Exposure to Secondhand Smoke and Risk of Cancer in Never Smokers: A Meta-Analysis of Epidemiologic Studies
Abstract
1. Introduction
2. Materials and Methods
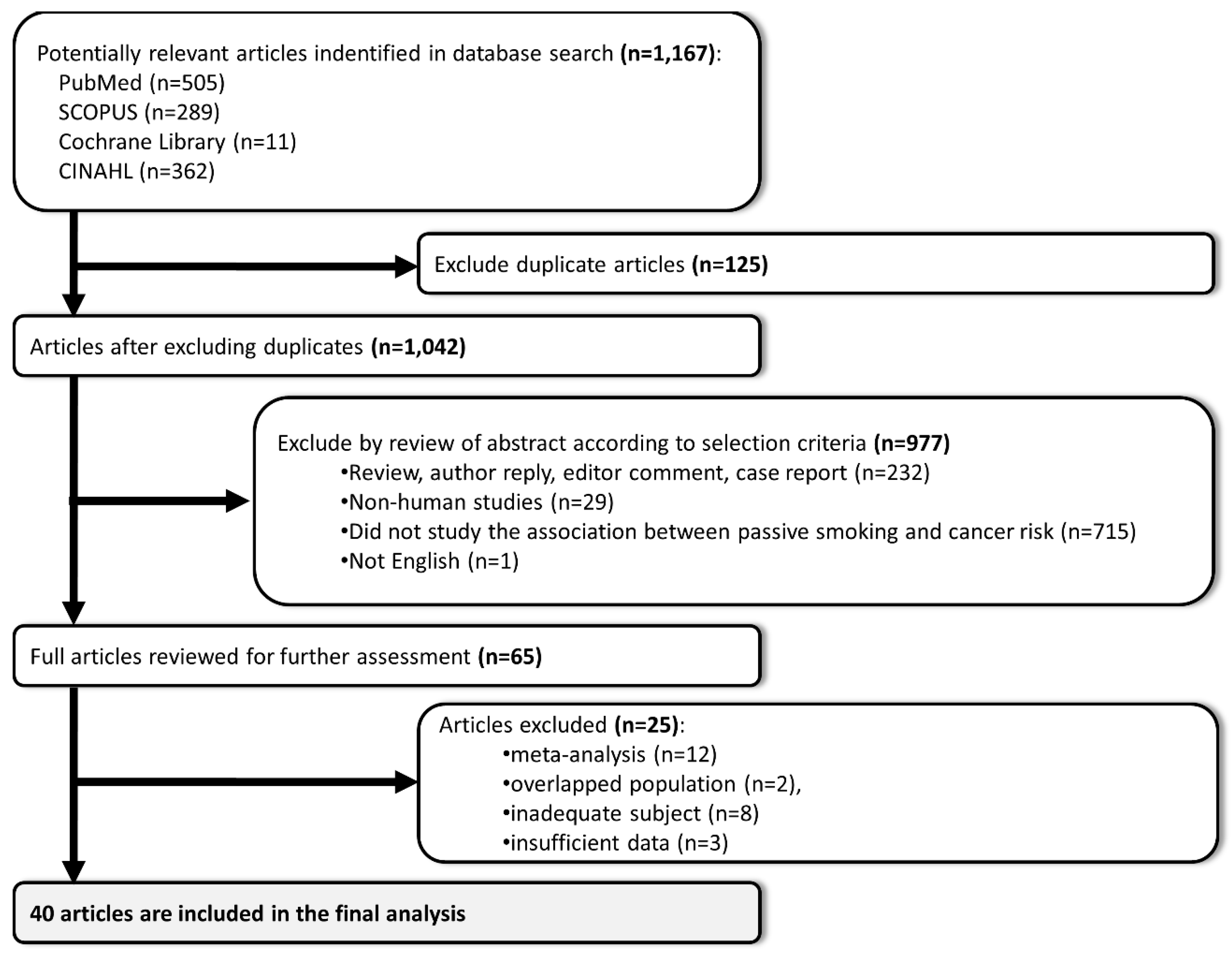
2.1. Literature Search
2.2. Study Selection
2.3. Data Extraction
2.4. Quality Assessment
2.5. Statistical Analysis
3. Results
3.1. Description of Selected Studies
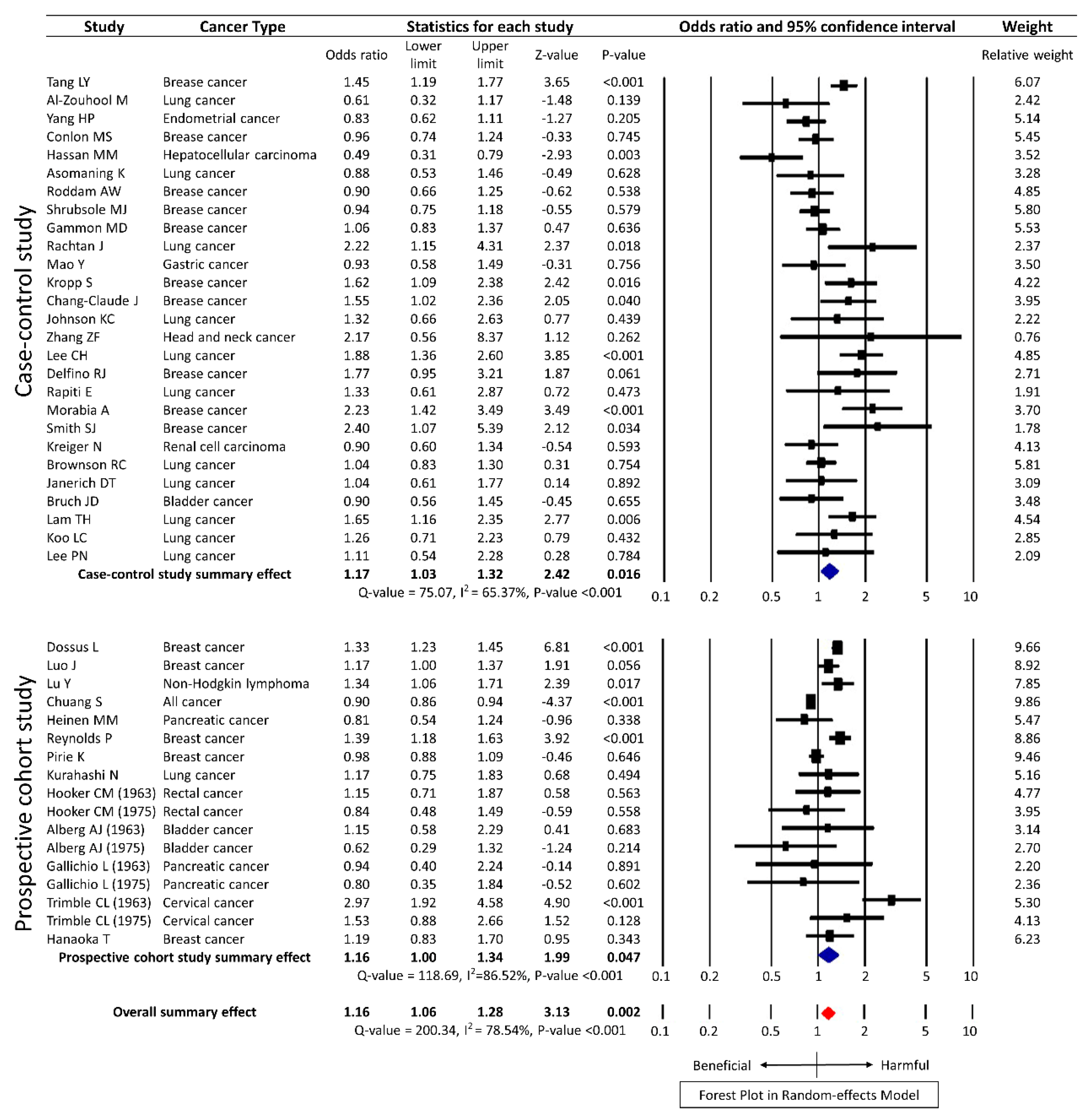
3.2. Secondhand Smoking and the Risk of Cancer
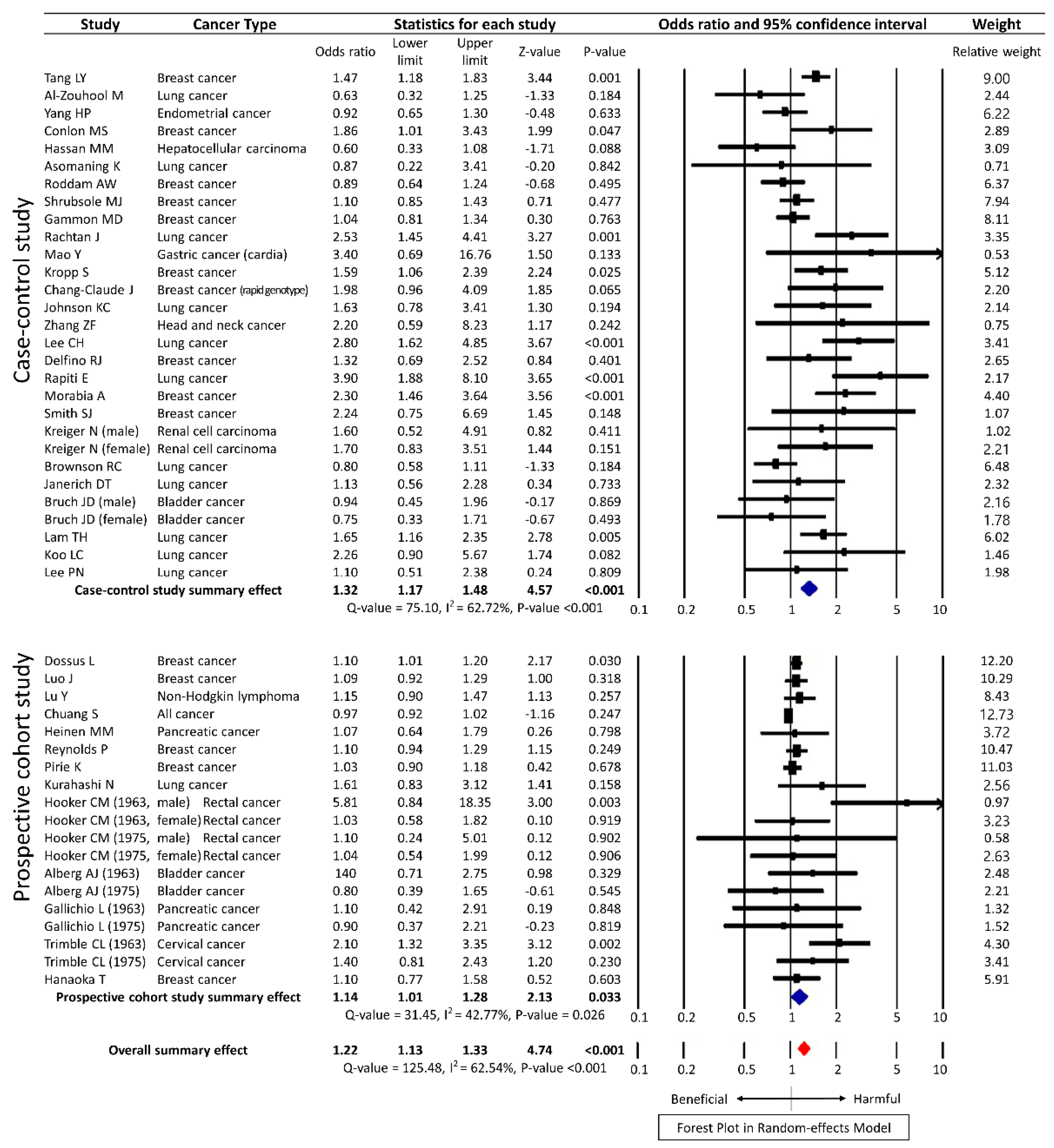
3.3. Subgroup Analysis
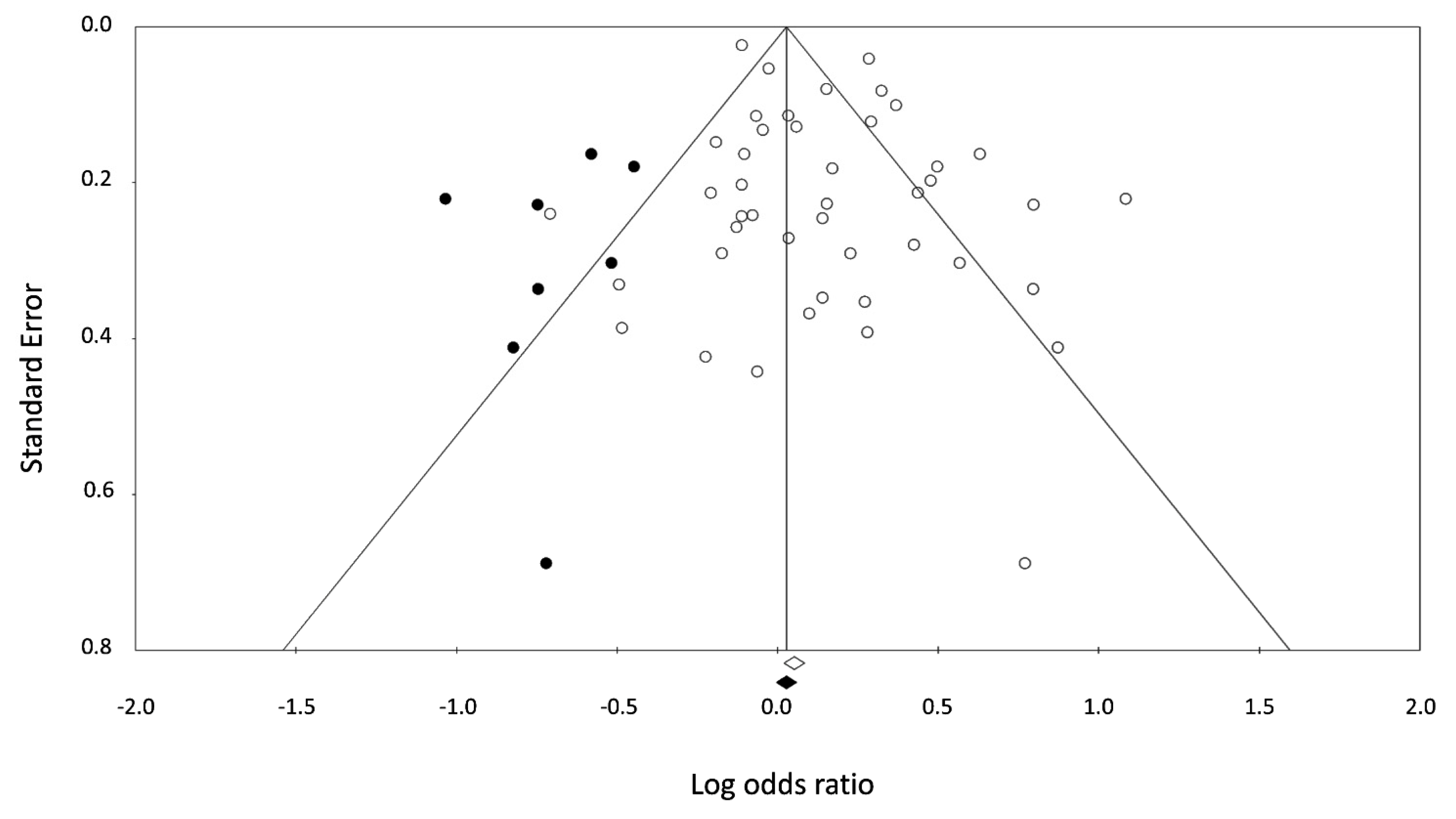
3.4. Publication Bias
4. Discussion
5. Conclusions
Author Contributions
Acknowledgments
Conflicts of Interest
Appendix A
| Study | Adjusted Factors |
|---|---|
| Dossus L. (2014) [29] | Body mass index, educational level, hormone use, menopausal status, parity and age at first-term pregnancy, age at menarche, alcohol consumption, physical activity. |
| Tang L.Y. (2013) [30] | Age, marital status, long-term alcohol use, age at menarche, body mass index, parity, education, family history of breast cancer. |
| Al-Zoughool M. (2013) [31] | Sex, age, educational level, household income. |
| Luo J. (2011) [32] | Age, ethnicity, education, body mass index, physical activity, alcohol intake, parity, family history of breast cancer, hormone therapy, age at menarche, age of first live birth. |
| Lu Y. (2011) [33] | Age, race, alcohol intake. |
| Chuang S.C. (2011) [34] | Age, sex, study canter, education, alcohol intake, body mass index, physical activity, vegetable intake, fruit intake, energy intake, adulthood passive smoking. |
| Yang H.P. (2010) [35] | Age, study site, education, age at menarche, parity, oral contraceptives, hormone use, body mass index, menopausal status. |
| Heinen M.M. (2010) [36] | Age, body mass index, education. |
| Conlon M.S. (2010) [37] | Age. |
