Health Risks Associated with Occupational Exposure to Ambient Air Pollution in Commercial Drivers: A Systematic Review
Abstract
:1. Introduction
2. Methods
2.1. Data Sources and Search Strategy
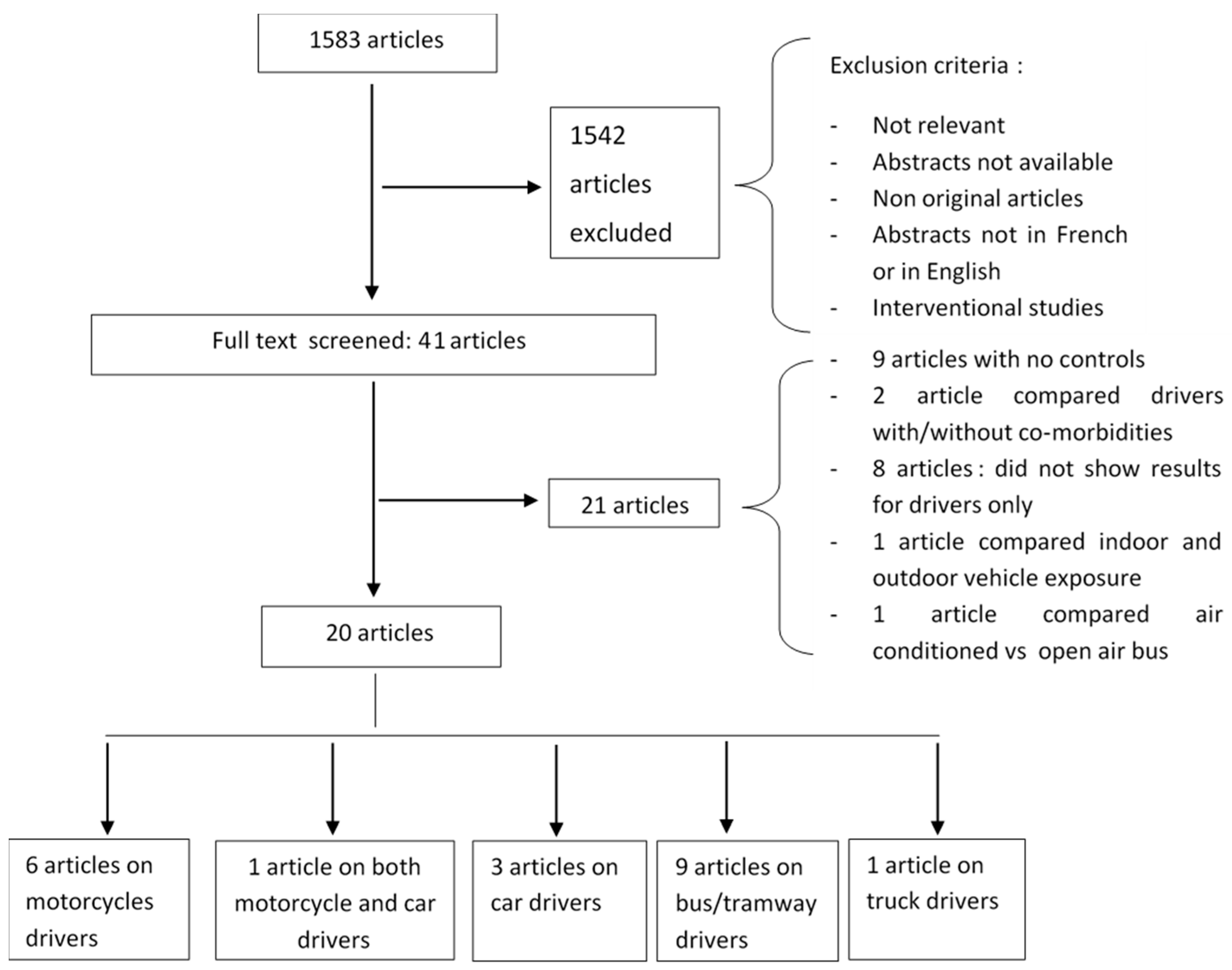
2.2. Study Selection
2.3. Data Extraction, Risk of Bias Assessment and Analysis
3. Results
3.1. Study Design and Site
3.2. Populations Studied
3.3. Exposure Variables Measured in Studies Included in the Review
3.4. Outcome Variables Measured in Studies Included in the Review
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- WHO. Oms|7 Millions de Décès Prématurés Sont Liés à la Pollution de L’air Chaque Année. Available online: http://www.who.int/mediacentre/news/releases/2014/air-pollution/fr/files/475/fr.html (accessed on 24 February 2018).
