OPENCRONIC Study. Knowledge and Experiences of Spanish Patients and Carers about Chronic Disease
Abstract
1. Introduction
2. Methods
2.1. Study Design
2.2. Sample Selection
2.3. Procedure
2.4. Questionnaire
2.5. Data Analysis
2.6. Data Confidentiality
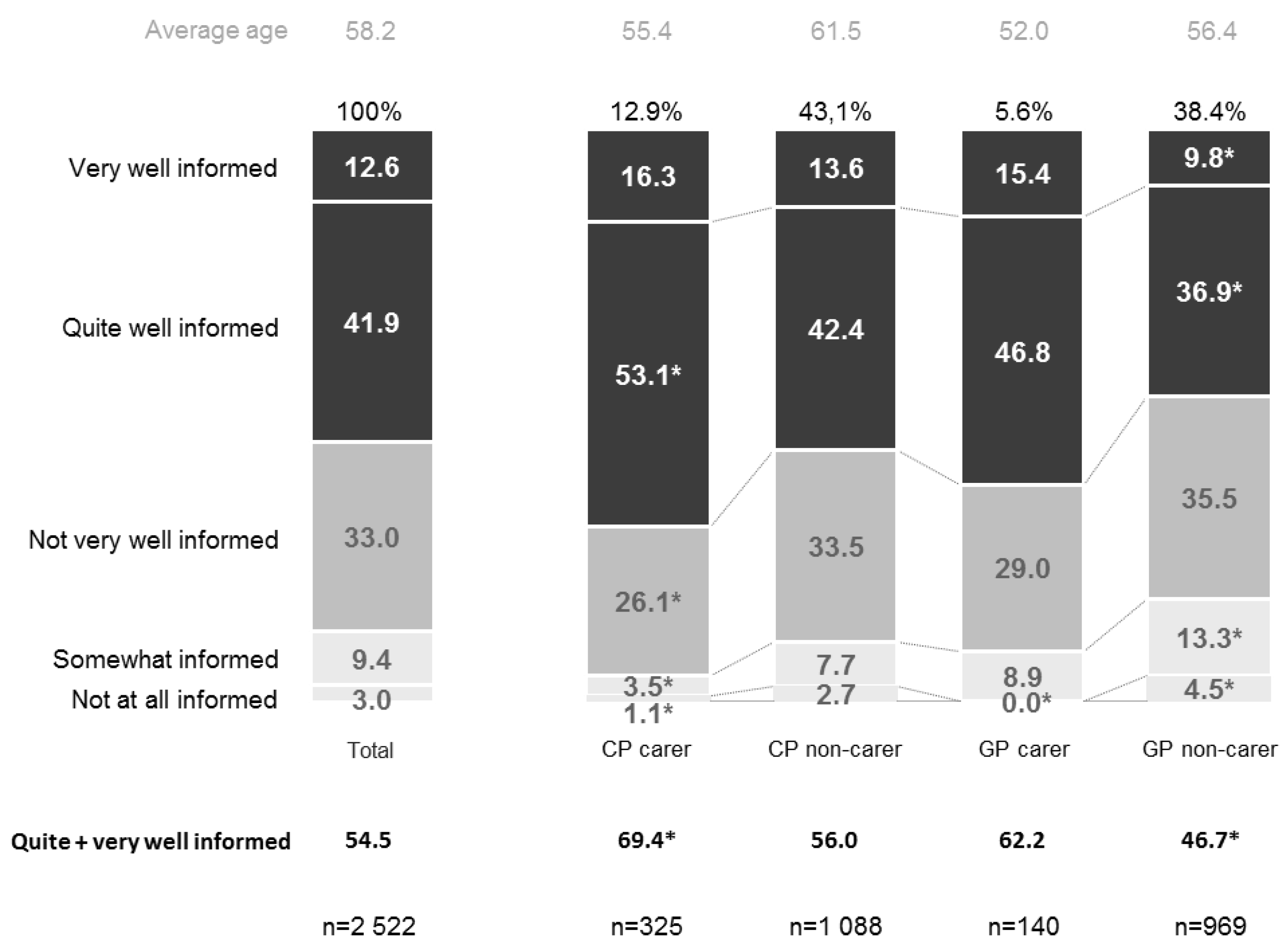
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- World Health Organisation. Enfermedades Crónicas. Available online: http://www.who.int/topics/chronic_diseases/es/ (accessed on 16 October 2018).
