A Randomized Controlled Trial of a Theory-Informed School-Based Intervention to Prevent Waterpipe Tobacco Smoking: Changes in Knowledge, Attitude, and Behaviors in 6th and 7th Graders in Lebanon
Abstract
1. Introduction
2. Methods
2.1. Sample Size
2.2. Randomization
2.3. Intervention
2.4. Outcomes
2.5. Variables
2.6. Blinding
2.7. Ethical Considerations
2.8. Analysis
3. Results
3.1. Effects of the Intervention on Knowledge Regarding WTS
3.2. Effects of the Intervention on Attitudes Regarding WTS
3.3. Effects of the Intervention on WTS Behavior
4. Discussion
5. Conclusion
Author contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Akl, E.A.; Ward, K.D.; Bteddini, D.; Khaliel, R.; Alexander, A.C.; Lotfi, T.; Alaouie, H.; Afifi, R.A. The allure of the waterpipe: A narrative review of factors affecting the epidemic rise in waterpipe smoking among young persons globally. Tob. Control 2015, 24 (Suppl. 1), i13–i21. [Google Scholar] [CrossRef] [PubMed]
- Salloum, R.G.; Abu-Rmeileh, N.; Hamadeh, R.; Thomas, J.; Mostafa, A.; Yusufali, A.; Kheirallah, K.A.; Macauda, M.M.; Theis, R.P.; El Kadi, L.; et al. Policy-Relevant Context of Waterpipe Tobacco Smoking among University Students in Six Countries Across the Eastern Mediterranean Region: A Qualitative Study. Asian Pac. J. Cancer Prev. 2017, 18, 2533–2540. [Google Scholar] [PubMed]
- Alomari, M.A.; Al-Sheyab, N.A. Impact of waterpipe smoking on blood pressure and heart rate among adolescents: The Irbid-TRY. J. Subst. Use 2018, 23, 280–285. [Google Scholar] [CrossRef]
- El-Zaatari, Z.M.; Chami, H.A.; Zaatari, G.S. Health effects associated with waterpipe smoking. Tob. Control 2015, 24 (Suppl. 1), i31–i43. [Google Scholar] [CrossRef]
- Mamtani, R.; Cheema, S.; Sheikh, J.; Al Mulla, A.; Lowenfels, A.; Maisonneuve, P. Cancer risk in waterpipe smokers: A meta-analysis. Int. J. Public Health 2017, 62, 73–83. [Google Scholar] [CrossRef] [PubMed]
- Montazeri, Z.; Nyiraneza, C.; El-Katerji, H.; Little, J. Waterpipe smoking and cancer: Systematic review and meta-analysis. Tob. Control 2017, 26, 92–97. [Google Scholar] [CrossRef] [PubMed]
- Ramji, R.; Arnetz, B.B.; Nilsson, M.; Wiklund, Y.; Jamil, H.; Maziak, W.; Arnetz, J. Waterpipe use in adolescents in Northern Sweden: Association with mental well-being and risk and health behaviours. Scand. J. Public Health 2017. [Google Scholar] [CrossRef] [PubMed]
- Waziry, R.; Jawad, M.; Ballout, R.A.; Al Akel, M.; Akl, E.A. The effects of waterpipe tobacco smoking on health outcomes: An updated systematic review and meta-analysis. Int. J. Epidemiol. 2017, 46, 32–43. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. TobReg—Advisory Note: Waterpipe Tobacco Smoking: Health Effects, Research Needs and Recommended Actions by Regulators; World Health Organization: Geneva, Switzerland, 2005. [Google Scholar]
- Abdullah, P.; Costanian, C.; Khanlou, N.; Tamim, H. Prevalence and characteristics of water-pipe smoking in Canada: Results from the Canadian Tobacco Use Monitoring Survey. Public Health 2017, 148, 102–108. [Google Scholar] [CrossRef] [PubMed]
- Combrink, A.; Irwin, N.; Laudin, G.; Naidoo, K.; Plagerson, S.; Mathee, A. High prevalence of hookah smoking among secondary school students in a disadvantaged community in Johannesburg. S. Afr. Med. J. Suid-Afrik. Tydskr. Vir Geneeskd. 2010, 100, 297–299. [Google Scholar] [CrossRef]
