jacques, R.; Nicholl, J. Characterising non-urgent users of the emergency department (ed): A retrospective analysis of routine ed data. PLoS ONE 2018, 13. [Google Scholar] [CrossRef] [PubMed]
- Kua, P.H.J.; Wu, L.; Ong, E.L.T.; Lim, Z.Y.; Yiew, J.L.; Thia, X.H.M.; Sung, S.C. Understanding decisions leading to nonurgent visits to the paediatric emergency department: Caregivers‘ perspectives. Singap. Med. J. 2016, 57, 314–319. [Google Scholar] [CrossRef] [PubMed]
- Hsia, R.Y.; Nath, J.B.; Baker, L.C. Emergency department visits by children, adolescents, and young adults in california by insurance status, 2005–2010. JAMA 2014, 312, 1587–1588. [Google Scholar] [CrossRef] [PubMed]
- Andrews, H.; Kass, L. Non-urgent use of emergency departments: Populations most likely to overestimate illness severity. Intern. Emerg. Med. 2018, 13, 893–900. [Google Scholar] [CrossRef] [PubMed]
- Colineaux, H.; Le Querrec, F.; Pourcel, L.; Gallart, J.C.; Azema, O.; Lang, T.; Kelly-Irving, M.; Charpentier, S.; Lamy, S. Is the use of emergency departments socially patterned? Int. J. Public Health 2018, 63, 397–407. [Google Scholar] [CrossRef] [PubMed]
- Durand, A.C.; Palazzolo, S.; Tanti-Hardouin, N.; Gerbeaux, P.; Sambuc, R.; Gentile, S. Nonurgent patients in emergency departments: Rational or irresponsible consumers? Perceptions of professionals and patients. BMC Res. Notes 2012, 5, 525. [Google Scholar] [CrossRef] [PubMed]
- Baier, N.; Geissler, A.; Bech, M.; Bernstein, D.; Cowling, T.E.; Jackson, T.; van Manen, J.; Rudkjobing, A.; Quentin, W. Emergency and urgent care systems in australia, denmark, england, france, germany and the Netherlands—Analyzing organization, payment and reforms. Health Policy 2019, 123, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.-C.; Yeh, H.-Y.; Wu, J.-C.; Haschler, I.; Chen, T.-J.; Wetter, T. Taiwan‘s national health insurance research database: Administrative health care database as study object in bibliometrics. Scientometrics 2011, 86, 365–380. [Google Scholar] [CrossRef]
- Billings, J.; Parikh, N.; Mijanovich, T. Emergency department use in new york city: A substitute for primary care? Issue Brief Commonw. Fund 2000, 433, 1–5. [Google Scholar]
- Chan, C.L.; Lin, W.; Yang, N.P.; Huang, H.T. The association between the availability of ambulatory care and non-emergency treatment in emergency medicine departments: A comprehensive and nationwide validation. Health Policy 2013, 110, 271–279. [Google Scholar] [CrossRef]
- Ballard, D.W.; Price, M.; Fung, V.; Brand, R.; Reed, M.E.; Fireman, B.; Newhouse, J.P.; Selby, J.V.; Hsu, J. Validation of an algorithm for categorizing the severity of hospital emergency department visits. Med. Care 2010, 48, 58–63. [Google Scholar] [CrossRef]
- Johnston, K.J.; Allen, L.; Melanson, T.A.; Pitts, S.R. A “patch” to the nyu emergency department visit algorithm. Health Serv. Res. 2017, 52, 1264–1276. [Google Scholar] [CrossRef]
