Abstract
The 2016 U.S. Environmental Protection Agency (EPA) Integrated Risk Information System (IRIS) assessment for ethylene oxide (EO) estimated a 10−6 increased inhalation cancer risk of 0.1 parts per trillion, based on National Institute of Occupational Safety and Health (NIOSH) epidemiology studies of sterilization facility workers exposed to EO between 1938 and 1986. The worker exposure estimates were based on a NIOSH statistical regression (NSR) model “validated” with EO levels measured after 1978. Between 1938 and 1978, when EO data was unavailable, the NSR model predicts exposures lowest in 1938 increasing to peak levels in 1978. That increasing EO concentration trend arose, in part, because engineering/industrial-hygiene (E/IH) factors associated with evolving EO-sterilization equipment and operations before 1978 were not properly considered in the NSR model. To test the NSR model trend prediction, a new E/IH-based model was developed using historical data on EO kill concentrations, EO residue levels in sterilized materials, post-wash EO concentrations in a sterilization chamber, and information on facility characteristics and sterilizer operator practices from operators familiar with pre-1978 industry conditions. The E/IH 90th percentile of 8 h time-weighted average EO exposures (C90) for highly exposed sterilizer operators was calibrated to match 1978 C90 values from the NSR model. E/IH model C90 exposures were estimated to decrease over time from levels 16 and were four-fold greater than NSR-estimated exposures for workers during 1938–1954 and 1955–1964. This E/IH modeled trend is opposite to that of NSR model predictions of exposures before 1978, suggesting that EPA’s exclusive reliance on the NIOSH cohort to estimate EO cancer risk should be re-examined.
1. Introduction
In 2016, the U.S. Environmental Protection Agency (EPA) Integrated Risk Information System (IRIS) completed a cancer risk assessment of ethylene oxide (EO), concluding that human lifetime chronic respiratory exposure to EO poses a unit risk of 9.1 per part per trillion (ppt) in relation to increased combined risk of lymphoid and breast cancer. The EPA assessment implied a cancer slope of 0.005 (µg/m3)−1, and that exposure to 0.1 ppt EO to the general population may increase this risk by one chance in a million [1]. EPA’s conclusion was based on its re-analysis of epidemiology data from an industry-wide cohort study of 18,254 sterilization workers, undertaken by the National Institute of Occupational Safety and Health (NIOSH). This cohort includes 1,222 sterilizer operators—a highly exposed job category—in 14 plants from 1938 to 1986, with an average of 4.9 years of EO exposure and 16.1 years of follow-up [2,3,4]. Those sterilizer operators experienced an average respiratory EO exposure of 4.3 ppm between 1976 and 1985 based on 627 8 h time-weighted average (TWA) personal air samples from 13 plants, with most collected in the 1980s, during or after the introduction of engineering controls to reduce worker exposure. NIOSH determined that these data were sufficient to estimate corresponding historical exposures. The NIOSH cohort averaged 26.8 years of follow-up in an extended follow-up study through 1998, by which time 16% of the cohort had died [5].
Log-transformed EO exposures for the NIOSH cohort were estimated using a NIOSH-developed statistical regression (NSR) model. The NSR model was “validated” using 2700 TWA charcoal tube measurements for workers’ personal breathing zones in 18 sterilization facilities (13 of which included workers represented in the NIOSH cohort). Virtually all measurements were obtained during 1978–1985, with only seven mean (derived from 23 total) measurements made during 1976–1977, and no measurements obtained before 1976 [6,7]. Most of the air samples were obtained in the 1980s, about the time that engineering controls and new work practices designed to lower worker exposure levels were introduced. The data were divided into two sets, one for developing the NSR model and the second for testing it. Of 23 independent variables tested for model inclusion, seven were determined to be significant (p ≤ 0.10) predictors of EO exposure and included in the final NSR model: job category, type of product sterilized, rear exhaust, aeration, days since product sterilization, sterilizer volume, and calendar year. Five of these variables were linear predictors, two (sterilizer volume and calendar year) were linear quadratic predictors, each representing inverted parabolic predicted contributions to exposure, with maximum predicted contributions at calendar year = 1978 and sterilizer volume = 1000 ft3. Sterilizer volume and calendar year were determined to have the greatest exposure predictivity for the period when measurements were also available [7].