- Greenhalgh, E.M.; Bayly, M.; Winstanley, M.H. Prevalence of use of different types of tobacco product. In Tobacco in Australia: Facts and Issues; Scollo, M.M., Winstanley, M.H., Eds.; Cancer Council Victoria Melbourne: Melbourne, Australia, 2017. [Google Scholar]
- Maziak, W.; Taleb, Z.B.; Bahelah, R.; Islam, F.; Jaber, R.; Auf, R.; Salloum, R.G. The global epidemiology of waterpipe smoking. Tob. Control 2015, 24 (Suppl. 1), i3–i12. [Google Scholar] [CrossRef]
- Salloum, R.G.; Thrasher, J.F.; Getz, K.R.; Barnett, T.E.; Asfar, T.; Maziak, W. Patterns of Waterpipe Tobacco Smoking Among U.S. Young Adults, 2013–2014. Am. J. Prev. Med. 2017, 52, 507–512. [Google Scholar] [CrossRef] [PubMed]
- Akl, E.A.; Gunukula, S.K.; Aleem, S.; Obeid, R.; Jaoude, P.A.; Honeine, R.; Irani, J. The prevalence of waterpipe tobacco smoking among the general and specific populations: A systematic review. BMC Public Health 2011, 11, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Jawad, M.; Lee, J.T.; Millett, C. Waterpipe Tobacco Smoking Prevalence and Correlates in 25 Eastern Mediterranean and Eastern European Countries: Cross-Sectional Analysis of the Global Youth Tobacco Survey. Nicot. Tob. Res. 2016, 18, 395–402. [Google Scholar] [CrossRef] [PubMed]
- Kheirallah, K.A.; Alsulaiman, J.W.; Mohammad, H.A.; Alzyoud, S.; Veeranki, S.P.; Ward, K.D. Waterpipe Tobacco Smoking among Arab Youth; a Cross-Country Study. Ethn. Dis. 2016, 26, 107–112. [Google Scholar] [CrossRef] [PubMed]
- Dugas, E.; Tremblay, M.; Low, N.C.P.; Cournoyer, D.; O’Loughlin, J. Water-Pipe Smoking Among North American Youths. Pediatrics 2010. [Google Scholar] [CrossRef] [PubMed]
- Ghafouri, N.; Hirsch, J.D.; Heydari, G.; Morello, C.M.; Kuo, G.M.; Singh, R.F. Waterpipe smoking among health sciences university students in Iran: Perceptions, practices and patterns of use. BMC Res. Notes 2011, 4, 496. [Google Scholar] [CrossRef] [PubMed]
- Maziak, W.; Ben Taleb, Z.; Jawad, M.; Afifi, R.; Nakkash, R.; Akl, E.A.; Ward, K.D.; Salloum, R.G.; Barnett, T.E.; Primack, B.A.; et al. Consensus statement on assessment of waterpipe smoking in epidemiological studies. Tob. Control 2017, 26, 338–343. [Google Scholar] [CrossRef] [PubMed]
- WHO (World Health Organization). Global Youth Tobacco Survey, Country Fact Sheets: Lebanon (Ages 13–15); WHO: Geneva, Switzerland, 2012. [Google Scholar]
- Saade, G.; Abou Jaoude, S.; Afifi, R.; Warren, C.; Jones, N. Patterns of tobacco use: Results from the 2005 Global Youth Tobacco Survey in Lebanon. East Mediterr. Health J. 2008, 14, 1280–1289. [Google Scholar] [PubMed]
- Bahelah, R.; DiFranza, J.R.; Ward, K.D.; Eissenberg, T.; Fouad, F.M.; Taleb, Z.B.; Jaber, R.; Maziak, W. Waterpipe smoking patterns and symptoms of nicotine dependence: The Waterpipe Dependence in Lebanese Youth Study. Addict. Behav. 2017, 74, 127–133. [Google Scholar] [CrossRef] [PubMed]
- Lopez, A.A.; Eissenberg, T.; Jaafar, M.; Afifi, R. Now is the time to advocate for interventions designed specifically to prevent and control waterpipe tobacco smoking. Addict. Behav. 2017, 66, 41–47. [Google Scholar] [CrossRef] [PubMed]
- Albuquerque, M.; Starr, G.; Schooley, M.; Pechacek, T.; Henson, R. Advancing Tobacco Control through Evidence-Based Programs; Centers for Disease Control and Prevention, Department of Health and Human Services: Atlanta, GA, USA, 2003.
