Impact of the Case Management Model through Community Liaison Nurses
Abstract
:1. Introduction
2. Materials and Methods
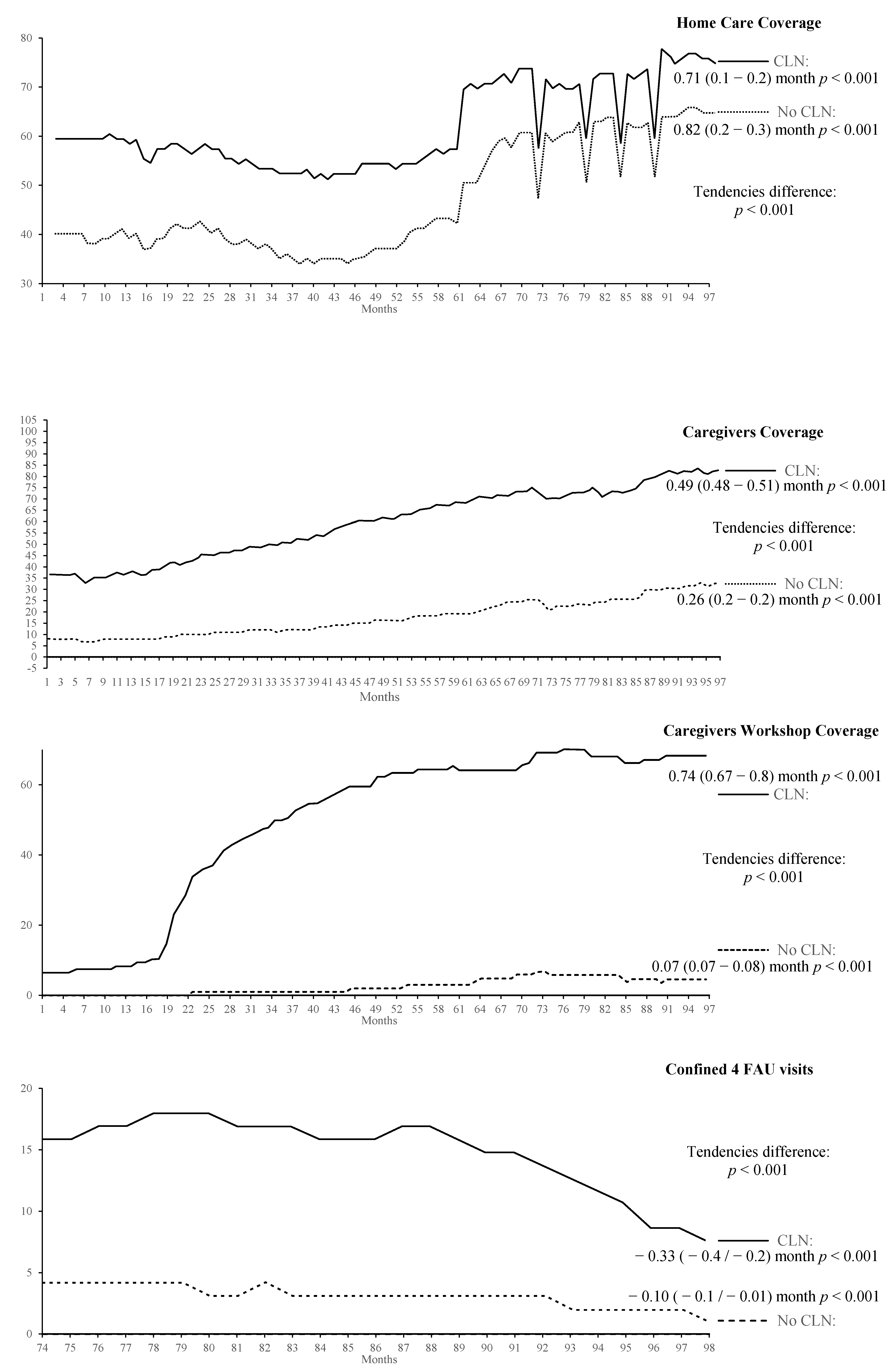
- Home care coverage: Relationship between home care persons included and expected (14% of those older than 65 years included). Terminal and immobilised patients aged less than 65 were included in the numerator.