- Bernell, S.; Howard, S.W. Use your words carefully: What is a chronic disease? Front. Public Health 2016, 4, 159. [Google Scholar] [CrossRef] [PubMed]
- World Health Organisation. Enfermedades no Transmisibles: Perfiles de Países 2014. Available online: http://www.who.int/nmh/countries/esp_es.pdf?ua=1 (accessed on 16 October 2018).
- Tóthová, V.; Bártlová, S.; Dolák, F.; Kaas, J.; Kimmer, D.; Manhalová, J.; Martinek, L.; Olisarová, V. Quality of life in patients with chronic diseases. Neuro Endocrinol. Lett. 2014, 35, 11–18. [Google Scholar] [PubMed]
- Dueñas, M.; Ojeda, B.; Salazar, A.; Mico, J.A.; Failde, I. A review of chronic pain impact on patients, their social environment and the health care system. J. Pain Res. 2016, 9, 457–467. [Google Scholar] [CrossRef] [PubMed]
- World Health Organisation. Enfermedades no Transmisibles: Datos y Cifras (Junio 2017). Available online: http://www.who.int/es/news-room/fact-sheets/detail/noncommunicable-diseases (accessed on 16 October 2018).
- Ministerio de Sanidad Consumo y Bienestar Social [Spanish Ministry of Health Consumption and Social Welfare]. Encuesta Nacional de Salud de España 2011–2012. Nota técnica. Available online: https://www.msssi.gob.es/estadEstudios/estadisticas/encuestaNacional/encuestaNac2011/NotaTecnica2011-12.pdf (accessed on 16 October 2018).
- Organisation for Economic Co-operation and Development. Sickness, Disability and Work: Breaking the Barriers; OECD Publishing: Paris, France, 2007. [Google Scholar]
- Arredondo, A.; Avilés, R. Costs and epidemiological changes of chronic diseases: Implications and challenges for health systems. PLoS ONE 2015, 10, e0118611. [Google Scholar] [CrossRef] [PubMed]
- Wagner, E.H.; Austin, B.T.; Davis, C.; Hindmarsh, M.; Schaefer, J.; Bonomi, A. Improving chronic illness care: Translating evidence into action. Health Aff. (Millwood) 2001, 20, 64–78. [Google Scholar] [CrossRef] [PubMed]
- Wagner, E.H. Chronic disease management: What will it take to improve care for chronic illness? Eff. Clin. Pract. 1998, 1, 2–4. [Google Scholar] [PubMed]
- Martin, C.M. Chronic disease and illness care: Adding principles of family medicine to address ongoing health system redesign. Can. Fam. Phys. 2007, 53, 2086–2091. [Google Scholar]
- Instituto Nacional de Estadística [Spanish National Institute of Statistics]. Encuesta Sobre Equipamiento y uso de Tecnologías de Información y Comunicación en Los Hogares. Available online: http://www.ine.es/dyngs/INEbase/es/operacion.htm?c=Estadistica_C&cid=1254736176741&menu=ultiDatos&idp=1254735576692 (accessed on 16 October 2018).
- Ministerio de Sanidad Consumo y Bienestar Social [Spanish Ministry of Health Consumption and Social Welfare]. Encuesta Nacional de Salud de España 2011–2012. Estado de Salud. Available online: https://www.msssi.gob.es/estadEstudios/estadisticas/encuestaNacional/encuestaNac2011/EstadoSalud_DistribucionPorcentual.pdf (accessed on 16 October 2018).
