Overexpression of LGR-5 as a Predictor of Poor Outcome in Patients with Hepatocellular Carcinoma
Abstract
1. Introduction
2. Patients and Methods
2.1. Patients
2.2. IHC and Scoring
2.3. Statistical Analysis
3. Results
3.1. Patient Characteristics
3.2. LGF-5 Expression
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Hung, T.H.; Liang, C.M.; Hsu, C.N.; Tai, W.C.; Tsai, K.L.; Ku, M.K.; Wang, J.W.; Tseng, K.L.; Yuan, L.T.; Nguang, S.H.; et al. Association between complicated liver cirrhosis and the risk of hepatocellular carcinoma in Taiwan. PLoS ONE 2017, 12, e0181858. [Google Scholar] [CrossRef]
- Kim, G.A.; Lee, H.C.; Choe, J.; Kim, M.J.; Lee, M.J.; Chang, H.S.; Bae, I.Y.; Kim, H.K.; An, J.; Shim, J.H.; et al. Association between non-alcoholic fatty liver disease and cancer incidence rate. J. Hepatol. 2017. [Google Scholar] [CrossRef] [PubMed]
- Huang, Y.T.; Yang, H.I.; Liu, J.; Lee, M.H.; Freeman, J.R.; Chen, C.J. Mediation Analysis of Hepatitis B and C in Relation to Hepatocellular Carcinoma Risk. Epidemiology 2016, 27, 14–20. [Google Scholar] [CrossRef] [PubMed]
- Wu, M.Y.; Yiang, G.T.; Cheng, P.W.; Chu, P.Y.; Li, C.J. Molecular Targets in Hepatocarcinogenesis and Implications for Therapy. J. Clin. Med. 2018, 7, 213. [Google Scholar] [CrossRef] [PubMed]
- Zhou, Y.; Wang, B.; Wu, J.; Zhang, C.; Zhou, Y.; Yang, X.R.; Zhou, J.; Guo, W.; Fan, J. Association of preoperative EpCAM Circulating Tumor Cells and peripheral Treg cell levels with early recurrence of hepatocellular carcinoma following radical hepatic resection. BMC Cancer 2016, 16, 506. [Google Scholar] [CrossRef] [PubMed]
- Yu, G.P.; Xiao, Q.Y.; Shi, Z.Q.; Tang, L.S.; Ma, X.P.; Zhang, L.Y.; Chen, H.T.; Wang, W.J.; Zhang, P.Y.; Ding, D.L.; et al. Genetic polymorphisms in apoptosis-related genes and the prognosis of hepatocellular carcinoma. Am. J. Cancer Res. 2015, 5, 3249–3259. [Google Scholar] [PubMed]
- Cai, J.; Li, B.; Zhu, Y.; Fang, X.; Zhu, M.; Wang, M.; Liu, S.; Jiang, X.; Zheng, J.; Zhang, X.; et al. Prognostic Biomarker Identification Through Integrating the Gene Signatures of Hepatocellular Carcinoma Properties. EBioMedicine 2017, 19, 18–30. [Google Scholar] [CrossRef] [PubMed]