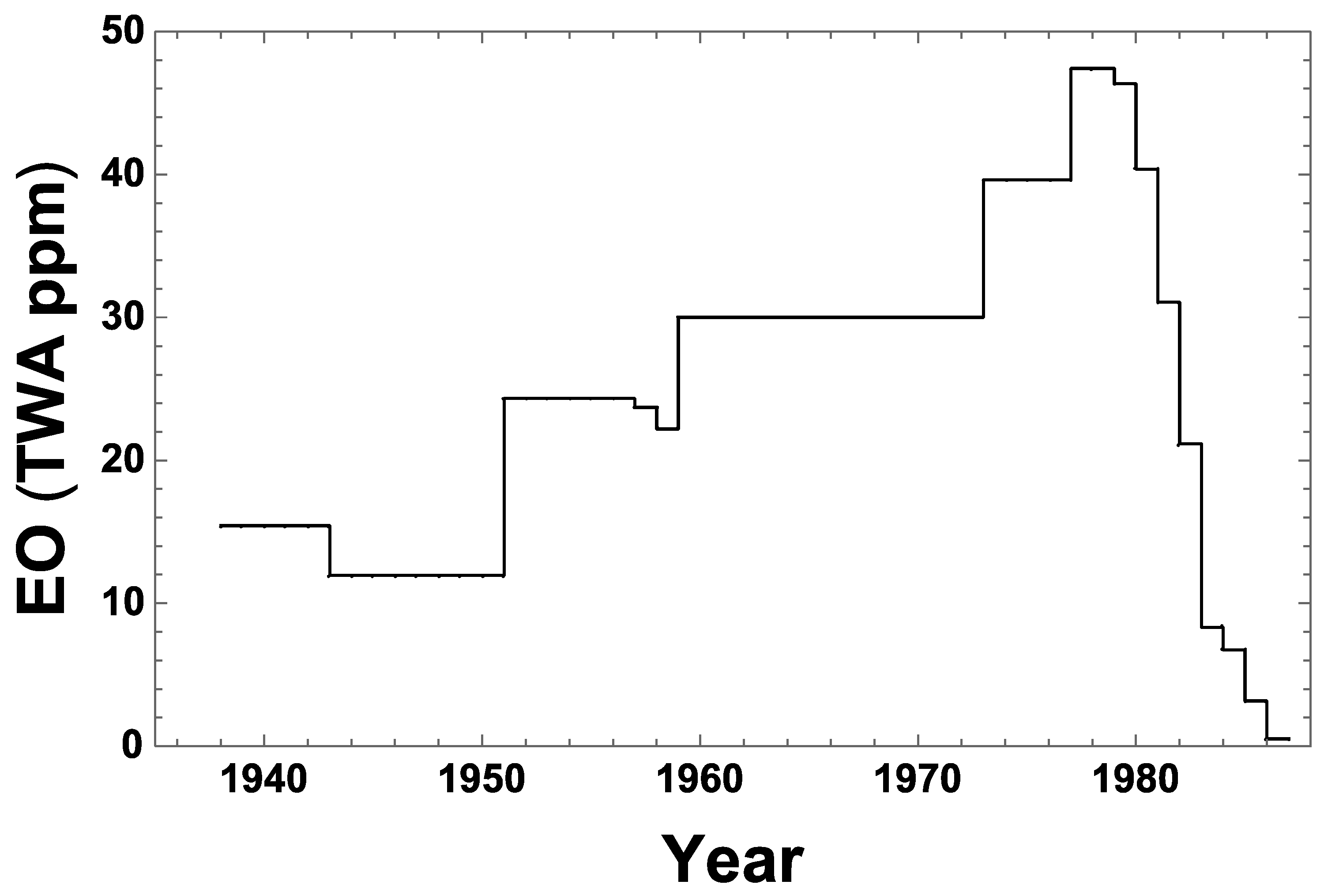
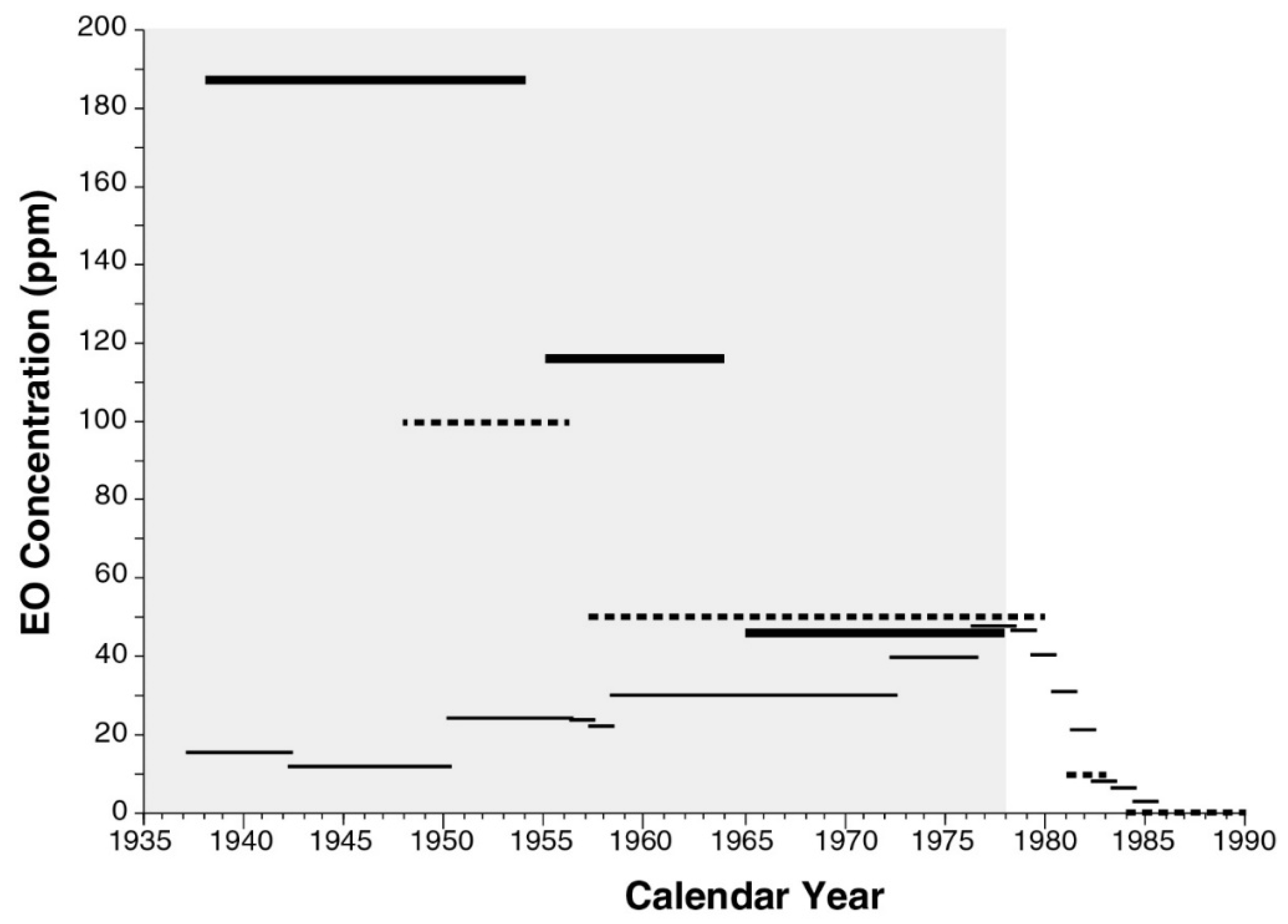
The resulting fitted NSR model explains 85% of the variation in measured TWA EO exposure levels used to validate the model [7]. However, this model was applied by NIOSH conditional on year = max (1978, calendar year), thus ignoring for the years before 1978 the inverse parabolic fit NIOSH obtained for available EO measurement data specifically in relation to calendar year. It was this conditional model that NIOSH applied to estimate exposure levels for all periods, facilities, and job categories [7]. Figure 1 plots the resulting NSR estimates of the annual 90th percentile values of occupational, 8 h TWA EO inhalation exposure (C90), relative to values of all facility and job category-specific EO exposure levels represented in the NIOSH cohort data set. This figure shows a clearly increasing EO concentration trend during 1938–1978, similar to the C90 trend estimated for NIOSH cohort cases calculated by EPA (USEPA 2016 [1], Appendix D-5, Figure D-23 on p. D 67). The increasing trend in estimated EO exposures during 1938–1978 was recognized by EPA as being due to two combined factors: sterilizer volumes tended to increase during that period, and measured (nearly all post-1977) EO levels were determined by NIOSH to fit best to an inverse parabolic function of sterilizer volume [1] (Appendix I, pp. I-26–I-27). However, these two factors are likely coincidental, insofar as they are not linked directly by data available during the earlier period. It was not the volume of each sterilizer used that determined total EO usage in a facility, but rather the capacity and utilization of all sterilizers combined in that facility. The EO concentrations experienced depended not only on the EO mass used, but also on the volumes and air turnover rates of rooms in which sterilization and storage of sterilized materials took place. It is reasonable to assume that during earlier decades when fewer sterilizers were operated using less total EO mass to treat smaller total masses of products, correspondingly smaller facilities were used for this purpose. Moreover, the NSR model did not directly address other substantial changes in pre-1978 sterilizer facilities and operations that may have reduced EO exposures during that period, when industrial hygiene EO data were either very limited (1976–1977) or unavailable (pre-1976), as a direct basis to verify pre-1978 NSR model predictions.
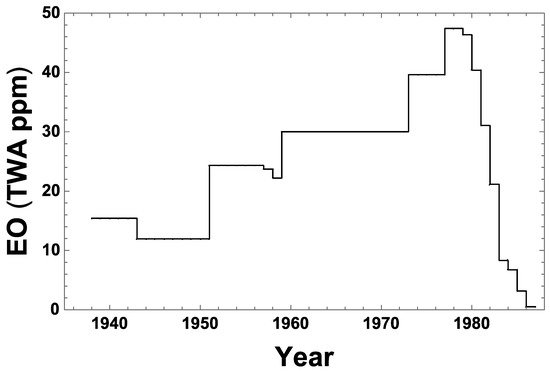
Figure 1.
National Institute of Occupational Safety and Health (NIOSH) statistical regression (NSR) exposure model predictions of historical 90th percentile 8-h time-weighted average (TWA) occupational ethylene oxide (EO) concentration (C90) during 1936–1986, specific to all facilities and job categories addressed by that model. Nearly all of the facilities sterilized medical/health products. The NSR model predicts that C90 = 47.4, 30.0, and 11.9 ppm in 1978, 1959, and 1949, respectively, and predicts TWA C90 values of 34.3, 27.5, and 15.9 ppm during the late, middle, and early periods defined for the present study, respectively.
After reviewing a limited set of NSR-model predictions showing an increasing trend in predicted EO levels during 1938–1978, an EPA Science Advisory Board concluded that such “surprising historical behavior” was “unlikely” [8]. It was well recognized by others at NIOSH that before the late 1970s, EO exposures among sterilizer workers “were likely to have been higher … before installation of engineering controls, when the OSHA standard was 50 ppm” [2]. Industrial hygiene data collected in other industries indicate historical occupational exposure levels as well as industrial exposure limits for nearly all chemical toxicants show generally decreasing historical trends in exposure concentrations since the establishment of corresponding industrial exposure guidelines, such as the American Council of Government and Industrial Hygienists (ACGIH) threshold limit value (TLV) guidelines and regulatory limits such as OSHA regulations. For example, such trends are well documented for industries using perchloroethylene and/or trichloroethylene [9,10,11]. Such decreasing historical trends reflect improvements in technology sophistication, operational efficiency, knowledge concerning toxicological effects, and the implementation of workplace guidance values and standards. In the case of EO, such trends are reflected by the decrease in ACGIH 8 h TLVs for respiratory EO exposure over the period 1948–1984 [12] (see Table 1). Thus, the surprising historical pattern predicted by the NSR model indicates a need for closer examination.