- Soriano, J.B.; Calle, M.; Montemayor, T.; Álvarez-Sala, J.L.; Ruiz-Manzano, J.; Miravitlles, M. The general public’s knowledge of chronic obstructive pulmonary disease and its determinants: Current situation and recent changes. Arch. Bronconeumol. 2012, 48, 308–315. [Google Scholar] [CrossRef] [PubMed]
- Rapado Errazti, A.; Sosa Henríquez, M.; García Borrás, J.J.; Calvo Catalá, A.; Díaz Curiel, M.; Garcés Puentes, V. Encuesta sobre el grado de conocimiento de la osteoporosis en mujeres españolas. Rev. Esp. Enferm. Metab. Oseas 2001, 10, 46–49. [Google Scholar]
- Hocking, A.; Laurence, C.; Lorimer, M. Patients’ knowledge of their chronic disease—The influence of socio-demographic characteristics. Aust. Fam. Phys. 2013, 42, 411–416. [Google Scholar]
- Corbin, J.M.; Strauss, A. Unending Work and Care: Managing Chronic Illness at Home; JOssey-Bass: San Francisco, CA, USA, 1988; p. 358. [Google Scholar]
- Berkman, N.D.; Sheridan, S.L.; Donahue, K.E.; Halpern, D.J.; Crotty, K. Low health literacy and health outcomes: An updated systematic review. Ann. Intern. Med. 2011, 155, 97–107. [Google Scholar] [CrossRef] [PubMed]
- Pereira, D.A.; Costa, N.M.; Sousa, A.L.; Jardim, P.C.; Zanini, C.R. The effect of educational intervention on the disease knowledge of diabetes mellitus patients. Rev. Lat. Am. Enferm. 2012, 20, 478–485. [Google Scholar] [CrossRef]
- Corry, M.; While, A.; Neenan, K.; Smith, V. A systematic review of systematic reviews on interventions for caregivers of people with chronic conditions. J. Adv. Nurs. 2015, 71, 718–734. [Google Scholar] [CrossRef] [PubMed]
- Vinaccia, S.; Orozco, L.M. Aspectos psicosociales asociados con la calidad de vida de personas con enfermedades crónicas. Divers. Perspect. Psicol. 2005, 1, 125–137. [Google Scholar] [CrossRef]
- Kimmel, P.L. Psychosocial factors in dialysis patients. Kidney Int. 2001, 59, 1599–1613. [Google Scholar] [CrossRef] [PubMed]
- Avellaneda, A.; Izquierdo, M.; Torrent-Farnell, J.; Ramón, J.R. Rare Diseases: Chronic diseases that need a new approach. An. Sist. Sanit. Navar. 2007, 30, 177–190. [Google Scholar] [CrossRef] [PubMed]
| Characteristics | N | % |
|---|---|---|
| Age | ||
| 40–44 years | 347 | 13.8 |
| 45–49 years | 329 | 13.0 |
| 50–54 years | 321 | 12.7 |
| 55–59 years | 342 | 13.6 |
| 60–64 years | 335 | 13.3 |
| 65–69 years | 331 | 13.1 |
| 70 years or over | 517 | 20.5 |
| Educational Level | ||
| Elementary/no studies | 414 | 16.4 |
| Primary/secondary education | 1154 | 45.8 |
| Higher education | 954 | 37.8 |
| General Population | 1109 | 44.0 |
| Carers of chronic patients | 140 | 12.6 # |
| Non-carers of chronic patients | 969 | 87.4 # |
| Chronic Patients | 1413 | 55.0 |
| Carers of other chronic patients | 325 | 23.0 # |
| Non-carers of other chronic patients | 1088 | 76.0 # |
| With 1 disease | 772 | 54.6 # |
| With 2 diseases | 370 | 26.2 # |
| With 3 or more diseases | 271 | 19.2 # |
| With pain | 550 | 38.9 # |
| No pain | 863 | 61.1 # |
| With hospitalisation ‡ | 357 | 25.3 # |
| No hospitalisation | 1056 | 74.7 # |
| With pharmacological treatment | 1225 | 86.7 # |
| No pharmacological treatment | 188 | 13.3 # |
| Diseases Referred to by the Respondents * | ||
| High blood pressure | 542 | 21.5 |
| Arthritis/arthrosis | 477 | 18.9 |
| Mood disorders (depression/anxiety) | 262 | 10.4 |
| Type 1/2 diabetes | 248 | 9.8 |
| Respiratory diseases (COPD/asthma) | 151 | 6.0 |
| Non-valvular atrial fibrillation/heart failure | 89 | 3.5 |
| Other | 212 | 8.4 |
| Body Mass Index ** | ||
| General population | 1109 | 100.0 |
| ≤24.9 kg/m2 | 542 | 48.9 |
| 25–29.9 kg/m2 | 434 | 39.1 |
| ≥30 kg/m2 | 133 | 12.0 |
| Chronic patients | 1413 | 100.0 |
| ≤24.9 kg/m2 | 506 | 35.8 |
| 25–29.9 kg/m2 | 619 | 43.8 |
| ≥30 kg/m2 | 288 | 20.4 |
