Rural Versus Urban Patients: Benchmarking the Outcomes of Patients with Acute Myocardial Infarction in Shanxi, China from 2013 to 2017
Abstract
1. Introduction
2. Methods
2.1. Data Source
2.2. Study Population
2.3. Variables of Interest
2.4. Patient and Hospital Level Covariates
2.5. Statistical Models
3. Results
3.1. Patient Characteristics
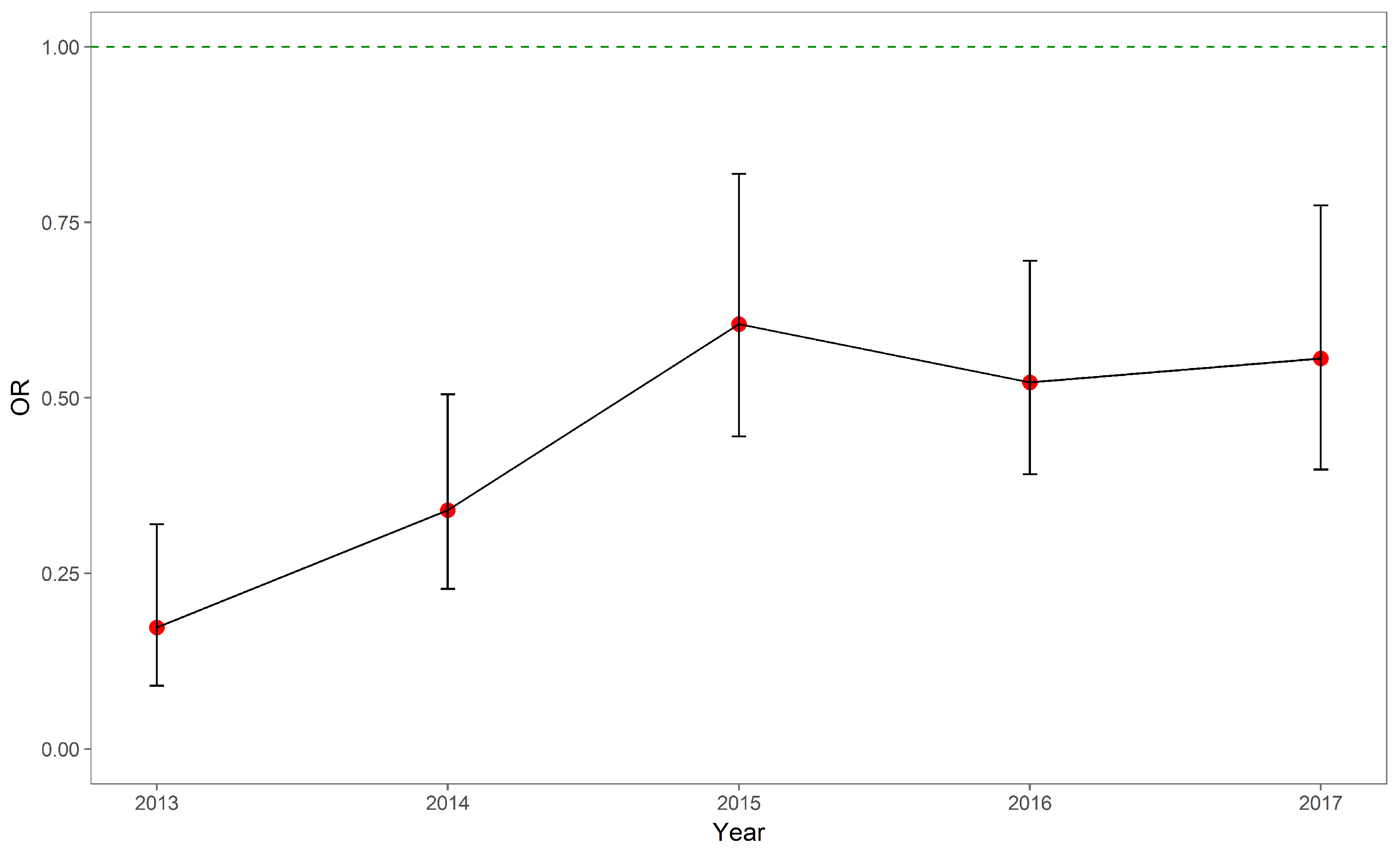
3.2. In-Hospital Mortality
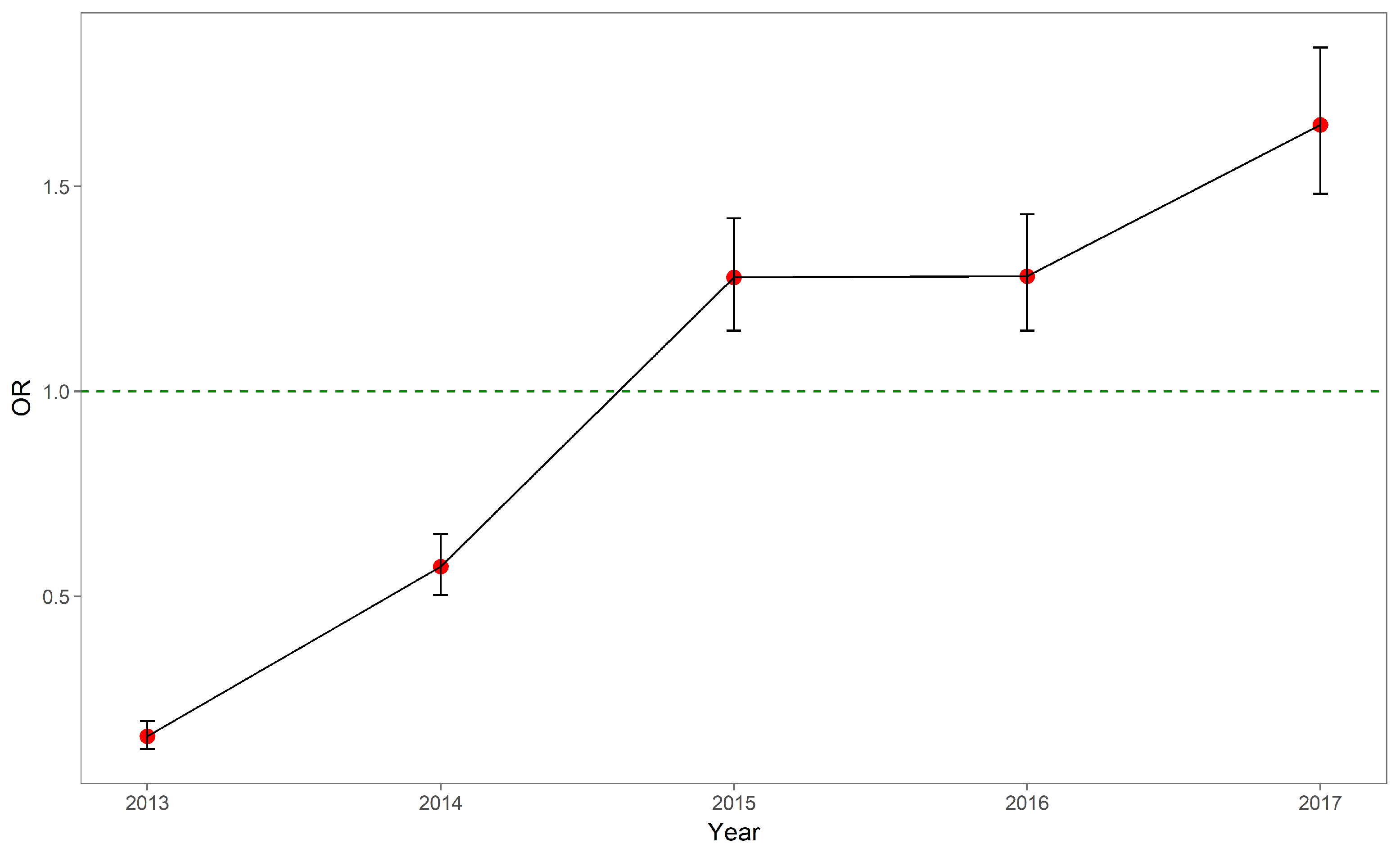
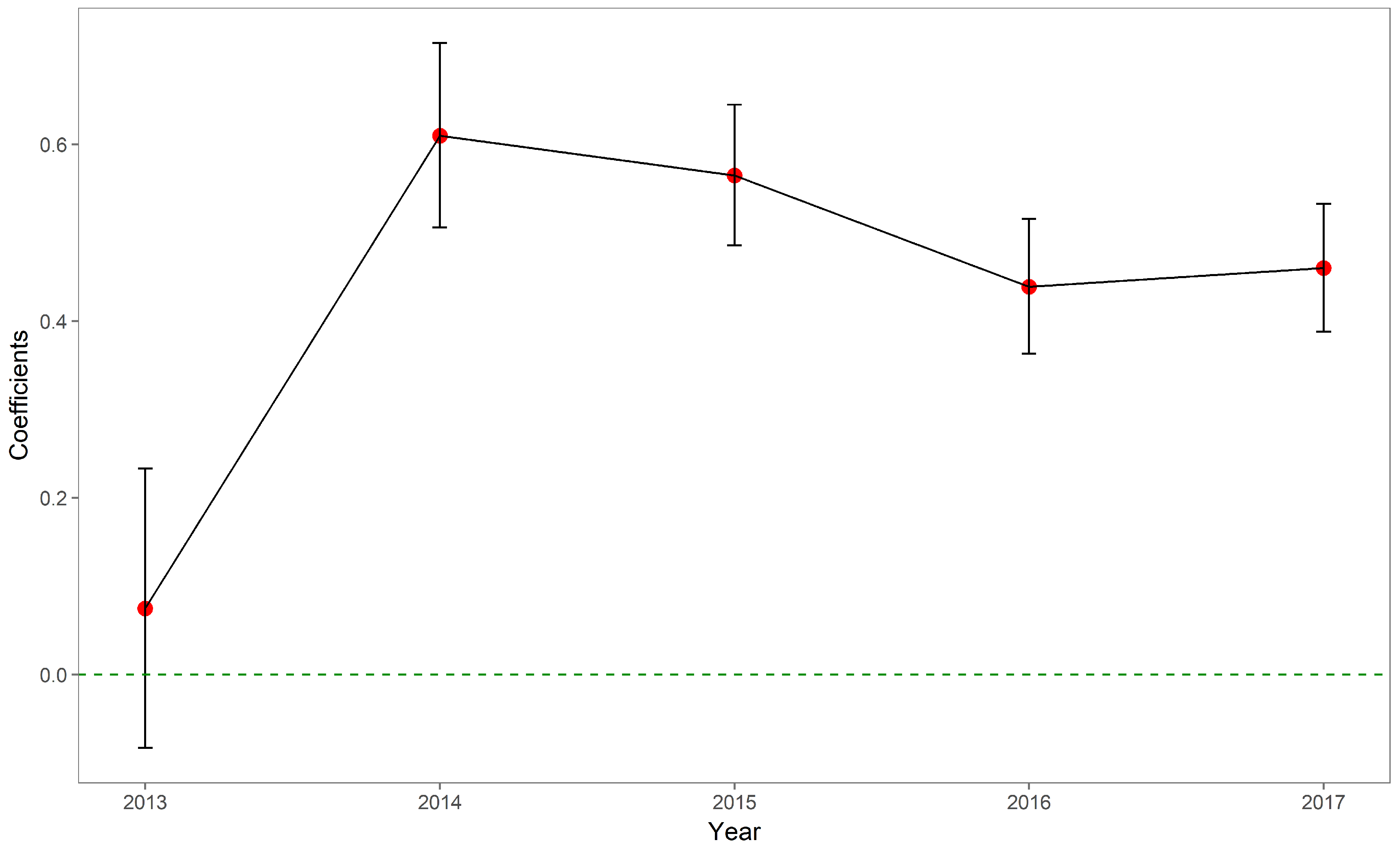
3.3. OOP Expenses
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Abbreviations
| AMI | Acute Myocardial Infarction |
| EMR | Electronic Medical Records |
| ICD-9 | The International Classification of Disease, Ninth Revision |
| ICD-10 | The International Classification of Disease, Tenth Revision |
| NCMS | New Cooperative Medical Scheme |
| OR | Odds Ratio |
| OOP | Out-of-pocket |
| PCI | Percutaneous Coronary Intervention |
| URBMI | Urban Resident-based Basic Medical Insurance Scheme |
| UEBMI | Urban Employee-based Basic Medical Insurance Scheme |
References
- Pong, R.W.; DesMeules, M.; Lagacé, C. Rural–urban disparities in health: How does Canada fare and how does Canada compare with Australia? Aust. J. Rural Health 2009, 17, 58–64. [Google Scholar] [CrossRef] [PubMed]
- Riva, M.; Curtis, S.; Gauvin, L.; Fagg, J. Unravelling the extent of inequalities in health across urban and rural areas: Evidence from a national sample in England. Soc. Sci. Med. 2009, 68, 654–663. [Google Scholar] [CrossRef] [PubMed]