- Krzyżanowski, M.; Kuna-Dibbert, B.; Schneider, J. Health Effects of Transport-Related Air Pollution; WHO Regional Office Europe: København, Denmark, 2005; p. 205. [Google Scholar]
- Loomis, D.; Grosse, Y.; Lauby-Secretan, B.; Ghissassi, F.E.; Bouvard, V.; Benbrahim-Tallaa, L.; Guha, N.; Baan, R.; Mattock, H.; Straif, K. The carcinogenicity of outdoor air pollution. Lancet Oncol. 2013, 14, 1262–1263. [Google Scholar] [CrossRef]
- Assamoi, A.Y.E.-M. Emissions Anthropiques D’aérosols Carbonés en Afrique en 2005 et en 2030: Laboration D’inventaires et Évaluation. Ph.D. Thesis, Université de Toulouse, Université Toulouse III-Paul Sabatier, Toulouse, France, 2011. [Google Scholar]
- Sahabana, M. Les Motos-Taxis à Douala et Leur Perception par les Pouvoirs, Publics: Entre Tolérance d’un Secteur Pourvoyeur D’emplois et de Transport et Volonté D’éradiquer une Activité Incontrôlable; Laboratoire d’Economie des Transports: Vaulx-en-Velin, France, 2014. [Google Scholar]
- Choudhary, H.; Tarlo, S.M. Airway effects of traffic-related air pollution on outdoor workers. Curr. Opin. Allergy Clin. Immunol. 2014, 14, 106–112. [Google Scholar] [CrossRef] [PubMed]
- Avogbe, P.H.; Ayi-Fanou, L.; Autrup, H.; Loft, S.; Fayomi, B.; Sanni, A.; Vinzents, P.; Moller, P. Ultrafine particulate matter and high-level benzene urban air pollution in relation to oxidative DNA damage. Carcinogenesis 2005, 26, 613–620. [Google Scholar] [CrossRef] [PubMed]
- Ayi Fanou, L.; Mobio, T.A.; Creppy, E.E.; Fayomi, B.; Fustoni, S.; Møller, P.; Kyrtopoulos, S.; Georgiades, P.; Loft, S.; Sanni, A.; et al. Survey of air pollution in Cotonou, Benin—Air monitoring and biomarkers. Sci. Total Environ. 2006, 358, 85–96. [Google Scholar] [CrossRef] [PubMed]
- Ayi-Fanou, L.; Avogbe, P.H.; Fayomi, B.; Keith, G.; Hountondji, C.; Creppy, E.E.; Autrup, H.; Rihn, B.H.; Sanni, A. DNA-adducts in subjects exposed to urban air pollution by benzene and polycyclic aromatic hydrocarbons (pahs) in Cotonou, Benin. Environ. Toxicol. 2011, 26, 93–102. [Google Scholar] [CrossRef] [PubMed]
- Ekpenyong, C.E.; Ettebong, E.O.; Akpan, E.E.; Samson, T.K.; Daniel, N.E. Urban city transportation mode and respiratory health effect of air pollution: A cross-sectional study among transit and non-transit workers in Nigeria. BMJ Open 2012, 2, e001253. [Google Scholar] [CrossRef] [PubMed]
- Fourn, L.; Fayomi, E.B. Air pollution in urban area in Cotonou and Lokossa, Benin. Bull. Soc. Pathol. Exot. 2006, 99, 264–268. [Google Scholar] [PubMed]
- Avogbe, P.H.; Ayi-Fanou, L.; Cachon, B.; Chabi, N.; Debende, A.; Dewaele, D.; Aissi, F.; Cazier, F.; Sanni, A. Hematological changes among beninese motor-bike taxi drivers exposed to benzene by urban air pollution. Afr. J. Environ. Sci. Technol. 2011, 57, 464–472. [Google Scholar]
- Lawin, H.; Agodokpessi, G.; Ayelo, P.; Kagima, J.; Sonoukon, R.; Mbatchou Ngahane, B.H.; Awopeju, O.; Vollmer, W.M.; Nemery, B.; Burney, P.; et al. A cross-sectional study with an improved methodology to assess occupational air pollution exposure and respiratory health in motorcycle taxi driving. Sci. Total Environ. 2016, 550, 1–5. [Google Scholar] [CrossRef] [PubMed]