- Song, B.N.; Chu, I.S. A gene expression signature of FOXM1 predicts the prognosis of hepatocellular carcinoma. Exp. Mol. Med. 2018, 50, e418. [Google Scholar] [CrossRef] [PubMed]
- Ko, C.J.; Li, C.J.; Wu, M.Y.; Chu, P.-Y. Overexpression of Epithelial Cell Adhesion Molecule as a Predictor of Poor Outcome in Patients with Hepatocellular Carcinom. Exp. Ther. Med. 2018, 16, 4810–4816. [Google Scholar] [CrossRef] [PubMed]
- Al-Kharusi, M.R.; Smartt, H.J.; Greenhough, A.; Collard, T.J.; Emery, E.D.; Williams, A.C.; Paraskeva, C. LGR5 promotes survival in human colorectal adenoma cells and is upregulated by PGE2: Implications for targeting adenoma stem cells with NSAIDs. Carcinogenesis 2013, 34, 1150–1157. [Google Scholar] [CrossRef] [PubMed]
- McClanahan, T.; Koseoglu, S.; Smith, K.; Grein, J.; Gustafson, E.; Black, S.; Kirschmeier, P.; Samatar, A.A. Identification of overexpression of orphan G protein-coupled receptor GPR49 in human colon and ovarian primary tumors. Cancer Biol. Ther. 2006, 5, 419–426. [Google Scholar] [CrossRef] [PubMed]
- Tanese, K.; Fukuma, M.; Yamada, T.; Mori, T.; Yoshikawa, T.; Watanabe, W.; Ishiko, A.; Amagai, M.; Nishikawa, T.; Sakamoto, M. G-protein-coupled receptor GPR49 is up-regulated in basal cell carcinoma and promotes cell proliferation and tumor formation. Am. J. Pathol. 2008, 173, 835–843. [Google Scholar] [CrossRef] [PubMed]
- Hou, M.F.; Chen, P.M.; Chu, P.Y. LGR5 overexpression confers poor relapse-free survival in breast cancer patients. BMC Cancer 2018, 18, 219. [Google Scholar] [CrossRef] [PubMed]
- Becker, L.; Huang, Q.; Mashimo, H. Lgr5, an intestinal stem cell marker, is abnormally expressed in Barrett’s esophagus and esophageal adenocarcinoma. Diseases Esophagus 2010, 23, 168–174. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.L.; Chen, P.M.; Lin, P.Y.; Hsiau, Y.T.; Chu, P.Y. ABCG2 Overexpression Confers Poor Outcomes in Hepatocellular Carcinoma of Elderly Patients. Anticancer Res. 2016, 36, 2983–2988. [Google Scholar] [PubMed]