| Reynolds P. (2009) [38] | Age, race, family history of breast cancer, age at menarche, pregnancy history, lifetime duration of breast-feeding, physical activity, alcohol intake, body mass index, menopausal status, hormone use. |
| Pirie K. (2008) [39] | Age, region of residence, socio-economic status, age at menarche, parity, age at first birth, menopausal status, body mass index, physical activity, alcohol intake, hormone use. |
| Kurahashi N. (2008) [17] | Age, area, alcohol intake, family history of lung cancer, menopausal status. |
| Hooker C.M. (2008) [19] | Age, education, marital status. |
| Hassan M.M. (2008) [40] | Age, sex, race, education, marital status, area, Hepatitis C, Hepatitis B, diabetes, alcohol intake, family history of cancer. |
| Asomaning K. (2008) [41] | Age, sex, smoking status. |
| Roddam A.W. (2007) [42] | Age, region, socioeconomic status, alcohol intake, body mass index, parity, age at first birth, hormone use, family history of breast cancer, age at menarche, menopausal status. |
| Alberg A.J. (2007) [20] | Age, education, marital status. |
| Gallicchio L. (2006) [21] | Age, education, marital status. |
| Trimble C.L. (2005) [22] | Age, education, marital status. |
| Hanaoka T. (2005) [18] | Age, public health center, employment status, education level, body mass index, family history of breast cancer, past history of benign breast disease, age at menarche, number of births, menopausal status, hormone use, alcohol intake. |
| Shrubsole M.J. (2004) [43] | Age, education, family history of breast cancer, personal history of fibroadenoma, age at menarche, parity, age at first live birth, menopausal status, physical activity, waist-to-hip ratio. |
| Gammon M.D. (2004) [44] | Age, history of benign breast disease, body mass index, family history of breast cancer, history of fertility problems, number of pregnancies, menopausal status, weight in year prior to reference date. |