- Coverage of caregivers for continuity care related to the confined: Percentage of caregivers regarding confined persons included in the Home Care Continuity Care Service.
- Coverage of workshops for caregivers: Percentage of caregivers included in the caregivers’ workshop.
- Confined with more than four visits to the Family Care Unit: Percentage of confined persons within the home care service who have had four or more home visits from physicians or nurses who are not liaison nurses in the last year.
- Social risk assessed by the social worker: Percentage of persons in social risk included in the Home Care Continuity Care Service who have been assessed by social workers.
- Hospitalisations: Percentage of hospital admissions in the last year among the people included in the quota as confined within the Home Care Continuity Care Service.
- Pressure ulcers: Percentage of patients with pressure ulcers among the people included in the quota as confined within the Home Care Continuity Care Service.
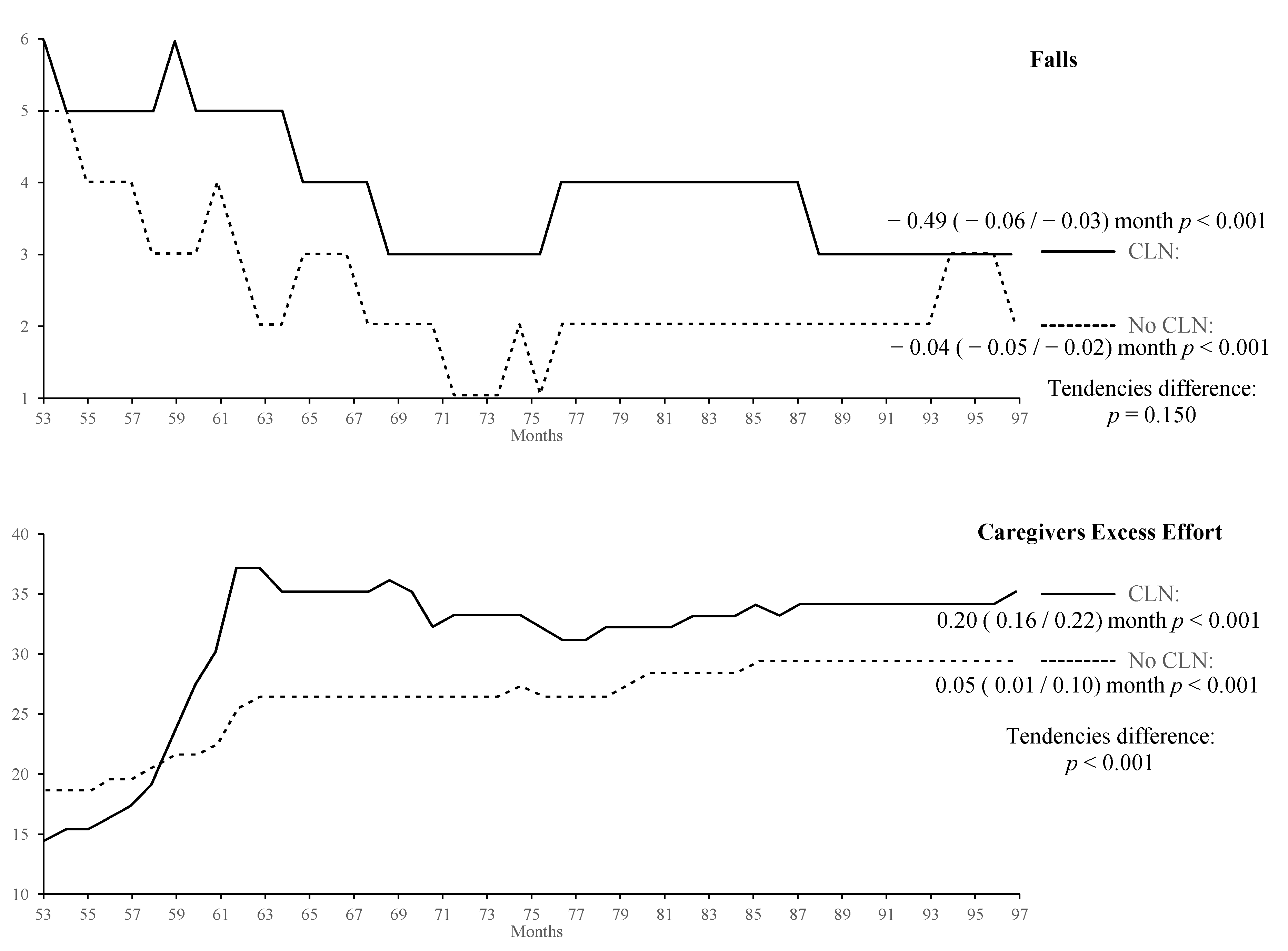
- Falls: Percentage of patients with falls among the people included in the quota as confined within the Home Care Continuity Care Service.
