Socioeconomic Inequalities of Undiagnosed Diabetes in a Resource-Poor Setting: Insights from the Cross-Sectional Bangladesh Demographic and Health Survey 2011
Abstract
:1. Introduction
2. Materials and Methods
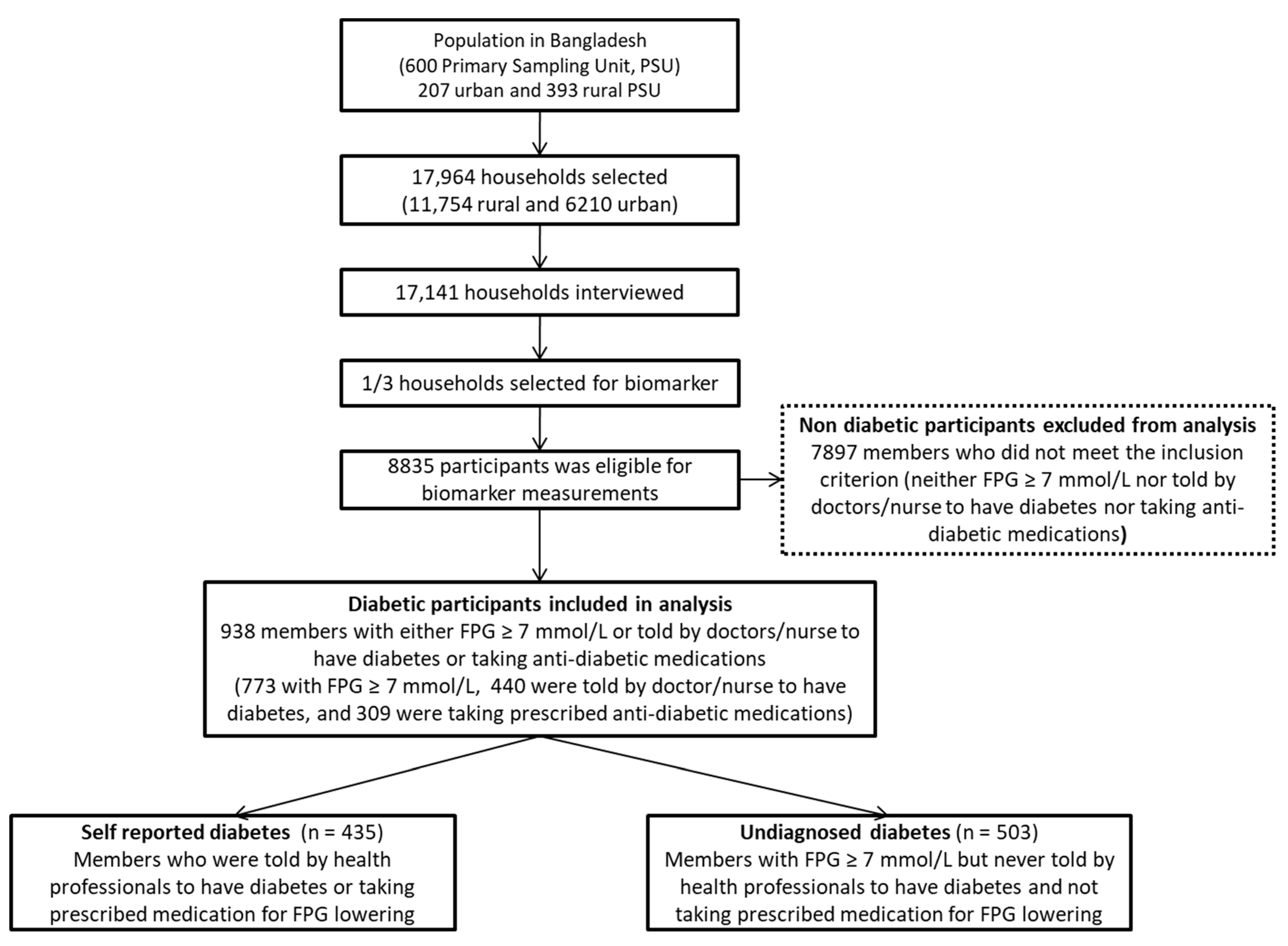
2.1. Participants and Procedures
2.2. Outcome Variable
2.3. Explanatory Variables
2.4. Statistical Analyses
2.5. Ethical Clearance
3. Results
3.1. General Characteristics of the Study Participants
3.2. Prevalence of Undiagnosed Diabetes among Adult Diabetic Patients
3.3. Determinants of Undiagnosed Diabetes
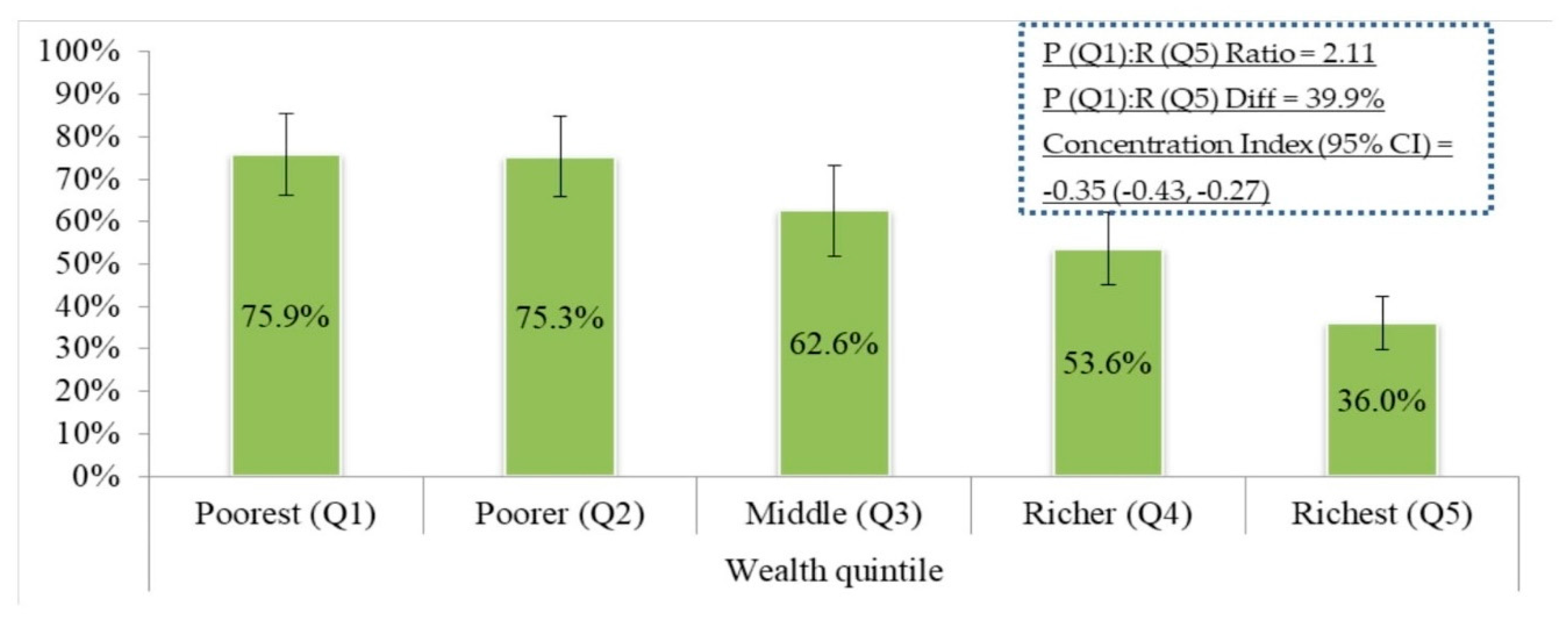
3.4. Socioeconomic Inequalities in Undiagnosed Diabetes
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Terzic, A.; Waldman, S. Chronic diseases: The emerging pandemic. Clin. Transl. Sci. 2011, 4, 225–226. [Google Scholar] [CrossRef] [PubMed]
- Zimmet, P.; Alberti, K.G.; Magliano, D.J.; Bennett, P.H. Diabetes mellitus statistics on prevalence and mortality: Facts and fallacies. Nat. Rev. Endocrinol. 2016, 12, 616–622. [Google Scholar] [CrossRef] [PubMed]
- Shaw, J.E.; Sicree, R.A.; Zimmet, P.Z. Global estimates of the prevalence of diabetes for 2010 and 2030. Diabetes Res. Clin. Pract. 2010, 87, 4–14. [Google Scholar] [CrossRef] [PubMed]
- Ramachandran, A.; Snehalatha, C.; Ma Wan, R.C. Diabetes in South-East Asia: An update. Diabetes Res. Clin. Pract. 2014, 103, 231–237. [Google Scholar] [CrossRef] [PubMed]
- Biswas, T.; Islam, A.; Rawal, L.B.; Islam, S.M.S. Increasing prevalence of diabetes in Bangladesh: A scoping review. Public Health 2016, 138, 4–11. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. World Health Report 2002: Reducing Risks, Promoting Healthy Life; World Health Organization: Geneva, Switzerland, 2003. [Google Scholar]
- World Health Organization. Non-communicable Disease Risk Factor Survey, Bangladesh 2010. Dhaka, Bangladesh; World Health Organization: Dhaka, Bangladesh, 2011. [Google Scholar]