| Rachtan J. (2002) [45] | Age. |
| Mao Y. (2002) [46] | Age, province, education, social class, food consumption. |
| Kropp S. (2002) [47] | Age, alcohol intake, breastfeeding, education family history of breast cancer, menopausal status, body mass index. |
| Chang-Claude J. (2002) [48] | Age, number of pregnancy, breastfeeding, body mass index, alcohol intake, family history, education, menopausal status. |
| Johnson K.C. (2001) [11] | Age, province, education, fruit and vegetable consumption. |
| Zhang Z.F. (2000) [49] | Age, sex. |
| Lee C.H. (2000) [10] | Residential area, education, occupation, tuberculosis, cooking fuels and fume extractor. |
| Delfino R.J. (2000) [50] | Age, menopausal status, family history of breast cancer. |
| Rapiti E. (1999) [51] | Age, sex, residence, religion. |
| Morabia A. (1996) [52] | Age, education, body mass index, age at menarche, age at first live birth, hormone use, family history of breast cancer, history of breast biopsy. |
| Smith S.J. (1994) [53] | Age, region, age at menarche, nulliparity, age at first full-term pregnancy, breastfeeding, hormone use, family history of breast cancer, biopsy for benign breast disease, alcohol intake. |
| Kreiger N. (1993) [54] | Age, combined Quetelet index. |
| Brownson R.C. (1992) [55] | Age, history of previous lung disease. |
| Janerich D.T. (1990) [56] | Age, sex, country of residence. |
| Burch J.D. (1989) [57] | Age, sex, location. |
| Lam T.H. (1987) [58] | Age. |
| Koo L.C. (1987) [59] | Age, number of live births, education, years since exposure. |
| Lee P.N. (1986) [60] | Age, sex, hospital region, hospital ward, time of interview. |
References
- Korea, S. Annual Report on the Cause of Death Statistics in 2015. Statistics Korea: Daejeon, Korea. Available online: http://kostat.go.kr/ (accessed on 24 February 2016).