- Lantz, P.M.; Jacobson, P.D.; Warner, K.E.; Wasserman, J.; Pollack, H.A.; Berson, J.; Ahlstrom, A. Investing in youth tobacco control: A review of smoking prevention and control strategies. Tob. Control 2000, 9, 47–63. [Google Scholar] [CrossRef] [PubMed]
- CDC. Best Practices for Comprehensive Tobacco Control Programs—2014; U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health: Atlanta, GA, USA, 2014.
- Vickers, K.S.; Thomas, J.L.; Patten, C.A.; Mrazek, D.A. Prevention of tobacco use in adolescents: Review of current findings and implications for healthcare providers. Curr. Opin. Pediatr. 2002, 14, 708–712. [Google Scholar] [CrossRef] [PubMed]
- Jawad, M.; Jawad, S.; Waziry, R.K.; Ballout, R.A.; Akl, E.A. Interventions for waterpipe tobacco smoking prevention and cessation: A systematic review. Sci. Rep. 2016, 6, 25872. [Google Scholar] [CrossRef] [PubMed]
- Brinker, T.J.; Stamm-Balderjahn, S.; Seeger, W.; Groneberg, D.A. Education Against Tobacco (EAT): A quasi-experimental prospective evaluation of a programme for preventing smoking in secondary schools delivered by medical students: A study protocol. BMJ Open 2014, 4, e004909. [Google Scholar] [CrossRef] [PubMed]
- Miller, M.P.; Gillespie, J.; Billian, A.; Davel, S. Prevention of smoking behaviors in middle school students: Student nurse interventions. Public Health Nurs. 2001, 18, 77–81. [Google Scholar] [CrossRef] [PubMed]
- Reddy, K.S.; Arora, M.; Perry, C.L.; Nair, B.; Kohli, A.; Lytle, L.A.; Stigler, M.; Prabhakaran, D. Tobacco and alcohol use outcomes of a school-based intervention in New Delhi. Am. J. Health Behav. 2002, 26, 173–181. [Google Scholar] [CrossRef] [PubMed]
- Wiehe, S.E.; Garrison, M.M.; Christakis, D.A.; Ebel, B.E.; Rivara, F.P. A systematic review of school-based smoking prevention trials with long-term follow-up. J. Adolesc. Health 2005, 36, 162–169. [Google Scholar] [CrossRef] [PubMed]
- Thomas, R.E.; McLellan, J.; Perera, R. School-based programmes for preventing smoking. Cochrane Database Syst. Rev. 2013, 4, Cd001293. [Google Scholar]
- Lovato, C.Y.; Zeisser, C.; Campbell, H.S.; Watts, A.W.; Halpin, P.; Thompson, M.; Eyles, J.; Adlaf, E.; Brown, K.S. Adolescent smoking: Effect of school and community characteristics. Am. J. Prev. Med. 2010, 39, 507–514. [Google Scholar] [CrossRef] [PubMed]
- Wakefield, M.A.; Chaloupka, F.J.; Kaufman, N.J.; Orleans, C.T.; Barker, D.C.; Ruel, E.E. Effect of restrictions on smoking at home, at school, and in public places on teenage smoking: Cross sectional study. BMJ 2000, 321, 333–337. [Google Scholar] [CrossRef] [PubMed]
- Johnson, C.A.; Cen, S.; Gallaher, P.; Palmer, P.H.; Xiao, L.; Ritt-Olson, A.; Unger, J.B. Why smoking prevention programs sometimes fail. Does effectiveness depend on sociocultural context and individual characteristics? Cancer Epidemiol. Biomark. Prev. 2007, 16, 1043–1049. [Google Scholar] [CrossRef] [PubMed]
- Saraf, D.S.; Nongkynrih, B.; Pandav, C.S.; Gupta, S.K.; Shah, B.; Kapoor, S.K.; Krishnan, A. A systematic review of school-based interventions to prevent risk factors associated with noncommunicable diseases. Asia-Pac. J. Public Health 2012, 24, 733–752. [Google Scholar] [CrossRef] [PubMed]
- Milton, M.; Maule, C.; Yee, S.; Backinger, C.; Malarcher, A.; Husten, C. Youth Tobacco Cessation: A Guide for Making Informed Decisions; U.S. Department of Health and Human Services, Centers for Disease Control and Prevention: Atlanta, GA, USA, 2004.