- Brown, A.F.; Ettner, S.L.; Piette, J.; Weinberger, M.; Gregg, E.; Shapiro, M.F.; Karter, A.J.; Safford, M.; Waitzfelder, B.; Prata, P.A.; et al. Socioeconomic position and health among persons with diabetes mellitus: A conceptual framework and review of the literature. Epideniol. Rev. 2004, 26, 63–77. [Google Scholar] [CrossRef]
- World Health Organization. Equity and Social Determinants. Equity, Social Determinants and Public Health Programmes; World Health Organization: Geneva, Switzerland, 2010. [Google Scholar]
- Connolly, V.; Unwin, N.; Sherriff, P.; Bilous, R.; Kelly, W. Diabetes prevalence and socioeconomic status: A population based study showing increased prevalence of type 2 diabetes mellitus in deprived areas. J. Epidemiol. Community Health 2000, 54, 173–177. [Google Scholar] [CrossRef]
- Espelt, A.; Arriola, L.; Borrell, C.; Larranaga, I.; Sandin, M.; Escolar, P.A. Socioeconomic position and type 2 diabetes mellitus in Europe 1999–2009: A panorama of inequalities. Curr. Diabetes Rev. 2011, 7, 148–158. [Google Scholar] [CrossRef]
- Robbins, J.M.; Vaccarino, V.; Zhang, H.; Kasl, S.V. Socioeconomic status and diagnosed diabetes incidence. Diabetes Res. Clin. Pract. 2005, 68, 230–236. [Google Scholar] [CrossRef]
- Gnavi, R.; Karaghiosoff, L.; Costa, G.; Merletti, F.; Bruno, G. Socio-economic differences in the prevalence of diabetes in Italy: The population-based Turin study. Nutr. Metab. Cardiovasc. Dis. 2008, 18, 678–682. [Google Scholar] [CrossRef]
- WHO. Screening for Type 2 Diabetes. Diabetes Care 2004, 27. [Google Scholar] [CrossRef]
- Akter, S.; Rahman, M.M.; Abe, S.K.; Sultana, P. Prevalence of diabetes and prediabetes and their risk factors among Bangladeshi adults: A nationwide survey. Bull. World Health Organ. 2014, 92, 204–213. [Google Scholar] [CrossRef] [PubMed]
- Harshfield, E.; Chowdhury, R.; Harhay, M.N.; Bergquist, H.; Harhay, M.O. Association of hypertension and hyperglycaemia with socioeconomic contexts in resource-poor settings: The Bangladesh Demographic and Health Survey. Int. J. Epidemiol. 2015, 44, 1625–1636. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Definition and Diagnosis of Diabetes Mellitus and Intermediate Hyperglycemia: Report of a WHO/IDF Consultation; World Health Organization: Geneva, Switzerland, 2006. [Google Scholar]