- Excess effort of caregivers: Percentage of patients with caregiver’s excess effort among the people included in the quota as caregivers in the Home Care Continuity Care Service.
Data Processing
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Ross, S.; Curry, N.; Goodwin, N. Case Management: What It Is and How It Can Best Be Implemented. 2011. Available online: http://www.kingsfund.org.uk/sites/files/kf/Case-Management-paper-The-Kings-Fund-Paper-November-2011_0.pdf (accessed on 3 October 2018).
- Hutt, R.; Rosen, R.; McCauley, J. Case-Managing Long-Term Conditions: What Impact Does It Have in the Treatment of Older People? 2004. Available online: https://www.kingsfund.org.uk/sites/default/files/casemanagement.pdf (accessed on 3 October 2018).
- Case Management Society of America (2008–11). What Is a Case Manager? Available online: www.cmsa.org/Home/CMSA/WhatisaCaseManager/tabid/224/Default.aspx (accessed on 3 October 2018).
- Duncan, J. Clinical observations on a failure in the antiseptic management of a case of empyema. Br. Med. J. 1878, 1, 476–478. [Google Scholar] [CrossRef]
- Bird, J.; Marks, I.M.; Lindley, P. Nurse therapists in psychiatry: Developments, controversies and implications. Br. J. Psychiatry 1979, 135, 321–329. [Google Scholar] [CrossRef]
- Grau, L. Case management and the nurse. Geriatr. Nurs. 1984, 5, 372–375. [Google Scholar] [CrossRef]
- Feachem, R.G.; Hogan, R.C.; Merson, M.H. Diarrhoeal disease control: Reviews of potential interventions. Bull. World Health Organ. 1983, 61, 637–640. [Google Scholar]
- Ferguson, J.A.; Weinberger, M. Case management programs in primary care. J. Gen. Intern. Med. 1998, 13, 123–126. [Google Scholar] [CrossRef]
- Casarin, S.N.A.; Villa, T.C.S.; Gonzáles, R.I.C.; de Freitas, M.C.; Caliri, M.H.L.; Sassaki, C.M. Case management: Evolution of the concept in the 80’s and 90’s. Rev. Lat. Am. Enfermagem. 2002, 10, 472–477. [Google Scholar] [CrossRef]
- Reimanis, C.L.; Cohen, E.L.; Redman, R. Nurse case manager role attributes: Fifteen years of evidence-based literature. Lippincotts Case Manag. 2001, 6, 230–239. [Google Scholar] [CrossRef]
- Krumholz, H.M.; Currie, P.M.; Riegel, B.; Phillips, C.O.; Peterson, E.D.; Smith, R.; Yancy, C.W.; Faxon, D.P.; American Heart Association Disease Management Taxonomy Writing Group. A taxonomy for disease management: A scientific statement from the American Heart Association Disease Management Taxonomy Writing Group. Circulation 2006, 114, 1432–1445. [Google Scholar] [CrossRef]
- Duarte, G.; Izquierdo, M.D.; Reyes, J.M. Análisis de la Situación y Líneas de Desarrollo de la Enfermería de Atención Primaria en Canarias; Servicio Canario de la Salud: Santa Cruz de Tenerife, Spain, 2000. [Google Scholar]
- Duarte-Clíments, G.; Sánchez-Gómez, M.B. Gestión de Casos en Atención Primaria: La Enfermera Comunitaria de Enlace Atención Comunitaria; Enfo Ediciones: Madrid, Spain, 2009. [Google Scholar]
- Pérez, R.M.; López, S.R.; Lacida, M.; Rodríguez, S. La Enfermera Comunitaria de Enlace en el Servicio Andaluz de Salud. Enferm. Comun. 2005, 1, 43–48. [Google Scholar]
- Duarte-Clíments, G.; Izquierdo-Mora, M.D.; Pérez-Díaz, G.; Aguirre-Jaime, A. La enfermera comunitaria de enlace, una propuesta para la mejora de la atención domiciliaria: Fundamento, modelo y evaluación de impacto. Revista Iberoamericana de Enfermería Comunitaria 2008, 1, 19–24. [Google Scholar]
- Contel-Segura, J.C.; Gené-Badía, J.; Peya-Gascons, M. Atención Domiciliaria: Organización y Práctica; Springer: Berlin, Germany, 1999. [Google Scholar]
- Fundación SAR. Calidad y Dependencia. Grados de Dependencia y Necesidad de Servicios. Ministerio de Trabajo y Asuntos Sociales. 2007. Available online: http://www.imsersodependencia.csic.es/documentacion/biblioteca/registro.htm?id=52409 (accessed on 15 October 2018).