Table 1.
Historical summary guidance values and standards for EO exposure.
A comprehensive re-examination of the intended basis of the NSR model is no longer possible, because the original data NIOSH used to develop that model no longer exist [1] (Appendix H, p. H-28). However, only a few personal air measurements were available during 1976–1977, and none were available before 1976. Consequently, this model’s surprising prediction that EO exposures generally increased historically through to 1978 remain effectively unvalidated. To better assess the reliability of pre-1978 NSR model predictions, an alternative engineering/industrial-hygiene (E/IH) factors-based model was developed, as described in the Materials and Methods section. This E/IH model uses historical data on measured EO residue levels in sterilized materials, post-wash EO concentrations in a sterilization chamber, and facility characteristics and sterilizer operator practices obtained by interviews with highly experienced former sterilizer operators, experts who were familiar with 1960s–1970s EO sterilization industry conditions. These interviews focused on EO-exposure conditions experienced by sterilizer operators, whose tasks during that period involved among the highest EO exposures relative to those of other sterilization industry workers in facilities represented in the NIOSH cohort. For this reason, the E/IH model focused on predicting C90 as a measure of EO exposure for such relatively highly exposed workers, and was calibrated to match the NSR model prediction of C90 in 1978, the first year in which the NSR model was empirically validated using a large number of average measures of EO in personal air. Key assumptions of the E/IH model were then modified, as explained in the Materials and Methods section, to reflect operating conditions expected to be pertinent to medical/health products sterilization during each of the two earlier periods of sterilization industry operations we considered (1938–1954 and 1955–1964). In addition, a spice products sterilization scenario during the latest period was also examined, to provide insight on the other primary product type that is sterilized. To assess the plausibility of the NSR model, E/IH model predictions were compared with corresponding NSR model predictions, as shown in Figure 1. The primary objectives of this modeling study were to examine whether any historical trend (increasing, decreasing, or constant) is exhibited in the EO exposure levels estimated by the E/IH approach before 1978 and to compare the consistency of any such trend with results produced using the NSR model.
2. Materials and Methods
2.1. E/IH Model Focus
Modeling for the NIOSH sterilization worker cohort focused on operations involving medical/health products sterilized during three periods of industry development before 1978: 1938–1954 (Early Period), 1955–1964 (Middle Period), and 1965–1978 (Late Period). These operations are listed in Box 1. The beginning years of the Middle and Late periods were set to reflect an approximate seven year lag, reflecting time to implement technological and operational improvements after adoption of the initial and second ACGIH 8 h TLV exposure levels for EO of 100 ppm in 1948 and 50 ppm in 1957 [12] (see Table 1). In addition, a typical Late Period spice-sterilization facility operation was modeled. There was inadequate data to model for spice product operations in earlier years, although exposure trends would likely have been similar to those for medical health products, as operating conditions are believed to have been similar. The selected modeling scenarios reflect that most of the 14 facilities in the NIOSH cohort primarily sterilized medical/health-related products and supplies with EO, whereas three of the plants “treated spices with ethylene oxide and another manufactured and tested sterilizers with ethylene oxide” [4]. The periods addressed include all of the pre-1978 years for which NIOSH had no (pre-1976) or relatively few (1976–1977) average measures of personal air EO.
Box 1. Summary of EO Sterilization Operations (Activities Implemented to Conduct Historical EO Sterilization Operations).
- (1)
- Implanting efficacy test samples into selected boxes of materials on pallets to be sterilized
- (2)
- Loading pallets of materials to be sterilized into a chamber
- (3)
- Adding EO as a mixed or pure gas to the chamber to the desired level (kill concentration)
- (4)
- Running the chamber under the desired temperature and relative humidity conditions for a duration to achieve the desired level of microbial mortality
- (5)
- Exhausting some EO gas from chambers to in-room water traps (inefficient traps released EO into work room air)
- (6)
- In some cases, implementing air/nitrogen washes to reduce remaining EO concentrations in chamber air and residue levels in sterilized materials before unloading the chamber (no or few washes were used during the time frame of interest)
- (7)
- Unloading the processed materials from the chamber (released EO into work room air)
- (8)
- Removing test samples from boxes for efficacy analysis (operators in close contact with off-gassing packaging and materials emitting EO into work room air)
- (9)
- Transporting the sterilized materials to a storage area in or separate from the work room, and working in the storage area where materials remained until returned to customers (sterilized packaging and materials continue to off-gas during storage contributing additional EO to work room or storage room air)
2.2. E/IH Model Structure and Parameters
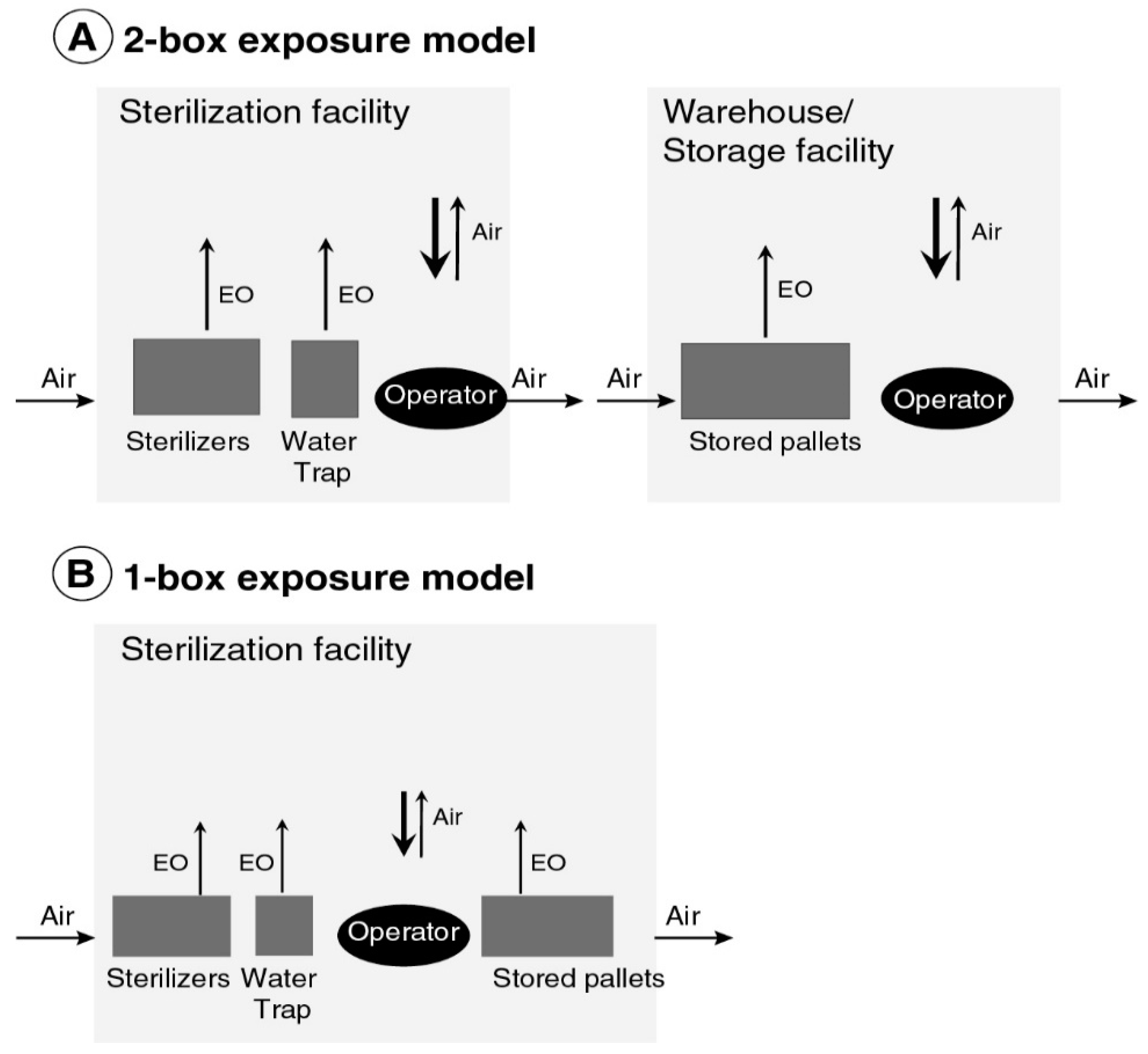
During each of the three periods examined, C90 was estimated to represent sterilizer operator exposures using either of two compartmental E/IH model structures summarized in Figure 2, which were parameterized as summarized in Table 2 and Table 3. Based on information from interviews with three highly experienced former sterilizer operators who initially worked in the late 1960s and early 1970s, and a group of current EO sterilization experts who provided both information and written materials to support modeling, the E/IH model structures used imply that historical sterilization worker exposures resulted from:
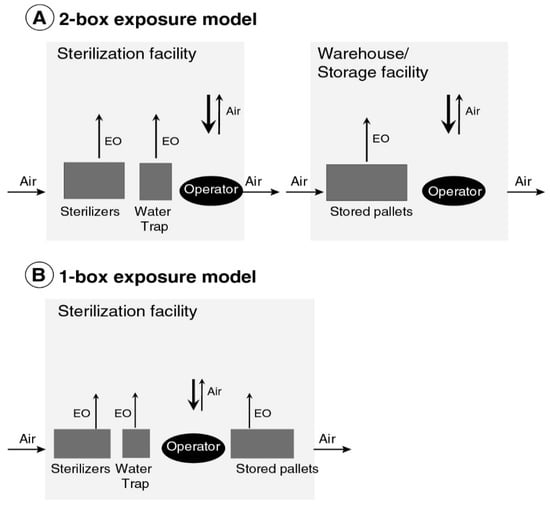
Figure 2.