- Moody, A.; Cowley, G.; Ng Fat, L.; Mindell, J.S. Social inequalities in prevalence of diagnosed and undiagnosed diabetes and impaired glucose regulation in participants in the Health Surveys for England series. BMJ Open 2016, 6, e010155. [Google Scholar] [CrossRef] [PubMed]
- Filmer, D.; Pritchett, L.H. Estimating Wealth Effects Without Expenditure Data or Tears. Demography 2001, 38, 115–132. [Google Scholar] [CrossRef] [PubMed]
- Gujarati, D.; Porter, D. Basic Econometrics; McGraw-Hill/Irwin: New York, NY, USA, 2008; ISBN 0073375772. [Google Scholar]
- Koolman, X.; Doorslaer, E. van On the interpretation of a concentration index of inequality. Health Econ. 2004, 13, 649–656. [Google Scholar] [CrossRef] [PubMed]
- National Institute of Population Research and Training (NIPORT), Mitra and Associates, and ICF International. Bangladesh Demographic and Health Survey 2011; NIPORT, Mitra and Associates, and ICF International: Dhaka, Bangladesh; Calverton, MD, USA, 2013. [Google Scholar]
- Clarke, P.M.; Gerdtham, U.G.; Johannesson, M.; Bingefors, K.; Smith, L. On the measurement of relative and absolute income-related health inequality. Soc. Sci. Med. 2002, 55, 1923–1928. [Google Scholar] [CrossRef]
- Wagstaff, A. The bounds of the concentration index when the variable of interest is binary, with an application to immunization inequality. Health Econ. 2005, 14, 429–432. [Google Scholar] [CrossRef]
- O’Donnell, O.; O’Neill, S.; Ourti, T.V.; Walsh, B. conindex: Estimation of concentration indices. Stata J. 2016, 16, 112–138. [Google Scholar] [CrossRef]
- Erreygers, G. Correcting the Concentration Index. J. Health Econ. 2009, 28, 504–515. [Google Scholar] [CrossRef]
- National Institute of Population Research and Training (NIPORT), Associates for Community and Population Research (ACPR), and ICF International. Bangladesh Health Facility Survey 2014; NIPORT, ACPR and ICF International: Dhaka, Bangladesh, 2014. [Google Scholar]