- Dirección General de Programas Asistenciales Servicio de Atención Primaria. Planificación y Evaluación. Protocolo del Servicio de Continuidad de Cuidados para la Atención Domiciliaria; Servicio Canario de la Salud: San Cristóbal de La Laguna, Spain, 2006. [Google Scholar]
- Doughty, C. Effective models of mental health service provision and workforce configuration in the primary care setting. Christchurch: New Zealand Health Technology Assessment (NZHTA). NZHTA Tech. Brief Ser. 2006, 5. Available online: http://nzhta.chmeds.ac.nz/publications/mental_healthpc.pdf (accessed on 3 October 2018).
- Chiu, W.K.; Newcomer, R. A systematic review of nurse-assisted case management to improve hospital discharge transition outcomes for the elderly. Prof. Case Manag. 2007, 12, 330–336. [Google Scholar] [CrossRef]
- Oeseburg, B.; Wynia, K.; Middel, B.; Reijneveld, S.A. Effects of case management for frail older people or those with chronic illness: A systematic review. Nurs. Res. 2009, 58, 201–210. [Google Scholar] [CrossRef]
- You, E.C.; Dunt, D.; Doyle, C.; Hsueh, A. Effects of case management in community aged care on client and carer outcomes: A systematic review of randomized trials and comparative observational studies. BMC Health Serv. Res. 2012, 12, 395. [Google Scholar] [CrossRef]
- Trivedi, D.; Goodman, C.; Gage, H.; Baron, N.; Scheibl, F.; Iliffe, S.; Manthorpe, J.; Bunn, F.; Drennan, V. The effectiveness of inter-professional working for older people living in the community: A systematic review. Health Soc. Care Community 2013, 21, 113–128. [Google Scholar] [CrossRef]
- Keleher, H.; Parker, R.; Abdulwadud, O.; Francis, K. Systematic review of the effectiveness of primary care nursing. Int. J. Nurs. Pract. 2009, 15, 16–24. [Google Scholar] [CrossRef]
- Latour, C.H.; van der Windt, D.A.; de Jonge, P.; Riphagen, I.I.; de Vos, R.; Huyse, F.J.; Stalman, W.A. Nurse-led case management for ambulatory complex patients in general health care: A systematic review. J. Psychosom. Res. 2007, 62, 385–395. [Google Scholar] [CrossRef]
- Saxena, S.; Misra, T.; Car, J.; Netuveli, G.; Smith, R.; Majeed, A. Systematic review of primary healthcare interventions to improve diabetes outcomes in minority ethnic groups. J. Ambul. Care Manag. 2007, 30, 218–230. [Google Scholar] [CrossRef]
- Christensen, H.; Griffiths, K.M.; Gulliver, A.; Clack, D.; Kljakovic, M.; Wells, L. Models in the delivery of depression care: A systematic review of randomised and controlled intervention trials. BMC Fam. Pract. 2008, 9, 25–39. [Google Scholar] [CrossRef]
- Fraser, K.D.; Estabrooks, C. What factors influence case managers’ resource allocation decisions? A systematic review of the literature. Med. Decis. Mak. 2008, 28, 394–410. [Google Scholar] [CrossRef]
- Sutherland, D.; Hayter, M. Structured review: Evaluating the effectiveness of nurse case managers in improving health outcomes in three major chronic diseases. J. Clin. Nurs. 2009, 18, 2978–2992. [Google Scholar] [CrossRef]
- Young, T.; Busgeeth, K. Home-based care for reducing morbidity and mortality in people infected with HIV/AIDS. Cochrane Database Syst. Rev. 2010, CD005417. [Google Scholar] [CrossRef]