- Srinivasan, C.S.; Zanello, G.; Shankar, B. Rural-urban disparities in child nutrition in Bangladesh and Nepal. BMC Public Health 2013, 13, 581. [Google Scholar] [CrossRef] [PubMed]
- Nennecke, A.; Geiss, K.; Hentschel, S.; Vettorazzi, E.; Jansen, L.; Eberle, A.; Holleczek, B.; Gondos, A.; Brenner, H.; GEKID cancer survival working group. Survival of cancer patients in urban and rural areas of Germany—A comparison. Cancer Epidemiol. 2014, 38, 259–265. [Google Scholar] [CrossRef] [PubMed]
- Singh, G.K.; Siahpush, M. Widening rural–urban disparities in life expectancy, US, 1969–2009. Am. J. Prev. Med. 2014, 46, e19–e29. [Google Scholar] [CrossRef] [PubMed]
- Sonnappa, S.; Lum, S.; Kirkby, J.; Bonner, R.; Wade, A.; Subramanya, V.; Lakshman, P.T.; Rajan, B.; Nooyi, S.C.; Stocks, J. Disparities in pulmonary function in healthy children across the Indian urban–rural continuum. Am. J. Respir. Crit. Care Med. 2015, 191, 79–86. [Google Scholar] [CrossRef] [PubMed]
- Choi, K.M. Investigation of cancer mortality inequalities between rural and urban areas in South Korea. Aust. J. Rural Health 2016, 24, 61–66. [Google Scholar] [CrossRef] [PubMed]
- Amoah, P.A.; Edusei, J.; Amuzu, D. Social Networks and Health: Understanding the Nuances of Healthcare Access between Urban and Rural Populations. Int. J. Environ. Res. Public Health 2018, 15, 973. [Google Scholar] [CrossRef] [PubMed]