- Anjum, Q.; Ahmed, F.; Ashfaq, T. Knowledge, attitude and perception of water pipe smoking (Shisha) among adolescents aged 14–19 years. J. Pak. Med. Assoc. 2008, 58, 312–317. [Google Scholar] [PubMed]
- Stamm-Balderjahn, S.; Groneberg, D.A.; Kusma, B.; Jagota, A.; Schönfeld, N. Smoking Prevention in School Students. Deutsch. Aerzteblatt Int. 2012, 109, 746–752. [Google Scholar] [CrossRef] [PubMed]
- Quadri, M.F.; Saleh, S.M.; Alsanosy, R.; Abdelwahab, S.I.; Tobaigy, F.M.; Maryoud, M.; Al-Hebshi, N. Effectiveness of an intervention program on knowledge of oral cancer among the youth of Jazan, Saudi Arabia. Asian Pac. J. Cancer Prev. 2014, 15, 1913–1918. [Google Scholar] [CrossRef] [PubMed]
- Essa-Hadad, J.; Linn, S.; Rafaeli, S. A Web-Based Program to Increase Knowledge and Reduce Cigarette and Nargila Smoking Among Arab University Students in Israel: Mixed-Methods Study to Test Acceptability. J. Med. Internet Res. 2015, 17, e39. [Google Scholar] [CrossRef] [PubMed]
- Lipkus, I.M.; Eissenberg, T.; Schwartz-Bloom, R.D.; Prokhorov, A.V.; Levy, J. Affecting Perceptions of Harm and Addiction among College Waterpipe Tobacco Smokers. Nicot. Tob. Res. 2011, 13, 599–610. [Google Scholar] [CrossRef] [PubMed]
- Mays, D.; Tercyak, K.P.; Lipkus, I.M. The Effects of Brief Waterpipe Tobacco Use Harm and Addiction Education Messages Among Young Adult Waterpipe Tobacco Users. Nicot. Tob. Res. 2016, 18, 777–784. [Google Scholar] [CrossRef] [PubMed]
- Islam, F.; Salloum, R.G.; Nakkash, R.; Maziak, W.; Thrasher, J.F. Effectiveness of health warnings for waterpipe tobacco smoking among college students. Int. J. Public Health 2016, 61, 709–715. [Google Scholar] [CrossRef] [PubMed]
- Sutfin, E.L.; Cornacchione Ross, J.; Lazard, A.J.; Orlan, E.; Suerken, C.K.; Wiseman, K.D.; Reboussin, B.A.; Wolfson, M.; Noar, S.M. Developing a Point-of-Sale Health Communication Campaign for Cigarillos and Waterpipe Tobacco. Health Commun. 2017, 1–9. [Google Scholar] [CrossRef] [PubMed]
- CAS. Multiple Indicators Cluster Survey, Round 3 (MICS3): Final Report; Central Administration of Statistics in collaboration with UNICEF: Lebanon, IN, USA, 2009.
- Moher, D.; Hopewell, S.; Schulz, K.F.; Montori, V.; Gøtzsche, P.C.; Devereaux, P.J.; Elbourne, D.; Egger, M.; Altman, D.G. CONSORT 2010 explanation and elaboration: Updated guidelines for reporting parallel group randomised trials. Int. J. Surg. 2012, 10, 28–55. [Google Scholar] [CrossRef] [PubMed]
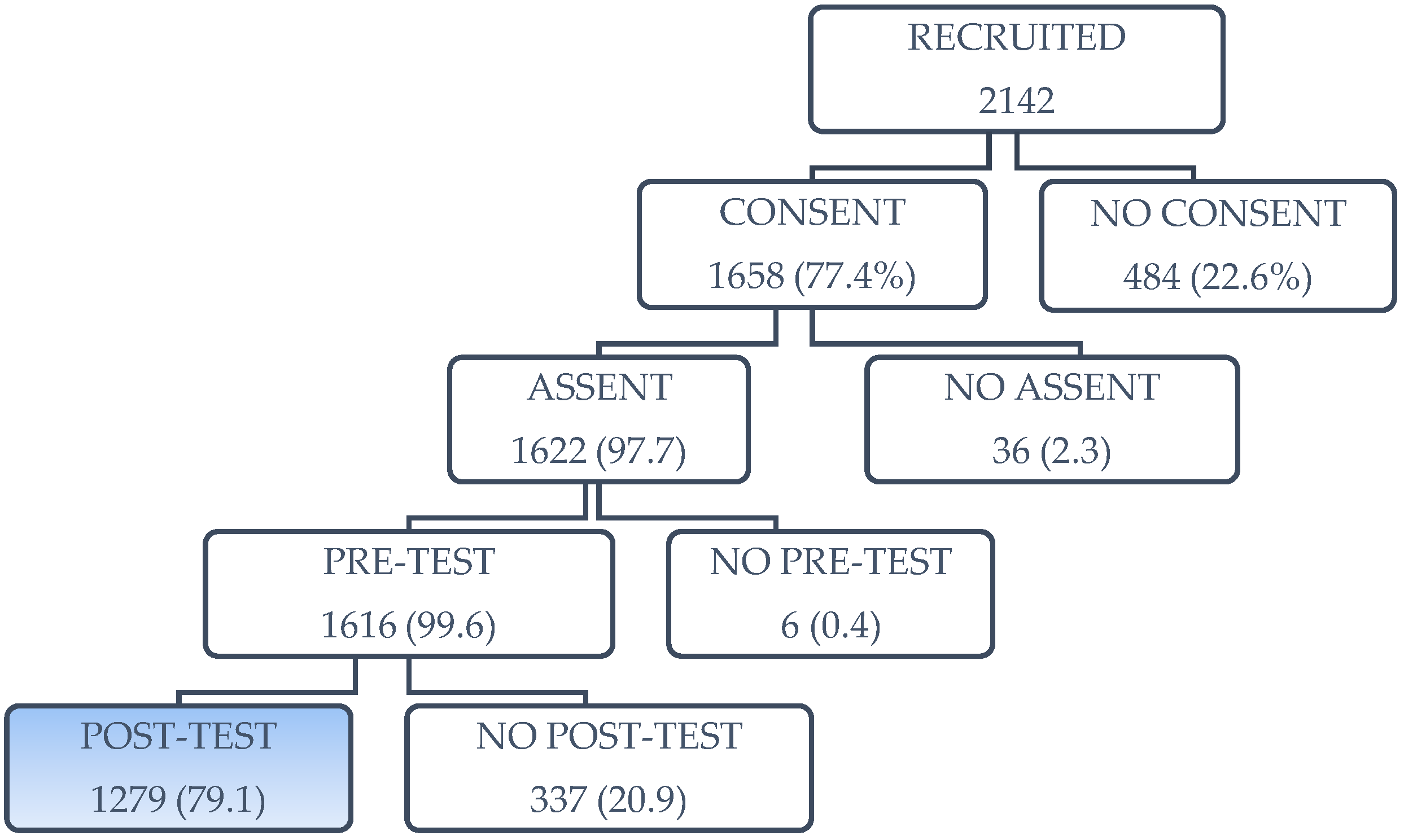
- Nakkash, R.T.; Al Mulla, A.; Torossian, L.; Karhily, R.; Shuayb, L.; Mahfoud, Z.R.; Janahi, I.; Al Ansari, A.A.; Afifi, R.A. Challenges to obtaining parental permission for child participation in a school-based waterpipe tobacco smoking prevention intervention in Qatar. BMC Med. Ethics 2014, 15, 70. [Google Scholar] [CrossRef] [PubMed]