Engineering/industrial-hygiene (E/IH) model of occupational respiratory exposure to EO used to sterilize (A) medical/health products during the Late Period and (B) medical/health products during the Early and Middle periods, and spices during the Late Period.

Table 2.
Scenario assumptions applied for all modeled periods.

Table 3.
Scenario assumptions for specific periods of E/IH model application.
- accumulation of EO in a room in which sterilization operations occurred, resulting from emissions from chambers and water traps for exhausted gas;
Specifically, to model EO exposure in the Late Period medical/health sterilization scenario, two unlinked compartments were used for modeling total exposure: one representing the building volume in which sterilization occurred and one representing a separate warehouse or storage building in which pallets of sterilized materials removed from sterilizers were stored before delivery. In this case, 8 h TWA exposure was calculated as a weighted average of separate TWA exposures estimated for each compartment, using as weights the respective average fractions of a sterilizer operator’s 8 h shift spent in each compartment (Figure 2A, Table 3). To model EO exposure in each of the three other scenarios considered (Early and Middle Period medical/health scenarios and Late Period spices scenario), a one compartment model was used to estimate exposures, assuming that all pallets of sterilized materials were stored in the same building in which sterilization operations also occurred (Figure 2B).
In sterilization areas, the percentage 100Fch% of all sterilizer operations associated EO exposure was assumed to arise from the mass (Mair) of all post-cycle EO remaining in the chamber void space after the chamber doors were opened. The remaining percentage, 100(1–Fch)%, was assumed to arise from sterilizer leaks and periodic maintenance operations and from EO not captured by floor-level water-operated EO vapor traps. Many facilities used such traps to vent EO extracted from chambers during and/or just before opening a chamber door after completing the sterilization process [16]. The value of additional EO exposure was assumed to arise from the combined masses (Mprod and Mpack) of EO released after being adsorbed/absorbed during sterilization into (1) sterilized products and (2) cardboard packaging (medical/health scenario) or bags (spices scenario) in which products were loaded onto pallets. Scenario-specific estimates of Mair, Mprod, and Mpack are listed in Table 3.
To estimate C90, the 8 h TWA concentration of EO for each E/IH-model compartment was evaluated at the dynamic equilibrium (at which, by definition, the rates of input and output are equal), using Equation (1):
in which N is the number of input units per shift; M is the input 90th percentile EO mass (mg) per unit of input (pallet or chamber) (Mair or (Mpack + Mprod), depending on modeled input contribution); V is the compartment volume (m3); AEReff is the expected effective unitless air exchange rate; T is the shift duration and averaging period (8 h); A = 1 if M is Mair or 0 otherwise (i.e., if M is Mpack + Mprod); Fch is the fraction of chamber-associated EO exposure assumed to arise from mass Mair; and H is the EO concentration enhancement factor, due to the heavier-than-air density of EO.
Note that rates of dynamic (e.g., 1st order or 0 order) input do not appear in Equation (1), regardless of the complexity of the input patterns involved, provided that the air exchange rate (AER) is, on average, sufficiently large to ensure that dynamic equilibrium conditions are eventually closely approximated. The additional modeling assumptions and parameters listed in Table 2 and Table 3 were, as cited in these tables, based on relevant literature and/or interviews of sterilizer operators who began work in the late 1960s and early 1970s, as well as of other sterilization experts, who had detailed knowledge concerning earlier EO sterilizer industry facilities and operations. Information providing context for key modeling assumptions and parameters listed in Table 2 and Table 3 is discussed in the following subsections.
2.2.1. Compartment Volumes
During the modeled Late Period operations for medical/health products, the interview-based estimates listed in Table 2 and Table 3 indicate a daily sterilization room volume/pallet ratio (VPRSR) equal to 11,000 m3 (19 pallets/day). The analogous ratio (VPRWS) for warehouse/storage areas was equal to 8500 m3 (19 × 3 × 7 pallets/day), assuming 19 pallets/shift, three shifts/day, and an average of seven days of treated pallet storage before delivery. The E/IH-model compartment volumes during the Early and Middle periods listed in Table 3 (for which no separate pallet storage area was assumed) were estimated as the product of (VPRSR + VPRWS) and the assumed value of period-specific pallets/day, listed in Table 2. Thus, it was assumed that space utilization efficiency remained nearly constant over all modeled periods.