- The World Bank Group. Rural Population (% of Total Population) 1960–2017. 2018. Available online: https://data.worldbank.org/indicator/SP.RUR.TOTL.ZS (accessed on 30 August 2018).
- Hartley, D. Rural health disparities, population health, and rural culture. Am. J. Public Health 2004, 94, 1675–1678. [Google Scholar] [CrossRef] [PubMed]
- Kulshreshtha, A.; Goyal, A.; Dabhadkar, K.; Veledar, E.; Vaccarino, V. Urban-rural differences in coronary heart disease mortality in the United States: 1999–2009. Public Health Rep. 2014, 129, 19–29. [Google Scholar] [CrossRef] [PubMed]
- Fang, H.; Chen, J.; Rizzo, J.A. Explaining urban-rural health disparities in China. Med. Care 2009, 47, 1209–1216. [Google Scholar] [CrossRef] [PubMed]
- Jian, W.; Chan, K.Y.; Reidpath, D.D.; Xu, L. China’s rural-urban care gap shrank for chronic disease patients, but inequities persist. Health Aff. 2010, 29, 2189–2196. [Google Scholar] [CrossRef] [PubMed]
- Gong, P.; Liang, S.; Carlton, E.J.; Jiang, Q.; Wu, J.; Wang, L.; Remais, J.V. Urbanisation and health in China. Lancet 2012, 379, 843–852. [Google Scholar] [CrossRef]
- National Bureau of Statistics of China. Tabulation on the 2010 Population Census of the People’s Republic of China. 2010. Available online: http://www.stats.gov.cn/tjsj/pcsj/rkpc/6rp/indexch.htm (accessed on 30 August 2018).