- Glanz, K.; Rimer, B.K.; Viswanath, K. Theory, Research, and Practice in Health Behavior and Health Education. In Health Behavior: Theory, Research, and Practice, 5th ed.; Glanz, K., Rimer, B.K., Viswanath, K., Eds.; Jossey-Bass: San Francisco, CA, USA, 2015. [Google Scholar]
- Bteddini, D.; Afifi, R.; Haddad, P.; Jbara, L.; Alaouie, H.; Al Aridi, L.; Mahfoud, Z.; Al Mulla, A.; Nakkash, R. Process evaluation and challenges of implementation of a school-based waterpipe tobacco smoking prevention program for teens in Lebanon. Tob. Prev. Cessat. 2017, 3. [Google Scholar] [CrossRef]
- Jawad, M.; Afifi, R.A.; Mahfoud, Z.; Bteddini, D.; Haddad, P.; Nakkash, R. Validation of a simple tool to assess risk of waterpipe tobacco smoking among sixth and seventh graders in Lebanon. J. Public Health 2016, 38, 403–410. [Google Scholar] [CrossRef] [PubMed]
- Jawad, M.; Nakkash, R.T.; Mahfoud, Z.; Bteddini, D.; Haddad, P.; Afifi, R.A. Parental smoking and exposure to environmental tobacco smoke are associated with waterpipe smoking among youth: Results from a national survey in Lebanon. Public Health 2015, 129, 370–376. [Google Scholar] [CrossRef] [PubMed]
- Kandel, D.S.E.; Kessler, R.C. The Epidemiology of Drug Use among New York State High School Students: Distribution, Trends, and Change in Rates of Use. Am. J. Public Health 1976, 66, 43–53. [Google Scholar] [CrossRef] [PubMed]
- Hansen, W.B.; Graham, J.W. Preventing alcohol, marijuana, and cigarette use among adolescents: Peer pressure resistance training versus establishing conservative norms. Prev. Med. 1991, 20, 414–430. [Google Scholar] [CrossRef]
- Faggiano, F.; Vigna-Taglianti, F.; Burkhart, G.; Bohrn, K.; Cuomo, L.; Gregori, D.; Panella, M.; Scatigna, M.; Siliquini, R.; Varona, L.; et al. The effectiveness of a school-based substance abuse prevention program: 18-month follow-up of the EU-Dap cluster randomized controlled trial. Drug Alcohol Depend. 2010, 108, 56–64. [Google Scholar] [CrossRef] [PubMed]
- Green, L.W.; Kreuter, M.W. Health Program Planning: An Educational and Ecological Approach; McGraw-Hill Higher Education: New York, NY, USA, 2005. [Google Scholar]
- McLeroy, K.R.; Bibeau, D.; Steckler, A.; Glanz, K. An ecological perspective on health promotion programs. Health Educ. Q. 1988, 15, 351–377. [Google Scholar] [CrossRef] [PubMed]
- Wong, S.L.; Shields, M.; Leatherdale, S.; Malaison, E.; Hammond, D. Assessment of validity of self-reported smoking status. Health Rep. 2012, 23, 47–53. [Google Scholar] [PubMed]
- WHO. WHO Report on the Global Tobacco Epidemic, 2017: Monitoring Tobacco Use and Prevention Policies; World Health Organization: Geneva, Switzerland, 2017. [Google Scholar]