- Brucker, N.; Moro, A.M.; Charao, M.F.; Durgante, J.; Freitas, F.; Baierle, M.; Nascimento, S.; Gauer, B.; Bulcao, R.P.; Bubols, G.B.; et al. Biomarkers of occupational exposure to air pollution, inflammation and oxidative damage in taxi drivers. Sci. Total Environ. 2013, 463–464, 884–893. [Google Scholar] [CrossRef] [PubMed]
- Burgaz, S.; Demircigil, G.C.; Karahalil, B.; Karakaya, A.E. Chromosomal damage in peripheral blood lymphocytes of traffic policemen and taxi drivers exposed to urban air pollution. Chemosphere 2002, 47, 57–64. [Google Scholar] [CrossRef]
- Taghizadeh, S.; Najmabadi, H.; Kamali, K.; Behjati, F. Evaluation of chromosomal aberrations caused by air pollutants in some taxi drivers from two polluted districts of urban tehran and its comparison with drivers from rural areas of Lahijan: A pilot study. J. Environ. Health Sci. Eng. 2014, 12, 144. [Google Scholar] [CrossRef] [PubMed]
- Hart, J.E.; Garshick, E.; Smith, T.J.; Davis, M.E.; Laden, F. Ischaemic heart disease mortality and years of work in trucking industry workers. Occup. Environ. Med. 2013, 70, 523–528. [Google Scholar] [CrossRef] [PubMed]
- Bagryantseva, Y.; Novotna, B.; Rossner, P., Jr.; Chvatalova, I.; Milcova, A.; Svecova, V.; Lnenickova, Z.; Solansky, I.; Sram, R.J. Oxidative damage to biological macromolecules in prague bus drivers and garagemen: Impact of air pollution and genetic polymorphisms. Toxicol. Lett. 2010, 199, 60–68. [Google Scholar] [CrossRef] [PubMed]
- Han, Y.Y.; Donovan, M.; Sung, F.C. Increased urinary 8-hydroxy-2’-deoxyguanosine excretion in long-distance bus drivers in Taiwan. Chemosphere 2010, 79, 942–948. [Google Scholar] [CrossRef] [PubMed]
- Hansen, A.M.; Wallin, H.; Binderup, M.L.; Dybdahl, M.; Autrup, H.; Loft, S.; Knudsen, L.E. Urinary 1-hydroxypyrene and mutagenicity in bus drivers and mail carriers exposed to urban air pollution in Denmark. Mutat. Res. 2004, 557, 7–17. [Google Scholar] [CrossRef] [PubMed]
- Merlo, D.F.; Stagi, E.; Fontana, V.; Consonni, D.; Gozza, C.; Garrone, E.; Bertazzi, P.A.; Pesatori, A.C. A historical mortality study among bus drivers and bus maintenance workers exposed to urban air pollutants in the city of Genoa, Italy. Occup. Environ. Med. 2010, 67, 611–619. [Google Scholar] [CrossRef] [PubMed]
- Nielsen, P.S.; de Pater, N.; Okkels, H.; Autrup, H. Environmental air pollution and DNA adducts in copenhagen bus drivers—Effect of gstm1 and nat2 genotypes on adduct levels. Carcinogenesis 1996, 17, 1021–1027. [Google Scholar] [CrossRef] [PubMed]
- Petchpoung, K.; Kaojarern, S.; Yoovathaworn, K.; Sura, T.; Sirivarasai, J. The influence of metabolic gene polymorphisms on urinary 1-hydroxypyrene concentration in thai bus drivers. Environ. Toxicol. Pharmacol. 2011, 31, 160–164. [Google Scholar] [CrossRef] [PubMed]
- Rossner, P., Jr.; Svecova, V.; Milcova, A.; Lnenickova, Z.; Solansky, I.; Santella, R.M.; Sram, R.J. Oxidative and nitrosative stress markers in bus drivers. Mutat. Res. 2007, 617, 23–32. [Google Scholar] [CrossRef] [PubMed]