- Liu, M.; Zhang, Q.; Lu, M.; Kwon, C.S.; Quan, H. Rural and urban disparity in health services utilization in China. Med. Care 2007, 45, 767–774. [Google Scholar] [CrossRef] [PubMed]
- Anand, S.; Fan, V.Y.; Zhang, J.; Zhang, L.; Ke, Y.; Dong, Z.; Chen, L.C. China’s human resources for health: quantity, quality, and distribution. Lancet 2008, 372, 1774–1781. [Google Scholar] [CrossRef]
- Yip, W.C.M.; Hsiao, W.C.; Chen, W.; Hu, S.; Ma, J.; Maynard, A. Early appraisal of China’s huge and complex health-care reforms. Lancet 2012, 379, 833–842. [Google Scholar] [CrossRef]
- Yip, W.; Hsiao, W. Harnessing the privatisation of China’s fragmented health-care delivery. Lancet 2014, 384, 805–818. [Google Scholar] [CrossRef]
- Yao, Q.; Liu, C.; Ferrier, J.A.; Liu, Z.; Sun, J. Urban-rural inequality regarding drug prescriptions in primary care facilities—A pre-post comparison of the National Essential Medicines Scheme of China. Int. J. Equity Health 2015, 14, 58. [Google Scholar] [CrossRef] [PubMed]
- Ge, D.; Chu, J.; Zhou, C.; Qian, Y.; Zhang, L.; Sun, L. Rural–urban difference in the use of annual physical examination among seniors in Shandong, China: A cross-sectional study. Int. J. Equity Health 2017, 16, 86. [Google Scholar] [CrossRef] [PubMed]
- Bragg, F.; Holmes, M.V.; Iona, A.; Guo, Y.; Du, H.; Chen, Y.; Bian, Z.; Yang, L.; Herrington, W.; Bennett, D.; et al. Association between diabetes and cause-specific mortality in rural and urban areas of China. JAMA 2017, 317, 280–289. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.H.; Guan, T.; Mao, J.; Liu, L. Disparity and its time trends in stroke mortality between urban and rural populations in China 1987 to 2001: Changing patterns and their implications for public health policy. Stroke 2007, 38, 3139–3144. [Google Scholar] [CrossRef] [PubMed]
- Fu, R.; Wang, Y.; Bao, H.; Wang, Z.; Li, Y.; Su, S.; Liu, M. Trend of urban-rural disparities in hospital admissions and medical expenditure in China from 2003 to 2011. PLoS ONE 2014, 9, e108571. [Google Scholar] [CrossRef] [PubMed]
- Hu, Z.; Yuan, X.; Rao, K.; Zheng, Z.; Hu, S. National trend in congenital heart disease mortality in China during 2003 to 2010: A population-based study. J. Thorac. Cardiovasc. Surg. 2014, 148, 596–602. [Google Scholar] [CrossRef] [PubMed]
- Sun, W.; Zhou, Y.; Zhang, Z.; Cao, L.; Chen, W. The Trends in Cardiovascular Diseases and Respiratory Diseases Mortality in Urban and Rural China, 1990–2015. Int. J. Environ. Res. Public Health 2017, 14, 1391. [Google Scholar] [CrossRef] [PubMed]
- Chung, S.C.; Sundström, J.; Gale, C.P.; James, S.; Deanfield, J.; Wallentin, L.; Timmis, A.; Jernberg, T.; Hemingway, H. Comparison of hospital variation in acute myocardial infarction care and outcome between Sweden and United Kingdom: Population based cohort study using nationwide clinical registries. BMJ 2015, 351, h3913. [Google Scholar] [CrossRef] [PubMed]
- Kessler, D.P.; McClellan, M.B. Is hospital competition socially wasteful? Q. J. Econ. 2000, 115, 577–615. [Google Scholar] [CrossRef]
- Gaynor, M.; Moreno-Serra, R.; Propper, C. Death by market power: Reform, competition, and patient outcomes in the National Health Service. Am. Econ. J. Econ. Policy 2013, 5, 134–166. [Google Scholar] [CrossRef]
- Moore, B.J.; White, S.; Washington, R.; Coenen, N.; Elixhauser, A. Identifying increased risk of readmission and in-hospital mortality using hospital administrative data. Med. Care 2017, 55, 698–705. [Google Scholar] [CrossRef] [PubMed]
- Deb, P.; Norton, E.C. Modeling Health Care Expenditures and Use. Annu. Rev. Public Health 2018, 39, 489–505. [Google Scholar] [CrossRef] [PubMed]
- R Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2013. [Google Scholar]
- Abubakar, I.; Tillmann, T.; Banerjee, A. Global, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990–2013: A systematic analysis for the Global Burden of Disease Study 2013. Lancet 2015, 385, 117–171. [Google Scholar]
- Chen, H.; Shi, L.; Xue, M.; Wang, N.; Dong, X.; Cai, Y.; Chen, J.; Zhu, W.; Xu, H.; Meng, Q. Geographic Variations in In-Hospital Mortality and Use of Percutaneous Coronary Intervention Following Acute Myocardial Infarction in China: A Nationwide Cross-Sectional Analysis. J. Am. Heart Assoc. 2018, 7, e008131. [Google Scholar] [CrossRef]