2.2.2. Air Exchange Rate
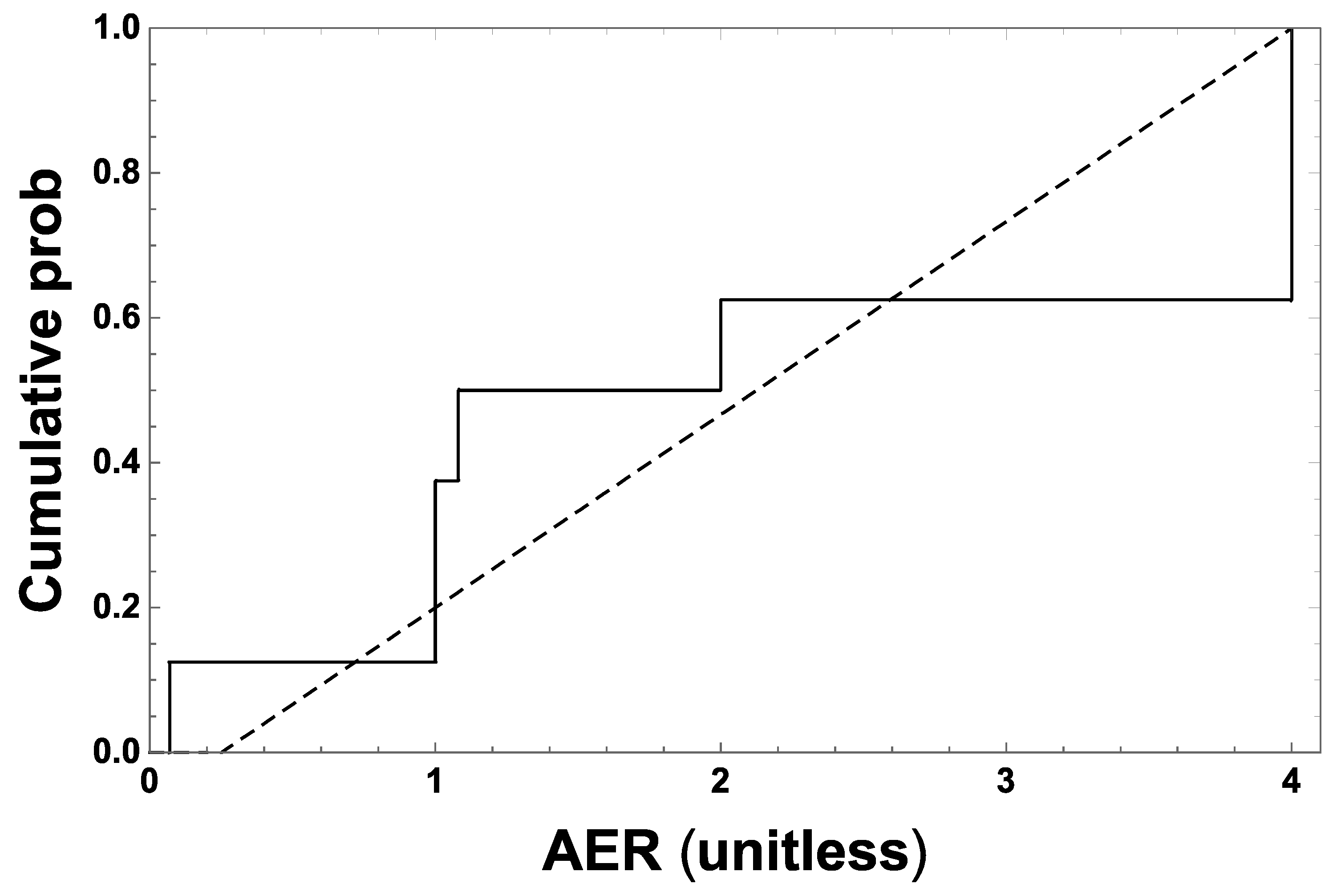
The air exchange rate (AER) applicable to sterilization and (if applicable) to separate warehouse/storage areas was assumed to be constant at the modeled facilities. Its estimated effective expected value (AEReff), applied over all modeled periods, was defined as the unbiased estimator in the multiplicative factor (1/AEReff) that appears in Equation (1). AER data for sterilization areas in 21 facilities that sterilized spices in the 1978–1981 period [16] indicate that forced-air ventilation was not widespread, even during that period and, where not used, was consistent with AER values approximately uniformly distributed between 0.25 and 4 per hour (Figure 3). This assumption implies that between these bounds, 1/AER has the cumulative probability distribution F(x) = (16 − 4/x)/15 and density f(x) = 4/(15 2), and thus that AEReff = 1/ = 15/(4 ln(16))/h = ~1.35/h.
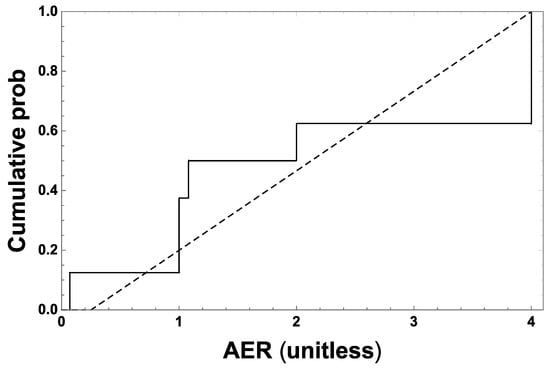
Figure 3.
Empirical cumulative distribution of the subset of air exchange rate (AER) values reported for sterilization rooms in the spice sterilization facilities listed in Appendix C-10 of Goldgraben and Zank [16], for which AER ≤ 4/h, representative of sterilization rooms assumed not to have used forced-air ventilation. The data are consistent with an approximately uniform AER distribution between 0.25 and 4 per hour, as assessed (p = 0.52) by the Kolmogorov one sample test [26].
2.2.3. EO Concentration in Sterilization Chambers
EO sterilization methods employed different concentrations of administered EO that varied over the periods considered. For example, the Mainz sterilization method involves a 10% EO:90% CO2 mixture at pressures of 3 to 6 atmospheres and temperatures of 35 to 65 °C, a 12% EO:88% halogenated hydrocarbon (e.g., freon) gas mixture introduced under pressure, and 100% EO introduced under vacuum [16,20,21,22,27]. Regardless of the EO formulation applied, substantial sustained chamber concentrations of EO ranging from 400 to 1200 mg/L—depending on duration, temperature, humidity, and product type—have always been required to achieve acceptable levels of sterilization. Sterilization efficacy was historically verified by recovering enclosed biological test samples placed into packaged materials on pallets before sterilization and removed after completion of the sterilization for quantifying microbial mortality [20,21,22,28]. It is assumed the period-specific final chamber concentrations of EO listed in Table 3 were derived to be consistent with the kill concentration range for EO just mentioned, by using EO concentrations measured in relation to the number of wash cycles applied (described below), and using a modern industrial sterilization chamber (Supplemental Materials, Figure S1).
2.2.4. Wash Cycles
Since the 1980s, increasing numbers of repeated cycles of in-chamber, post-exposure vacuum and air- or nitrogen-washes, as well as post-treatment heating and aeration, have been applied in the sterilization process to drive down residual levels of EO in treated products and in workplace air. The wash cycle assumptions listed in Table 3 reflect the fact that two or fewer vacuum and air or nitrogen washes were used in earlier sterilization operations (e.g., Goldgraben and Zank [16]), resulting in higher residual EO levels in the chamber air and sterilized materials. For example, in the 1980s it was observed that a 98% reduction in post-sterilization residual EO could be achieved in treated medical products after 25 vacuum/wash cycles, however, at the end of EO exposure before such cycling, most (i.e., ~64%) EO was observed to be adsorbed/absorbed into packaging materials, whereas residual EO was observed predominantly (i.e., >80%) in/on treated materials after the application of multiple evacuation cycles, although specific residual values of retained EO mass were noted to be highly product dependent [23].
2.2.5. Storage of Sterilized Materials
An important difference in the operating conditions of the periods is the storage of sterilized materials in the same room as the sterilization chambers in Early and Middle Period operations and storage in a separate warehouse room during Late Period operations (Table 3).
2.2.6. Rate of EO De-Gassing
Approximate first-order rates of EO release from sterilized EO absorbent medical product materials are consistent with the corresponding approximate 2 h typical half-time of EO release (approximate range: 1–6 h) [21,22,24,25]. Similar rates of first-order EO loss from product sterilization of packaging materials (EO permeable plastic enclosures, cardboard boxes and separators, spice bags, etc.) were likely, whereas EO entries into sterilization room air from chamber leaks, chamber maintenance, and floor-trap areas were likely to have been either episodic and/or roughly continuous. However, EO release kinetics do not affect the E/IH-model prediction of long-term TWA EO concentration given by Equation (1).