- Rossner, P., Jr.; Svecova, V.; Milcova, A.; Lnenickova, Z.; Solansky, I.; Sram, R.J. Seasonal variability of oxidative stress markers in city bus drivers. Part ii. Oxidative damage to lipids and proteins. Mutat. Res. 2008, 642, 21–27. [Google Scholar] [CrossRef] [PubMed]
- Soll-Johanning, H.; Bach, E.; Olsen, J.H.; Tuchsen, F. Cancer incidence in urban bus drivers and tramway employees: A retrospective cohort study. Occup. Environ. Med. 1998, 55, 594–598. [Google Scholar] [CrossRef] [PubMed]
- Eye, P. Swiss Commodity Trader Trafigura Is Selling Toxic Fuel to Africa. Available online: https://www.publiceye.ch/en/campaigns/dirtydiesel/files/708/dirtydiesel.html (accessed on 18 January 2018).
- Ryan, P.H.; LeMasters, G.K. A review of land-use regression models for characterizing intraurban air pollution exposure. Inhal. Toxicol. 2007, 19, 127–133. [Google Scholar] [CrossRef] [PubMed]
| MeSH* Keywords | ||
|---|---|---|
| And | “Air pollution” |
| Inclusion Criteria | Exclusion Criteria |
|---|---|
|
|
| Authors | Study Design/Site | Type of Drivers (Number) | Comparative Study Population (Number) | Exposure | Outcomes | Key Findings |
|---|---|---|---|---|---|---|
| Avogbe et al. [7] | Cross-sectional/Cotonou (Benin) | Motorcycle (n = 29) | 1. Rural subjects (n = 27) 2. Roadside residents (n = 37) 3. Suburban subjects (n = 42) | 1. PM0.1 (fixed site) measured during the working day 2. S-phenylmercapturic acid (S-PMA) | 1. oxidative DNA damage in mononuclear blood cells: strand breaks (SB) and formamidopyrimidine glycosylase (FPG) 2. GlutathioneS-transferase (GST) 3. Glutathione peroxidase (GPX) 4. NAD(P)H:quinone oxidoreductase 1 (NQO1) | 1. Stepwise exposure gradient (rural Subjects < suburban subjects < Roadside residents < taxi-moto drivers) 2. NSD in the distribution of most of the genes + inhomogeneous distribution 3. SD in the distribution of SB and FPG sensitive sites |
| Ayi Fanou et al. [8] | Panel study/Cotonou (Benin) | Motorcycle stage 1 (n = 35) stage 2 (n = 6) | Stage 1 1. Rural subjects (n = 6) Stage 2 1. Rural subjects (n = 5) 2. Roadside residents (n = 12) | 1. Urine benzene 2. S-PMA 3. 1-hydroxypyrene (1-OHP)4. Personal exposure to Benzene, Toluene, Ethyl benzene and Xylene (BTEX) per week | 1. DNA adducts 2. DNA fragmentation 3. oxidized DNA: 8-hydroxy-2V-deoxyguanosine (8-oxodG) and 5-methylcytosine (m5dC) | 1. More BTEX and S-PMA in urban drivers than in rural residents 2. NSD of BTEX and S-PMA difference in taxi-drivers and roadside residents 3. NSD of 1-hydroxypyrene (urban drivers vs. rural area) 4. SD in DNA damage (when compared urban drivers vs. rural area inhabitants) but NSD in oxidized DNA (when comparing urban drivers vs. rural area inhabitants) |
| Ayi Fanou et al. [9] | Cross-sectional/Cotonou (Benin) | Motorcycle (n = 13) | 1. Street vendors (n = 16) 2. Gasoline sellers (n = 17) 3. Roadside residents(n = 11) 4. Suburban residents(n = 20) 5. Rural inhabitants | 1. Benzene (fixed site)/working day 2. Polycyclic aromatic hydrocarbons (PAHs)mainly benzo(a)pyrene (B[a]P) (6h/day/3 consecutive days) 4. 1-OHP 5. Phenol (urine) | DNA adducts | 1. urban drivers are more exposed than rural inhabitants 2. NSD in Phenol and 1-OH level among urban drivers, street vendors, gasoline sellers vs. roadside residents 3. More DNA adducts in urban drivers than rural inhabitants |