- Zhang, Y.X.; Zhou, J.Y.; Zhao, J.S.; Chu, Z.H. Urban–rural and regional disparities in the prevalence of elevated blood pressure among children and adolescents in Shandong, China. Int. J. Cardiol. 2014, 176, 1053–1055. [Google Scholar] [CrossRef] [PubMed]
- Pingali, P. Westernization of Asian diets and the transformation of food systems: Implications for research and policy. Food Policy 2007, 32, 281–298. [Google Scholar] [CrossRef]
- Lee, Y.H.; Shelley, M.; Liu, C.T.; Chang, Y.C. Assessing the association of food preferences and self-reported psychological well-being among middle-aged and older adults in contemporary China-results from the China Health and Nutrition Survey. Int. J. Environ. Res. Public Health 2018, 15, 463. [Google Scholar] [CrossRef] [PubMed]
- Garg, C.C.; Karan, A.K. Reducing out-of-pocket expenditures to reduce poverty: A disaggregated analysis at rural-urban and state level in India. Health Policy Plan. 2008, 24, 116–128. [Google Scholar] [CrossRef] [PubMed]
- Kruk, M.E.; Mbaruku, G.; Rockers, P.C.; Galea, S. User fee exemptions are not enough: Out-of-pocket payments for ‘free’delivery services in rural Tanzania. Trop. Med. Int. Health 2008, 13, 1442–1451. [Google Scholar] [CrossRef] [PubMed]
- Lin, X.; Cai, M.; Tao, H.; Liu, E.; Cheng, Z.; Xu, C.; Wang, M.; Xia, S.; Jiang, T. Insurance status, inhospital mortality and length of stay in hospitalised patients in Shanxi, China: A cross-sectional study. BMJ Open 2017, 7, e015884. [Google Scholar] [CrossRef] [PubMed]
- Meng, Q.; Fang, H.; Liu, X.; Yuan, B.; Xu, J. Consolidating the social health insurance schemes in China: Towards an equitable and efficient health system. Lancet 2015, 386, 1484–1492. [Google Scholar] [CrossRef]
- Wang, H.Q.; Liu, Z.H.; Zhang, Y.Z.; Luo, Z.J. Integration of current identity-based district-varied health insurance schemes in China: Implications and challenges. Front. Med. 2012, 6, 79–84. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Zheng, A.; He, X.; Jiang, H. Integration of rural and urban healthcare insurance schemes in China: An empirical research. BMC Health Serv. Res. 2014, 14, 142. [Google Scholar] [CrossRef] [PubMed]
- Cai, M.; Liu, E.; Tao, H.; Qian, Z.; Lin, X.; Cheng, Z. Does Level of Hospital Matter? A Study of Mortality of Acute Myocardial Infarction Patients in Shanxi, China. Am. J. Med. Qual. 2018, 33, 185–192. [Google Scholar] [CrossRef] [PubMed]
- Xu, Y.; Liu, Y.; Shu, T.; Yang, W.; Liang, M. Variations in the quality of care at large public hospitals in Beijing, China: A condition-based outcome approach. PLoS ONE 2015, 10, e0138948. [Google Scholar] [CrossRef] [PubMed]
- Wu, H.; Liu, L.; Wang, Y.; Gao, F.; Zhao, X.; Wang, L. Factors associated with burnout among Chinese hospital doctors: A cross-sectional study. BMC Public Health 2013, 13, 786. [Google Scholar] [CrossRef] [PubMed]
- Menees, D.S.; Peterson, E.D.; Wang, Y.; Curtis, J.P.; Messenger, J.C.; Rumsfeld, J.S.; Gurm, H.S. Door-to-balloon time and mortality among patients undergoing primary PCI. N. Engl. J. Med. 2013, 369, 901–909. [Google Scholar] [CrossRef] [PubMed]
| 2013 | 2014 | 2015 | 2016 | 2017 | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Urban/Rural | Urban | Rural | Urban | Rural | Urban | Rural | Urban | Rural | Urban | Rural |
| n (%) | 2243 (54.7) | 1854 (45.3) | 7073 (50.4) | 6966 (49.6) | 9092 (41.4) | 12,882 (58.6) | 10,349 (41.7) | 14,458 (58.3) | 9233 (41.4) | 13,069 (58.6) |
| Death | 0.03 (0.18) | 0.01 (0.10) | 0.03 (0.17) | 0.01 (0.12) | 0.03 (0.17) | 0.01 (0.12) | 0.03 (0.18) | 0.01 (0.12) | 0.03 (0.17) | 0.01 (0.12) |
| Out-of-pocket expenses | ||||||||||
| % of 0 values | 68.9 | 86.7 | 72.4 | 76.4 | 71.8 | 76.1 | 76.2 | 80.1 | 71.8 | 75.3 |
| median | 12,331 | 10,953 | 12,591 | 22,714 | 12,701 | 17,602 | 11,939 | 13,694 | 12,582 | 15,664 |
| 1st quartile | 4652 | 6168 | 4796 | 9260 | 4677 | 8216 | 4911 | 7749 | 5542 | 8015 |
| 3rd quartile | 24,837 | 33,465 | 22,864 | 45,539 | 25,065 | 42,488 | 22,304 | 35,545 | 24,338 | 37,474 |
| Female | 0.22 (0.42) | 0.29 (0.45) | 0.22 (0.41) | 0.29 (0.45) | 0.22 (0.41) | 0.31 (0.46) | 0.21 (0.41) | 0.30 (0.46) | 0.21 (0.41) | 0.30 (0.46) |
| Age (%) | ||||||||||
| 18–45 | 226 (10.1) | 246 (13.3) | 651 (9.2) | 892 (12.8) | 831 (9.1) | 1392 (10.8) | 910 (8.8) | 1476 (10.2) | 711 (7.7) | 1252 (9.6) |