- Slyer, J.T.; Concert, C.M.; Eusebio, A.M.; Rogers, M.E.; Singleton, J. A systematic review of the effectiveness of nurse coordinated transitioning of care on readmission rates for patients with heart failure. JBI Database Syst. Rev. Implement. Rep. 2011, 9, 464–490. [Google Scholar] [CrossRef]
- Joo, J.Y.; Huber, D.L. An integrative review of case management for diabetes. Prof Case Manag. 2012, 17, 72–85. [Google Scholar] [CrossRef]
- Nurmatov, U.; Buckingham, S.; Kendall, M.; Murray, S.A.; White, P.; Sheikh, A.; Pinnock, H. Effectiveness of holistic interventions for people with severe chronic obstructive pulmonary disease: Systematic review of controlled clinical trials. PLoS ONE 2012, 7, e46433. [Google Scholar] [CrossRef]
- Thota, A.B.; Sipe, T.A.; Byard, G.J.; Zometa, C.S.; Hahn, R.A.; McKnight-Eily, L.R.; Chapman, D.P.; Abraido-Lanza, A.F.; Pearson, J.L.; Anderson, C.W.; et al. Collaborative care to improve the management of depressive disorders: A community guide systematic review and meta-analysis. Am. J. Prev. Med. 2012, 42, 525–538. [Google Scholar] [CrossRef]
- Coller, R.J.; Nelson, B.B.; Sklansky, D.J.; Saenz, A.A.; Klitzner, T.S.; Lerner, C.F.; Chung, P.J. Preventing hospitalizations in children with medical complexity: A systematic review. Pediatrics 2014, 134, e1628–e1647. [Google Scholar] [CrossRef] [PubMed]
- Joo, J.Y.; Huber, D.L. An integrative review of nurse-led community-based case management effectiveness. Int. Nurs. Rev. 2014, 61, 14–24. [Google Scholar] [CrossRef]
- Watts, S.A.; Lucatorto, M. A review of recent literature—Nurse case managers in diabetes care: Equivalent or better outcomes compared to primary care providers. Curr. Diab. Rep. 2014, 14, 504–517. [Google Scholar] [CrossRef] [PubMed]
- Martínez-González, N.A.; Berchtold, P.; Ullman, K.; Busato, A.; Egger, M. Integrated care programmes for adults with chronic conditions: A meta-review. Int. J. Qual. Health Care 2014, 26, 561–570. [Google Scholar] [CrossRef]
- Stokes, J.; Panagioti, M.; Alam, R.; Checkland, K.; Cheraghi-Sohi, S.; Bower, P. Effectiveness of case management for “At Risk” patients in primary care: A systematic review and meta-analysis. PLoS ONE 2015, 10, e0132340. [Google Scholar] [CrossRef]
- Holland, D.E.; Vnderboom, C.E.; Harder, T.M. Fostering cross-sector partnerships: Lessons learned from a community care team. Prof. Case Manag. 2019, 24, 66–75. [Google Scholar] [CrossRef]
- Morales-Asencio, J.M.; Cuevas-Fernández-Gallego, M.; Morilla-Herrera, J.C.; Martín-Santos, F.J.; Silvano Arranz, A.; Batres Siciliad, J.P.; Delgado-Romero, A.; Palacios-Gómez, L.; Cejudo López, A.; Kaknani-Uttumchandania, S. Characteristics of the provision of case management services in the community setting in Andalusia based on the RANGECOM registry. Enferm. Clin. 2019, 29, 67–73. [Google Scholar] [CrossRef]
- Jadad, A.R.; Cabrera, A.; Martos, F.; Smith, R.; Lyons, R.F. Modelos de Gestión de Enfermedades Crónicas Complejas, Capítulo 4 en: Cuando las Personas Viven con Múltiples Enfermedades Crónicas: Aproximación Colaborativa Hacia un Reto Global Emergente; Escuela Andaluza de Salud Pública: Granada, Spain, 2010. [Google Scholar]
- Solinís, R.N. Buenas prácticas en gestión sanitaria: El caso Kaiser Permanente. Rev. Adm. Sanit. 2007, 5, 283–292. [Google Scholar]