- Chen, L.C.; Schafheutle, E.I.; Noyce, P.R. The impact of nonreferral outpatient co-payment on medical care utilization and expenditures in taiwan. Res. Soc. Adm. Pharm. 2009, 5, 211–224. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.; Jung, H.; Chou, P.; Kunihara, T.; Tosanguan, J.; Tang, Z.; Brydon, S.; Cook, G. From regulatory approval to subsidised patient access in the asia-pacific region: A comparison of systems across australia, china, japan, korea, new zealand, taiwan and thailand. Value Health 2014, 17, A794. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Chen, B.K.; Hibbert, J.; Cheng, X.; Bennett, K. Travel distance and sociodemographic correlates of potentially avoidable emergency department visits in california, 2006–2010: An observational study. Int. J. Equity Health 2015, 14, 8. [Google Scholar] [CrossRef] [PubMed]
- Gandhi, S.O.; Sabik, L. Emergency department visit classification using the nyu algorithm. Am. J. Manag. Care 2014, 20, 315–320. [Google Scholar] [PubMed]
- Chen, W.W.; Waters, T.M.; Chang, C.F. Insurance impact on nonurgent and primary care-sensitive emergency department use. Am. J. Manag. Care 2015, 21, 210–217. [Google Scholar]
- Tsai, J.C.H.; Chen, W.Y.; Liang, Y.W. Nonemergent emergency department visits under the national health insurance in taiwan. Health Policy 2011, 100, 189–195. [Google Scholar] [CrossRef] [PubMed]
- Ben-Isaac, E.; Schrager, S.M.; Keefer, M.; Chen, A.Y. National profile of nonemergent pediatric emergency department visits. Pediatrics 2010, 125, 454–459. [Google Scholar] [CrossRef]
- Raven, M.C.; Lowe, R.A.; Maselli, J.; Hsia, R.Y. Comparison of presenting complaint vs discharge diagnosis for identifying “nonemergency” emergency department visits. JAMA 2013, 309, 1145–1153. [Google Scholar] [CrossRef]
- Graham, B.; Bond, R.; Quinn, M.; Mulvenna, M. Using data mining to predict hospital admissions from the emergency department. IEEE Access 2018, 6, 10458–10469. [Google Scholar] [CrossRef]
- Casalino, E.; Wargon, M.; Peroziello, A.; Choquet, C.; Leroy, C.; Beaune, S.; Pereira, L.; Bernard, J.; Buzzi, J.C. Predictive factors for longer length of stay in an emergency department: A prospective multicentre study evaluating the impact of age, patient‘s clinical acuity and complexity, and care pathways. Emerg. Med. J. 2014, 31, 361–368. [Google Scholar] [CrossRef]
- Scherer, M.; Luhmann, D.; Kazek, A.; Hansen, H.; Schafer, I. Patients attending emergency departments a cross-sectional study of subjectively perceived treatment urgency and motivation for attending. Dtsch. Arztebl. Int. 2017, 114, 645. [Google Scholar] [PubMed]
- Schumacher, J.R.; Hall, A.G.; Davis, T.C.; Arnold, C.L.; Bennett, R.D.; Wolf, M.S.; Carden, D.L. Potentially preventable use of emergency services the role of low health literacy. Med Care 2013, 51, 654–658. [Google Scholar] [CrossRef] [PubMed]
- Hsia, R.Y.; Friedman, A.B.; Niedzwiecki, M. Urgent care needs among nonurgent visits to the emergency department. JAMA Intern. Med. 2016, 176, 852–854. [Google Scholar] [CrossRef] [PubMed]
- Morgan, S.R.; Chang, A.M.; Alqatari, M.; Pines, J.M. Non-emergency department interventions to reduce ed utilization: A systematic review. Acad. Emerg. Med. 2013, 20, 969–985. [Google Scholar] [CrossRef] [PubMed]