| 46–65 | 993 (44.3) | 981 (52.9) | 3205 (45.3) | 3836 (55.1) | 4145 (45.6) | 6552 (50.9) | 4632 (44.8) | 7390 (51.1) | 4143 (44.9) | 6755 (51.7) |
| 66–75 | 559 (24.9) | 386 (20.8) | 1592 (22.5) | 1457 (20.9) | 2021 (22.2) | 3033 (23.5) | 2248 (21.7) | 3402 (23.5) | 2069 (22.4) | 3190 (24.4) |
| 75+ | 465 (20.7) | 241 (13.0) | 1625 (23.0) | 781 (11.2) | 2095 (23.0) | 1905 (14.8) | 2559 (24.7) | 2190 (15.1) | 2310 (25.0) | 1872 (14.3) |
| Marriage (%) | ||||||||||
| Married | 2101 (93.7) | 1680 (90.6) | 6578 (93.0) | 6439 (92.4) | 8355 (91.9) | 11,853 (92.0) | 9525 (92.0) | 13,343 (92.3) | 8330 (90.2) | 11,932 (91.3) |
| Unmarried | 26 (1.2) | 79 (4.3) | 94 (1.3) | 213 (3.1) | 94 (1.0) | 216 (1.7) | 97 (0.9) | 253 (1.7) | 223 (2.4) | 360 (2.8) |
| Widowed | 60 (2.7) | 51 (2.8) | 194 (2.7) | 156 (2.2) | 372 (4.1) | 471 (3.7) | 401 (3.9) | 496 (3.4) | 373 (4.0) | 431 (3.3) |
| Divorced | 48 (2.1) | 23 (1.2) | 167 (2.4) | 112 (1.6) | 159 (1.7) | 145 (1.1) | 173 (1.7) | 155 (1.1) | 176 (1.9) | 140 (1.1) |
| Other | 8 (0.4) | 21 (1.1) | 40 (0.6) | 46 (0.7) | 112 (1.2) | 197 (1.5) | 153 (1.5) | 211 (1.5) | 131 (1.4) | 206 (1.6) |
| Occupation (%) | ||||||||||
| Public institution | 194 (8.6) | 33 (1.8) | 902 (12.8) | 127 (1.8) | 1273 (14.0) | 145 (1.1) | 1421 (13.7) | 157 (1.1) | 1258 (13.6) | 105 (0.8) |
| Private institution | 617 (27.5) | 97 (5.2) | 1989 (28.1) | 346 (5.0) | 2041 (22.4) | 386 (3.0) | 2321 (22.4) | 462 (3.2) | 1998 (21.6) | 448 (3.4) |
| Farmer | 370 (16.5) | 1249 (67.4) | 385 (5.4) | 5553 (79.7) | 634 (7.0) | 10,526 (81.7) | 680 (6.6) | 12,158 (84.1) | 621 (6.7) | 10,928 (83.6) |
| Jobless | 110 (4.9) | 47 (2.5) | 383 (5.4) | 223 (3.2) | 560 (6.2) | 236 (1.8) | 640 (6.2) | 294 (2.0) | 563 (6.1) | 268 (2.1) |
| Retired | 601 (26.8) | 90 (4.9) | 2581 (36.5) | 292 (4.2) | 3437 (37.8) | 350 (2.7) | 4203 (40.6) | 412 (2.8) | 3872 (41.9) | 286 (2.2) |
| Other | 351 (15.6) | 338 (18.2) | 833 (11.8) | 425 (6.1) | 1147 (12.6) | 1239 (9.6) | 1084 (10.5) | 975 (6.7) | 921 (10.0) | 1034 (7.9) |
| Length of stay (%) | ||||||||||
| 1st quartile | 432 (19.3) | 484 (26.1) | 1380 (19.5) | 1768 (25.4) | 2082 (22.9) | 3882 (30.1) | 2519 (24.3) | 4470 (30.9) | 2370 (25.7) | 4458 (34.1) |
| 2nd quartile | 536 (23.9) | 521 (28.1) | 1807 (25.5) | 2018 (29.0) | 2467 (27.1) | 3665 (28.5) | 3076 (29.7) | 4534 (31.4) | 3007 (32.6) | 4340 (33.2) |
| 3rd quartile | 525 (23.4) | 406 (21.9) | 1650 (23.3) | 1544 (22.2) | 2074 (22.8) | 2885 (22.4) | 2180 (21.1) | 3037 (21.0) | 1899 (20.6) | 2454 (18.8) |
| 4th quartile | 750 (33.4) | 443 (23.9) | 2236 (31.6) | 1636 (23.5) | 2469 (27.2) | 2450 (19.0) | 2574 (24.9) | 2417 (16.7) | 1957 (21.2) | 1817 (13.9) |
| Gravity of disease (%) | ||||||||||
| Dangerous | 488 (21.8) | 337 (18.2) | 1719 (24.3) | 1181 (17.0) | 2106 (23.2) | 2253 (17.5) | 2193 (21.2) | 2843 (19.7) | 1915 (20.7) | 2560 (19.6) |
| Severe | 628 (28.0) | 499 (26.9) | 1873 (26.5) | 2141 (30.7) | 2074 (22.8) | 2771 (21.5) | 2610 (25.2) | 3642 (25.2) | 2321 (25.1) | 3267 (25.0) |
| Normal | 1127 (50.2) | 1018 (54.9) | 3481 (49.2) | 3644 (52.3) | 4912 (54.0) | 7858 (61.0) | 5546 (53.6) | 7973 (55.1) | 4997 (54.1) | 7242 (55.4) |
| Percutaneous coronary intervention | 0.14 (0.34) | 0.15 (0.36) | 0.17 (0.38) | 0.15 (0.36) | 0.19 (0.39) | 0.13 (0.33) | 0.23 (0.42) | 0.17 (0.38) | 0.31 (0.46) | 0.24 (0.43) |
| Tertiary hospitals (%) | 2215 (98.8) | 1840 (99.2) | 7013 (99.2) | 6841 (98.2) | 7773 (85.5) | 7855 (61.0) | 8634 (83.4) | 8889 (61.5) | 7859 (85.1) | 8195 (62.7) |
| Elixhauser score | 4.91 (5.90) | 4.99 (5.68) | 6.10 (6.11) | 6.08 (5.91) | 6.46 (6.21) | 5.90 (6.26) | 7.17 (6.18) | 6.46 (6.17) | 7.42 (6.30) | 6.63 (6.28) |
| 2013 | 2014 | 2015 | 2016 | 2017 | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| OR | p-Value | OR | p-Value | OR | p-Value | OR | p-Value | OR | p-Value | |
| (Intercept) | 0.211 | 0.097 | 0.04 | <0.001 | 0.035 | <0.001 | 0.017 | <0.001 | 0.009 | <0.001 |
| Rural (Ref. = Urban) | 0.173 | <0.001 | 0.34 | <0.001 | 0.605 | 0.001 | 0.522 | <0.001 | 0.556 | 0.001 |
| Female (Ref. = Male) | 1.82 | 0.023 | 1.153 | 0.305 | 1.164 | 0.179 | 1.404 | 0.001 | 1.392 | 0.003 |
| Age (Ref. = 18–45) | ||||||||||
| 46–65 | 0.661 | 0.373 | 2.291 | 0.038 | 1.398 | 0.218 | 1.662 | 0.067 | 1.313 | 0.348 |