- Doll, R.; Hill, A.B. Smoking and carcinoma of the lung; preliminary report. Br. Med. J. 1950, 2, 739–748. [Google Scholar] [CrossRef] [PubMed]
- Wynder, E.L.; Graham, E.A. Tobacco smoking as a possible etiologic factor in bronchiogenic carcinoma; a study of 684 proved cases. J. Am. Med. Assoc. 1950, 143, 329–336. [Google Scholar] [CrossRef] [PubMed]
- Sasco, A.J.; Secretan, M.B.; Straif, K. Tobacco smoking and cancer: A brief review of recent epidemiological evidence. Lung Cancer 2004, 45 (Suppl. 2), S3–S9. [Google Scholar] [CrossRef]
- Lee, P.N.; Forey, B.A.; Coombs, K.J. Systematic review with meta-analysis of the epidemiological evidence in the 1900s relating smoking to lung cancer. BMC Cancer 2012, 12, 385. [Google Scholar] [CrossRef] [PubMed]
- Thun, M.J.; Henley, S.J.; Burns, D.; Jemal, A.; Shanks, T.G.; Calle, E.E. Lung cancer death rates in lifelong nonsmokers. J. Natl. Cancer Inst. 2006, 98, 691–699. [Google Scholar] [CrossRef] [PubMed]
- Centers for Disease Control and Prevention. Annual smoking-attributable mortality, years of potential life lost, and productivity losses–United States, 1997–2001. Morb. Mortal. Wkly. Rep. 2005, 54, 625–628. [Google Scholar]
- Hirayama, T. Non-smoking wives of heavy smokers have a higher risk of lung cancer: A study from Japan. Br. Med. J. (Clin. Res. Ed.) 1981, 282, 183–185. [Google Scholar] [CrossRef]
- Trichopoulos, D.; Kalandidi, A.; Sparros, L.; MacMahon, B. Lung cancer and passive smoking. Int. J. Cancer 1981, 27, 1–4. [Google Scholar] [CrossRef] [PubMed]
- Lee, C.H.; Ko, Y.C.; Goggins, W.; Huang, J.J.; Huang, M.S.; Kao, E.L.; Wang, H.Z. Lifetime environmental exposure to tobacco smoke and primary lung cancer of non-smoking Taiwanese women. Int. J. Epidemiol. 2000, 29, 224–231. [Google Scholar] [CrossRef] [PubMed]
- Johnson, K.C.; Hu, J.; Mao, Y. Lifetime residential and workplace exposure to environmental tobacco smoke and lung cancer in never-smoking women, Canada 1994–1997. Int. J. Cancer 2001, 93, 902–906. [Google Scholar] [CrossRef] [PubMed]
- Hecht, S.S.; Carmella, S.G.; Murphy, S.E.; Akerkar, S.; Brunnemann, K.D.; Hoffmann, D. A tobacco-specific lung carcinogen in the urine of men exposed to cigarette smoke. N. Engl. J. Med. 1993, 329, 1543–1546. [Google Scholar] [CrossRef] [PubMed]
- Maclure, M.; Katz, R.B.; Bryant, M.S.; Skipper, P.L.; Tannenbaum, S.R. Elevated blood levels of carcinogens in passive smokers. Am. J. Public Health 1989, 79, 1381–1384. [Google Scholar] [CrossRef] [PubMed]
- Mauderly, J.L.; Gigliotti, A.P.; Barr, E.B.; Bechtold, W.E.; Belinsky, S.A.; Hahn, F.F.; Hobbs, C.A.; March, T.H.; Seilkop, S.K.; Finch, G.L. Chronic inhalation exposure to mainstream cigarette smoke increases lung and nasal tumor incidence in rats. Toxicol. Sci. 2004, 81, 280–292. [Google Scholar] [CrossRef] [PubMed]
- Hackshaw, A.K.; Law, M.R.; Wald, N.J. The accumulated evidence on lung cancer and environmental tobacco smoke. Br. Med. J. 1997, 315, 980–988. [Google Scholar] [CrossRef]
- US Department of Health and Human Services. The Health Consequences of Involuntary Exposure to Tobacco Smoke: A Report of the Surgeon General; Surgeon General’s Report; US Department of Health and Human Services, Centers for Disease Control and Prevention, Coordinating Center for Health Promotion, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health: Atlanta, GA, USA, 2006.