- Yang, C.J.; Tsai, Y.C.; Tien, J.J. The impacts of persistent behaviour and cost-sharing policy on demand for outpatient visits by the elderly: Evidence from taiwan‘s national health insurance. Geneva Pap. Risk Insur.-Issues Pract. 2017, 42, 31–52. [Google Scholar] [CrossRef]
- Chen, W.Y.; Liang, Y.W.; Lin, Y.H. Npricing-out effect from possible user-fee policies under taiwan’s national health insurance. Expert Rev. Pharmacoecon. Outcomes Res. 2010, 10, 453–464. [Google Scholar] [CrossRef] [PubMed]
- Brousseau, D.C.; Nimmer, M.R.; Yunk, N.L.; Nattinger, A.B.; Greer, A. Nonurgent emergency-department care: Analysis of parent and primary physician perspectives. Pediatrics 2011, 127, E375–E381. [Google Scholar] [CrossRef]
- Mazza, D.; Pearce, C.; Joe, A.; Turner, L.R.; Brijnath, B.; Browning, C.; Shearer, M.; Lowthian, J. Emergency department utilisation by older people in metropolitan melbourne, 2008–2012: Findings from the reducing older patient‘s avoidable presentations for emergency care treatment (redirect) study. Aust. Health Rev. 2018, 42, 181–188. [Google Scholar] [CrossRef]
- Hwang, U.; Shah, M.N.; Han, J.H.; Carpenter, C.R.; Siu, A.L.; Adams, J.G. Transforming emergency care for older adults. Health Aff. 2013, 32, 2116–2121. [Google Scholar] [CrossRef]
- Gasperini, B.; Cherubini, A.; Pierri, F.; Barbadoro, P.; Fedecostante, M.; Prospero, E. Potentially preventable visits to the emergency department in older adults: Results from a national survey in italy. PloS ONE 2017, 12, 11. [Google Scholar] [CrossRef]
- McHale, P.; Wood, S.; Hughes, K.; Bellis, M.A.; Demnitz, U.; Wyke, S. Who uses emergency departments inappropriately and when—A national cross-sectional study using a monitoring data system. BMC Med. 2013, 11, 258. [Google Scholar] [CrossRef] [PubMed]
- Hsia, R.Y.; Niedzwiecki, M. Avoidable emergency department visits: A starting point. Int. J. Qual. Health Care 2017, 29, 642–645. [Google Scholar] [CrossRef] [PubMed]
- May, M.; Brousseau, D.C.; Nelson, D.A.; Flynn, K.E.; Wolf, M.S.; Lepley, B.; Morrison, A.K. Why parents seek care for acute illness in the clinic or the ed: The role of health literacy. Acad. Pediatr. 2018, 18, 289–296. [Google Scholar] [CrossRef] [PubMed]
- Mathison, D.J.; Chamberlain, J.M.; Cowan, N.M.; Engstrom, R.N.; Fu, L.D.Y.; Shoo, A.; Teach, S.J. Primary care spatial density and nonurgent emergency department utilization: A new methodology for evaluating access to care. Acad. Pediatr. 2013, 13, 278–285. [Google Scholar] [CrossRef] [PubMed]
- Fishman, J.; McLafferty, S.; Galanter, W. Does spatial access to primary care affect emergency department utilization for nonemergent conditions? Health Serv. Res. 2018, 53, 489–508. [Google Scholar] [CrossRef] [PubMed]
- Urbanoski, K.; Cheng, J.; Rehm, J.; Kurdyak, P. Frequent use of emergency departments for mental and substance use disorders. Emerg. Med. J. 2018, 35, 220–225. [Google Scholar] [CrossRef] [PubMed]
- Ohns, M.J.; Oliver-McNeil, S.; Nantais-Smith, L.M.; George, N.M. Nonurgent use of the emergency department by pediatric patients: A theory-guided approach for primary and acute care pediatric nurse practitioners. J. Pediatr. Health Care 2016, 30, 339–346. [Google Scholar] [CrossRef] [PubMed]