| 66–75 | 0.961 | 0.935 | 4.059 | 0.001 | 2.915 | <0.001 | 2.863 | <0.001 | 2.069 | 0.014 |
| ≥76 | 2.344 | 0.072 | 6.347 | <0.001 | 3.307 | <0.001 | 4.358 | <0.001 | 3.08 | <0.001 |
| Marriage (Ref. = Married) | ||||||||||
| Unmarried | 2.875 | 0.067 | 1.363 | 0.483 | 0.768 | 0.61 | 0.478 | 0.215 | 1.059 | 0.886 |
| Widowed | 0.376 | 0.136 | 1.119 | 0.686 | 1.22 | 0.297 | 1.015 | 0.93 | 1.293 | 0.171 |
| Divorced | 3.281 | 0.014 | 1.941 | 0.012 | 2.09 | 0.006 | 0.691 | 0.308 | 0.854 | 0.662 |
| Other | 5.028 | 0.141 | 1.642 | 0.438 | 0.882 | 0.767 | 1.501 | 0.18 | 2.387 | 0.003 |
| Occupation (Ref. = Public institution) | ||||||||||
| Private institution | 0.824 | 0.729 | 1.608 | 0.193 | 0.877 | 0.627 | 1.107 | 0.73 | 1.908 | 0.104 |
| Farmer | 1.411 | 0.526 | 2.382 | 0.022 | 0.67 | 0.128 | 1.174 | 0.575 | 2.145 | 0.055 |
| Jobless | 0.478 | 0.305 | 0.731 | 0.509 | 0.738 | 0.357 | 1.209 | 0.559 | 2.059 | 0.09 |
| Retired | 1.082 | 0.882 | 2.273 | 0.017 | 1.399 | 0.15 | 2.052 | 0.006 | 3.615 | 0.001 |
| Other | 0.556 | 0.32 | 0.891 | 0.776 | 0.604 | 0.065 | 1.082 | 0.788 | 1.459 | 0.361 |
| Length of stay (Ref. 1st quartile) | ||||||||||
| 2nd quartile | 0.112 | <0.001 | 0.136 | <0.001 | 0.13 | <0.001 | 0.103 | <0.001 | 0.116 | <0.001 |
| 3rd quartile | 0.023 | <0.001 | 0.062 | <0.001 | 0.085 | <0.001 | 0.048 | <0.001 | 0.076 | <0.001 |
| 4th quartile | 0.107 | <0.001 | 0.118 | <0.001 | 0.149 | <0.001 | 0.119 | <0.001 | 0.225 | <0.001 |
| Gravity of disease (Ref. Normal) | ||||||||||
| Dangerous | 1.655 | 0.041 | 1.707 | <0.001 | 1.553 | <0.001 | 2.305 | <0.001 | 2.323 | <0.001 |
| Severe | 0.48 | 0.032 | 0.825 | 0.23 | 0.866 | 0.308 | 0.968 | 0.794 | 0.97 | 0.831 |
| PCI | 0.566 | 0.292 | 0.137 | <0.001 | 0.296 | <0.001 | 0.339 | <0.001 | 0.423 | <0.001 |
| Level of hospitals (Ref. = Secondary) | ||||||||||
| Tertiary | 0.377 | 0.181 | 0.352 | 0.001 | 0.953 | 0.686 | 1.185 | 0.11 | 1.474 | 0.002 |
| Elixhauser score | 1.053 | 0.002 | 1.023 | 0.011 | 1.023 | 0.002 | 1.018 | 0.008 | 1.016 | 0.025 |
| 2013 | 2014 | 2015 | 2016 | 2017 | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Coefficient | p-Value | Coefficient | p-Value | Coefficient | p-Value | Coefficient | p-Value | Coefficient | p-Value | |
| (Intercept) | 0.33 | 0.012 | 0.515 | 0.001 | 0.163 | <0.001 | 0.147 | <0.001 | 0.154 | <0.001 |
| Rural (Ref. = Urban) | 0.159 | <0.001 | 0.573 | <0.001 | 1.278 | <0.001 | 1.281 | <0.001 | 1.65 | <0.001 |
| Female (Ref. = Male) | 0.895 | 0.282 | 0.968 | 0.524 | 1.013 | 0.753 | 1.082 | 0.056 | 1.147 | 0.001 |
| Age (Ref. = 18–45) | ||||||||||
| 46–65 | 1.006 | 0.964 | 0.965 | 0.588 | 1.003 | 0.956 | 1.015 | 0.803 | 1.184 | 0.006 |
| 66–75 | 1.208 | 0.22 | 1.083 | 0.298 | 1.088 | 0.191 | 1.001 | 0.991 | 1.278 | <0.001 |
| 75+ | 1.508 | 0.014 | 0.999 | 0.994 | 1.009 | 0.898 | 1.158 | 0.042 | 1.405 | <0.001 |
| Marriage (Ref. = Married) | ||||||||||
| Unmarried | 0.151 | <0.001 | 0.343 | <0.001 | 0.627 | 0.004 | 1.114 | 0.437 | 0.882 | 0.219 |
| Widowed | 0.839 | 0.509 | 0.975 | 0.849 | 0.646 | <0.001 | 0.753 | 0.005 | 0.676 | <0.001 |
| Divorced | 0.24 | 0.003 | 0.254 | <0.001 | 0.691 | 0.015 | 0.973 | 0.852 | 1.91 | <0.001 |
| Other | 0.206 | 0.124 | 0.163 | <0.001 | 0.147 | <0.001 | 0.223 | <0.001 | 0.34 | <0.001 |
| Occupation (Ref. = Public institution) | ||||||||||
| Private institution | 2.46 | <0.001 | 0.878 | 0.11 | 0.871 | 0.059 | 1.339 | <0.001 | 1.317 | <0.001 |
| Farmer | 6.43 | <0.001 | 1.134 | 0.175 | 0.575 | <0.001 | 0.776 | 0.003 | 0.585 | <0.001 |
| Jobless | 2.625 | 0.001 | 1.101 | 0.411 | 0.902 | 0.303 | 1.486 | <0.001 | 1.257 | 0.026 |
| Retired | 1.011 | 0.96 | 0.549 | <0.001 | 0.603 | <0.001 | 1.188 | 0.025 | 1.037 | 0.634 |
| Other | 1.784 | 0.008 | 0.203 | <0.001 | 0.348 | <0.001 | 0.318 | <0.001 | 0.551 | <0.001 |
| Length of stay (Ref. 1st quartile) | ||||||||||
| 2nd quartile | 1.261 | 0.054 | 1.279 | <0.001 | 1.085 | 0.077 | 0.914 | 0.044 | 0.766 | <0.001 |
| 3rd quartile | 1.279 | 0.047 | 1.383 | <0.001 | 1.142 | 0.006 | 0.854 | 0.002 | 0.704 | <0.001 |
| 4th quartile | 1.093 | 0.452 | 1.192 | 0.003 | 1.328 | <0.001 | 0.977 | 0.637 | 0.918 | 0.079 |
| Gravity of disease (Ref. Normal) | ||||||||||
| Dangerous | 0.984 | 0.883 | 1.207 | <0.001 | 1.368 | <0.001 | 1.598 | <0.001 | 1.504 | <0.001 |