| Variable | Total | Intervention Gp. | Control Gp. | |
|---|---|---|---|---|
| % (N) | % (N) | % (N) | ||
| Group (N = 1279) | Control | 47.4% (606) | ||
| Intervention | 52.6% (673) | |||
| Age (N = 1267) | Mean (SD) | 12.27 (1.12) | 12.26 (1.11) | 12.28 (1.13) |
| Sex (N = 1264) | Male | 48.7% (615) | 48.4% (322) | 48.9% (293) |
| Female | 51.3% (649) | 51.6% (343) | 51.1% (306) | |
| Governorate (N = 1279) * | Beirut | 12.4% (159) | 15.2% (102) | 9.4% (57) |
| Bekaa | 14.9% (190) | 19.9% (134) | 9.2% (56) | |
| Mount Lebanon | 25.9% (331) | 21.5% (145) | 30.7% (186) | |
| Nabatieh | 8.0% (103) | 8.3% (56) | 7.8% (47) | |
| North | 28.2% (361) | 27.2% (183) | 29.4% (178) | |
| South | 10.6% (135) | 7.9% (53) | 13.5% (82) | |
| Student’s self-reported school performance (N = 1219) | Below average | 3.4% (42) | 3.4% (22) | 3.5% (20) |
| Average | 65.9% (803) | 65.9% (425) | 65.8% (378) | |
| Above average | 30.7% (374) | 30.7% (198) | 30.7% (176) | |
| Socioeconomic Status (N = 1173) | Much poorer & poorer | 5.5% (64) | 4.7% (29) | 6.3% (35) |
| No difference | 71.4% (838) | 71.5% (444) | 71.4% (394) | |
| Wealthier & much wealthier | 23.1% (271) | 23.8% (148) | 22.3% (123) | |
| Grade Level (N = 1279)* | 6th grade | 46.7% (598) | 43.7% (294) | 50.2% (304) |
| 7th grade | 53.2% (681) | 56.3% (379) | 49.8% (302) | |
| School type (N = 1279) | Public | 49.4% (632) | 49.9% (336) | 48.8% (296) |
| Private | 50.6% (647) | 50.1% (337) | 51.2% (310) | |
| Parents smoke cigarettes (N = 1234) | At least one parent | 62.6% (768) | 64.9% (417) | 60.1% (351) |
| Neither parent | 37.4% (458) | 35.1% (225) | 39.9% (233) | |
| Parents smoke waterpipe (N = 1256) | At least one parent | 43.6% (544) | 43.1% (290) | 44.1% (254) |
| Neither parent | 56.4% (704) | 55.9% (368) | 56.9% (336) | |
| Pre-Assessment (% Yes) | Post-Assessment (% Yes) | |||||
|---|---|---|---|---|---|---|
| Variable | Intervention | Control | p-Value † | Intervention | Control | p-Value † |
| Waterpipe smoking can cause lung cancer. | 74.80% | 78.85% | 0.286 | 93.40% | 80.65% | <0.001 * |
| Waterpipe smoking can cause oral (mouth) cancer. | 44.39% | 43.41% | 0.840 | 90.09% | 65.63% | <0.001 * |
| Waterpipe smoking can cause bladder cancer. | 32.28% | 26.89% | 0.213 | 71.91% | 43.18% | <0.001 * |
| Waterpipe smoking can cause heart problems. | 77.61% | 81.47% | 0.080 | 91.51% | 81.31% | <0.001 * |
| Waterpipe smoking can cause respiratory problems. | 80.16% | 81.63% | 0.646 | 90.48% | 83.36% | 0.009 * |
| Waterpipe smoking can cause addiction. | 61.09% | 57.58% | 0.481 | 90.59% | 69.91% | <0.001 * |
| Waterpipe tobacco has nicotine in it. | 52.12% | 51.26% | 0.879 | 90.73% | 60.24% | <0.001 * |