| Ekpenyong, Ettebong et al. [10] * | Cross-sectional/Uyo metropolis, (South-South Nigeria) | Motorcycle (n = 24) Automobile taxi (n = 18) | Civil servants (n = 6) | 1. CO 2. SO2 3. NO2 4. PM2.5 and PM10 Fixed station /07:30 and 09:30 (peak traffic periods) and 15:30 to 17: 30 (low traffic periods) and some personal exposure | 1.Respiratory symptoms 2. Lung function | 1. NSD in lung function impairment in drivers vs. civil servants 2. More respiratory symptoms among drivers |
| Fourn and Fayomi [11] | Cross-sectional/Cotonou and Lokossa (Benin) | Motorcycle (n = 250 in Cotonou n = 150 in Lokossa) | Non-drivers in each location | 1. Personal Carboxyhaemoglobin 2. CO/morning and afternoon/Fixed station 3. Benzène/morning/Fixed station | Health disorders (headache, arterial hypertension, respiratory symptoms, digestive disorders, conjunctival hyperemia, photophobia) | 1. More health disorders in Cotonou drivers 2. NSD for most of the health disorders especially respiratory symptoms (Drivers vs. non-drivers in Cotonou) |
| Avogbe et al. [12] | Cross-sectional/Cotonou (Benin) | Motorcycle (n = 144) | “Age and sex matched” Rural inhabitants (n = 30) | 1. Benzene (personal) 3. BTEX | 12 parameters from complete blood counts: total white blood cells (WBC) with four WBCsubtypes (neutrophils, eosinophils, monocytes, and lymphocytes), total red blood cells (RBC) with five red cell-related measures (hemoglobin, hematocrit, mean corpuscular volume (MCV), mean corpuscular hemoglobin concentration (MCHC) and mean corpuscular hemoglobin (MCH)) and platelets | 1. Drivers were more exposed than rural inhabitants 2. Decrease only in white blood cells, lymphocyte and eosinophil counts |
| Lawin et al. [13] | Cross-sectional/Cotonou (Benin) | Motorcycle (n = 85) | Individual matched group (n = 85) | CO | Lung function | 1. Drivers were more exposed 2. NSD in lung function and respiratory symptoms |
| Authors | Study Design/Site | Type of Drivers (Number) | Comparative Study Population (Number) | Exposure | Outcomes | Key Findings |
|---|---|---|---|---|---|---|
| Brucker et al. [14] | Cross-sectional/Porto Alegre, Brazil | Automobile taxi (n = 39) | Non-occupationally exposed (n = 21) | 1. Carboxyhaemoglobin (COHb) 2. 1-hydroxypyrene (1-OHP) | 1. Platelets 2. Glucose (mg dL−1)3. Total cholesterol, HDL cholesterol, LDL cholesterol, Total cholesterol/HDL-c ratio, Triglycerides 3. Oxidized-LDL (Ox-LDL) and autoantibodies against ox-LDL (Ox-LDL-Ab) 4. Malondialdehyde (MDA) 5. Protein carbonyl (PCO) 6. Catalase (CAT) 7. Glutathione peroxidase (GPX) 8. GST 9. High-sensitivity C reactive protein (hs-CRP) 10. Homocysteine(Hcy) 11. Cytokines: Interleukin-1β (IL-1β), IL-6, IL-10,tumour necrosis factor-α (TNF-α), interferon-γ (IFN-γ) 12. Vitamin C | 1. More 1-OHP in drivers than in controls but not for COHb 2. NSD for platelets, glucose, total cholesterol 3. More ox-LDL and Ox-LDL-Ab, cytokines,hs-CRP,MDA, PCO in drivers than in controls 4. Decrease in CAT, GPX, GST, vitamin C among drivers |