- Yu, H.C.; Hung, M.H.; Chen, Y.L.; Chu, P.Y.; Wang, C.Y.; Chao, T.T.; Liu, C.Y.; Shiau, C.W.; Chen, K.F. Erlotinib derivative inhibits hepatocellular carcinoma by targeting CIP2A to reactivate protein phosphatase 2A. Cell Death Disease 2014, 5, e1359. [Google Scholar] [CrossRef] [PubMed]
- Cao, H.Z.; Liu, X.F.; Yang, W.T.; Chen, Q.; Zheng, P.S. LGR5 promotes cancer stem cell traits and chemoresistance in cervical cancer. Cell Death Disease 2017, 8, e3039. [Google Scholar] [CrossRef] [PubMed]
- Liu, J.; Yu, G.Z.; Cheng, X.K.; Li, X.D.; Zeng, X.T.; Ren, X.Q. LGR5 promotes hepatocellular carcinoma metastasis through inducting epithelial-mesenchymal transition. Oncotarget 2017, 8, 50896–50903. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Chen, W.; Fu, Q.; Fang, F.; Fang, J.; Zhang, Q.; Hong, Y. Overexpression of leucine-rich repeat-containing G protein-coupled receptor 5 predicts poor prognosis in hepatocellular carcinoma. Saudi J. Biol. Sci. 2017. [Google Scholar] [CrossRef] [PubMed]


| Variables | Total | LGR-5 | p-Value | |
|---|---|---|---|---|
| Low Expression | High Expression | |||
| Age (years) | 63.0 ± 11.9 | 63.3 ± 12.2 | 62.6 ± 11.6 | 0.935 |
| Gender, n | ||||
| Female | 70 | 35 | 35 | 0.506 |
| Male | 282 | 128 | 154 | |
| Recurrence, n | ||||
| Negative | 291 | 135 | 156 | 1.000 |
| Positive | 61 | 28 | 33 | |
| Differentiation, n | ||||
| Well/ Moderate | 168 | 92 | 76 | 0.003 |
| Poor | 184 | 71 | 113 | |
| Clinical stage, n | ||||
| Stage I, II | 276 | 127 | 149 | 0.897 |
| Stage III, IV | 76 | 36 | 40 | |
| Tumor size, (mm) | 54.4 ± 46.0 | 56.5 ± 47.7 | 52.6 ± 44.7 | 0.319 |
| Child–Pugh score | 5.23 ± 0.73 | 5.21 ± 0.65 | 5.24 ± 0.78 | 0.545 |
| Survival days | 809.1 ± 418.7 | 800.1 ± 396.7 | 816.8 ± 437.9 | 0.029 |
| Survive, n | 298 | 146 | 152 | 0.018 |
| Hepatitis B, n | ||||
| Negative | 167 | 77 | 90 | 1.000 |
| Positive | 185 | 86 | 99 | |
| Hepatitis C, n | ||||