- Kurahashi, N.; Inoue, M.; Liu, Y.; Iwasaki, M.; Sasazuki, S.; Sobue, T.; Tsugane, S. Passive smoking and lung cancer in Japanese non-smoking women: A prospective study. Int. J. Cancer 2008, 122, 653–657. [Google Scholar] [CrossRef] [PubMed]
- Hanaoka, T.; Yamamoto, S.; Sobue, T.; Sasaki, S.; Tsugane, S. Active and passive smoking and breast cancer risk in middle-aged Japanese women. Int. J. Cancer 2005, 114, 317–322. [Google Scholar] [CrossRef] [PubMed]
- Hooker, C.M.; Gallicchio, L.; Genkinger, J.M.; Comstock, G.W.; Alberg, A.J. A prospective cohort study of rectal cancer risk in relation to active cigarette smoking and passive smoke exposure. Ann. Epidemiol. 2008, 18, 28–35. [Google Scholar] [CrossRef] [PubMed]
- Alberg, A.J.; Kouzis, A.; Genkinger, J.M.; Gallicchio, L.; Burke, A.E.; Hoffman, S.C.; Diener-West, M.; Helzlsouer, K.J.; Comstock, G.W. A prospective cohort study of bladder cancer risk in relation to active cigarette smoking and household exposure to secondhand cigarette smoke. Am. J. Epidemiol. 2007, 165, 660–666. [Google Scholar] [CrossRef] [PubMed]
- Gallicchio, L.; Kowzis, A.; Genkinger, J.M.; Burke, A.E.; Hoffman, S.C.; Diener-West, M.; Helzlsouer, K.J.; Comstock, G.W.; Alberg, A.J. Active cigarette smoking, household passive smoke exposure, and the risk of developing pancreatic cancer. Prev. Med. 2006, 42, 200–205. [Google Scholar] [CrossRef] [PubMed]
- Trimble, C.L.; Genkinger, J.M.; Burke, A.E.; Hoffman, S.C.; Helzlsouer, K.J.; Diener-West, M.; Comstock, G.W.; Alberg, A.J. Active and passive cigarette smoking and the risk of cervical neoplasia. Obstet. Gynecol. 2005, 105, 174–181. [Google Scholar] [CrossRef] [PubMed]
- Stang, A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur. J. Epidemiol. 2010, 25, 603–605. [Google Scholar] [CrossRef] [PubMed]
- DerSimonian, R.; Laird, N. Meta-analysis in clinical trials. Control. Clin. Trials 1986, 7, 177–188. [Google Scholar] [CrossRef]
- Borenstein, M.; Hedges, L.V.; Higgins, J.P.T.; Rothstein, H.R. Introduction to Meta-Analysis; John Wiley & Sons, Ltd.: Chichester, UK, 2009. [Google Scholar]
- Macaskill, P.; Walter, S.D.; Irwig, L. A comparison of methods to detect publication bias in meta-analysis. Stat. Med. 2001, 20, 641–654. [Google Scholar] [CrossRef] [PubMed]
- Persaud, R. Misleading meta-analysis. “Fail safe N” is a useful mathematical measure of the stability of results. Br. Med. J. 1996, 312, 125. [Google Scholar] [CrossRef]
- Duval, S.; Tweedie, R. Trim and fill: A simple funnel-plot-based method of testing and adjusting for publication bias in meta-analysis. Biometrics 2000, 56, 455–463. [Google Scholar] [CrossRef] [PubMed]
- Dossus, L.; Boutron-Ruault, M.C.; Kaaks, R.; Gram, I.T.; Vilier, A.; Fervers, B.; Manjer, J.; Tjonneland, A.; Olsen, A.; Overvad, K.; et al. Active and passive cigarette smoking and breast cancer risk: Results from the epic cohort. Int. J. Cancer 2014, 134, 1871–1888. [Google Scholar] [CrossRef] [PubMed]
- Tang, L.Y.; Chen, L.J.; Qi, M.L.; Su, Y.; Su, F.X.; Lin, Y.; Wang, K.P.; Jia, W.H.; Zhuang, Z.X.; Ren, Z.F. Effects of passive smoking on breast cancer risk in pre/post-menopausal women as modified by polymorphisms of PARP1 and ESR1. Gene 2013, 524, 84–89. [Google Scholar] [CrossRef] [PubMed]
- Al-Zoughool, M.; Pintos, J.; Richardson, L.; Parent, M.E.; Ghadirian, P.; Krewski, D.; Siemiatycki, J. Exposure to environmental tobacco smoke (ETS) and risk of lung cancer in montreal: A case-control study. Environ. Health 2013, 12, 112. [Google Scholar] [CrossRef] [PubMed]
- Luo, J.; Margolis, K.L.; Wactawski-Wende, J.; Horn, K.; Messina, C.; Stefanick, M.L.; Tindle, H.A.; Tong, E.; Rohan, T.E. Association of active and passive smoking with risk of breast cancer among postmenopausal women: A prospective cohort study. Br. Med. J. 2011, 342, d1016. [Google Scholar] [CrossRef] [PubMed]
- Lu, Y.; Wang, S.S.; Reynolds, P.; Chang, E.T.; Ma, H.; Sullivan-Halley, J.; Clarke, C.A.; Bernstein, L. Cigarette smoking, passive smoking, and non-hodgkin lymphoma risk: Evidence from the california teachers study. Am. J. Epidemiol. 2011, 174, 563–573. [Google Scholar] [CrossRef] [PubMed]
- Chuang, S.C.; Gallo, V.; Michaud, D.; Overvad, K.; Tjønneland, A.; Clavel-Chapelon, F.; Romieu, I.; Straif, K.; Palli, D.; Pala, V.; et al. Exposure to environmental tobacco smoke in childhood and incidence of cancer in adulthood in never smokers in the european prospective investigation into cancer and nutrition. Cancer Causes Control 2011, 22, 487–494. [Google Scholar] [CrossRef] [PubMed]
- Yang, H.P.; Brinton, L.A.; Platz, E.A.; Lissowska, J.; Lacey, J.V., Jr.; Sherman, M.E.; Peplonska, B.; Garcia-Closas, M. Active and passive cigarette smoking and the risk of endometrial cancer in poland. Eur. J. Cancer 2010, 46, 690–696. [Google Scholar] [CrossRef] [PubMed]
- Heinen, M.M.; Verhage, B.A.; Goldbohm, R.A.; van den Brandt, P.A. Active and passive smoking and the risk of pancreatic cancer in the Netherlands cohort study. Cancer Epidemiol. Biomark. Prev. 2010, 19, 1612–1622. [Google Scholar] [CrossRef] [PubMed]
- Conlon, M.S.; Johnson, K.C.; Bewick, M.A.; Lafrenie, R.M.; Donner, A. Smoking (active and passive), N-acetyltransferase 2, and risk of breast cancer. Cancer Epidemiol. 2010, 34, 142–149. [Google Scholar] [CrossRef] [PubMed]