| Severe | 1 | 0.997 | 1.058 | 0.236 | 1.075 | 0.078 | 0.623 | <0.001 | 0.62 | <0.001 |
| PCI | 3.083 | <0.001 | 1.923 | <0.001 | 2.875 | <0.001 | 4.389 | <0.001 | 2.886 | <0.001 |
| Level of hospital (Ref. = Secondary hospital) | ||||||||||
| Tertiary | 0.508 | 0.077 | 0.638 | 0.008 | 2.375 | <0.001 | 1.74 | <0.001 | 2.004 | <0.001 |
| Elixhauser score | 0.966 | <0.001 | 1.027 | <0.001 | 1.005 | 0.048 | 0.97 | <0.001 | 0.985 | <0.001 |
| 2013 | 2014 | 2015 | 2016 | 2017 | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| OR | p-Value | OR | p-Value | OR | p-Value | OR | p-Value | OR | p-Value | |
| (Intercept) | 8.278 | <0.001 | 7.913 | <0.001 | 7.91 | <0.001 | 7.998 | <0.001 | 7.883 | <0.001 |
| Rural (Ref. = Urban) | 0.075 | 0.352 | 0.61 | <0.001 | 0.565 | <0.001 | 0.439 | <0.001 | 0.46 | <0.001 |
| Female (Ref. = Male) | −0.034 | 0.69 | −0.101 | 0.012 | −0.072 | 0.017 | −0.01 | 0.741 | −0.006 | 0.845 |
| Age (Ref. = 18–45) | ||||||||||
| 46–65 | −0.204 | 0.054 | −0.021 | 0.69 | −0.111 | 0.006 | −0.07 | 0.094 | −0.143 | 0.001 |
| 66–75 | −0.25 | 0.042 | −0.237 | <0.001 | −0.222 | <0.001 | −0.182 | <0.001 | −0.189 | <0.001 |
| 75+ | −0.533 | <0.001 | −0.493 | <0.001 | −0.474 | <0.001 | −0.379 | <0.001 | −0.385 | <0.001 |
| Marriage (Ref. = Married) | ||||||||||
| Unmarried | 0.9 | 0.065 | 0.169 | 0.336 | 0.009 | 0.945 | −0.158 | 0.107 | −0.424 | <0.001 |
| Widowed | 0.281 | 0.185 | −0.168 | 0.109 | 0.01 | 0.9 | −0.183 | 0.019 | −0.051 | 0.499 |
| Divorced | 0.045 | 0.917 | 0.026 | 0.894 | 0.082 | 0.486 | 0.074 | 0.476 | −0.108 | 0.177 |
| Other | −0.071 | 0.941 | 0.007 | 0.987 | −0.015 | 0.956 | −0.056 | 0.799 | −0.396 | 0.022 |
| Occupation (Ref. = Public institution) | ||||||||||
| Private institution | −0.586 | 0.001 | −0.603 | <0.001 | −0.349 | <0.001 | −0.196 | <0.001 | −0.055 | 0.314 |
| Farmer | 0.582 | 0.001 | −0.106 | 0.145 | 0.065 | 0.243 | 0.046 | 0.434 | 0.205 | <0.001 |
| Jobless | −0.195 | 0.407 | −0.142 | 0.107 | 0.039 | 0.572 | −0.046 | 0.526 | 0.16 | 0.026 |
| Retired | −0.199 | 0.292 | -0.362 | <0.001 | −0.045 | 0.374 | 0.01 | 0.859 | 0.069 | 0.204 |
| Other | −0.015 | 0.935 | −0.214 | 0.048 | 0.021 | 0.769 | 0.042 | 0.607 | 0.313 | <0.001 |
| Length of stay (Ref. 1st quartile) | ||||||||||
| 2nd quartile | 0.4 | <0.001 | 0.501 | <0.001 | 0.509 | <0.001 | 0.396 | <0.001 | 0.41 | <0.001 |
| 3rd quartile | 0.584 | <0.001 | 0.689 | <0.001 | 0.749 | <0.001 | 0.625 | <0.001 | 0.577 | <0.001 |
| 4th quartile | 1.047 | <0.001 | 1.139 | <0.001 | 1.224 | <0.001 | 1.115 | <0.001 | 1.035 | <0.001 |
| Gravity of disease | ||||||||||
| Dangerous | −0.201 | 0.019 | 0.079 | 0.055 | 0.005 | 0.855 | 0.213 | <0.001 | 0.091 | 0.001 |
| Severe | −0.171 | 0.028 | −0.027 | 0.465 | −0.1 | 0.001 | −0.131 | <0.001 | −0.094 | 0.003 |
| PCI | 1.233 | <0.001 | 0.887 | <0.001 | 0.752 | <0.001 | 0.844 | <0.001 | 0.869 | <0.001 |
| Level of hospital (Ref. = Secondary hospital) | ||||||||||
| Tertiary | 0.418 | 0.173 | 0.875 | <0.001 | 0.722 | <0.001 | 0.535 | <0.001 | 0.603 | <0.001 |
| Elixhauser score | −0.01 | 0.076 | 0.005 | 0.045 | 0.008 | <0.001 | −0.002 | 0.274 | 0.011 | <0.001 |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cai, M.; Liu, E.; Li, W. Rural Versus Urban Patients: Benchmarking the Outcomes of Patients with Acute Myocardial Infarction in Shanxi, China from 2013 to 2017. Int. J. Environ. Res. Public Health 2018, 15, 1930. https://doi.org/10.3390/ijerph15091930
Cai M, Liu E, Li W. Rural Versus Urban Patients: Benchmarking the Outcomes of Patients with Acute Myocardial Infarction in Shanxi, China from 2013 to 2017. International Journal of Environmental Research and Public Health. 2018; 15(9):1930. https://doi.org/10.3390/ijerph15091930
Chicago/Turabian StyleCai, Miao, Echu Liu, and Wei Li. 2018. "Rural Versus Urban Patients: Benchmarking the Outcomes of Patients with Acute Myocardial Infarction in Shanxi, China from 2013 to 2017" International Journal of Environmental Research and Public Health 15, no. 9: 1930. https://doi.org/10.3390/ijerph15091930
APA StyleCai, M., Liu, E., & Li, W. (2018). Rural Versus Urban Patients: Benchmarking the Outcomes of Patients with Acute Myocardial Infarction in Shanxi, China from 2013 to 2017. International Journal of Environmental Research and Public Health, 15(9), 1930. https://doi.org/10.3390/ijerph15091930