| Negative | 235 | 104 | 131 | 0.308 |
| Positive | 117 | 59 | 58 | |
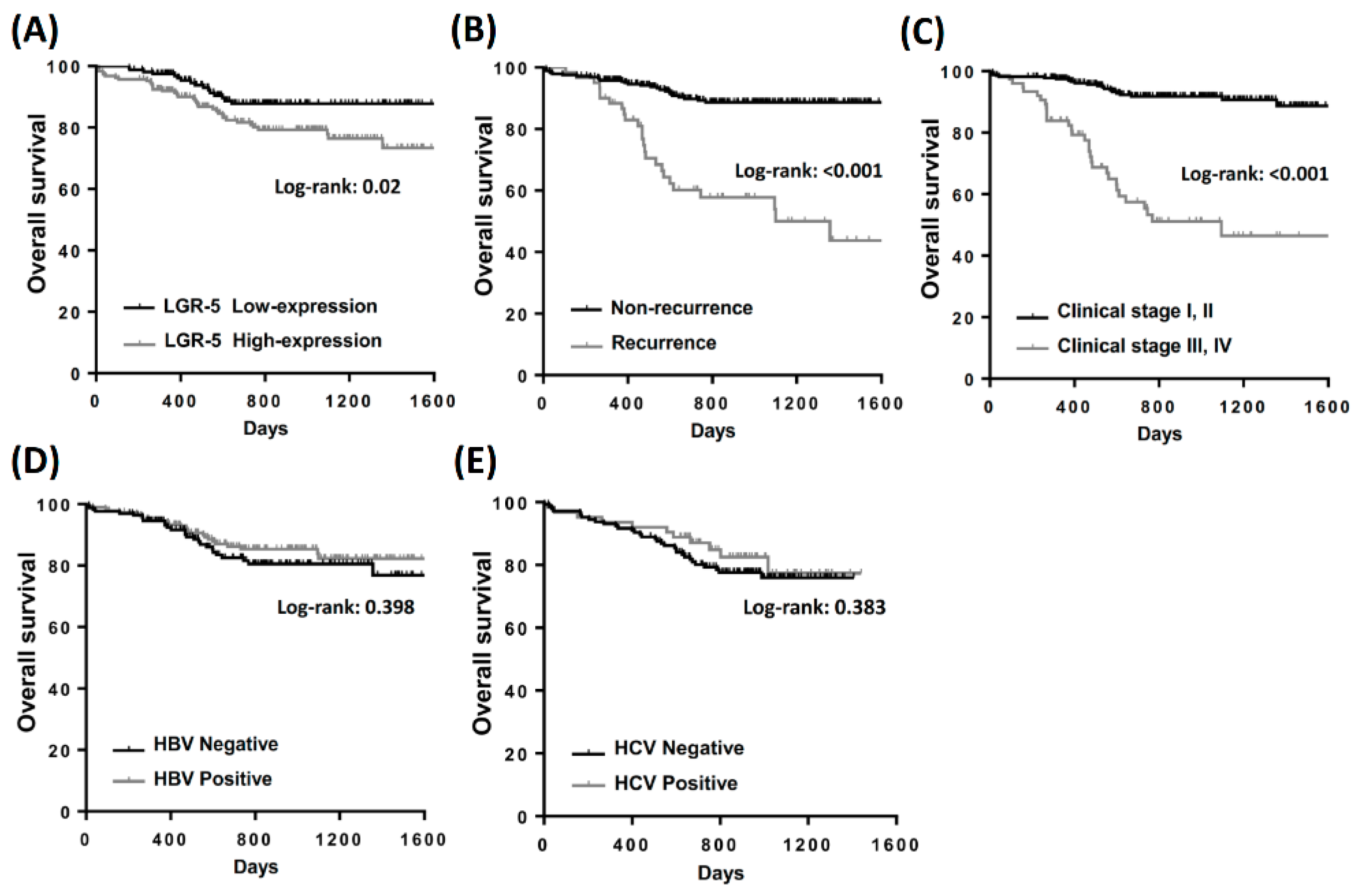
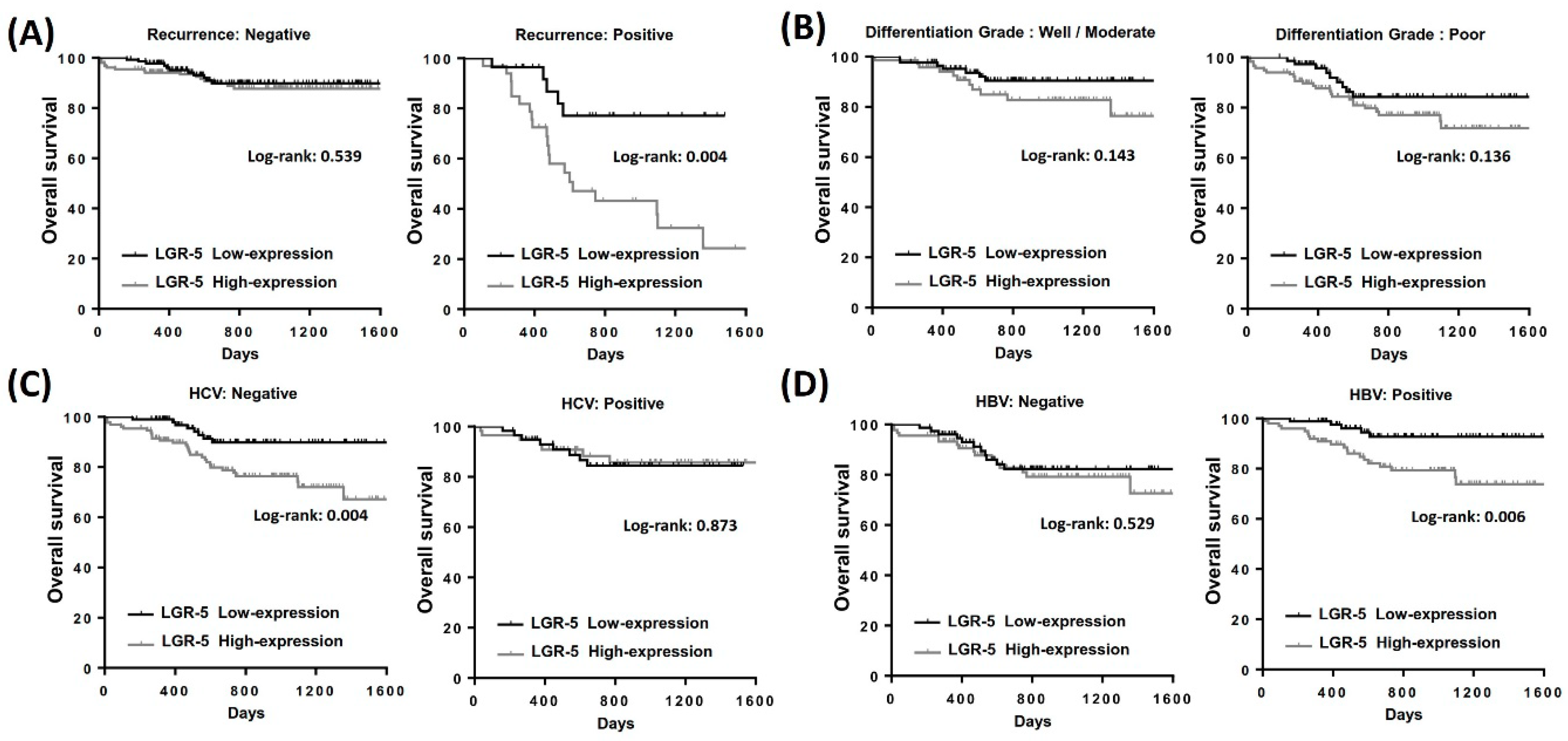
| Variables | Number | Overall Survival | Log-Rank | |
|---|---|---|---|---|
| Median Survival Days | Survival (%) | |||
| Gender | ||||
| Female | 70 | 845 | 91.4 | 0.068 |
| Male | 282 | 741 | 83.3 | |
| Recurrence | ||||
| Negative | 291 | 804 | 90.3 | <0.001 |
| Positive | 61 | 599 | 59.0 | |
| Differentiation | ||||
| Well/Moderate | 168 | 804 | 86.9 | 0.215 |
| Poor | 184 | 736 | 83.1 | |
| Clinical stage | ||||
| Stage I, II | 276 | 818 | 92.0 | <0.001 |
| Stage III, IV | 76 | 531 | 58.7 | |
| Hepatitis B | ||||
| Negative | 167 | 812 | 82.1 | 0.607 |
| Positive | 185 | 740 | 83.3 | |
| Hepatitis C | ||||
| Negative | 235 | 732 | 82.1 | 0.463 |
| Positive | 117 | 848 | 84.5 | |
| LGR-5 | ||||
| Low | 163 | 755 | 89.6 | 0.020 |
| High | 189 | 741 | 80.9 | |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ko, C.-J.; Li, C.-J.; Wu, M.-Y.; Chu, P.-Y. Overexpression of LGR-5 as a Predictor of Poor Outcome in Patients with Hepatocellular Carcinoma. Int. J. Environ. Res. Public Health 2019, 16, 1836. https://doi.org/10.3390/ijerph16101836
Ko C-J, Li C-J, Wu M-Y, Chu P-Y. Overexpression of LGR-5 as a Predictor of Poor Outcome in Patients with Hepatocellular Carcinoma. International Journal of Environmental Research and Public Health. 2019; 16(10):1836. https://doi.org/10.3390/ijerph16101836
Chicago/Turabian StyleKo, Chih-Jan, Chia-Jung Li, Meng-Yu Wu, and Pei-Yi Chu. 2019. "Overexpression of LGR-5 as a Predictor of Poor Outcome in Patients with Hepatocellular Carcinoma" International Journal of Environmental Research and Public Health 16, no. 10: 1836. https://doi.org/10.3390/ijerph16101836
APA StyleKo, C.-J., Li, C.-J., Wu, M.-Y., & Chu, P.-Y. (2019). Overexpression of LGR-5 as a Predictor of Poor Outcome in Patients with Hepatocellular Carcinoma. International Journal of Environmental Research and Public Health, 16(10), 1836. https://doi.org/10.3390/ijerph16101836