2.2.7. Fraction (Fch) of Mair Attributable to EO in Chamber Void
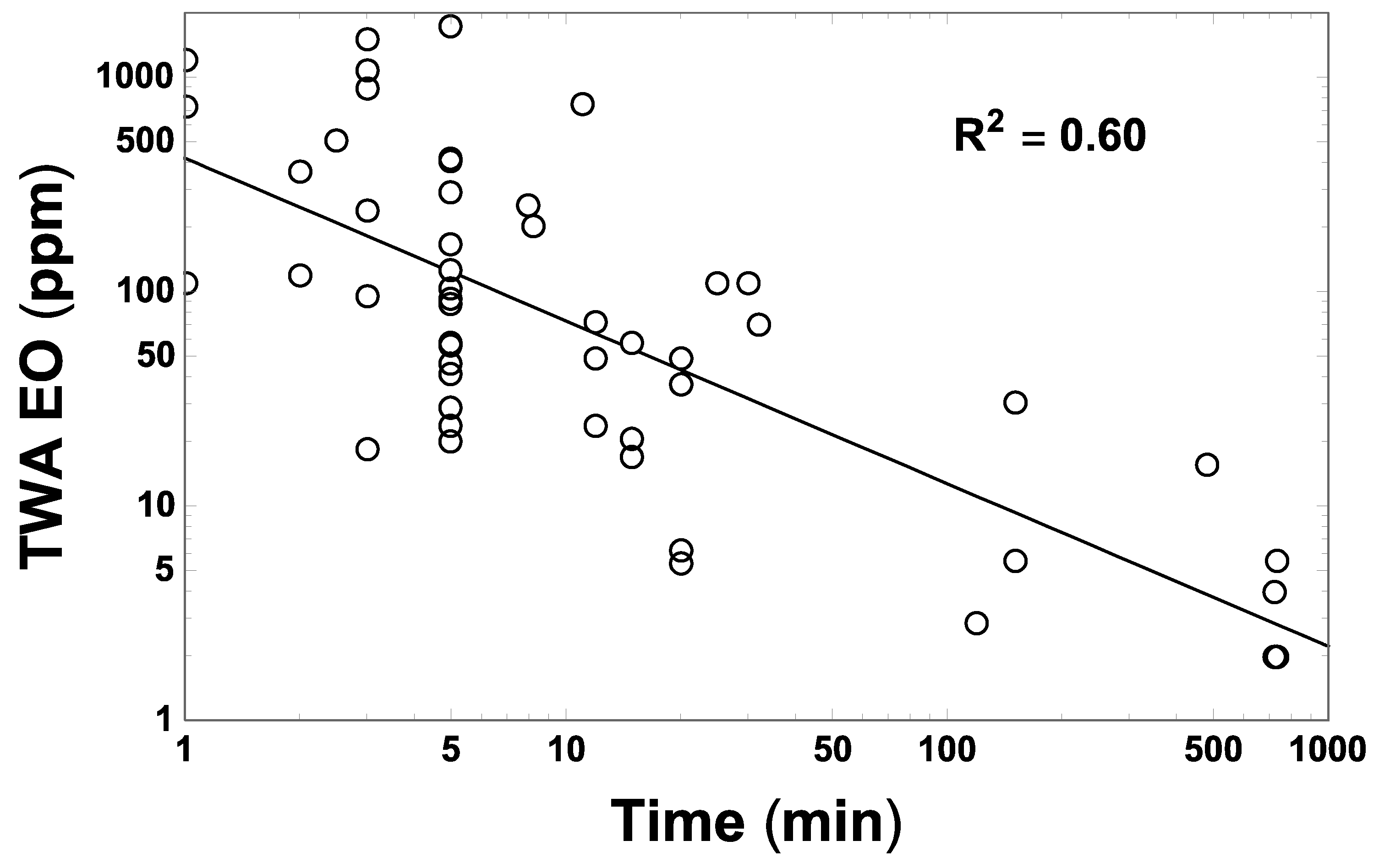
The values of Fch used in Equation (1) (namely, 0.44 and 0.39 for medical/health and spice product scenarios, respectively) were selected to predict a contribution to the overall 8 h TWA EO concentration attributable specifically to Mair. This is consistent with that (~3.9 ppm) predicted by the log–log linear regression fit obtained to 55 TWA EO concentration measures discussed by Goldgraben and Zank [16], which were made in spice sterilization facilities over various averaging periods (Figure 4).
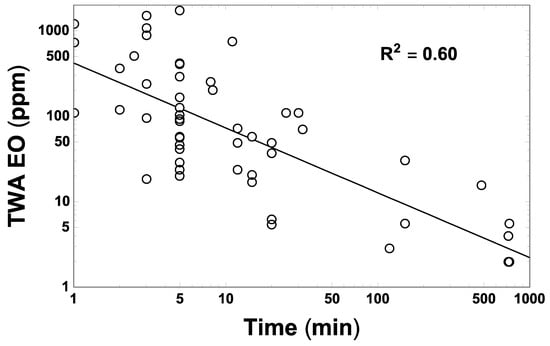
Figure 4.
Fifty-five measures (open points) of TWA EO concentration made around sterilization chambers in the spice sterilization facilities listed and cited by Goldgraben and Zank [16], in relation to corresponding reported durations (t, in min) over which these measurements were made. The straight line shows the corresponding unweighted log–log linear regression fit to these data, EOTWA = 419.65(t/min)−0.7592 ppm (p = ~0, R2 = 0.60), which predicts an 8 h TWA EO concentration of approximately 3.9 ppm.
2.2.8. EO Concentration in Worker Breathing Zone Due to EO Density
EO has a relative gas density of 1.5 compared to air. The experienced EO operators who were interviewed reported clear recollections of relatively greater EO concentrations at lower vertical positions, including recollections that had been confirmed by the EO concentration measurements taken, e.g., in low versus high positions in a storage warehouse. Using X and Y to denote EO mass in the lower and upper halves of each relevant compartment volume, and assuming sterilization operators were exposed to EO concentrations representative of those in the lower half of each compartment, it was conservatively assumed that the rate of vertical-diffusion gain of EO mass to X is 1.5-fold that of loss from Y. At dynamic equilibrium, the average EO concentration CTWA = (X + Y)/2 was thus assumed to equal (X + X/1.5)/2 or (5/6)X, implying that X = (6/5)CTWA. Thus, the factor H in Equation (1) was assumed to be 6/5.
2.3. E/IH Model Calibration
Predictions made by the E/IH model for the Late Period medical/health products scenario were calibrated as follows to facilitate the comparison of predictions made using the E/IH and NSR models. Specifically, the 7% EO retention listed in Table 3, assumed to be applied after two vacuum/wash cycles, was selected to predict a value of C90 for the Late Period medical/health scenario that matches (to within ±0.5 ppm) the 47.4 ppm estimated by the NSR model [5,29,30]. This calibration enabled a direct, normalized comparison between predictions made by the E/IH and NSR models for the Early and Middle periods. E/IH estimates so generated were used to examine the plausibility of the pre-1976–1978 NSR predictions that could not be validated empirically by NIOSH because no personal air measurements were available. For the Early and Middle periods, EO retention was additionally assumed to vary in inverse proportion to the number of cycles assumed to be applied during those periods (Table 3).
2.4. Model Prediction Uncertainty
The interview- and literature-derived data used to construct period-specific E/IH-model assumptions for the input variables described above and their associated correlations were limited in scope and quantitative detail. For this reason, a Monte Carlo approach to quantifying the uncertainty associated with the C90 estimates generated by the E/IH model based on quantitative characterizations of uncertainty and variability associated with each model input was not feasible. Instead, C90 uncertainty for the year 1978 was estimated directly from the empirical distribution (FC) of 1806 facility and job category-specific estimates of occupational EO exposure estimated by the NSR model to have occurred during that year [29,30], which was the first year for which NSR model estimates could be validated, based on a large set of contemporary measurements of EO concentrations in personal air (Supplemental Materials, Figure S2). Ninety-five percent confidence bounds on the NSR-model value of C90 for the year 1978 were estimated robustly as corresponding maximally symmetrical 95% lower and upper confidence bounds (C90Lo and C90Hi, respectively) on C90, estimated from 10,000 bootstrap sets of 100 random samples generated from FC as a parent distribution. The uncertainty in the value of C90 generated by the E/IH model for medical/health products sterilized during the Late Period (including the year 1978) was thus assumed to characterize the relative magnitude of C90 uncertainty for this scenario via corresponding lower- and upper-bound ratios RLo = C90Lo/C90 and RHi = C90Hi/C90, respectively. The same ratios were also used to estimate the relative magnitude of C90 uncertainty estimated by the E/IH model for each period and the sterilization product type considered. The decision to project C90 uncertainty specific to 1978 onto earlier periods, instead of using a similar approach applying NSR-based FC distributions calculated using NIOSH summary data obtained for earlier years or sets of years, was made for three reasons. First, NSR-based estimates of occupational EO exposure before 1978 are potentially seriously biased. Very limited (1976–1977) or no (pre-1976) measured EO concentration data were available to validate pre-1978 historical estimates of worker exposures to EO generated by the NSR model. This lack of a substantive, contemporaneous empirical basis for the NSR model is also indicated by its failure to consider the historical evolution of specific engineering and industrial hygiene aspects of sterilization operations. Second, NSR-based estimates of upper-bound occupational EO exposure before 1978 are subject to increasingly serious sample-size bias for increasingly earlier years before 1978. The number of unique concentration estimates generated by the NSR model to separate facilities and job categories included in its set of NIOSH-cohort occupational exposure information was substantially less in earlier year (Supplementary Materials, Figure S3). Third, there is substantial uncertainty associated with extrapolating EO exposures for years and work conditions before data collection and sterilization industry regulation, using only a model fit to data and work conditions following industry regulations.