- Lewis and Newell: Patients’ perspectives of care for type 2 diabetes in Bangladesh—A qualitative study. BMC Public Health 2014, 14, 737.
- A collaboration between the Jordan Bennett Weiss Fund and the city of Newton Health Department. Warning Signs of Diabetes, Overview for School Nurses/Personnel/Families. Available online: https://www.joslin.org/Warning_Signs_of_Diabetes_Handout_JBW_Fund.pdf (accessed on 29 September 2018).
- Latif, Z.A.; Jain, A.; Rahman, M.M. Evaluation of Management, Control, Complications and Psychosocial Aspects of Diabetics in Bangladesh: DiabCare Bangladesh. Bangladesh Med. Res. Counc. Bull. 2011, 37, 11–16. [Google Scholar] [CrossRef] [PubMed]
- Islam, F.M.A.; Chakrabarti, R.; Islam, M.T.; Wahab, M.; Lamoureux, E.; Finger, R.P.; Shaw, J.E. Prediabetes, diagnosed and undiagnosed diabetes, their risk factors and association with knowledge of diabetes in rural Bangladesh: The Bangladesh Population-based Diabetes and Eye Study. J. Diabetes 2016, 8, 260–268. [Google Scholar] [CrossRef] [PubMed]
- Leong, A.; Dasgupta, K.; Chiasson, J.L.; Rahme, E. Estimating the population prevalence of diagnosed and undiagnosed diabetes. Diabetes Care 2013, 36, 3002–3008. [Google Scholar] [CrossRef] [PubMed]
- Demmer, R.T.; Zuk, A.M.; Rosenbaum, M.; Desvarieux, M. Prevalence of diagnosed and undiagnosed type 2 diabetes mellitus among us adolescents: Results from the continuous NHANES, 1999–2010. Am. J. Epidemiol. 2013, 178, 1106–1113. [Google Scholar] [CrossRef] [PubMed]
- Stoddard, P.; He, G.; Vijayaraghavan, M.; Schillinger, D. Disparities in undiagnosed diabetes among United States-Mexico border populations. Rev. Panam. Salud Publica 2010, 28, 198–206. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention. National Diabetes Fact Sheet: national Estimates and General Information on Diabetes and Prediabetes in the United States, 2011; Department of Health and Human Services, Centers for Disease Control and Prevention: Atlanta, GA, USA, 2011.