- Reynolds, P.; Goldberg, D.; Hurley, S.; Nelson, D.O.; Largent, J.; Henderson, K.D.; Bernstein, L. Passive smoking and risk of breast cancer in the California teachers study. Cancer Epidemiol. Biomark. Prev. 2009, 18, 3389–3398. [Google Scholar] [CrossRef] [PubMed]
- Pirie, K.; Beral, V.; Peto, R.; Roddam, A.; Reeves, G.; Green, J.; Million Women Study Collaborators. Passive smoking and breast cancer in never smokers: Prospective study and meta-analysis. Int. J. Epidemiol. 2008, 37, 1069–1079. [Google Scholar] [CrossRef] [PubMed]
- Hassan, M.M.; Spitz, M.R.; Thomas, M.B.; El-Deeb, A.S.; Glover, K.Y.; Nguyen, N.T.; Chan, W.; Kaseb, A.; Curley, S.A.; Vauthey, J.N.; et al. Effect of different types of smoking and synergism with hepatitis C virus on risk of hepatocellular carcinoma in American men and women: Case-control study. Int. J. Cancer 2008, 123, 1883–1891. [Google Scholar] [CrossRef] [PubMed]
- Asomaning, K.; Miller, D.P.; Liu, G.; Wain, J.C.; Lynch, T.J.; Su, L.; Christiani, D.C. Second hand smoke, age of exposure and lung cancer risk. Lung Cancer 2008, 61, 13–20. [Google Scholar] [CrossRef] [PubMed]
- Roddam, A.W.; Pirie, K.; Pike, M.C.; Chilvers, C.; Crossley, B.; Hermon, C.; McPherson, K.; Peto, J.; Vessey, M.; Beral, V. Active and passive smoking and the risk of breast cancer in women aged 36–45 years: A population based case-control study in the UK. Br. J. Cancer 2007, 97, 434–439. [Google Scholar] [CrossRef] [PubMed]
- Shrubsole, M.J.; Gao, Y.T.; Dai, Q.; Shu, X.O.; Ruan, Z.X.; Jin, F.; Zheng, W. Passive smoking and breast cancer risk among non-smoking Chinese women. Int. J. Cancer 2004, 110, 605–609. [Google Scholar] [CrossRef] [PubMed]
- Gammon, M.D.; Eng, S.M.; Teitelbaum, S.L.; Britton, J.A.; Kabat, G.C.; Hatch, M.; Paykin, A.B.; Neugut, A.I.; Santella, R.M. Environmental tobacco smoke and breast cancer incidence. Environ. Res. 2004, 96, 176–185. [Google Scholar] [CrossRef] [PubMed]
- Rachtan, J. Smoking, passive smoking and lung cancer cell types among women in Poland. Lung Cancer 2002, 35, 129–136. [Google Scholar] [CrossRef]
- Mao, Y.; Hu, J.; Semenciw, R.; White, K. Active and passive smoking and the risk of stomach cancer, by subsite, in Canada. Cancer Epidemiol. Biomark. Prev. 2002, 11, 27–38. [Google Scholar] [CrossRef]
- Kropp, S.; Chang-Claude, J. Active and passive smoking and risk of breast cancer by age 50 years among german women. Am. J. Epidemiol. 2002, 156, 616–626. [Google Scholar] [CrossRef] [PubMed]
- Chang-Claude, J.; Kropp, S.; Jager, B.; Bartsch, H.; Risch, A. Differential effect of NAT2 on the association between active and passive smoke exposure and breast cancer risk. Cancer Epidemiol. Biomark. Prev. 2002, 11, 698–704. [Google Scholar]
- Zhang, Z.F.; Morgenstern, H.; Spitz, M.R.; Tashkin, D.P.; Yu, G.P.; Hsu, T.C.; Schantz, S.P. Environmental tobacco smoking, mutagen sensitivity, and head and neck squamous cell carcinoma. Cancer Epidemiol. Biomark. Prev. 2000, 9, 1043–1049. [Google Scholar]
- Delfino, R.J.; Smith, C.; West, J.G.; Lin, H.J.; White, E.; Liao, S.Y.; Gim, J.S.; Ma, H.L.; Butler, J.; Anton-Culver, H. Breast cancer, passive and active cigarette smoking and N-acetyltransferase 2 genotype. Pharmacogenetics 2000, 10, 461–469. [Google Scholar] [CrossRef] [PubMed]
- Rapiti, E.; Jindal, S.K.; Gupta, D.; Boffetta, P. Passive smoking and lung cancer in Chandigarh, India. Lung Cancer 1999, 23, 183–189. [Google Scholar] [CrossRef]
- Morabia, A.; Bernstein, M.; Heritier, S.; Khatchatrian, N. Relation of breast cancer with passive and active exposure to tobacco smoke. Am. J. Epidemiol. 1996, 143, 918–928. [Google Scholar] [CrossRef] [PubMed]
- Smith, S.J.; Deacon, J.M.; Chilvers, C.E. Alcohol, smoking, passive smoking and caffeine in relation to breast cancer risk in young women. UK national case-control study group. Br. J. Cancer 1994, 70, 112–119. [Google Scholar] [CrossRef] [PubMed]
- Kreiger, N.; Marrett, L.D.; Dodds, L.; Hilditch, S.; Darlington, G.A. Risk factors for renal cell carcinoma: Results of a population-based case-control study. Cancer Causes Control 1993, 4, 101–110. [Google Scholar] [CrossRef] [PubMed]
- Brownson, R.C.; Alavanja, M.C.; Hock, E.T.; Loy, T.S. Passive smoking and lung cancer in nonsmoking women. Am. J. Public Health 1992, 82, 1525–1530. [Google Scholar] [CrossRef] [PubMed]
- Janerich, D.T.; Thompson, W.D.; Varela, L.R.; Greenwald, P.; Chorost, S.; Tucci, C.; Zaman, M.B.; Melamed, M.R.; Kiely, M.; McKneally, M.F. Lung cancer and exposure to tobacco smoke in the household. N. Engl. J. Med. 1990, 323, 632–636. [Google Scholar] [CrossRef] [PubMed]
- Burch, J.D.; Rohan, T.E.; Howe, G.R.; Risch, H.A.; Hill, G.B.; Steele, R.; Miller, A.B. Risk of bladder cancer by source and type of tobacco exposure: A case-control study. Int. J. Cancer 1989, 44, 622–628. [Google Scholar] [CrossRef] [PubMed]
- Lam, T.H.; Kung, I.T.; Wong, C.M.; Lam, W.K.; Kleevens, J.W.; Saw, D.; Hsu, C.; Seneviratne, S.; Lam, S.Y.; Lo, K.K.; et al. Smoking, passive smoking and histological types in lung cancer in Hong Kong Chinese women. Br. J. Cancer 1987, 56, 673–678. [Google Scholar] [CrossRef] [PubMed]
- Koo, L.C.; Ho, J.H.; Saw, D.; Ho, C.Y. Measurements of passive smoking and estimates of lung cancer risk among non-smoking Chinese females. Int. J. Cancer 1987, 39, 162–169. [Google Scholar] [CrossRef] [PubMed]