All calculations were performed using Mathematica® 11.3 software (Wolfram Research, Inc., Champaign, IL, USA) [31].
3. Results
The C90 estimates obtained using the E/IH modeling approach are summarized and compared in Table 4. The E/IH model results for medical/health product sterilization show an overall decreasing historical trend in estimated C90 during the period 1938–1978, with exposures in the Early Period higher than in 1978. The approximate values of C90 estimated by the E/IH model decrease from 190 to 120 to 48 ppm going forward in time from the Early to Middle to Late medical/health exposure periods considered. The former two E/IH-based estimates of C90 are ~3.9- and ~2.5-fold greater than that estimated for 1978 by both the E/IH and NSR models. In contrast, the NSR model predicts approximate C90 values of 12 and 30 ppm at the Early and Middle Period midpoints, respectively, implying that the C90 values predicted for the Early and Middle periods by the E/IH model for medical/health product sterilization are approximately 16- and 4-fold greater than those estimated by the NSR model, respectively (Table 4). The decreasing historical trend in occupational EO exposure levels predicted by the E/IH model during 1938–1978 contrasts sharply with the increasing trend predicted by the NSR model over this period. These contrasting trends are compared together with prevailing ACGIH TLV levels in Figure 5. The E/IH model generated very similar estimates of C90 for spice sterilization (not calibrated) and for medical/health product sterilization during the Late Period.

Table 4.
Comparison of E/IH and NSR model results.
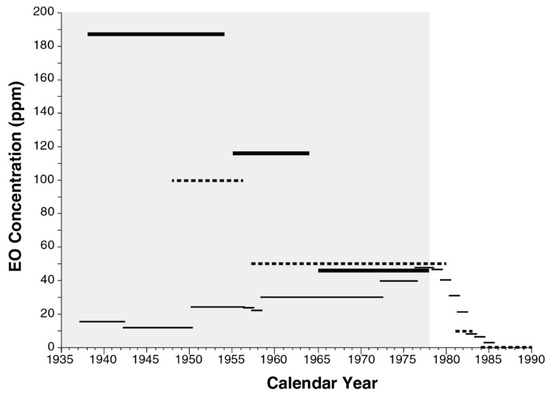
Figure 5.
Comparison of E/IH (thick lines) and NSR (thin lines) exposure model estimates of occupational respiratory exposures to EO in facilities that sterilized medical/health products and prevailing ACGIH TLV limits for EO (dashed lines). Shaded area represents the period during which very limited or (pre-1976) no contemporaneous measurements were available to validate NSR model predictions and during which no EO-specific regulations were in place to limit occupational EO exposures.
Using the bootstrap approach described in the Materials and Methods section, ratios RLo = 0.663 and RHi = 1.20 were calculated to estimate the relative magnitude of uncertainty in C90 (Table 4).
4. Discussion
The E/IH model estimated greater EO exposure concentrations in the Early and Middle periods examined relative to the concentrations it estimated for the Late Period. This decreasing historical trend over the period 1938–1978 is associated with a corresponding evolution in sterilization facility and operational characteristics, as reflected in the E/IH model parameter values and operational assumptions listed in Table 3. EO releases from the storage of sterilized products is predicted by the E/IH model to have been the primary contribution to total EO concentrations in workplace air over the periods examined. The two primary variables contributing to high EO residues in stored products during the Early and Middle periods are estimated to have been (1) the application of no or one vacuum and air/nitrogen wash and (2) the fact that sterilized product storage and sterilization operations typically occurred in the same building during those periods.
The NSR and E/IH models clearly predict opposite historical C90 trends, with the E/IH model predicting C90 values more than an order of magnitude greater than the NSR model during the Early Period considered for the sterilization of medical/health products. The E/IH model was calibrated to predict the same level of EO exposure (~48 ppm) during 1978, the end of the modeled Late exposure period. However, at midpoints of the Early and Middle exposure periods examined, the E/IH model estimated EO concentrations to be approximately 16- and 4-fold greater, respectively, than those predicted by the NSR model that was applied by NIOSH and EPA to estimate EO cancer risks based on analyses of NIOSH cohort epidemiological data. The substantial difference in the estimated historical trend of workplace EO concentrations during 1938–1978 between these two models clearly reflects the NIOSH model assumption that there were no substantive changes in sterilization operations before 1978, as well as an apparently spurious correlation imposed by that model between increased sterilizer volumes and its predicted EO concentrations during 1938–1978.
Results using the E/IH modeling approach reported here highlight the importance of considering combined sterilization and sterilization product storage in Early and Middle Period operations versus separate storage of sterilized materials in Late Period operations, which was not considered explicitly in the NSR model. These results clearly challenge the validity of NSR-based estimates of historical EO exposures, and thus challenge previous claims that the NSR model had been validated for this historical period [1,2,3,4]. Consequently, the results reported here imply that previous calculations of the elevated cancer risk experienced by members of the NIOSH sterilizer worker cohort [1,2,3,4] have greater uncertainty than had been described in those studies, insofar as those calculations presumed the validity of NSR model estimates of pre-1978 historical EO exposures experienced by members of that cohort.
5. Conclusions
In view of the uncertainty that the E/IH modeling analysis raises about NSR model predictions for early sterilization worker EO exposures, EPA’s exclusive reliance on the NIOSH cohort to estimate EO cancer potency and risk should be re-examined.
Supplementary Materials
The following are available online at https://www.mdpi.com/1660-4601/16/10/1738/s1: Figures S1–S4, Table S1, and supporting references.
Author Contributions
All authors contributed to conceptualization of the modeling analysis and gathering of information and data. Modeling was performed by K.T.B. and verification provided by P.J.S. and C.V.-F. All authors contributed to writing, review and editing of the manuscript. A.A.L. was responsible for acquisition of funding.
Funding
Funding and technical information for this research were provided by the Ethylene Oxide Sterilization Organization, an international consortium of industrial facilities that perform ethylene oxide sterilization. Funding also was received from the American Chemistry Council’s Ethylene Oxide panel.
Acknowledgments
Exposure estimates based on the NIOSH linear regression model were obtained from the National Institute for Occupational Safety and Health through a Freedom of Information Act request (13 May 2004). Soon after these NIOSH data were received, annual exposure estimates for each job code were extracted into a separate spreadsheet to generate corresponding summary estimates of EO exposure generated by that model.
Conflicts of Interest
The authors declare no conflict of interest. Three authors (KB, AL, PS) did this work as employees of Exponent, Inc., an engineering and health sciences consulting firm serving clients in government and industry. Decisions concerning organization, technical approach, content, preparation, editing, and submission of this manuscript were made solely by the authors and supporting technical and editorial staff at Exponent. The sponsors did not review the manuscript at any stage of development leading up to submission to the journal. The opinions of the authors do not necessarily reflect the opinions of the sponsors.
References
- USEPA. Evaluation of the Inhalation Carcinogenicity of Ethylene Oxide (CASRN 75-21-8) in Support of Summary Information on the Integrated Risk Information System; EPA/635/R-16/350Fa; U.S. Environmental Protection Agency, Office of Research and Development: Washington, DC, USA, 2016.