- Seeger, I.; Rupp, P.; Naziyok, T.; Rolker-Denker, L.; Rohrig, R.; Hein, A. Outpatient care in emergency departments and primary care services. A descriptive analysis of secondary data in a rural hospital. Med. Klin. Intensivmed. Und Notf. 2017, 112, 510–518. [Google Scholar] [CrossRef]
- Posocco, A.; Scapinello, M.P.; De Ronch, I.; Castrogiovanni, F.; Lollo, G.; Sergi, G.; Tomaselli, I.; Tonon, L.; Solmi, M.; Pescador, D.; et al. Role of out of hours primary care service in limiting inappropriate access to emergency department. Intern. Emerg. Med. 2018, 13, 549–555. [Google Scholar] [CrossRef]
- Bruni, M.L.; Mammi, I.; Ugolini, C. Does the extension of primary care practice opening hours reduce the use of emergency services? J. Health Econ. 2016, 50, 144–155. [Google Scholar] [CrossRef]
- Elder, E.; Johnston, A.N.B.; Crilly, J. Review article: Systematic review of three key strategies designed to improve patient flow through the emergency department. Emerg. Med. Australas. 2015, 27, 394–404. [Google Scholar] [CrossRef] [PubMed]
- Wesson, D.; Kitzman, H.; Halloran, K.H.; Tecson, K. Innovative population health model associated with reduced emergency department use and inpatient hospitalizations. Health Aff. 2018, 37, 543–550. [Google Scholar] [CrossRef] [PubMed]
| Characteristics | Emergent Visits | Non-Emergent ED Visits | |||
|---|---|---|---|---|---|
| n = 109,183 | (%) | n = 208,234 | (%) | p-Value | |
| Systematic-level factor | <0.001 | ||||
| 2000 | 72,624 | (27.1) | 49,381 | (23.7) | |
| 2005 | 95,635 | (35.7) | 72,348 | (34.7) | |
| 2010 | 99,469 | (37.2) | 86,405 | (41.5) | |
| Demographic factors | |||||
| Gender | <0.001 | ||||
| Female | 127,003 | (47.4) | 111,312 | (53.5) | |
| Male | 140,719 | (52.6) | 96,815 | (46.5) | |
| Age group | <0.001 | ||||
| 0–19 | 78,256 | (29.2) | 70,419 | (33.8) | |
| 20–39 | 67,189 | (25.1) | 52,477 | (25.2) | |
| 40–59 | 55,280 | (20.6) | 40,393 | (19.4) | |
| 60–79 | 48,729 | (18.2) | 33,726 | (16.2) | |
| 80– | 18,274 | (6.8) | 11,119 | (5.3) | |
| Comorbidities | <0.001 | ||||
| Charlson‘s index, mean, (SD) | 2.8 | (6.33) | 2.2 | (5.76) | |
| Socioeconomic factors | |||||
| Income level (NTD) | <0.001 | ||||
| Dependent | 109,087 | (40.7) | 93,241 | (44.8) | |
| 1–19999 | 89,431 | (33.4) | 61,322 | (29.5) | |
| 20000–39999 | 50,969 | (19.0) | 39,293 | (18.9) | |
| 40000– | 18,241 | (6.8) | 14,278 | (6.9) | |
| Geographical Residence | <0.001 | ||||
| Northern area | 137,985 | (51.5) | 103,466 | (49.7) | |
| East area | 9,771 | (3.6) | 6,090 | (2.9) | |
| Middle area | 45,387 | (17.0) | 38,390 | (18.4) | |
| Southern area | 74,585 | (27.9) | 60,188 | (28.9) | |
| Urbanization of living area | <0.001 | ||||
| Most urbanization | 75,390 | (28.2) | 58,356 | (28.0) | |
| More urbanization | 77,997 | (29.1) | 61,560 | (29.6) | |
| Middle urbanization | 47,178 | (17.6) | 37,252 | (17.9) | |
| Less urbanization | 38,749 | (14.5) | 30,436 | (14.6) | |
| Least urbanization | 28,414 | (10.6) | 20,530 | (9.9) | |
| Past health utilization in last year | |||||
| No. of hospitalizations | <0.001 | ||||
| None | 195,207 | (72.9) | 160,505 | (77.1) | |
| One time | 38,841 | (14.5) | 27,737 | (13.3) | |
| ≥ two times | 33,680 | (12.6) | 19,892 | (9.6) | |