- Lee, P.N.; Chamberlain, J.; Alderson, M.R. Relationship of passive smoking to risk of lung cancer and other smoking-associated diseases. Br. J. Cancer 1986, 54, 97–105. [Google Scholar] [CrossRef] [PubMed]
- Hecht, S.S. Tobacco smoke carcinogens and lung cancer. J. Natl. Cancer Inst. 1999, 91, 1194–1210. [Google Scholar] [CrossRef] [PubMed]
- Nakano, K.; Vousden, K.H. Puma, a novel proapoptotic gene, is induced by p53. Mol. Cell 2001, 7, 683–694. [Google Scholar] [CrossRef]
- Chesebro, M.J. Passive smoking. Am. Fam. Phys. 1988, 37, 212–218. [Google Scholar]
- Mohtashamipur, E.; Mohtashamipur, A.; Germann, P.G.; Ernst, H.; Norpoth, K.; Mohr, U. Comparative carcinogenicity of cigarette mainstream and sidestream smoke condensates on the mouse skin. J. Cancer Res. Clin. Oncol. 1990, 116, 604–608. [Google Scholar] [CrossRef] [PubMed]
- Nelson, E. The miseries of passive smoking. Hum. Exp. Toxicol. 2001, 20, 61–83. [Google Scholar] [CrossRef] [PubMed]
- Lee, C.K.; Brown, B.G.; Reed, E.A.; Coggins, C.R.; Doolittle, D.J.; Hayes, A.W. Ninety-day inhalation study in rats, using aged and diluted sidestream smoke from a reference cigarette: DNA adducts and alveolar macrophage cytogenetics. Fundam. Appl. Toxicol. 1993, 20, 393–401. [Google Scholar] [CrossRef] [PubMed]
- Taylor, R.; Najafi, F.; Dobson, A. Meta-analysis of studies of passive smoking and lung cancer: Effects of study type and continent. Int. J. Epidemiol. 2007, 36, 1048–1059. [Google Scholar] [CrossRef] [PubMed]
- Park, S.; Jee, S.H.; Shin, H.R.; Park, E.H.; Shin, A.; Jung, K.W.; Hwang, S.S.; Cha, E.S.; Yun, Y.H.; Park, S.K.; et al. Attributable fraction of tobacco smoking on cancer using population-based nationwide cancer incidence and mortality data in Korea. BMC Cancer 2014, 14, 406. [Google Scholar] [CrossRef] [PubMed]
- Pisani, P.; Bray, F.; Parkin, D.M. Estimates of the world-wide prevalence of cancer for 25 sites in the adult population. Int. J. Cancer 2002, 97, 72–81. [Google Scholar] [CrossRef] [PubMed]
| Study | Country | Study Design | Number of Cases (Female %) | Number of Controls (Female %) | Cancer Type | Secondhand Smoking Exposure | Quality Assessment (Stars) |
|---|---|---|---|---|---|---|---|
| Dossus L. (2014) [29] | Europe | Prospective Cohort | 78,217 (100) | 26,072 (100) | Breast cancer | Lifetime * | 8 |
| Tang L.Y. (2013) [30] | China | Case-control | 765 (100) | 818 (100) | Breast cancer | Adulthood * | 6 |
| Al-Zoughool M. (2013) [31] | Canada | Case-control | 44 (70.45) | 436 (70.64) | Lung cancer | Childhood, Adulthood, Lifetime * | 7 |
| Luo J. (2011) [32] | USA | Prospective Cohort | 1692 (100) | 39,330 (100) | Breast cancer | Childhood, Adulthood, Lifetime * | 8 |
| Lu Y. (2011) [33] | USA | Prospective Cohort | 56,015 (100) | 22,991 (100) | Non-Hodgkin lymphoma | Childhood, Adulthood, Lifetime * | 8 |
| Chuang S.C. (2011) [34] | Europe | Prospective Cohort | 72,091 (86.8) | 33,887 (86.7) | All cancer | Childhood * | 8 |
| Yang H.P. (2010) [35] | Poland | Case-control | 358 (100) | 898 (100) | Endometrial cancer | Lifetime * | 7 |
| Heinen M.M. (2010) [36] | Netherland | Prospective Cohort | 1029 (94.5) | 310 (58.7) | Pancreatic cancer | Adulthood *,‡ | 8 |
| Conlon M.S. (2010) [37] | Canada | Case-control | 347 (100) | 775 (100) | Breast cancer | Lifetime * | 7 |
| Reynolds P. (2009) [38] | USA | Prospective Cohort | 49,468 (100) | 7070 (100) | Breast cancer | Childhood, Adulthood, Lifetime * | 8 |
| Pirie K. (2008) [39] | UK | Prospective Cohort | 174,819 (100) | 35,828 (100) | Breast cancer | Adulthood, Lifetime * | 6 |
| Kurahashi N. (2008) [17] | Japan | Prospective Cohort | 21,083 (100) | 7331 (100) | Lung cancer | Adulthood * | 8 |
| Hooker C.M. (2008) [19] | USA | Prospective Cohort (1963) | 7117 (86.9) | 11,722 (72.9) | Rectal cancer | Adulthood * | 7 |
| USA | Prospective Cohort (1975) | 4929 (82.5) | 15,245 (71.5) | ||||
| Hassan M.M. (2008) [40] | USA | Case-control | 88 (53.4) | 471 (52.4) | Hepatocellular carcinoma | Childhood, Adulthood, Lifetime * | 7 |
| Asomaning K. (2008) [41] | USA | Case-control | 138 (59) | 466 (62) | Lung cancer | Lifetime *,‡ | 6 |
| Roddam A.W. (2007) [42] | UK | Case-control | 297 (100) | 310 (100) | Breast cancer | Lifetime * | 8 |
| Alberg A.J. (2007) [20] | USA | Prospective Cohort (1963) | 7117 (NA) | 11,722 (NA) | Bladder cancer | Adulthood * | 7 |
| USA | Prospective Cohort (1975) | 4932 (NA) | 15,249 (NA) | ||||
| Gallicchio L. (2006) [21] | USA | Prospective Cohort (1963) | 7117 (86.9) | 11,722 (72.9) | Pancreatic cancer | Adulthood * | 7 |
| USA | Prospective Cohort (1975) | 4932 (82.5) | 15,249 (71.5) | ||||
| Trimble C.L. (2005) [22] | USA | Prospective Cohort (1963) | 6184 (100) | 8538 (100) | Cervical cancer | Adulthood * | 7 |
| USA | Prospective Cohort (1975) | 4071 (100) | 10,907 (100) | ||||
| Hanaoka T. (2005) [18] | Japan | Prospective Cohort | 14,533 (100) | 5660 (100) | Breast cancer | Lifetime * | 8 |
| Shrubsole M.J. (2004) [43] | China | Case-control | 1013 (100) | 1117 (100) | Breast cancer | Adulthood * | 8 |
| Gammon M.D. (2004) [44] | USA | Case-control | 598 (100) | 627 (100) | Breast cancer | Lifetime * | 6 |
| Rachtan J. (2002) [45] | Poland | Case-control | 54 (100) | 251 (100) | Lung cancer | Childhood * | 8 |
| Mao Y. (2002) [46] | Canada | Case-control | 132 (0) | 343 (0) | Gastric cancer | Lifetime * | 7 |