- Bergrem, H.A.; Valderhaug, T.G.; Hartmann, A.; Hjelmesaeth, J.; Leivestad, T.; Bergrem, H.; Jenssen, T. Undiagnosed diabetes in kidney transplant candidates: A case-finding strategy. Clin. J. Am. Soc. Nephrol. 2010, 5, 616–622. [Google Scholar] [CrossRef]
- Alam, D.S.; Talukder, S.H.; Chowdhury, M.A.H.; Siddiquee, A.T.; Ahmed, S.; Pervin, S.; Khan, S.; Hasan, K.; Koehlmoos, T.L.P.; Niessen, L.W. Overweight and abdominal obesity as determinants of undiagnosed diabetes and pre-diabetes in Bangladesh. BMC Obes. 2016, 3, 19. [Google Scholar] [CrossRef]
- Hoque, M.E.; Khokan, M.R.; Bari, W. Impact of stature on non-communicable diseases: Evidence based on Bangladesh Demographic and Health Survey, 2011 data. BMC Public Health 2014, 14, 1007. [Google Scholar] [CrossRef]
- Rahman, M.S.; Akter, S.; Abe, S.K.; Islam, M.R.; Mondal, M.N.; Rahman, J.S.; Rahman, M.M. Awareness, Treatment, and Control of Diabetes in Bangladesh: A Nationwide Population-Based Study. PLoS ONE 2015, 10, E0118365. [Google Scholar] [CrossRef]
- Fottrell, E.; Ahmed, N.; Shaha, S.K.; Jennings, H.; Kuddus, A.; Morrison, J.; Akter, K.; Nahar, B.; Nahar, T.; Haghparast-Bidgoli, H.; et al. Diabetes knowledge and care practices among adults in rural Bangladesh: A cross-sectional survey. BMJ Glob. Health 2018, 3, e000891. [Google Scholar] [CrossRef] [PubMed]
- Biswas, T.; Islam, M.S.; Linton, N.; Rawal, L.B. Socio-Economic Inequality of Chronic Non-Communicable Diseases in Bangladesh. PLoS ONE 2016, 11, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Khan, J.A.M.; Ahmed, S.; MacLennan, M.; Sarker, A.R.; Sultana, M.; Rahman, H. Benefit incidence analysis of healthcare in Bangladesh—Equity matters for universal health coverage. Health Policy Plan. 2016. [Google Scholar] [CrossRef] [PubMed]
| Variables | Frequency (n = 938) | Percentage (%) | 95% Confidence Interval | |
|---|---|---|---|---|
| Lower Bound (%) | Upper Bound (%) | |||
| Age in years | ||||
| 35–39 | 136 | 14.6 | 11.9 | 17.3 |
| 40–44 | 147 | 15.6 | 13.0 | 18.2 |
| 45–49 | 151 | 15.7 | 13.0 | 18.4 |
| 50–54 | 120 | 12.8 | 10.2 | 15.3 |
| 55–59 | 123 | 13.3 | 10.9 | 15.8 |
| 60–64 | 82 | 8.8 | 6.8 | 10.8 |
| 65–69 | 53 | 6.4 | 4.5 | 8.3 |
| ≥70 | 126 | 12.9 | 10.3 | 15.4 |
| Sex | ||||
| Male | 468 | 49.0 | 45.7 | 52.4 |
| Female | 470 | 51.0 | 47.6 | 54.3 |
| Educational status | ||||
| No education | 297 | 35.5 | 31.4 | 39.5 |
| Primary | 260 | 27.5 | 24.1 | 30.9 |
| Secondary | 221 | 21.5 | 18.5 | 24.4 |
| Higher | 160 | 15.5 | 12.6 | 18.5 |
| Marital status | ||||
| Currently married | 777 | 83.4 | 80.6 | 86.2 |
| Divorced/separated/others | 161 | 16.6 | 13.8 | 19.4 |
| Nutritional status | ||||
| Normal | 495 | 55.1 | 51.8 | 58.5 |
| Thin | 154 | 18.4 | 15.2 | 21.5 |
| Overweight/obese | 261 | 26.5 | 23.3 | 29.7 |
| Physical activity levels at work | ||||
| Light physical activity | 576 | 63.0 | 59.7 | 66.3 |
| Moderate physical activity | 175 | 18.4 | 15.5 | 21.3 |
| Heavy physical activity | 178 | 18.6 | 15.7 | 21.5 |
| Households with children | ||||
| No child | 589 | 64.2 | 60.4 | 68.0 |