| Waterpipe tobacco has dangerous chemical substances in it. | 62.32% | 63.83% | 0.664 | 85.14% | 66.96% | <0.001 * |
| The waterpipe smoke has carbon monoxide in it. | 39.58% | 42.60% | 0.563 | 72.07% | 43.81% | <0.001 * |
| The fruits in the tobacco make the waterpipe a healthier choice. | 15.02% | 14.95% | 0.986 | 19.56% | 12.46% | 0.011 * |
| The water in the bowl helps clean the waterpipe from toxic substances. | 28.01% | 24.14% | 0.358 | 30.02% | 23.86% | 0.092 |
| Using a filter will prevent the exposure to toxic substances. | 35.23% | 34.90% | 0.929 | 37.75% | 33.51% | 0.234 |
| Using a mouth piece will prevent transfer of bacteria. | 34.33% | 35.56% | 0.760 | 42.35% | 39.89% | 0.406 |
| Sharing the waterpipe can cause the transfer of infectious diseases from one person to the other. | 62.94% | 65.36% | 0.458 | 76.53% | 68.33% | 0.019 * |
| Smoking waterpipe around people who are not smoking puts them at risk of health problems. | 66.29% | 64.73% | 0.569 | 76.13% | 69.07% | 0.031 * |
| Pre-assessment (% Agree) | Post-assessment (% Agree) | |||||
|---|---|---|---|---|---|---|
| Variable | Intervention | Control | p-Value † | Intervention | Control | p-Value † |
| Smoking waterpipe is a bad habit. | 83.76% | 83.19% | 0.865 | 86.50% | 84.21% | 0.458 |
| Once someone has started using the waterpipe, it is difficult to quit. | 57.45% | 63.62% | 0.103 | 69.20% | 65.69% | 0.359 |
| If I smoke waterpipe, I would relax. | 29.37% | 32.10% | 0.277 | 26.57% | 30.12% | 0.376 |
| If I smoke waterpipe, I would have more friends. | 21.99% | 25.09% | 0.340 | 23.03% | 23.85% | 0.847 |
| If I smoke waterpipe, I would be more attractive. | 30.35% | 30.00% | 0.927 | 27.30% | 28.06% | 0.842 |
| If I smoke waterpipe, I would have a good time. | 33.22% | 33.99% | 0.829 | 28.85% | 35.63% | 0.139 |
| If I smoke waterpipe, I can get addicted to it. | 52.76% | 51.50% | 0.792 | 69.60% | 56.26% | 0.009 * |
| If I smoke waterpipe, there is a chance that my hair, clothes or breath will smell. | 65.62% | 60.88% | 0.265 | 75.59% | 71.45% | 0.297 |
| I’m more likely to have lung cancer when I grow up if I smoke waterpipe than if I don’t. | 59.46% | 63.44% | 0.331 | 72.58% | 65.30% | 0.055 |
| I’m more likely to have oral (mouth) cancer when I grow up if I smoke waterpipe than if I don’t. | 43.52% | 46.42% | 0.393 | 68.35% | 55.75% | 0.001 * |
| I’m more likely to have bladder cancer when I grow up if I smoke waterpipe than if I don’t. | 33.01% | 34.88% | 0.602 | 57.42% | 42.76% | <0.001 * |
| I’m more likely to have heart problems when I grow up if I smoke waterpipe than if I don’t. | 58.08% | 60.89% | 0.404 | 68.83% | 60.31% | 0.057 |