| Kropp S. (2002) [47] | German | Case-control | 197 (100) | 454 (100) | Breast cancer | Childhood, Adulthood, Lifetime * | 7 |
| Chang-Claude J. (2002) [48] | German | Case-control | 174 (100) | 365 (100) | Breast cancer | Childhood, Adulthood, Lifetime * | 7 |
| Johnson K.C. (2001) [11] | Canada | Case-control | 71 (100) | 761 (100) | Lung cancer | Childhood, Adulthood, Lifetime * | 6 |
| Zhang Z.F. (2000) [49] | USA | Case-control | 26 (NA) | 59 (NA) | Head and neck cancer | Lifetime * | 6 |
| Lee C.H. (2000) [10] | Taiwan | Case-control | 268 (100) | 445 (100) | Lung cancer | Lifetime *,† | 7 |
| Delfino R.J. (2000) [50] | USA | Case-control | 64 (100) | 147 (100) | Breast cancer | Adulthood * | 5 |
| Rapiti E. (1999) [51] | India | Case-control | 58 (70.7) | 123 (54.5) | Lung cancer | Childhood, Adulthood * | 4 |
| Morabia A. (1996) [52] | Switzerland | Case-control | 126 (100) | 620 (100) | Breast cancer | Adulthood | 8 |
| Smith S.J. (1994) [53] | UK | Case-control | 204 (100) | 199 (100) | Breast cancer | Childhood, Adulthood, Lifetime * | 7 |
| Kreiger N. (1993) [54] | Canada | Case-control | 119 (60.5) | 524 (65.8) | Renal cell carcinoma | Adulthood * | 7 |
| Brownson R.C. (1992) [55] | USA | Case-control | 431 (100) | 1166 (100) | Lung cancer | Childhood, Adulthood * | 5 |
| Janerich D.T. (1990) [56] | USA | Case-control | 191 (NA) | 191 (NA) | Lung cancer | Childhood, Adulthood, Lifetime * | 7 |
| Burch J.D. (1989) [57] | Canada | Case-control | 142 (57.0) | 217 (48.4) | Bladder cancer | Adulthood *,‡ | 7 |
| Lam T.H. (1987) [58] | Hong Kong | Case-control | 199 (100) | 335 (100) | Lung cancer | Adulthood * | 7 |
| Koo L.C. (1987) [59] | Hong Kong | Case-control | 88 (100) | 137 (100) | Lung cancer | Childhood, Adulthood, Lifetime * | 7 |
| Lee P.N. (1986) [60] | UK | Case-control | 47 (68.0) | 96 (68.8) | Lung cancer | Adulthood * | 5 |
| Variable | Studies | Estimated Effect Size (HR or OR) | 95% CI | p-value | I2 Value, % |
|---|---|---|---|---|---|
| Sex | |||||
| Female only | 29 studies [15,16,17,20,27,28,30,31,32,33,34,35,36,37,40,41,42,43,45,47,49,50,52,53,54,55,57,58,59] | 1.25 | 1.14–1.37 | <0.001 | 56.14 |
| Male only | 4 studies [17,44,54,57] | 1.59 | 0.91–2.79 | 0.100 | 44.27 |
| Cancer type | |||||
| Breast cancer | 15 studies [16,27,28,30,35,36,37,40,41,42,45,46,50,52,53] | 1.24 | 1.10–1.39 | <0.001 | 73.90 |
| Lung cancer | 12 studies [15,29,39,43,47,49,51,55,56,58,59,60] | 1.25 | 1.03–1.51 | 0.026 | 48.20 |
| Bladder cancer | 2 studies [18,57] | 0.89 | 0.63–1.25 | 0.492 | 0.00 |
| Pancreatic cancer | 2 studies [19,34] | 0.83 | 0.59–1.17 | 0.291 | 0.00 |
| Cervical cancer | 1 study [20] | 2.18 | 1.15–4.16 | 0.018 | 70.54 |
| Endometrial cancer | 1 study [33] | 0.83 | 0.62–1.11 | 0.205 | 0.00 |
| Gastric cancer | 1 study [44] | 0.93 | 0.58–1.49 | 0.756 | 0.00 |
| Hepatic cancer | 1 study [38] | 0.49 | 0.31–0.79 | 0.003 | 0.00 |
| Rectal cancer | 1 study [17] | 1.01 | 0.70–1.46 | 0.949 | 0.00 |
| Renal cancer | 1 study [54] | 0.90 | 0.60–1.34 | 0.593 | 0.00 |
| Head and neck cancer | 1 study [48] | 2.17 | 0.56–8.37 | 0.262 | 0.00 |
| Lymphoma | 1 study [31] | 1.34 | 1.06–1.71 | 0.017 | 0.00 |
| All cancer | 1 study [32] | 0.90 | 0.86–0.94 | <0.001 | 0.00 |
| Methodological quality | |||||
| High quality | 26 studies [15,16,27,29,30,31,32,33,34,35,36,38,40,41,43,44,45,46,49,52,53,54,56,57,58,59] | 1.15 | 1.02–1.30 | 0.023 | 84.00 |
| Low quality | 14 studies [17,18,19,20,28,37,39,42,47,48,50,51,55,60] | 1.19 | 1.02–1.39 | 0.031 | 59.81 |
| Country | |||||
| Western | 32 studies [17,18,19,20,27,29,30,31,32,33,34,35,36,37,38,39,40,42,43,44,45,46,47,48,50,52,53,54,55,56,57,60] | 1.13 | 1.01–1.25 | 0.026 | 79.20 |
| Asian | 8 studies [15,16,28,41,49,51,58,59] | 1.33 | 1.10–1.61 | 0.003 | 57.24 |
| Period of exposure to secondhand smoking | |||||
| Childhood | 15 studies [28,30,31,32,36,38,43,45,46,47,51,53,55,56,59] | 1.00 | 0.81–1.23 | 0.998 | 83.93 |
| Adulthood | 28 studies [15,17,18,19,20,28,29,30,31,34,36,37,38,41,45,46,47,50,51,52,53,54,55,56,57,58,59,60] | 1.03 | 0.77–1.39 | 0.840 | 95.90 |
| Lifetime | 22 studies [16,27,29,30,31,33,35,36,37,38,39,40,42,44,45,46,47,48,49,53,56,59] | 1.14 | 1.02–1.27 | 0.023 | 70.89 |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, A.-S.; Ko, H.-J.; Kwon, J.-H.; Lee, J.-M. Exposure to Secondhand Smoke and Risk of Cancer in Never Smokers: A Meta-Analysis of Epidemiologic Studies. Int. J. Environ. Res. Public Health 2018, 15, 1981. https://doi.org/10.3390/ijerph15091981
Kim A-S, Ko H-J, Kwon J-H, Lee J-M. Exposure to Secondhand Smoke and Risk of Cancer in Never Smokers: A Meta-Analysis of Epidemiologic Studies. International Journal of Environmental Research and Public Health. 2018; 15(9):1981. https://doi.org/10.3390/ijerph15091981
Chicago/Turabian StyleKim, A-Sol, Hae-Jin Ko, Jin-Hyun Kwon, and Jong-Myung Lee. 2018. "Exposure to Secondhand Smoke and Risk of Cancer in Never Smokers: A Meta-Analysis of Epidemiologic Studies" International Journal of Environmental Research and Public Health 15, no. 9: 1981. https://doi.org/10.3390/ijerph15091981
APA StyleKim, A.-S., Ko, H.-J., Kwon, J.-H., & Lee, J.-M. (2018). Exposure to Secondhand Smoke and Risk of Cancer in Never Smokers: A Meta-Analysis of Epidemiologic Studies. International Journal of Environmental Research and Public Health, 15(9), 1981. https://doi.org/10.3390/ijerph15091981