| Has child | 349 | 35.8 | 32.0 | 39.6 |
| Wealth quintile | ||||
| Poorest | 101 | 12.1 | 9.4 | 14.9 |
| Poorer | 98 | 12.3 | 9.5 | 15.2 |
| Middle | 125 | 14.3 | 11.6 | 17.1 |
| Richer | 191 | 22.1 | 18.6 | 25.5 |
| Richest | 423 | 39.1 | 35.0 | 43.2 |
| Division | ||||
| Barisal | 110 | 5.8 | 4.9 | 6.8 |
| Chittagong | 171 | 21.5 | 18.4 | 24.5 |
| Dhaka | 168 | 33.7 | 30.1 | 37.4 |
| Khulna | 123 | 9.7 | 8.4 | 11.0 |
| Rajshahi | 132 | 14.1 | 12.1 | 16.1 |
| Rangpur | 103 | 9.1 | 7.5 | 10.8 |
| Sylhet | 131 | 6.0 | 5.0 | 6.9 |
| Place of residence | ||||
| Urban | 420 | 33.9 | 30.5 | 37.3 |
| Rural | 518 | 66.1 | 62.7 | 69.5 |
| Variables | Undiagnosed Diabetes (%) | 95% Confidence Interval | Chi-Square Statistic (p-value) | |
|---|---|---|---|---|
| Lower Bound | Upper Bound | |||
| Age in years | 12.1 (0.2207) | |||
| 35–39 | 62.3 | 52.8 | 71.9 | |
| 40–44 | 55.7 | 47.0 | 64.3 | |
| 45–49 | 52.4 | 42.8 | 62.1 | |
| 50–54 | 50.1 | 40.3 | 60.0 | |
| 55–59 | 56.3 | 46.4 | 66.2 | |
| 60–64 | 40.3 | 28.1 | 52.6 | |
| 65–69 | 47.5 | 32.1 | 63.0 | |
| ≥70 | 53.4 | 43.4 | 64.2 | |
| Sex | 4.5 (0.0496) | |||
| Male | 56.9 | 51.5 | 62.2 | |
| Female | 50.0 | 44.8 | 55.2 | |
| Educational status | 61.0 (<0.001) | |||
| No education | 67.2 | 60.7 | 73.1 | |
| Primary | 56.1 | 48.7 | 63.2 | |
| Secondary | 41.8 | 33.8 | 50.2 | |
| Higher | 33.2 | 25.4 | 42.0 | |
| Marital status | 0.1 (0.8388) | |||
| Currently married | 53.6 | 49.0 | 58.1 | |
| Divorced/separated/others | 52.4 | 42.6 | 62.1 | |
| Nutritional status | 27.0 (<0.001) | |||
| Normal | 55.1 | 49.8 | 60.3 | |
| Thin | 66.8 | 56.2 | 76.0 | |
| Overweight/obese | 41.2 | 34.2 | 48.7 | |
| Physical activity levels at work | 29.1 (<0.001) | |||
| Light physical activity | 50.2 | 45.4 | 55.0 | |
| Moderate physical activity | 45.3 | 36.9 | 54.0 | |
| Heavy physical activity | 71.3 | 62.9 | 78.5 | |
| Households with children | 0.1 (0.7585) | |||
| No child | 53.8 | 48.6 | 59.0 | |
| Has child | 52.6 | 46.2 | 58.9 | |
| Division | 28.4 (<0.001) | |||
| Barisal | 68.0 | 59.2 | 75.8 | |
| Chittagong | 54.8 | 46.8 | 62.6 | |
| Dhaka | 44.4 | 35.8 | 53.3 | |
| Khulna | 53.1 | 42.8 | 63.1 | |
| Rajshahi | 52.9 | 43.8 | 61.8 | |
| Rangpur | 72.9 | 61.6 | 81.8 | |
| Sylhet | 56.6 | 44.9 | 67.5 | |
| Place of residence | 22.8 (<0.001) | |||
| Urban | 42.5 | 35.9 | 49.4 | |
| Rural | 59.0 | 53.9 | 63.8 | |
| Overall | 53.4 | 49.3 | 57.5 | |
| Variables | Unadjusted OR (95% CI) | Adjusted OR (95% CI) |
|---|---|---|
| Age in years | ||
| 35–39 (Reference) | 1 | 1 |
| 40–44 | 0.68 (0.43, 1.09) | 0.67 (0.39, 1.13) |
| 45–49 | 0.64 * (0.40, 1.05) | 0.53 ** (0.30, 0.90) |
| 50–54 | 0.43 *** (0.26, 0.71) | 0.33 *** (0.19, 0.59) |
| 55–59 | 0.61 ** (0.38, 0.98) | 0.57 ** (0.33, 0.99) |
| 60–64 | 0.41 *** (0.24, 0.71) | 0.35 *** (0.19, 0.66) |
| 65–69 | 0.59 * (0.32, 1.10) | 0.50 ** (0.25, 1.00) |
| ≥70 | 0.55 ** (0.33, 0.91) | 0.35 *** (0.19, 0.64) |
| Sex | ||
| Male (Reference) | 1 | |
| Female | 0.81 * (0.64, 1.03) | n/a |
| Educational status | ||