| If I smoke there’s a chance that my teeth color might change with time. | 65.97% | 68.96% | 0.172 | 80.94% | 73.10% | 0.075 |
| Variable | Intervention-Control (Unadjusted) Mean±SE | p-Value † | Intervention-Control (Adjusted) ‡ Mean±SE | p-Value † |
|---|---|---|---|---|
| More knowledgeable about the harms of WTS | 2.12 (0.30) | <0.001 * | 2.17 (0.25) | <0.001 * |
| More negative attitude towards WTS ** | 0.75 (0.24) | 0.031 * | 0.87 (0.21) | 0.005 * |
| OR (95% CI) | p-Value † | Adjusted OR (95% CI) | p-Value † | |
| Have you ever tried waterpipe (even one or two inhalations)? | 0.881 (0.701, 1.106) | 0.631 | 1.070 (0.815, 1.404) | 0.751 |
| Did you smoke waterpipe at least once in the last month? | 1.043 (0.743, 1.466) | 0.836 | 0.906 (0.591, 1.389) | 0.484 |
| Have you tried to stop smoking waterpipe? | 0.733 (0.476, 1.13) | 0.331 | 0.554(0.321, 0.954) | 0.052 |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nakkash, R.; Lotfi, T.; Bteddini, D.; Haddad, P.; Najm, H.; Jbara, L.; Alaouie, H.; Al Aridi, L.; Al Mulla, A.; Mahfoud, Z.; et al. A Randomized Controlled Trial of a Theory-Informed School-Based Intervention to Prevent Waterpipe Tobacco Smoking: Changes in Knowledge, Attitude, and Behaviors in 6th and 7th Graders in Lebanon. Int. J. Environ. Res. Public Health 2018, 15, 1839. https://doi.org/10.3390/ijerph15091839
Nakkash R, Lotfi T, Bteddini D, Haddad P, Najm H, Jbara L, Alaouie H, Al Aridi L, Al Mulla A, Mahfoud Z, et al. A Randomized Controlled Trial of a Theory-Informed School-Based Intervention to Prevent Waterpipe Tobacco Smoking: Changes in Knowledge, Attitude, and Behaviors in 6th and 7th Graders in Lebanon. International Journal of Environmental Research and Public Health. 2018; 15(9):1839. https://doi.org/10.3390/ijerph15091839
Chicago/Turabian StyleNakkash, Rima, Tamara Lotfi, Dima Bteddini, Pascale Haddad, Hala Najm, Lina Jbara, Hala Alaouie, Lama Al Aridi, Ahmad Al Mulla, Ziyad Mahfoud, and et al. 2018. "A Randomized Controlled Trial of a Theory-Informed School-Based Intervention to Prevent Waterpipe Tobacco Smoking: Changes in Knowledge, Attitude, and Behaviors in 6th and 7th Graders in Lebanon" International Journal of Environmental Research and Public Health 15, no. 9: 1839. https://doi.org/10.3390/ijerph15091839
APA StyleNakkash, R., Lotfi, T., Bteddini, D., Haddad, P., Najm, H., Jbara, L., Alaouie, H., Al Aridi, L., Al Mulla, A., Mahfoud, Z., & Afifi, R. A. (2018). A Randomized Controlled Trial of a Theory-Informed School-Based Intervention to Prevent Waterpipe Tobacco Smoking: Changes in Knowledge, Attitude, and Behaviors in 6th and 7th Graders in Lebanon. International Journal of Environmental Research and Public Health, 15(9), 1839. https://doi.org/10.3390/ijerph15091839