| No. of ED visits | <0.001 | ||||
| None | 124,897 | (46.7) | 102,837 | (49.4) | |
| Low (1–2 times) | 90,953 | (34.0) | 70,450 | (33.8) | |
| High (≥3 times) | 51,878 | (19.4) | 34,847 | (16.7) | |
| No. of outpatient visits | <0.001 | ||||
| Low (0-11 times) | 96,740 | (36.1) | 76,866 | (36.9) | |
| Middle (12-26 times) | 86,096 | (32.2) | 68,418 | (32.9) | |
| High (≥ 27 times) | 84,892 | (31.7) | 62,850 | (30.2) | |
| No. of TCM outpatient visits 1 | <0.001 | ||||
| None | 185,426 | (69.3) | 141,928 | (68.2) | |
| Low (1–2 times) | 39,721 | (14.8) | 31,578 | (15.2) | |
| High (≥ 3 times) | 42,581 | (15.9) | 34,628 | (16.6) | |
| Hospital accreditation level | <0.001 | ||||
| Medical centers | 36,954 | (13.8) | 95,237 | (45.8) | |
| Metropolitan hospitals | 50,656 | (18.9) | 177,672 | (85.4) | |
| Local community hospitals | 21,573 | (8.1) | 93,770 | (45.1) | |
| Season | <0.001 | ||||
| Spring (Mar–May) | 69,444 | (25.9) | 52,606 | (25.3) | |
| Summer (Jun–Aug) | 66,096 | (24.7) | 55,362 | (26.6) | |
| Fall (Sep–Nov) | 60,918 | (22.8) | 46,896 | (22.5) | |
| Winter (Dec–Feb) | 71,270 | (26.6) | 53,270 | (25.6) | |
| Public holiday | <0.001 | ||||
| No (781 days) | 168,376 | (62.9) | 126,754 | (60.9) | |
| Yes (314 days) | 99,352 | (37.1) | 81,380 | (39.1) | |
| Day of the week | <0.001 | ||||
| Monday | 36,650 | (13.7) | 28,267 | (13.6) | |
| Tuesday | 33,885 | (12.7) | 25,950 | (12.5) | |
| Wednesday | 33,222 | (12.4) | 24,966 | (12.0) | |
| Thursday | 33,461 | (12.5) | 24,562 | (11.8) | |
| Friday | 33,582 | (12.5) | 25,178 | (12.1) | |
| Saturday | 40,349 | (15.1) | 31,139 | (15.0) | |
| Sunday | 56,579 | (21.1) | 48,072 | (23.1) | |
| Cost-sharing payment | <0.001 | ||||
| Yes | 221,614 | (82.8) | 170,475 | (81.9) | |
| Waived | 46,114 | (17.2) | 37,659 | (18.1) | |
| Characteristics | Adjusted Odds Ratios | |||
|---|---|---|---|---|
| AOR | (95 % C.I.) | p-Value | Sig. 1 | |
| Systematic-level factor | ||||
| 2000 | -ref- | |||
| 2005 | 1.12 | (1.10–1.14) | <0.001 | *** |
| 2010 | 1.30 | (1.28–1.32) | <0.001 | *** |
| Personal-level factors | ||||
| Demographic factors | ||||
| Gender | ||||
| Female | 1.27 | (1.26–1.29) | <0.001 | *** |
| Male | -ref- | |||
| Age group | ||||
| 0-19 | 1.36 | (1.32–1.40) | <0.001 | *** |
| 20-39 | 1.18 | (1.15–1.21) | <0.001 | *** |
| 40-59 | 1.12 | (1.09–1.16) | <0.001 | *** |
| 60-79 | 1.14 | (1.11–1.17) | <0.001 | *** |
| 80- | -ref- | |||
| Comorbidities | ||||
| Charlson‘s index | 1.00 | (1.00–1.00) | <0.001 | *** |
| Socioeconomic factors | ||||
| Income level (NTD) | ||||
| Dependent | 1.07 | (1.05–1.09) | <0.001 | *** |
| 1–19999 | -ref- | |||
| 20000–39999 | 1.05 | (1.03–1.07) | <0.001 | *** |
| 40000– | 1.12 | (1.09–1.15) | <0.001 | *** |
| Geographical Residence | ||||
| Northern area | 1.12 | (1.08–1.16) | <0.001 | *** |
| East area | -ref- | |||
| Middle area | 1.31 | (1.27–1.36) | <0.001 | *** |
| Southern area | 1.25 | (1.20–1.29) | <0.001 | *** |
| Urbanization of living area | ||||
| Most urbanization | 1.11 | (1.08–1.13) | <0.001 | *** |
| More urbanization | 1.11 | (1.08–1.13) | <0.001 | *** |
| Middle urbanization | 1.08 | (1.05–1.10) | <0.001 | *** |