| No education (Reference) | 1 | 1 |
| Primary | 0.56 *** (0.40, 0.79) | 0.63 ** (0.43, 0.93) |
| Secondary | 0.40 *** (0.27, 0.58) | 0.48 *** (0.30, 0.76) |
| Higher | 0.27 *** (0.18, 0.41) | 0.36 *** (0.21, 0.62) |
| Marital status | ||
| Currently married (Reference) | 1 | |
| Divorced/separated/others | 0.99 (0.69, 1.41) | n/a |
| Nutritional status | ||
| Normal (Reference) | 1 | 1 |
| Thin | 1.90 *** (1.27, 2.85) | 1.17 (0.74, 1.87) |
| Overweight/obese | 0.71 ** (0.52, 0.97) | 1.04 (0.74, 1.47) |
| Physical activity levels at work | ||
| Light physical activity (Reference) | 1 | 1 |
| Moderate physical activity | 0.90 (0.64, 1.25) | 1.53 ** (1.01, 2.32) |
| Heavy physical activity | 2.06 *** (1.42, 3.01) | 1.73 ** (1.14, 2.64) |
| Households with children | ||
| No child (Reference) | 1 | |
| Has child | 0.96 (0.73, 1.27) | n/a |
| Wealth quintile | ||
| Richest (Reference) | 1 | 1 |
| Richer | 2.12 *** (1.45, 3.11) | 1.75 *** (1.15, 2.67) |
| Middle | 2.65 *** (1.69, 4.15) | 2.05 *** (1.21, 3.47) |
| Poorer | 4.66 *** (2.81, 7.71) | 3.52 *** (1.89, 6.54) |
| Poorest | 6.08 *** (3.63, 10.17) | 4.08 *** (2.12, 7.86) |
| Division | ||
| Barisal (Reference) | 1 | 1 |
| Chittagong | 0.64 * (0.40, 1.02) | 0.61 * (0.36, 1.03) |
| Dhaka | 0.41 *** (0.25, 0.69) | 0.36 *** (0.21, 0.64) |
| Khulna | 0.62 * (0.37, 1.03) | 0.51 ** (0.28, 0.92) |
| Rajshahi | 0.52 ** (0.31, 0.87) | 0.38 *** (0.22, 0.67) |
| Rangpur | 1.07 (0.58, 1.97) | 0.75 (0.38, 1.51) |
| Sylhet | 0.65 (0.38, 1.12) | 0.61 (0.34, 1.11) |
| Place of residence | ||
| Urban (Reference) | 1 | 1 |
| Rural | 1.75 *** (1.31, 2.34) | 0.89 (0.64, 1.25) |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hasan, M.M.; Tasnim, F.; Tariqujjaman, M.; Ahmed, S. Socioeconomic Inequalities of Undiagnosed Diabetes in a Resource-Poor Setting: Insights from the Cross-Sectional Bangladesh Demographic and Health Survey 2011. Int. J. Environ. Res. Public Health 2019, 16, 115. https://doi.org/10.3390/ijerph16010115
Hasan MM, Tasnim F, Tariqujjaman M, Ahmed S. Socioeconomic Inequalities of Undiagnosed Diabetes in a Resource-Poor Setting: Insights from the Cross-Sectional Bangladesh Demographic and Health Survey 2011. International Journal of Environmental Research and Public Health. 2019; 16(1):115. https://doi.org/10.3390/ijerph16010115
Chicago/Turabian StyleHasan, Md. Mehedi, Fariha Tasnim, Md. Tariqujjaman, and Sayem Ahmed. 2019. "Socioeconomic Inequalities of Undiagnosed Diabetes in a Resource-Poor Setting: Insights from the Cross-Sectional Bangladesh Demographic and Health Survey 2011" International Journal of Environmental Research and Public Health 16, no. 1: 115. https://doi.org/10.3390/ijerph16010115
APA StyleHasan, M. M., Tasnim, F., Tariqujjaman, M., & Ahmed, S. (2019). Socioeconomic Inequalities of Undiagnosed Diabetes in a Resource-Poor Setting: Insights from the Cross-Sectional Bangladesh Demographic and Health Survey 2011. International Journal of Environmental Research and Public Health, 16(1), 115. https://doi.org/10.3390/ijerph16010115