| Total population | 2522 | 100.0 |
| ≤24.9 kg/m2 | 1048 | 41.6 |
| 25–29.9 kg/m2 | 1053 | 41.8 |
| ≥30 kg/m2 | 421 | 16.7 |
| Having Chronic Diseases Has a Significant or Quite Significant Effect on the Following Aspects | Chronic Patients | General Population | Total | ||
|---|---|---|---|---|---|
| Carer (n = 325) | Non-Carer (n = 1088) | Carer (n = 140) | Non-Carer (n = 969) | ||
| They affect mood | 55.5% | 45.3% * | 71.5% * | 64.2% * | 55.5% |
| They involve making sacrifices, for example not being able to consume certain foods or drinks (salt, alcohol, etc.) | 58.5% | 46.0% * | 70.0% * | 62.20% * | 55.3% |
| They involve loss of quality of life | 51.0% | 46.8% * | 65.3% * | 58.9% * | 53.1% |
| They force you to radically change your lifestyle | 54.1% | 44.2% * | 66.3% * | 60.2% * | 53.0% |
| They increase the risk of serious events such as heart attack, stroke, etc. | 51.5% | 44.0% * | 58.4% * | 51.7% | 48.8% |
| They increase the risk of early death | 47.6% | 40.4% * | 58.0% * | 53.7% * | 47.5% |
| They lead to situations of dependency at a younger age | 47.8% | 39.6% * | 64.9% * | 53.8% * | 47.5% |
| They cause professional difficulties/restrictions | 44.0% | 28.9% * | 56.4% * | 54.6% * | 46.6% |
| They make you withdrawn and lose the will to do things | 45.4% | 38.5% * | 59.4% * | 58.2% * | 46.3% |
| They have a negative effect on social relationships/friendships | 31.0% | 25.7% * | 42.1% * | 38.2% * | 32.2% |
| They have a negative effect on family relationships | 31.6% | 23.3% * | 40.7% * | 38.5% * | 31.2% |
| Implications of Having a Chronic Disease with Which the Respondents Agree Strongly or Quite Strongly | High Level of Information | Average Level of Information | Low Level of Information | |||
|---|---|---|---|---|---|---|
| Chronic Disease (%) | General Population (%) | Chronic Disease (%) | General Population (%) | Chronic Disease (%) | General Population (%) | |
| They increase the risk of serious events such as heart attack, stroke, etc. | 63.6 # | 52.8 * | 28.5 | 33.1 | 7.9 | 14.1 |
| They lead to situations of dependency at a younger age | 64.6 # | 53.6 * | 25.4 | 31.3 | 10.0 | 15.1 |
| They force you to radically change your lifestyle | 61.7 # | 53.1 * | 29.3 | 32.6 | 9.0 | 14.3 |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Casariego, E.; Cebrián-Cuenca, A.M.; Llisterri, J.L.; Micó-Pérez, R.M.; Orozco-Beltran, D.; Otero-Cacabelos, M.; Román-Sánchez, P.; Sáez, F.J. OPENCRONIC Study. Knowledge and Experiences of Spanish Patients and Carers about Chronic Disease. Int. J. Environ. Res. Public Health 2019, 16, 39. https://doi.org/10.3390/ijerph16010039
Casariego E, Cebrián-Cuenca AM, Llisterri JL, Micó-Pérez RM, Orozco-Beltran D, Otero-Cacabelos M, Román-Sánchez P, Sáez FJ. OPENCRONIC Study. Knowledge and Experiences of Spanish Patients and Carers about Chronic Disease. International Journal of Environmental Research and Public Health. 2019; 16(1):39. https://doi.org/10.3390/ijerph16010039
Chicago/Turabian StyleCasariego, Emilio, Ana M. Cebrián-Cuenca, José Luis Llisterri, Rafael Manuel Micó-Pérez, Domingo Orozco-Beltran, Mercedes Otero-Cacabelos, Pilar Román-Sánchez, and Francisco José Sáez. 2019. "OPENCRONIC Study. Knowledge and Experiences of Spanish Patients and Carers about Chronic Disease" International Journal of Environmental Research and Public Health 16, no. 1: 39. https://doi.org/10.3390/ijerph16010039
APA StyleCasariego, E., Cebrián-Cuenca, A. M., Llisterri, J. L., Micó-Pérez, R. M., Orozco-Beltran, D., Otero-Cacabelos, M., Román-Sánchez, P., & Sáez, F. J. (2019). OPENCRONIC Study. Knowledge and Experiences of Spanish Patients and Carers about Chronic Disease. International Journal of Environmental Research and Public Health, 16(1), 39. https://doi.org/10.3390/ijerph16010039