| Burgaz et al. [15] | Cross-sectional/Ankara (Turkey) | Automobile drivers (n = 7) | Traffic policemen (n = 5) Office workers (n = 9) | 1-hydroxypyrene (1-OHP) | Chromosomal aberration (CA) | 1. Controls excreted more 1-OHP than drivers and traffic policemen 2. Drivers had more CA |
| Taghizadeh et al. [16] | Cross-sectional/Teheran (Iran) | Urban taxi (n = 30) | Rural taxi drivers (n = 30) | N/A | 1. Chromosome breakage (CB) 2. Chromosome aberration (CA) rate (including both chromosome andchromatid gaps) | 1. Urban drivers had more CA 2. NSD in urban vs rural drivers regarding CB |
| Authors | Study Design/Site | Type of Drivers (Number) | Comparative Study Population (Number) | Exposure | Outcomes | Key Findings |
|---|---|---|---|---|---|---|
| Hart et al. [17] | Cohort study (1985–2000)/US | Long haul up (n = 13,752) and Pick- and delivery (P&D) drivers (n = 8930) | Non-drivers in trucking industry | Job title and residential exposure to PM10, NO2 and SO2 | Ischemic heart Disease (IHD) deaths (number and Hazard ratios for IHD mortality associated with at least one year of work in each specific job category) | Long haul drivers had more IHD deaths Hazard ratio = 1.44 [1.22, 1.70] |
| Authors | Study Design/Site | Type of Drivers (Number) | Comparative Study Population (Number) | Exposure | Outcomes | Key Findings |
|---|---|---|---|---|---|---|
| Bagryantseva et al. [18] | Cross-sectional/Prague (Czech Republic) | Bus (n = 50) | 1. Garagemen (n = 20) 2. Administrative workers (n = 50) | 1. total carcinogenic PAHs including B[a]P)/48 h 2. BTEX/24 h | 1. Percentage of DNA in the tail (Tail DNA %). 2. Total DNA damage (with enzymes) 3. DNA-SB or unspecified DNAdamage; without enzymes) 3. urinary excretion of 8-oxodG 4. Urinary 15-F2t-IsoP (oxidative damage to lipids) 5. Protein carbonyl 6. Polymorphisms of metabolic genes (CYP1A1, GSTM1, GSTP1, GSTT1, EPHX3,4), folic acid metabolism genes (MS, MTHFR) and DNA repair genes (XRCC1, XPD6, XPD23, hOGG1) | 1. Drivers were more exposed than administrative workers 2. Almost the same exposure for drivers and garagemen (p value not shown) 3. NSD in Tail DNA% (drivers vs administrative workers) 4. Drivers had more DNA-SB, 8-oxodG, 15-F2t-IsoP than administrative workers 5. Almost the same oxidative damage (drivers vs. garagemen, p value not shown) |
| Han et al. [19] | Cross-sectional/Taiwan | Bus (n = 120) | Office workers (n = 58) | N/A | 8-oxodG (24 h sampling) | drivers > office workers |
| Hansen et al. [20] | Cross-sectional (Denmark) | Bus (n = 60) | Mail carriers (n = 88) | 1-hydroxypyrene (working day and day off) | N-acetyltransferase (NAT2) phenotype | Drivers were more exposed than mail carriers |
| Merlo et al. [21] | Cohort study/Genoa (Italy) 1970–2005 | Bus (n = 6510) | 1.Maintenance workers (n = 2073) 2. White collar (n = 601) | Job title | Standardized mortality ratios (SMRs) | More SMRs for all causes of deaths and lung diseases in maintenance workers than in drivers than in white collar |