- Van der Plas, A.G.; Onwuteaka-Philipsen, B.D.; Vissers, K.C.; Deliens, L.; Jansen, W.J.; Francke, A.L. Appraisal of cooperation with a palliative care case manager by general practitioners and community nurses: A cross-sectional questionnaire study. J. Adv. Nurs. 2016, 72, 147–157. [Google Scholar] [CrossRef]
- Vieira de Miranda Neto, M.; Rewa, T.; Marli Leonello, V.; de Campos Oliveira, M.A. Advanced practice nursing: A possibility for Primary Health Care? Rev. Bras Enferm. 2018, 71, 716–721. [Google Scholar] [CrossRef] [PubMed]
- Powell, R.E.; Doty, A.; Casten, R.J.; Rovner, B.W.; Rising, K.L. A qualitative analysis of interprofessional healthcare team members’ perceptions of patient barriers to healthcare engagement. BMC Health Serv. Res. 2016, 16, 493. [Google Scholar] [CrossRef] [PubMed]
- Park, J.; Wu, X.; Frogner, B.K.; Pittman, P. Does the patient-centered medical home model change staffing and utilization in the community health centers? Med. Care 2018, 56, 784–790. [Google Scholar] [CrossRef] [PubMed]
- Kamei, T.; Takahashi, K.; Omori, J.; Arimori, N.; Hishinuma, M.; Asahara, K.; Shimpuku, Y.; Ohashi, K.; Tashiro, J. Toward advanced nursing practice along with people-centered care partnership model for sustainable universal health coverage and universal access to health. Rev. Lat. Am. Enferm. 2017, 25, e2839. [Google Scholar] [CrossRef]
- Sochalski, J.; Jaarsma, T.; Krumholz, H.M.; Laramee, A.; McMurray, J.J.; Naylor, M.D.; Rich, M.W.; Riegel, B.; Stewart, S. What works in chronic care management: The case of heart failure. Health Aff. 2009, 28, 179–189. [Google Scholar] [CrossRef]
- Sánchez-Gómez, M.B.; Ramos-Santana, S.; Gómez-Salgado, J.; Sánchez-Nicolás, F.; Moreno-Garriga, C.; Duarte-Clíments, G. Benefits of advanced practice nursing for its expansion in the Spanish context. Int. J. Environ. Res. Public Health 2019, 16, 680. [Google Scholar] [CrossRef] [PubMed]


© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Duarte-Climents, G.; Sánchez-Gómez, M.B.; Rodríguez-Gómez, J.Á.; Rodríguez-Álvarez, C.; Sierra-López, A.; Aguirre-Jaime, A.; Gómez-Salgado, J. Impact of the Case Management Model through Community Liaison Nurses. Int. J. Environ. Res. Public Health 2019, 16, 1894. https://doi.org/10.3390/ijerph16111894
Duarte-Climents G, Sánchez-Gómez MB, Rodríguez-Gómez JÁ, Rodríguez-Álvarez C, Sierra-López A, Aguirre-Jaime A, Gómez-Salgado J. Impact of the Case Management Model through Community Liaison Nurses. International Journal of Environmental Research and Public Health. 2019; 16(11):1894. https://doi.org/10.3390/ijerph16111894
Chicago/Turabian StyleDuarte-Climents, Gonzalo, María Begoña Sánchez-Gómez, José Ángel Rodríguez-Gómez, Cristobalina Rodríguez-Álvarez, Antonio Sierra-López, Armando Aguirre-Jaime, and Juan Gómez-Salgado. 2019. "Impact of the Case Management Model through Community Liaison Nurses" International Journal of Environmental Research and Public Health 16, no. 11: 1894. https://doi.org/10.3390/ijerph16111894
APA StyleDuarte-Climents, G., Sánchez-Gómez, M. B., Rodríguez-Gómez, J. Á., Rodríguez-Álvarez, C., Sierra-López, A., Aguirre-Jaime, A., & Gómez-Salgado, J. (2019). Impact of the Case Management Model through Community Liaison Nurses. International Journal of Environmental Research and Public Health, 16(11), 1894. https://doi.org/10.3390/ijerph16111894