| Less urbanization | 1.07 | (1.05–1.10) | <0.001 | *** |
| Least urbanization | -ref- | |||
| Past health utilization in last year | ||||
| No. of hospitalizations | ||||
| None | 1.20 | (1.17–1.23) | <0.001 | *** |
| One time | 1.11 | (1.08–1.13) | <0.001 | *** |
| ≥ two times | -ref- | |||
| No. of ED visits | ||||
| None | 1.11 | (1.09–1.13) | <0.001 | *** |
| Low (1–2 times) | 1.06 | (1.04–1.08) | <0.001 | *** |
| High (≥3 times) | -ref- | |||
| No. of outpatient visits | ||||
| Low (0–11 times) | -ref- | |||
| Middle (12–26 times) | 1.02 | (1.00–1.03) | 0.03 | * |
| High (≥ 27 times) | 1.04 | (1.02–1.06) | <0.001 | *** |
| No. of TCM outpatient visits 2 | ||||
| None | -ref- | |||
| Low (1–2 times) | 1.04 | (1.02–1.05) | <0.001 | *** |
| High (≥ 3 times) | 1.05 | (1.04–1.07) | <0.001 | *** |
| ED visit-level factors | ||||
| Hospital accreditation level | ||||
| Medical centers | -ref- | |||
| Metropolitan hospitals | 1.14 | (1.12–1.16) | <0.001 | *** |
| Local community hospitals | 1.16 | (1.14–1.17) | <0.001 | *** |
| Season | ||||
| Spring (Mar–May) | 1.02 | (1.00–1.04) | 0.02 | * |
| Summer (Jun–Aug) | 1.13 | (1.12–1.15) | <0.001 | *** |
| Fall (Sep–Nov) | 1.05 | (1.03–1.06) | <0.001 | *** |
| Winter (Dec–Feb) | -ref- | |||
| Public holiday | ||||
| No | -ref- | |||
| Yes | 1.02 | (1.02–1.05) | 0.056 | |
| Day of the Week | ||||
| Monday | 1.05 | (1.02–1.07) | <0.001 | *** |
| Tuesday | 1.04 | (1.02–1.06) | 0.001 | ** |
| Wednesday | 1.02 | (1.02–1.06) | 0.129 | |
| Thursday | -ref- | |||
| Friday | 1.02 | (1.00–1.04) | 0.091 | |
| Saturday | 1.02 | (0.99–1.05) | 0.131 | |
| Sunday | 1.09 | (1.06–1.12) | <0.001 | *** |
| Cost-sharing payment | ||||
| Yes | -ref- | |||
| Waived | 1.14 | (1.12–1.16) | <0.001 | *** |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Huang, L.-C.; Chung, W.-F.; Liu, S.-W.; Wu, J.-C.; Chen, L.-F.; Chen, Y.-C. Characteristics of Non-Emergent Visits in Emergency Departments: Profiles and Longitudinal Pattern Changes in Taiwan, 2000–2010. Int. J. Environ. Res. Public Health 2019, 16, 1999. https://doi.org/10.3390/ijerph16111999
Huang L-C, Chung W-F, Liu S-W, Wu J-C, Chen L-F, Chen Y-C. Characteristics of Non-Emergent Visits in Emergency Departments: Profiles and Longitudinal Pattern Changes in Taiwan, 2000–2010. International Journal of Environmental Research and Public Health. 2019; 16(11):1999. https://doi.org/10.3390/ijerph16111999
Chicago/Turabian StyleHuang, Liang-Chung, Wu-Fu Chung, Shih-Wei Liu, Jau-Ching Wu, Li-Fu Chen, and Yu-Chun Chen. 2019. "Characteristics of Non-Emergent Visits in Emergency Departments: Profiles and Longitudinal Pattern Changes in Taiwan, 2000–2010" International Journal of Environmental Research and Public Health 16, no. 11: 1999. https://doi.org/10.3390/ijerph16111999
APA StyleHuang, L.-C., Chung, W.-F., Liu, S.-W., Wu, J.-C., Chen, L.-F., & Chen, Y.-C. (2019). Characteristics of Non-Emergent Visits in Emergency Departments: Profiles and Longitudinal Pattern Changes in Taiwan, 2000–2010. International Journal of Environmental Research and Public Health, 16(11), 1999. https://doi.org/10.3390/ijerph16111999