| Nielsen et al. [22] | Cross-sectional/Copenhagen (Denmark) | Bus (n = 90) Divided regarding gradient of exposition (central, dormitory and suburban | Rural inhabitants (n = 60) | N/A | DNA adducts | Drivers had more DNA adducts |
| Petchpoung et al. [23] | Cross-sectional/Bangkok (Thailand) | Bus (n = 100) | Rural inhabitants (n = 100) | 1-OHP | 1. cytochrome P4501A1 (CYP1A1) 2. GSTM1 3. GSTP1 4. GSTT1 | 1. Driver excreted more 1-hydroxypyrene (1-OHP) 2. The genotypedistribution was almost the same |
| Rossner et al. [24] | Cross-sectional/Prague (Czech Republic) | Bus (n = 50) | controls (n = 50) healthy male volunteers spending >90% of daily time indoors | PM 2.5 PM 10 cPAHs (B[a]P) | 1. PCO 2. 8-oxodG 3. 15-F2t-IsoP 4. Nitrotyrosine (NT) | 1. cPAHs: controls > drivers 2. More oxidative stress in drivers |
| Rossner et al. [25] | Cohort/Prague (Czech Republic) 03 seasons | Bus (n = 50) | controls (n = 50) healthy male volunteers spending >90% of daily time indoors | PM 2.5 PM 10 cPAHs (B[a]P)BTEX Personal/fixed monitoring | 1. PCO 2. 15-F2t-IsoP | PCO and 15-F2t-IsoP: Drivers > controls in both winter (2005–2006) but not in summer |
| Soll-Johanning et al. [26] | Cohort/Copenhagen (Denmark) | Bus (n = 18,120) | Other people in Denmark | Job title | Cancer risk | Drivers > general population Lung cancer rates [relative risk (RR) = 1.695% confidence interval (95% CI) = 1.5–1.8] and bladder cancer rates (RR = 1.4, 95% CI = 1.2–1.6) |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lawin, H.; Ayi Fanou, L.; Hinson, A.V.; Stolbrink, M.; Houngbegnon, P.; Kedote, N.M.; Fayomi, B.; Kagima, J.; Katoto, P.; Ouendo, E.M.D.; et al. Health Risks Associated with Occupational Exposure to Ambient Air Pollution in Commercial Drivers: A Systematic Review. Int. J. Environ. Res. Public Health 2018, 15, 2039. https://doi.org/10.3390/ijerph15092039
Lawin H, Ayi Fanou L, Hinson AV, Stolbrink M, Houngbegnon P, Kedote NM, Fayomi B, Kagima J, Katoto P, Ouendo EMD, et al. Health Risks Associated with Occupational Exposure to Ambient Air Pollution in Commercial Drivers: A Systematic Review. International Journal of Environmental Research and Public Health. 2018; 15(9):2039. https://doi.org/10.3390/ijerph15092039
Chicago/Turabian StyleLawin, Herve, Lucie Ayi Fanou, Antoine Vikkey Hinson, Marie Stolbrink, Parfait Houngbegnon, Nonvignon Marius Kedote, Benjamin Fayomi, Jacqueline Kagima, Patrick Katoto, Edgard Marius Dona Ouendo, and et al. 2018. "Health Risks Associated with Occupational Exposure to Ambient Air Pollution in Commercial Drivers: A Systematic Review" International Journal of Environmental Research and Public Health 15, no. 9: 2039. https://doi.org/10.3390/ijerph15092039
APA StyleLawin, H., Ayi Fanou, L., Hinson, A. V., Stolbrink, M., Houngbegnon, P., Kedote, N. M., Fayomi, B., Kagima, J., Katoto, P., Ouendo, E. M. D., & Mortimer, K. (2018). Health Risks Associated with Occupational Exposure to Ambient Air Pollution in Commercial Drivers: A Systematic Review. International Journal of Environmental Research and Public Health, 15(9), 2039. https://doi.org/10.3390/ijerph15092039