- Steenland, K.; Stayner, L.; Greife, A.; Halperin, W.; Hayes, R.; Hornung, R.; Nowlin, S. Mortality among workers exposed to ethylene oxide. N. Engl. J. Med. 1991, 324, 1402–1407. [Google Scholar] [CrossRef] [PubMed]
- Steenland, K.; Whelan, E.; Deddens, J.; Stayner, L.; Ward, E. Ethylene oxide and breast cancer incidence in a cohort study of 7576 women (United States). Cancer Causes Control 2003, 14, 531–539. [Google Scholar] [CrossRef] [PubMed]
- Stayner, L.; Steenland, K.; Greife, A.; Hornung, R.; Hayes, R.B.; Nowlin, S.; Morawetz, J.; Ringenburg, V.; Elliot, L.; Halperin, W. Exposure-response analysis of cancer mortality in a cohort of workers exposed to ethylene oxide. Am. J. Epidemiol. 1993, 138, 787–798. [Google Scholar] [CrossRef] [PubMed]
- Steenland, K.; Stayner, L.; Deddens, J. Mortality analyses in a cohort of 18,235 ethylene oxide exposed workers: Follow up extended from 1987 to 1998. Occup. Environ. Med. 2004, 61, 2–7. [Google Scholar] [PubMed]
- Greife, A.L.; Hornung, R.W.; Stayner, L.G.; Steenland, K.N. Development of a model for use in estimating exposure to ethylene oxide in a retrospective cohort mortality study. Scand. J. Work Environ. Health 1988, 14 (Suppl. 1), 29–30. [Google Scholar]
- Hornung, R.W.; Greife, A.L.; Stayner, L.T.; Steenland, N.K.; Herrick, R.F.; Elliott, L.J.; Ringenburg, V.L.; Morawetz, J. Statistical model for prediction of retrospective exposure to ethylene oxide in an occupational mortality study. Am. J. Ind. Med. 1994, 25, 825–836. [Google Scholar] [CrossRef] [PubMed]
- USEPA. Science Advisory Board Review of the EPA’s Evaluation of the Inhalation Carcinogenicity of Ethylene Oxide (Revised External Review Draft—August 2014); EPA-SAB-15-012 (2015 SAB Review); U.S. Environmental Protection Agency: Washington, DC, USA, 2015; p. 18.
- Von Grote, J.H.M. Occupational Exposure Assessment in Metal Degreasing and Dry Cleaning—Influences of Technology Innovation and Legislation. Ph.D. Dissertation, Swiss Federal Institute of Technology, Zürich, Switzerland, 2003. Available online: http://citeseerx.ist.psu.edu/viewdoc/download?doi=10.1.1.628.1123&rep=rep1&type=pdf (accessed on 3 January 2019).
- Von Grote, J.; Hürlimann, C.; Scheringer, M.; Hungerbühler, K. Reduction of occupational exposure to perchloroethylene and trichloroethylene in metal degreasing over the last 30 years: Influences of technology innovation and legislation. J Expo Anal. Environ. Epidemiol. 2003, 13, 325–340. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Von Grote, J.; Hürlimann, C.; Scheringer, M.; Hunger, K. Assessing occupational exposure to perchloroethylene in dry cleaning. J. Occup. Environ. Hyg. 2006, 3, 606–619. [Google Scholar] [CrossRef] [PubMed]
- ACGIH. Documentation of the TLVs and BEIs: Ethylene Oxide; American Conference of Governmental Industrial Hygienists: Cincinnati, OH, USA, 2015.
- FDA. Ethylene Oxide, Ethlyene Chlorohydrin, and Ethylene Glycol: Proposed Maximum Residue Limits and Maximum Levels of Exposure; 43 FR 27474; Food and Drug Administration: Washington, DC, USA, 1978.
- OSHA. Ethylene Oxide (EtO) Standard; 29 CFR 1910.1047; The Occupational Safety and Health Administration: Washington, DC, USA, 1984.
- SCOEL. Recommendation from the Scientific Committee on Occupational Exposure Limits for Ethylene Oxide; SCOEL/SUM/160; European Commission, Employment, Social Affairs & Inclusion: Brussels, Belgium, June 2012. [Google Scholar]
- Goldgraben, R.; Zank, N. Mitigation of Worker Exposure to Ethylene Oxide; Report Prepared for the U.S. Environmental Protection Agency; MTR-80 W333; Appendix C-10: Practices Relevant to Worker Exposure at Spice Industry Sites; The Mitre Corp.: McLean, VA, USA, March 1981; pp. C153–C175. [Google Scholar]
- Vollrath. General Specification, Corrugated Containers & Components for Purchased Products; Vollrath: Sheboygan, WI, USA, 2010; Available online: https://vollrath.com/Vollrath-Files/Suppliers/MIS_GeneralSpecificationCorrugatedContainersComponents_en_2010-04-30.pdf (accessed on 3 January 2019).
- Andersen, L.; Delvers, M.; Hu, E. An Introduction to Gas Diffusion Sterilization. MD&DI Magazine, 1 May 1997; 1–8. [Google Scholar]
- Perkins, J.J. Principles and Methods of Sterilization in Health Sciences, 1st ed.; Charles C. Thomas Publisher: Springfield, IL, USA, 1956; pp. 325–334. [Google Scholar]
- Perkins, J.J. Principles and Methods of Sterilization in Health Sciences, 2nd ed.; Charles C. Thomas Publisher: Springfield, IL, USA, 1969; pp. 501–530. [Google Scholar]
- Bruch, C.W. Gaseous sterilization. Annu. Rev. Microbiol. 1961, 15, 245–262. [Google Scholar] [CrossRef]
- Bruch, C.W. Sterilization of plastics: Toxicity of ethylene oxide residues. In Industrial Sterilization, Proceedings of the International Symposium, Amsterdam, The Netherlands, 2–4 May 1972; Phillips, G.B., Miller, W.S., Eds.; Duke University Press: Durham, NC, USA, 1972; pp. 49–78. [Google Scholar]
- Buonicore, A.J.; Desai, P.R.; Mangone, M.A. Post Evacuation Cycle Modifications to Reduce Ethylene Oxide Residual Levels and Worker Exposure. Presented at the Medical Device and Diagnostic Industries (MD & DI) East, New York, NY, USA, 14–17 May 1984; Chemrox Inc.: Bridgeport, CT, USA, 1984. [Google Scholar]
- Stetson, J.B.; Whitbourne, J.E.; Eastman, C. Ethylene oxide degassing of rubber and plastic materials. Anesthesiol 1976, 44, 174–180. [Google Scholar] [CrossRef]
- White, J.D. Standard aeration for gas-sterilized plastics. J. Hyg. 1977, 79, 225–232. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Friedrich, T.; Schellhaas, H. Computation of the percentage points and the power for the two-sided Kolmogorov-Smirnov one sample test. Stat. Pap. 1998, 39, 361–375. [Google Scholar] [CrossRef]
- Burgess, D.F.; Reich, R.R. Industrial ethylene oxide sterilization in sterilization technology. In Sterilization Technology: A Practical Guide to Manufacturers and Users of Health Care Products, 1st ed.; Morrissey, R.F., Phillips, G.B., Eds.; Van Nostrand Reinhold: New York, NY, USA, 1993; pp. 153–194. [Google Scholar]
- USEPA. Ethylene Oxide Emissions from Commercial Sterilization/Fumigation Operations—Background Information for Proposed Standards; Final EPA-453/D-93-016; U.S. Environmental Protection Agency, Office of Air Quality Planning and Standards: Research Triangle Park, NC, USA, March 1993. Available online: http://nepis.epa.gov/Exe/ZyPDF.cgi?Dockey=00002URQ.PDF (accessed on 3 January 2019).
- Lehman, E.; (Industry Studies Branch, NIOSH, Cincinnati, OH, USA). Personal communication, 5 January 2005.
- NIOSH. Data File of NIOSH Regression-Model-Based Summary (De-Identified) Estimates of Annual, Facility- and Job-Code-Specific EO Exposure for the NIOSH Sterilization Worker Cohort; National Institute of Occupational Safety and Health: Cincinnati, OH, USA, 2004.
- Wolfram Research. Wolfram Language and System Documentation Center; Wolfram Research, Inc.: Champaign, IL, USA, 2019; Available online: http://reference.wolfram.com/language/ (accessed on 15 November 2018).
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).